Abstract
Diabetes is a significant health issue that threatens patients’ overall wellbeing and quality of life. Critical public health concerns center on creating the best approach for diabetes management. Patients and caregivers have different approaches to diabetes management; however, this and the associated physiological, physical and mental health issues remain challenging. This review explores the potential influences of religiosity and religious coping strategies on people with diabetes. This study used a literature review approach to investigate how religiosity and religious coping strategies can influence the effective management of diabetes among patients. Based on the literature search, the researchers were able to identify and cite published papers that were analyzed using the descriptive-narrative analysis. An important goal of the descriptive-narrative analysis was to provide descriptions of the selected literature and take implications from the literature. The results of studies reviewed show some religious coping strategies for managing chronic diseases such as diabetes. The studies did establish a relationship between religiosity and diabetes management and suggest that religious coping strategies could positively impact the management of diabetes; however, they reported some adverse effects. Hence, we propose a pathway for the development of religion-oriented interventions and support framework for the management of diabetes.
Keywords: Diabetes mellitus, Religiosity, Religious belief, Religious coping strategies, Self-care management, Social support
Core tip: Diabetes is a significant health issue that threatens patients’ overall wellbeing and quality of life. Critical public health concerns center on creating the best approach for diabetes management. Patients and caregivers have different approaches to diabetes management; however, this and the associated physiological, physical and mental health issues remain challenging. This review explored the potential influences of religiosity and religious coping strategies on people with diabetes.
INTRODUCTION
Diabetes is a chronic disease that occurs when the pancreas is no longer able to produce the hormone insulin, or when the body cannot effectively use the insulin it produces. Insulin regulates the absorption of glucose from blood into the liver, fat and skeletal muscle cells to produce energy. Loss of insulin production or effective use leads to increased blood glucose levels (known as hyperglycemia). Chronic high glucose levels are associated with damage to the body and organs and tissue failure[1]. However, once diagnosed, insulin levels are controlled externally.
The prevalence of diabetes is increasing worldwide. In 2019, approximately 463 million people had diabetes mellitus (DM), which is projected to increase to 578 million by 2030 and 700 million by 2045[2]. The prevalence of diabetes is projected to be higher in urban areas (10.8%) than in rural areas (7.2%) and in high-income (10.4%) than in low-income (4.0%) nations[2]. In Africa, its prevalence is projected to increase by 98%, from 13.6 million in 2003 to 26.9 million by 2025[3]. A comparable increase (97%) is anticipated in the Middle East, with an estimated prevalence of 35.9 million[3].
DM can induce a series of reactions during diagnosis and several psychosocial stressors during its course[4]. Impending psychological stress and adverse emotional responses associated with DM have constituted overwhelming economic, social, and public health burdens[5]. In Africa, DM management has posed difficulties because of the diverse approaches used by patients and clinicians[6]. An emerging approach focuses on the use of religiosity and religious coping strategies by patients and family members. The relationship between religion and health has changed over time. For some time, religion has been discussed as a hindrance to medical treatment. However, since its inception, religion has addressed matters of paramount importance to humanity, matters of life, suffering, and death, including psychology and emotions[7]. Major religions portray life as a sacred gift that can be enjoyed and used wisely. There are countless religious injunctions on how to live life well as warnings about the failure to do so. Additionally, religion speaks powerfully to the darker aspects of human existence[8]. People with religious or spiritual beliefs adjust better to disease diagnosis and show greater compliance with drug therapy. Moreover, they have more positive mental health indicators with a lower frequency of anxiety or depressive symptoms than atheists[9]. To date, research has focused on the influence of religion on poor health management and chronic diseases, such as DM. This review sought to assess the influence of religiosity and religious coping strategies on people with diabetes.
METHODOLOGY
This study used a literature review approach to investigate how religiosity and religious coping strategies can improve the effective management of diabetes. Here, we propose a pathway for the development of religion-oriented interventions and support framework for the management of diabetes. Ethics approval was not required since the study did not involve human participants. As a mini-review, informed consent was also not required for this study. Based on the literature search, the researchers were able to identify and cite published papers which were then analyzed using the descriptive-narrative analysis. An important goal of the descriptive-narrative analysis was to provide descriptions of the selected literature and take implications from the literature. During the literature search, the authors were able to find information on people with diabetes, and the potential influences of religiosity and religious coping on people with diabetes from a number of databases and sources, such as Google Scholar, Professional Association Websites, PubMed, Scopus, JSTOR, and PsycArticles, which were used for obtaining peer-reviewed articles, gray literature, or books. A number of search terms were used, including religious coping with diabetes; religiosity and diabetes management; spirituality and diabetes support; and social support and diabetes. Searching, evaluating, selecting, and synthesizing qualitative and quantitative papers published in English was the responsibility of the authors.
DISCUSSION
Religiosity and diabetes self-care management
Religiosity is defined as an individual’s commitment to any religion[9]. The distinction between religion and religiosity is that religion is an organized and common system of beliefs that honors God. This is expressed through external rituals of devotion or worship, and promotes the relationship of the individual with God or with a higher power. In contrast, religiosity represents participation in observance within a specific religion[10]. The conceptualization of religiosity is a complex process because of the multidimensional nature of the construct[11]. Religiosity can affect the management of ill health, including diabetes, in areas like self-care[12], mental health[11,13] and social support[13]. Beyond providing a sense of global meaning to life, religiosity can help patients reframe their illness in a larger spiritual context, which is a form of situational meaning making. For example, Pakistani and Iranian Muslim patients stated that they believed that their medical conditions were gifts from God intended to strengthen their faith, absolve them of their sin, and foreshadow divine blessings in this life or the next[7].
