Abstract
Background
Depression is a prominent cause of mental disability globally, having a severe impact on mental and physical health. Depression rehabilitation and treatment, whether through psychiatric management or counseling therapy, is hampered by stigmatizing attitudes regarding psychiatric illness patients impacted by societal and cultural factors. However, little is known about the stigma toward people with depression among the students in Syria.
Methodology
A total of 1,056 students in Syria completed a questionnaire that included a case narrative illustrating depression. A total of 1,056 students in Syria completed a questionnaire that included a case narrative illustrating depression. The survey looked at attitudes toward depression, the desire to keep a safe distance from depressed people, stigma attitudes toward people with depression among college students, perceived beliefs about depressive people, gender (male and female), and the major section (medical and medical and non-medical) differences.
Results
Four questionnaires have refused to finish the survey, out of 1259 issued. Around 47.80% of respondents, most of whom were females, felt that sad people might snap out of it. 14.60 percent believe depression isn’t even an actual medical condition. Surprisingly, 2% of respondents with a medical background thought the same thing. Regarding more extreme stigmatization, 16.80% of respondents thought depressed persons were harmful. People with depression will be avoided by 19.50 percent of respondents, and people with medical backgrounds will be avoided by 5.20 percent of respondents. Nearly one-fifth of those polled said they would not tell anyone if they were depressed. Only a tiny percentage of respondents (6.90 percent) said they would not hire or vote for a politician who suffers from depression (8.40 percent).
Conclusion
According to the study, Syrian college students had a significant level of stigma and social distance toward mentally ill patients. Female students and non-medical students had a higher stigma in most subscale items for people with depression.
Introduction
Most people define "Depression" as a feeling of loss or being sad; however, it is more than that. Depression is a severe psychiatric condition that is highly prevalent worldwide [1]. WHO has ranked Major Depressive Disorders (M.D.D.) as the third cause of the burden of disease worldwide in 2008, and it is expected that it will be ranked first by 2030 [2]. About 350 million people of all ages worldwide are affected by depression [3]. The prevalence of Depression has risen recently, especially in children and adolescents, as shown by the U.S. national comorbidity survey, which found that between 2001 to 2004, about 11.7% of adolescents aged 13 to 18 years have met the criteria for major depressive disorder. Also, the 12-month prevalence of major depressive episodes has increased from 8.7% in 2005 to 11.3% in 2014 in adolescents and from 8.8% to 9.6% in young adults [4]. Researchers have also shown higher rates of Depression among university students compared to the general population [5, 6]; a Chinese study shows that about 23.8% of university students are affected by depression [7].
Although the exact cause of Depression is still unknown, studies show that the etiology of Depression is multifactorial, including Biological and environmental factors and psychological factors. Biological factors include genetic elements as the heritability of Depression is estimated to be approximately 35%, and hormones or abnormalities in neurotransmitters such as dopamine and norepinephrine are also involved in the etiology of M.D.D. Environmental factors include environmental stressors, sexual, physical, or emotional abuse during childhood, associated with the high risk of developing M.D.D. [2, 8]. Diagnosis of M.D.D. It depends on D.S.M.’s 5 diagnostic criteria, which require the presence of 5 of 9 symptoms for 2 weeks, provided that one of these symptoms must be the depressed mode or anhedonia [9]. Depression is associated with a high mortality rate and shorter life expectancy [10, 11]; an increased risk of suicide can explain this among affected people [12, 13], and a bad prognosis of other medical conditions lead to an increased risk of developing complication and high risk of Mortality [14]. Depression has chronic nature and requires lifelong treatment to diminish relapse and recurrence rates [15]. However, people affected by Depression suffer from stigmatizing beliefs [16] which may be considered a barrier to recovery.
Stigma means that people would distinguish one negatively, a pejorative attribute implying shame. When related to mental illness, it generates fear of being excluded or rejected by others due to false beliefs arising from a lack of knowledge about the nature of mental illness [17, 18]. Mentally ill people such as those affected by depression fight in two ways first, they fight against their disease and its symptoms affecting their lives; second, they fight against the general public stigmatizing attitudes against them, pushing them to be set apart from the others, causing them to feel lonely and aggravate their condition. Stigma is classified into public and self-stigma; public stigma is the attitude of the general population toward people with mental illness. In contrast, self-stigma is the internalized sensation of shame that those people have about themselves [19]. It has been reported that stigmatization of mental illness, including depressive disorders, is still highly prevalent [20]. Most mentally ill people express negative attitudes against them from others, such as (avoidance, forcing them for treatment, setting them isolated from the others, hostile behavior). This is almost because the general public considers them dangerous and responsible for their behavior (controllability and responsibility) [21]. Harmful consequences of stigmatized attitudes have been reported by WHO, including destroyed family relationships and social exclusion [22] As stigma against mental illness is highly prevalent [23], depressed people, like other mentally ill patients, suffer from stigmatizing and discriminative attitudes against them, making them embarrassed about seeking help leading to more deterioration in their condition which may affect their daily life, they prefer not to ask for help as they think that the others will distinguish them negatively if they sought such help [24, 25]. A Canadian study reported that people with mental illness using health services suffer from stigmatizing attitudes [26]. A study held in the School of Medicine at the University of California, San Francisco, showed that only 22% of students suffering from Depression were ready to receive counseling services, while others were not [27]. Studies show a high prevalence of perceived stigma of Depression among students [28], as demonstrated by Chinese research that reported high levels of stigmatizing attitudes towards Depression are prevalent among the Chinese public, with about 53.0% of participants reporting personal stigma and 83.4% reported perceived stigma [29], In addition, medical students show a high prevalence of stigma against depression [30]. To face stigma and discrimination, Anti-stigma initiatives have been set up to reduce their harmful effects on patients and improve the social understanding of mental illness [31].