The belief that God has control over one’s own efforts in promoting health has been shown among people with chronic illnesses such as rheumatoid arthritis and systemic sclerosis[12,14]. Religious beliefs are regarded as contributors to maintaining well-being and mental health in DM[12,15,16]. This can help determine self-care management efforts. Patients with DM who believe in and trust the process of disease management are more likely to utilize self-care strategies[17,18]. Self-care is a concept that is led, owned, and performed by the community, and entails actions embedded in the daily lives of people with chronic conditions[12,19]. This involves a wide range of behaviors that maintain well-being, such as health promotion and disease prevention, treatment, monitoring, and rehabilitation[12,19].
Other studies have revealed the negative influence of religious beliefs on the self-management of chronic conditions[12,20,21]. Swihart et al[21] reported that some religions have strict prayer times, which may interfere with medical treatment. In addition, Pfeiffer et al[17] found that high religious self-regulation skills increased the likelihood of healthy food intake in a community-based study. Furthermore, religious coping strategies tend to assist in the management of maladaptive eating[22]. Differences have emerged regarding the interpretation of religious teachings on self-management and its acceptability by the supreme God[10]. However, observing spiritual routines associated with religiosity can build support and change negative perceptions[23,24]. For example, church attendance promotes well-being through associated social support, building relationships, and an increased sense of belonging[23]. In addition, spiritual support, adherence to treatment programs, spiritual imaging, prayer, and spiritual self-defense can reduce negative emotions and improve patients’ mental health and hope[24].
Organizational religious activities such as church attendance promote private religious behaviors, including religious rituals such as prayer and scripture[17]. Personal spiritual routines are associated with health benefits and positive health outcomes[7,17,19,25]. Studies have revealed that engagement in private religious activities is associated with increased survival in elderly communities. Prayer is associated with decreased adverse outcomes in patients with cardiac disease[5-8,17,22]. In a qualitative review of how people with diabetes perceive the role of religion and/or spirituality in managing daily self-care, Permana[12] found several themes, such as relationships with God or the transcendent, religion, or spirituality as coping methods, religious practices, and social support. This finding suggests that religiosity can promote self-care.
Religiosity, mental health and social support among patients with diabetes
Patients with DM are more likely to experience mental health challenges than their nondiabetic counterparts[11]. Religiosity and self-acceptance can decrease anxiety disorders and depression among individuals with DM[13]. Religiosity decreases anxiety in patients who donate kidneys[22]. The factors suspected to influence depression include patients’ perceptions of social support and their acceptance of illness. Additionally, the factors that affect anxiety include religiosity and self-acceptance[13]. Most religious practices and beliefs encourage self-acceptance; therefore, religiosity can be an antidote for depression and anxiety, especially in chronic conditions. The religious dimension of coping mechanisms is often disregarded in research studies; nonetheless, there are some potential findings on its specific outcomes in health promotion. Many individuals report using religious coping when facing chronic and acute stressors[26,27].
Recent studies investigating the effects of religiosity on health consequences indicate a significant connection between religiosity and enhanced mental health[24], including reduced depression[27], anxiety[28] and psychological stress[29]. Moreover, studies on individuals with medical conditions have reported a positive link between religious coping, quality of life and better physical well-being[30]. For example, religion aids in stress reduction through coping and allows individuals to engage in healthier lifestyles[17]. Additionally, a positive relationship has been found between church attendance and good mental health, marital stability, improved social interactions, and healthier dietary and physical activity[17]. Religious service attendance is a protective factor against major depression[27] and anxiety[28].
Psychosocial aspects are essential elements of DM self-management[13,31]. These include the psychosocial aspects of social support, motivation (beliefs and attitudes), and coping skills. Research on social support suggests that it reduces psychological burden, such as depression and anxiety[32]. Additionally, people with high social support experience lower levels of stress than those with low social support[33]. Social support can reduce the possibility of illness, accelerate recovery, and reduce the risk of disease-related mortality[13,32]. Furthermore, it can help minimize the occurrence of complications from serious health problems[32]. Taken together, these data show that social support is helpful in managing chronic illnesses, such as DM. Furthermore, global religions focus on the importance of helping and supporting one another; therefore, religiosity affects DM management by influencing social support.
There is a correlation between social support for religiosity and DM management. For example, researchers[33,34] have found a positive relationship between religious support and lower depressive symptoms and heavy drinking over time. The authors further indicated a negative interaction between depressive symptoms and decreased emotional functioning. Perceived social support plays a significant role in depression, through self-acceptance. Perceived social support increases self-acceptance before decreasing depression[13] (Table 1).
Table 1.
Results on potential influence of religiosity on people with diabetes
|
Refs
|
Study objectives
|
Method/sample
|
Results
|
| Darvyri et al[6] | To evaluate the impact of spirituality/religiosity on T2DM management. To summarize the evidence regarding T2DM outcomes as they are related to religiosity or spirituality of patients | Qualitative studies (cross-sectional) | A positive relationship between religiosity/spirituality and improved T2DM management. Participation in church and spiritual beliefs had ameliorating effects on stress levels and glycemic control |
| Kilbourne et al[11] | To examine the impact of multiple dimensions of religiosity on depression among a lower income population of people with DM | Cross-sectional study (multi-centered random sampling) | Religious resources increase psychological resiliency among those managing the chronic stress of diabetes |
| Permana[12] | To identify, appraise and synthesize the best available evidence worldwide, including Indonesia, related to how people with DM perceive the role of religion and/or spirituality in managing daily self-care | A critical appraisal using an adapted CASP tool | Relationship with God or the transcendent, religion or spirituality, religious practices, and social support are crucial for people with DM |
| Yuniarti et al[13] | To examine the mediation states of the variables in three quantitative studies | Conducted using a quantitative approach, using 68 participants aged 40–75 yr. Interviewer-administered questionnaires were used for the data collection | Self-acceptance was significantly related to depression. Religiosity was significantly associated with stress |
| Berardi et al[32] | To determine if fatalistic beliefs were associated with elevated levels of glycated hemoglobin. To establish the role of religiosity in this relationship | Cross-sectional survey (simple random sampling) | Addressing fatalistic attitudes may be a viable strategy for improving DM management. Greater understanding of the interplay between religiosity and fatalism in this context is required |
| Rivera-Hernandez[35] | To examine the relationships between religiosity, social support, disease care and control, and self-rated health of people living in Mexico diagnosed with DM | Structural equation modelling using the Mexican Health and Aging Study | Emotional support from spouse/partner directly affects disease care and control, and health. No direct relationship between religiosity and health; however, religiosity was positively associated with disease care and management. No significant relationship with health |
| Nyarko et al[36] | To examine the influence of the illness perception of patients with DM and their levels of religiosity on their mental health problems | Cross-sectional survey study design | Patients’ level of religiosity was not correlated with their mental health problems. Illness perception was positively correlated with their general mental health, and specific problems, such as somatization, obsessive-compulsion, depression, anxiety, and psychoticism |
| Namageyo-Funa et al[37] | To explore how Black men use religion or spirituality to cope with DM management | In-depth interviews with 30 Black men recruited from a diabetes clinic in Atlanta, Georgia | Religion and spirituality use as a coping strategy for DM management. The following coping strategies were reported: Prayer and belief in God, keeping me alive, turning things over to God, changing my unhealthy behaviors, supplying my needs, reading the Bible, and religious or spiritual individuals helping me |
T2DM: Type 2 diabetes mellitus; DM: Diabetes mellitus; CASP: Critical Appraisal Skills Programme.
RELIGIOUS COPING STRATEGIES AND DIABETES MANAGEMENT
Religion is an essential element of human existence worldwide[33-37]. Additionally, it is an ideal tool when experiencing stressors, maintaining a sense of control, psychological balance after a traumatic experience, and a threatening disease condition[27,28,36-38]. Coping is a response aimed at diminishing the physical, emotional and psychological burdens associated with stressful life events and daily hassles[38,39]. It is a process of constantly changing cognitive, behavioral and emotional efforts to manage external and/or internal demands that are appraised as taxing or exceeding the resources of the individual[26]. Coping includes cognitive appraisals and behavioral efforts that change the relationship between a specific stressor and health reactions, thereby causing stress mitigation[40]. One study found that accepting responsibility is a mediator between stress and quality of life[6]. The mediating effect of coping strategies on religious/spiritual struggles and life satisfaction was shown by a positive correlation between religious comfort and life satisfaction. In contrast, fear/guilt, negative emotions towards God, and negative social interactions surrounding religion are negatively correlated with life satisfaction[41].
Increasing evidence suggests that religious beliefs and practices create options for coping with difficult situations such as illness[5,33,42]. Prayer, abstinence from alcohol and smoking, and persistent hope in God positively influence the treatment of DM[5]. Spiritual and religious beliefs and activities can aid in coping after a diagnosis of chronic illness by providing support, confidence and hope. However, it may interfere with successful coping[37,38]; dogmatic religious practices can hamper management by making patients neglect self-care activities and rely on prayer and/or meditation to manage their illnesses[18]. Most religious activities help eliminate worry and anxiety, which directly helps with stress reduction and DM management[5,17,33].
Religious coping strategies serve as emotional support because individuals can rely heavily on their relationship with God to handle negative subjective feelings associated with chronic conditions. Believing that God gives considerable strength to faithful patients because they believe in God as a superior power that can do all things. Reliance on supernatural power can minimize pressure to control circumstances and avoid anxiety about results[43,44]. This positive appraisal of a stressful life situation can control anxiety and feelings of hopelessness and despair[45]. Religious coping strategies provide emotional support and optimistic explanations of life events that can aid the use of other coping strategies[7]. For example, black men with DM reported using coping strategies such as prayer and belief in God, keeping one alive, turning things over to God, changing unhealthy behaviors, supplying their needs, reading the Bible, and religious or spiritual individuals helping them[37].
Religious coping operates in the domains of cognitive, emotional and behavioral responses to stress[45-47]. In this context, cognitive responses are spiritual explanations that aid mental efforts concerning spiritual holdups and imports[48]. Emotional responses involve personal and spiritual experiences of the supernatural. Emotional religious coping may also include collaborating closely with God as a partner and advancing perceived caregiving affiliation with God by building an imaginary bond of divine security[49]. Finally, behavioral responses to stress involve taking action to facilitate the construction of a coherent account of a traumatic event[49,50]. Behavioral religious coping may include praying, reading or reciting religious books, speaking positive religious words over oneself about a health condition, attending a religious gathering, and becoming a part of a faith community. These actions provide the context to make sense of trauma, construct meaning, and facilitate coping in the face of chronic diseases such as DM.
Coping strategies in DM can play a vital role in the maintenance and duration of, and psychosocial adjustment to, this disease[38]. Coping with the reality of being diabetic is a complex and lifelong process. Accepting the reality of the diagnosis and developing a positive attitude toward treatment are critical for successful coping and recovery[51]. Patients may cope by adjusting their social role to fit the demands and challenges associated with the illness, or they may cope by trying to reframe their experiences and view the situation in a more positive light[51].God’s image is linked to religious coping strategies[51,52]. Those with a more positive image of God are more likely to perceive stressors as challenging and beneficial. Similarly, those with a more religious focus perceived less loss and more benefits[52]. Moreover, many African Americans believe that God plays a significant role in DM treatment, and supports individual self-management practices[7,17,32,33]. This religious attitude helps to maintain hope, motivation and coping with the stigma associated with psychological well-being[34,35,45]. Collectively, these studies indicate that religious beliefs are a positive coping strategy for managing and treating DM.
Exploring the potential influence of religious coping strategies on the management of diabetes, we found that most of them showed a positive impact (Table 2). One study examined the role of religious coping in couples’ DM management processes. Fincham et al[43] showed that religious coping and glycemic control activities were integral to type 2 DM (T2DM) management and may serve as valuable points of intervention. Religious coping strategies are a practical approach to maintaining good health and interpersonal care relationships in families with diabetes. Other studies have identified the value of religious coping in patients living with DM and their family caregivers[20,21,53-56].
Table 2.
Results on potential influence of religious coping on people with diabetes
|
Refs
|
Study objectives
|
Method/sample
|
Results
|
| Amadi et al[5] | To assess the association between religiosity and coping style with the outcome of depression and diabetes | 112 participants with diabetes and an equal number with depression consecutively, matching for gender | High intrinsic and extrinsic religiosities are likely to be associated with positive coping skills and better treatment outcome in patients with depression or diabetes |
| Darvyri et al[6] | To evaluate the impact of spirituality/religiosity on T2DM management | PubΜed was searched thoroughly for relevant papers | A positive relationship between religiosity/spirituality and improved T2DM management |
| Saffari et al[9] | To investigate the impact of religiosity on medication adherence and HRQoL | 793 adults (> 65 yr, 45% female) were recruited from four diabetes care centers and followed for one year | Religious coping and social support were recognized as the significant mediators between religiosity and medication adherence |
| Sukarno et al[48] | To explore the meaning of religiousness on diabetes management among T2DM patients | Selecting a concept, determining the analysis purpose, identifying a model case, investigating attributes, antecedents, and consequences, as well as defining empirical referents | Attributes of religiousness have a role in DM care management context, including religious belief, religious practice, religious support, and religious coping |
| Newton et al[50] | To examine the role of specific religious beliefs in the coping process | Sample of 103 parents of children with disabilities | Loss appraisal mediated the relation of vertical focus and God image with engagement coping. The appraisal that God is in control further explained the link between vertical focus and engagement coping |
| Nasirzadeh et al[55] | To evaluate the relationship between religious beliefs and coping strategies in students at Shiraz University | 251 college students were selected by using a stratified random sampling procedure. Carver’s coping strategies questionnaire and Gorsuch's God concept scale were used for data collection | Problem-focused coping strategy correlated positively with the benevolent, Omni-ness, valuable God concept and negatively with the irrelevant, punishing, distinctness God concept |
| Korsah et al[56] | To explore the spiritual coping experiences of patients with diabetes mellitus in a Ghanaian hospital | The hermeneutic phenomenological approach to qualitative research was employed. Data were audio-recorded from both type 1 and 2 diabetes patients through one-on-one interviews | As noted by diabetes patients from their spiritual coping encounters, a disturbing experience was the exploitation and abuse in the form of fasting and over-starving by their spiritual healers in the deception of healing diabetes |
| Choi et al[51] | To explore how religion and spirituality impacted attitudes about self-management practices among African Americans with homelessness histories. To understand resilience in diabetes care practices | Qualitative semi-structured face-to-face interviews were conducted with 42 African Americans > 18 yr | Findings emphasized the importance of spirituality, religious beliefs, and coping strategies in diabetes self-care activities |
| Yazla et al[53] | To investigate the relationship of religious beliefs and forgiveness in diabetic patients with various socio-demographic characteristics, emotional problems, and glycemic control | Comprise 100 patients diagnosed with T2DM. Data collection form, the Scale of Forgiveness and Religiosity, Problem Areas in Diabetes Scale, Beck Depression Inventory, State-Trait Anxiety Inventory and the Audit of Diabetes-Dependent Quality of Life were used | A statistically significant relationship between the scores of the State-Trait Anxiety Inventory and the religious belief scales; forgiveness scale points; and the Beck Depression Inventory |
| How et al[54] | To determine the relationships between religiosity, religions, and glycemic control of T2DM | A cross-sectional study conducted at an urban, university-based, teaching outpatient clinic | Religiosity had a negative correlation with lower FPG but no correlation was found with hemoglobin A1c |
T2DM: Type 2 diabetes mellitus; DM: Diabetes mellitus; HRQoL: Health-related quality of life; FPG: Fasting plasma glucose.
Sukarno and Pamungkas[48] explored whether religiosity was associated with T2DM care management and found that all attributes of religiosity, including religious beliefs, practices, support, and coping, are linked to diabetes care and management (Table 2). This indicates that religious coping strategies influence diabetes care, including self-care and care from the immediate environment, and control how patients respond to medication and accept treatment. Finally, in a systematic literature review, Darvyri et al[6] investigated the roles of spirituality and religiosity in T2DM management. They found a positive relationship between religiosity and spirituality and improved T2DM management. None of the empirical research outcomes reviewed found a negative influence, indicating that religious coping strategies are effective in DM management (Table 2).
PATHWAYS TO THE INFLUENCE OF RELIGIOSITY AND RELIGIOUS COPING STRATEGIES IN THE MANAGEMENT OF DM
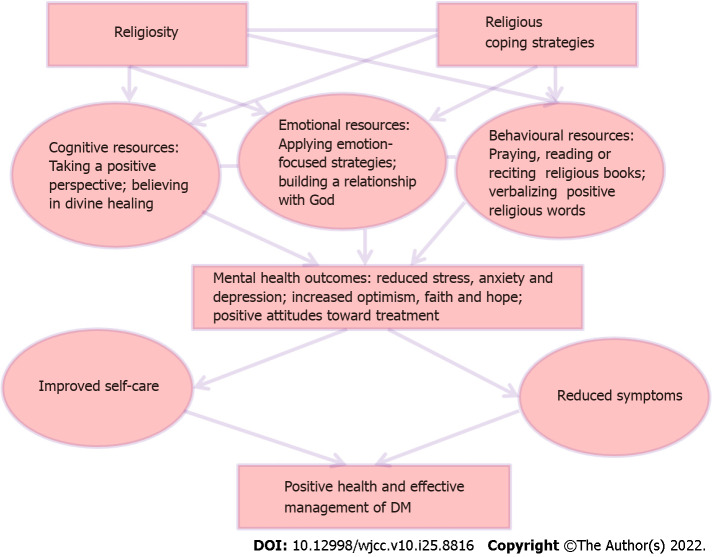
We hypothesize that religiosity and religious coping strategies influence diabetes management and create a pathway of influence. First, DM diagnosis raises tension in patients and their families, which can produce acute stress and anxiety[57]. DM is a chronic condition; therefore, impending stress and anxiety can be confounded through changes in diet and lifestyle, which can significantly affect mental health[26]. Figure 1 shows the potential influence of religiosity and religious coping strategies on DM management. Possible interventions can be anchored to this framework for effective practice (Figure 1).
Figure 1.
Pathway to the potential influences of religiosity and religious coping strategies on people with diabetes. → indicate ‘could result in’. DM: Diabetes mellitus.
Unstable mental health tends to mitigate efforts towards self-care and the management of DM. Patients become more vulnerable if they have a distorted view of lifelong illnesses, such as fear of losing their life, uncertainty about their ability to control or cure the disease, regrets and feelings of guilt, and holding incorrect beliefs about the cause and solution to the problem[58]. Continuing in this devastating state tends to limit patients’ resources, help-seeking behaviors, and their response to medical assistance. Therefore, patients can lose hope in their own efforts and focus on the supernatural, thereby drawing closer to a higher power believed to do all things.
Increasing their routine relationship with God (religiosity) increases their engagement in religious activities, such as church attendance, prayers and reliance on scriptures instead of their condition. This helps bring back hope and confidence that enables the patient to be more optimistic, which positively affects mental health[11,13]. Social support from religious organizations provides a sense of belonging and supports self-care[13] by applying religious coping strategies, such as cognitive, emotional and behavioral approaches, to overcoming the far-reaching impact of DM. Finally, religious beliefs affect patients’ decisions regarding palliative care[59], and religious coping is linked to the quality of life of patients with severe disease[60].
CONS OF RELIGIOSITY IN DM CARE
There are possible and/or known cons of hyper-religiosity and partial noncompliance with medical advice for religious reasons. Studies have demonstrated a significant correlation between religiosity and patient health status[6,61]. Patient beliefs about ill health are vital to the understanding and treatment of illness, and religions have schemes of health beliefs that tend to explain the causes and treatment processes of several illnesses[62]. In the case of chronic illnesses, including diabetes, religiosity is relevant in many ways yet can play an adverse role in the management of such conditions. For instance, current evidence suggests that hyper-religiosity has profound negative effects on the reception of information about diabetic conditions and the willingness to use treatment information[56]. Religious coping beliefs can result in a patient’s refusal of emerging treatment information, which could otherwise reduce fatality. In addition, patients might stick to baseless beliefs that some treatment modalities are against their faith, thereby restricting the use of some functional approaches for managing their health condition.
In addition, beliefs in mystical retribution as causes of illness and the belief that illness is God’s will or punishment and/or is caused by bad omen, evil spirit or witches can limit how patients seek health management information as well as how much they would comply with treatment recommendations[63,64]. In the case of diabetes, which requires patient-oriented and functional approaches, such beliefs may lead to negative health outcomes. Sometimes, the patient may resign to fate, believing that since the sickness came from God or the gods, their own personal efforts are not actually relevant. In cases where the patient sees the illness as a punishment, such patients tend to spend much time and money looking for ways to appease the gods instead of adopting positive management procedures.
Furthermore, within the framework of religious coping, diabetes may be perceived as caused by spirits and treated through mystical activities[64]. In most cases involving mystical healing, patients may be abused differently by the healer. Patients’ conditions could deteriorate and worsen owing to such an unscientific approach[63,64]. For instance, a patient may be asked to fast in prayer camps by a spiritual healer as part of the healing process[64]. Fasting may mean that the patient would not take food or oral medication, which could lead to worsening of the health condition. Additionally, religious coping may include the use of spiritual healing and herbs in addition to fasting and prayers. Other rituals, such as pouring animal blood on the head and feet of patients, are performed for cleansing and healing. Spiritual healers can manipulate patients in diverse ways.
Furthermore, in cases involving religious coping, patients are required to buy expensive materials that they do not have the financial capacity to afford. This may result in delays in treatment and hospital visits and invariably lead patients to develop more complications[61,65]. Past research has also revealed a significant negative relationship between religious beliefs, medication regimen adherence, and negative religious coping experiences[66]. Shahin et al[67] also observed that religious beliefs affected adherence to medication. This suggests that some religious coping practices in patients with diabetes can lead to complications[68]. Thus, even though religious coping has a positive impact on diabetes management, hyper-religiosity can cause enormous harm and should be checked within management modalities. Besides the cons of religiosity and religious coping practices in deconstructing challenges associated with DM care, faith communities have not relented in implementing spiritual care services as part of their religious activities to assist patients cope with diabetes[69,70].
CONCLUSION
Despite reports of adverse effects, religiosity and religious coping strategies could positively influence DM management. Interventions and training based on religious coping strategies could be valuable means of improving self-care attitudes and mental health among patients with DM. Therefore, religious practices and values should be considered part of DM management. Patients’ faith and beliefs should be at the core of DM treatment and management. Further research is required to assess the efficacy of different religion-based interventions in improving DM management. Other studies should investigate patients’ perceptions and lived experiences of the value of religious practices in DM management.
Footnotes
Conflict-of-interest statement: All the authors have no conflict of interest to declare.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: April 13, 2022
First decision: June 27, 2022
Article in press: July 18, 2022
Specialty type: Behavioral sciences
Country/Territory of origin: South Africa
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee KS, South Korea; Munteanu C, Romania S-Editor: Liu JH L-Editor: Kerr C P-Editor: Liu JH
Contributor Information
Charity Neejide Onyishi, Department of Educational Psychology, University of Johannesburg, Johannesburg 2006, Gauteng, South Africa.
Chiedu Eseadi, Department of Educational Psychology, University of Johannesburg, Johannesburg 2006, Gauteng, South Africa. chiedu.eseadi@unn.edu.ng.
Leonard Chidi Ilechukwu, Department of Arts Education, University of Nigeria, Nsukka 41001, Enugu, Nigeria.
Kingsley Nwannennaya Okoro, Department of Philosophy/Religion and Cultural Studies, Alex Ekwueme Federal University, Ndufu-Alike Ikwo 1010, Ebonyi, Nigeria.
Charles Nkem Okolie, Department of Philosophy/Religion and Cultural Studies, Alex Ekwueme Federal University, Ndufu-Alike Ikwo 1010, Ebonyi, Nigeria.
Emmanuel Egbule, Department of Philosophy/Religion and Cultural Studies, Alex Ekwueme Federal University, Ndufu-Alike Ikwo 1010, Ebonyi, Nigeria.
Emmanuel Asogwa, Department of Philosophy/Religion and Cultural Studies, Alex Ekwueme Federal University, Ndufu-Alike Ikwo 1010, Ebonyi, Nigeria.
References
- 1.The International Diabetes Federation. Diabetes facts and figures. 2020. [cited 20 April 2021]. In: The International Diabetes Federation. Available from: https://www.idf.org/aboutdiabetes/what-is-diabetes.html .
- 2.Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. doi: 10.1016/j.diabres.2019.107843. [DOI] [PubMed] [Google Scholar]
- 3.Elgzyri T. Basic Management of Diabetes Mellitus: Practical guidelines. Libyan J Med. 2006;1:176–184. doi: 10.4176/060813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sridhar GR. Diabetes, religion and spirituality. Int J Diabetes DevCtries. 2013;33:5–7. [Google Scholar]
- 5.Amadi KU, Uwakwe R, Odinka PC, Ndukuba AC, Muomah CR, Ohaeri JU. Religion, coping and outcome in out-patients with depression or diabetes mellitus. Acta Psychiatr Scand. 2016;133:489–496. doi: 10.1111/acps.12537. [DOI] [PubMed] [Google Scholar]
- 6.Darvyri P, Christodoulakis S, Galanakis M, Avgoustidis AG, Thanopoulou A, Chrousos GP. On the role of spirituality and religiosity in type 2 diabetes mellitus management—A systematic review. Psychology. 2018;9:728–744. [Google Scholar]
- 7.Kazemi MS. The relationship between religious coping strategies and mental health in MS patient. Procedia Soc Behav Sci. 2010;5:1387–1389. [Google Scholar]
- 8.Cummings JP, Pargament KI. Medicine for the spirit: religious coping in individuals with medical conditions. Religions. 2010;1:28–53. [Google Scholar]
- 9.Saffari M, Lin CY, Chen H, Pakpour AH. The role of religious coping and social support on medication adherence and quality of life among the elderly with type 2 diabetes. Qual Life Res. 2019;28:2183–2193. doi: 10.1007/s11136-019-02183-z. [DOI] [PubMed] [Google Scholar]
- 10.Robinson-Edwards S, Kewley S. Faith-based intervention: prison, prayer, and perseverance. Religions. 2018;9:130. [Google Scholar]
- 11.Kilbourne B, Cummings SM, Levine RS. The influence of religiosity on depression among low-income people with diabetes. Health Soc Work. 2009;34:137–147. doi: 10.1093/hsw/34.2.137. [DOI] [PubMed] [Google Scholar]
- 12.Permana I. How religiosity and/or spirituality might influence self-care in diabetes management: a structured review. Bangladesh J Med Sci. 2018;17:185–193. [Google Scholar]
- 13.Yuniarti KW, Dewi C, Ningrum RP, Widiastuti M, Asril NM. Illness perception, stress, religiosity, depression, social support, and self management of diabetes in Indonesia. Int J Res Stud Psychol. 2013;2:25–41. [Google Scholar]
- 14.Wallston KA, Malcarne VL, Flores L, Hansdottir I, Smith CA, Stein MJ, Clements PJ. Does God determine your health? CognitTher Res. 1999;23:131–142. [Google Scholar]
- 15.James A, Wells A. Religion and mental health: towards a cognitive-behavioural framework. Br J Health Psychol. 2003;8:359–376. doi: 10.1348/135910703322370905. [DOI] [PubMed] [Google Scholar]
- 16.Polzer RL, Miles MS. Spirituality in African Americans with diabetes: self-management through a relationship with God. Qual Health Res. 2007;17:176–188. doi: 10.1177/1049732306297750. [DOI] [PubMed] [Google Scholar]
- 17.Pfeiffer J, Li H, Martez M, Gillespie T. The role of religious behavior in health self-management: A community-based participatory research study. Religions. 2018;9:357. [Google Scholar]
- 18.Watkins YJ, Quinn LT, Ruggiero L, Quinn MT, Choi YK. Spiritual and religious beliefs and practices and social support's relationship to diabetes self-care activities in African Americans. Diabetes Educ. 2013;39:231–239. doi: 10.1177/0145721713475843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levin SL, Katz AH, Holst E. Self-care. Lay initiatives in health. London: Croom Helm, 1977. [Google Scholar]
- 20.Bai YL, Chiou CP, Chang YY. Self-care behaviour and related factors in older people with Type 2 diabetes. J Clin Nurs. 2009;18:3308–3315. doi: 10.1111/j.1365-2702.2009.02992.x. [DOI] [PubMed] [Google Scholar]
- 21.Swihart DL, Yarrarapu SNS, Martin RL. Cultural Religious Competence In Clinical Practice. 2021 Nov 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 22.Pirutinsky S, Rosmarin DH, Holt CL. Religious coping moderates the relationship between emotional functioning and obesity. Health Psychol. 2012;31:394–397. doi: 10.1037/a0026665. [DOI] [PubMed] [Google Scholar]
- 23.Pang H. Examining associations between university students' mobile social media use, online self-presentation, social support and sense of belonging. Aslib J Inf Manag . 2020;72:321–338. [Google Scholar]
- 24.Ghavi F, Hejazi F, Jahromi MK, Poorgholami F. Effect of spiritual therapy training on multiple sclerosis patients' hope. Int Med J. 2021;28:232–235. [Google Scholar]
- 25.Helm HM, Hays JC, Flint EP, Koenig HG, Blazer DG. Does private religious activity prolong survival? J Gerontol A Biol Sci Med Sci. 2000;55:M400–M405. doi: 10.1093/gerona/55.7.m400. [DOI] [PubMed] [Google Scholar]
- 26.Lukman NA, Leibing A, Merry L. Self-Care Experiences of Adults with Chronic Disease in Indonesia: An Integrative Review. Int J Chronic Dis. 2020;2020:1379547. doi: 10.1155/2020/1379547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maselko J, Hayward RD, Hanlon A, Buka S, Meador K. Religious service attendance and major depression: a case of reverse causality? Am J Epidemiol. 2012;175:576–583. doi: 10.1093/aje/kwr349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weber SR, Pargament KI. The role of religion and spirituality in mental health. Curr Opin Psychiatry. 2014;27:358–363. doi: 10.1097/YCO.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 29.Lorenz L, Doherty A, Casey P. The Role of Religion in Buffering the Impact of Stressful Life Events on Depressive Symptoms in Patients with Depressive Episodes or Adjustment Disorder. Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16071238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Banerjee AT, Boyle MH, Anand SS, Strachan PH, Oremus M. The relationship between religious service attendance and coronary heart disease and related risk factors in Saskatchewan, Canada. J Relig Health. 2014;53:141–156. doi: 10.1007/s10943-012-9609-6. [DOI] [PubMed] [Google Scholar]
- 31.Hekler EB, Lambert J, Leventhal E, Leventhal H, Jahn E, Contrada RJ. Commonsense illness beliefs, adherence behaviors, and hypertension control among African Americans. J Behav Med. 2008;31:391–400. doi: 10.1007/s10865-008-9165-4. [DOI] [PubMed] [Google Scholar]
- 32.Berardi V, Bellettiere J, Nativ O, Ladislav S, Hovell MF, Baron-Epel O. Fatalism, Diabetes Management Outcomes, and the Role of Religiosity. J Relig Health. 2016;55:602–617. doi: 10.1007/s10943-015-0067-9. [DOI] [PubMed] [Google Scholar]
- 33.Sohail MM, Mahmood QK, Sher F, Saud M, Mas'udah S, Ida R. Coping Through Religiosity, Spirituality and Social Support Among Muslim Chronic Hepatitis Patients. J Relig Health. 2020;59:3126–3140. doi: 10.1007/s10943-019-00909-4. [DOI] [PubMed] [Google Scholar]
- 34.Holt CL, Roth DL, Huang J, Clark EM. Role of religious social support in longitudinal relationships between religiosity and health-related outcomes in African Americans. J Behav Med. 2018;41:62–73. doi: 10.1007/s10865-017-9877-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rivera-Hernandez M. Religiosity, Social Support and Care Associated with Health in Older Mexicans with Diabetes. J Relig Health. 2016;55:1394–1410. doi: 10.1007/s10943-015-0105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nyarko K, Kugbey N, Atindanbila S. Illness perception, religiosity and mental health of diabetic patients in Ghana. Am J Appl Psychol. 2014;3:12–20. [Google Scholar]
- 37.Namageyo-Funa A, Muilenburg J, Wilson M. The role of religion and spirituality in coping with type 2 diabetes: a qualitative study among Black men. J Relig Health. 2015;54:242–252. doi: 10.1007/s10943-013-9812-0. [DOI] [PubMed] [Google Scholar]
- 38.Tuncay T, Musabak I, Gok DE, Kutlu M. The relationship between anxiety, coping strategies and characteristics of patients with diabetes. Health Qual Life Outcomes. 2008;6:79. doi: 10.1186/1477-7525-6-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blakely AA, Howard RC, Sosich RM, Murdoch JC, Menkes DB, Spears GF. Psychiatric symptoms, personality and ways of coping in chronic fatigue syndrome. Psychol Med. 1991;21:347–362. doi: 10.1017/s0033291700020456. [DOI] [PubMed] [Google Scholar]
- 40.Folkman S. Stress: Appraisal and Coping. In: Gellman MD, Turner JR. Encyclopedia of Behavioral Medicine. New York, NY: Springer, 2013. [Google Scholar]
- 41.Szcześniak M, Kroplewski Z, Szałachowski R. The mediating effect of coping strategies on religious/spiritual struggles and life satisfaction. Religions. 2020;11:195. [Google Scholar]
- 42.Aflakseir A, Mahdiyar M. The Role of Religious Coping Strategies in Predicting Depression among a Sample of Women with Fertility Problems in Shiraz. J Reprod Infertil. 2016;17:117–122. [PMC free article] [PubMed] [Google Scholar]
- 43.Fincham FD, Seibert GS, May RW, Wilson CM, Lister ZD. Religious Coping and Glycemic Control in Couples with Type 2 Diabetes. J Marital Fam Ther. 2018;44:138–149. doi: 10.1111/jmft.12241. [DOI] [PubMed] [Google Scholar]
- 44.King M, Marston L, McManus S, Brugha T, Meltzer H, Bebbington P. Religion, spirituality and mental health: results from a national study of English households. Br J Psychiatry. 2013;202:68–73. doi: 10.1192/bjp.bp.112.112003. [DOI] [PubMed] [Google Scholar]
- 45.Koenig HG. The Connection between psychoneuroimmunology and religion. In: Koenig HG, Cohen HJ. The link between religion and health: Psychoneuroimmunology and the faith factor. New York: Oxford University Press, 2002. [Google Scholar]
- 46.Celik S, Taskin Yilmaz F, Anataca G. The Effect of Religious Coping on Disease Acceptance and Management Among Patients with Diabetes in Turkey. J Relig Health. 2022;61:1980–1993. doi: 10.1007/s10943-021-01260-3. [DOI] [PubMed] [Google Scholar]
- 47.Pargament K, Feuille M, Burdzy D. The Brief RCOPE: Current psychometric status of a short measure of religious coping. Religions. 2011;2:51–76. [Google Scholar]
- 48.Sukarno A, Pamungkas RA. Religiousness associated with type 2 diabetes care management: a concept analysis. nt J Nurs Health Serv. 2020;3:462–470. [Google Scholar]
- 49.Muldoon OT, Haslam SA, Haslam C, Cruwys T, Kearns M, Jetten J. The social psychology of responses to trauma: Social identity pathways associated with divergent traumatic responses. Eur Rev Soc Psychol. 2019;30:311–348. [Google Scholar]
- 50.Newton AT, McIntosh DN. Specific religious beliefs in a cognitive appraisal model of stress and coping. Int J Psychol Relig. 20:39–58. [Google Scholar]
- 51.Choi SA, Hastings JF. Religion, spirituality, coping, and resilience among African Americans with diabetes. J Relig Spiritual Soc Work. 2019;38:93–114. doi: 10.1080/15426432.2018.1524735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Snodgrass JL. Spirituality and Homelessness: Implications for pastoral counseling. Pastoral Psychol. 2014;63:307–317. [Google Scholar]
- 53.Yazla E, Karadere ME, Küçükler FK, Karşıdağ Ç, İnanç L, Kankoç E, Dönertaş M, Demir E. The Effect of Religious Belief and Forgiveness on Coping with Diabetes. J Relig Health. 2018;57:1010–1019. doi: 10.1007/s10943-017-0504-z. [DOI] [PubMed] [Google Scholar]
- 54.How CB, Ming KE, Chin CY. Does religious affiliation influence glycaemic control in primary care patients with type 2 diabetes mellitus? Ment Health Fam Med. 2011;8:21–28. [PMC free article] [PubMed] [Google Scholar]
- 55.Nasirzadeh R, Rasoulzadeh TS. Religious beliefs and coping strategies in students. Ofogh-E-Danesh. 2009;15:36–45. [Google Scholar]
- 56.Korsah KA, Domfeh KA. Research Topic: The realities of religious coping experiences of patients with diabetes mellitus: Implications for policy formulation in Ghana. Int J Afri Nurs Sci. 2020;13:100245. [Google Scholar]
- 57.Wong H, Singh J, Go RM, Ahluwalia N, Guerrero-Go MA. The Effects of Mental Stress on Non-insulin-dependent Diabetes: Determining the Relationship Between Catecholamine and Adrenergic Signals from Stress, Anxiety, and Depression on the Physiological Changes in the Pancreatic Hormone Secretion. Cureus. 2019;11:e5474. doi: 10.7759/cureus.5474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bickett A, Tapp H. Anxiety and diabetes: Innovative approaches to management in primary care. Exp Biol Med (Maywood) 2016;241:1724–1731. doi: 10.1177/1535370216657613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rego F, Gonçalves F, Moutinho S, Castro L, Nunes R. The influence of spirituality on decision-making in palliative care outpatients: a cross-sectional study. BMC Palliat Care. 2020;19:22. doi: 10.1186/s12904-020-0525-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tarakeshwar N, Vanderwerker LC, Paulk E, Pearce MJ, Kasl SV, Prigerson HG. Religious coping is associated with the quality of life of patients with advanced cancer. J Palliat Med. 2006;9:646–657. doi: 10.1089/jpm.2006.9.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vitorino LM, Lucchetti G, Leão FC, Vallada H, Peres MFP. The association between spirituality and religiousness and mental health. Sci Rep. 2018;8:17233. doi: 10.1038/s41598-018-35380-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Adejumo H, Odusan O, Sogbein O, Laiteerapong N, Dauda M, Ahmed O. The impact of religion and culture on diabetes care in Nigeria. African J Diabetes Med. 2015;23:17–19. [Google Scholar]
- 63.Asare M, Danquah S. The African belief system and the patient’s choice of treatment from existing health models-the case of Ghana. Acta Psychopathol. 2017;3:1–4. [Google Scholar]
- 64.Venkatraju B, Prasad S. Beliefs of patients about the causes of Tuberculosis in rural Andhra Pradesh. Int J Nurs Midwifery. 2010;2:21–27. [Google Scholar]
- 65.Brundisini F, Vanstone M, Hulan D, DeJean D, Giacomini M. Type 2 diabetes patients' and providers' differing perspectives on medication nonadherence: a qualitative meta-synthesis. BMC Health Serv Res. 2015;15:516. doi: 10.1186/s12913-015-1174-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Movahedizadeh M, Sheikhi MR, Shahsavari S, Chen H. The association between religious belief and drug adherence mediated by religious coping in patients with mental disorders. Soc Health Behav. 2019;2:77–82. [Google Scholar]
- 67.Shahin W, Kennedy GA, Stupans I. The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: a systematic review. Patient Prefer Adherence. 2019;13:1019–1035. doi: 10.2147/PPA.S212046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Amadi KU, Aguocha CM, Attama MC, Onu JU, Odinka PC, Nduanya CU, Muomah RC, Ndukuba AC. Religiosity and treatment adherence among out-patients with schizophrenia. Ment Health Relig Cult. 2021;14:1. [Google Scholar]
- 69.Kelley S. The Role of the Faith Community Nurse in Weight Management. J Christ Nurs. 2018;35:53–59. doi: 10.1097/CNJ.0000000000000449. [DOI] [PubMed] [Google Scholar]
- 70.Subrata SA. Implementation of spiritual care in patients with diabetic foot ulcers: a literature review. Br J Nurs. 2020;29:S24–S32. doi: 10.12968/bjon.2020.29.15.S24. [DOI] [PubMed] [Google Scholar]