By checking the literature, we found no similar studies in Syria that assess the stigma among the population toward mental health patients. However, some studies have followed post-traumatic self-stigmitizing Syrians in asylum countries [32, 33]. Similar studies have taken part in Arab countries like Saudi, Lebanon, and Oman [34–36]. Also, there is a considerable gap related to suitable and supported management of mental illnesses patients by citizens in Arab countries, especially low-income countries such as Syria.
Our goal was to establish the frequency of public stigma against Depression in a sample of Syrian students, including personal and perceived stigma and the explanations behind these stigmata. We hypothesized that, given the high prevalence of stigma attitudes toward Depression, stigma attitudes toward Depression are prevalent among Syrian students, so we conducted this study to determine: 1) whether stigma is prevalent among Syrian students and 2) the degree of stigmatizing attitudes and social distancing among them. The fighting stigma connected with Depression is a vital method of enhancing mental and physical health and offering those suffering in silence a voice. To make all communities and community members safer and healthier, stigma must be eliminated. So we recommend paying attention to the disastrous effect of stigma on depressed individuals and the importance of developing anti-stigma programs in health facilities with more future investment in health facility stigma reduction.
Methods
Study design
We conducted an online cross-sectional to collect data from Syrian university students using an online questionnaire based on similar research [37] in the literature. We modified the survey and translated it into the Arabic language in a suitable form for Syrian students. The used questionnaire was uploaded in S1 Table.
Setting and participants
1259 Syrian students from different universities took part in this survey and filled out a Google Form website questionnaire. The data collection duration lasted from 18th to 27th March 2021. Only the Syrian students above 18 years were eligible to participate in the study.
To acquire the requisite responders, convenience and snowball strategies were used. The online questionnaire was shared on social media groups such as WhatsApp, Facebook, and telegram by collaborators to gather the responses. We didn’t perform a statistical power analysis to calculate the required sample size because there are no accurate reports of the number of Syrian students. Twenty-five random responses were gathered to study if the questionnaire was suitable and easy to understand and answer or not, and we conducted some modifications depending on the participants’ comments.
We also conducted a pilot analysis involving 40 responses to check that the questionnaire’s reliability was validated. The Cronbach’s alpha values range from 0.712 to 0.861, demonstrating that the used tool had a high internal consistency level. We published the questionnaire once the pilot study was finished.
Measurements in the survey questionnaires
The questionnaires consisted of seven parts: the first part was a range of questions about demographic data like age, gender and social status, the second part was questions about personal stigma toward depression scale, the third part includes questions about perceived stigma towards depression scale, the fourth part was closed-ended questions about social distance with depressed people with Yes or No answers, the fifth part consists of questions about the participants’ usual source of their knowledge about depression like newspapers, TV or websites, the sixth part is concerned by helpfulness or intervention, this part is subdivided into four subgroups of question with multiple answer, these subgroups are People who can help, Medications which can help, other interventions and help methods, the last part is concerned by supporting information, it includes three cases participants should answer in order to give confirmation about their knowledge towards 3 mental health disorders (Depression, schizophrenia and anxiety). The used questionniare was uploaded as a suplemanteray material.
Depression Stigma Scales
The DSS contains personal stigma subscales (nine items) and perceived stigma subscales (nine items). The statements in each item of the two subscales are the same except for the subject of items. In the personal stigma subscales, respondents were asked about their attitude toward people with depression symptoms described in the vignette (e.g., “People with depression could snap out of it if they wanted”). In the perceived stigma subscales, respondents were asked their beliefs about most of the other people’s attitudes toward people with depression symptoms described in the vignette (e.g., “Most people believe that people with depression could snap out of it if they wanted”). The response of each item was measured on a five-point scale ranging from “strongly agree” to “strongly disagree” [32]. The Chinese version of the scale has been widely used with good reliability and validity [38].
There are two sections in the questionnaire that explain the Participants’ usual sources of mental health knowledge, especially depression, and the recommended opinions towards supporting interventions for helping depressed persons.
In addition, this questionnaire includes a vignette of 3 patients with mental illnesses (depression, schizophrenia, and GAD) to assess the students’ knowledge of the diagnosis of these psychiatric disorders.
Social distance scale
The five-item short measurement of SDS was developed by [39] to measure the desire for social distancing from a person with mental illness. The Chinese version of the SDS was used to estimate the willingness to come into contact (such as live next door, marry into the family) with the person described in the vignette. The response of each item was measured on a four-point scale, which ranged from “definitely willing” to “definitely unwilling.” The reliability and validity of its Chinese version have been tested, and the results showed that all the indicators met the requirements of psychometrics.
The used questionnaire was uploaded as suplementrail file.
Ethics statement
The protocol was approved by the dean of Damascus University and Aleppo University in March 2021. The convenience sampling method was used in the present study. Considering the sample’s representativeness, this study randomly selected different classes by the school, grade, and significance. The aim of the present study was explained in the questionnaires, and oral informed consent was obtained from all the respondents. They were encouraged to independently analyze the vignette and answer a battery of questions, including demographic information, depression stigma scales (DSS), and social distance scale SDS. The survey contained a cover page stating responses were anonymous and voluntary and would have no impact on the participants.
Statistical analysis
All data were analyzed by SPSS 28 and Excel. Descriptive statistics, including demographic characteristics, Participants’ usual sources of mental health knowledge, and helpful interventions, were presented as numbers and percentages. Still, continuous variables were presented as mean and standard deviation. Stigma attitudes toward people with depression (percentage frequencies and 95% CI) and social distance (percentage frequencies and 95% CI). The options of “agree” and “strongly agree” were combined into one option on the DSS, and the possibilities of “Yes” and “No” were combined into one option on the SDS. The integrated options represent the positive and negative attitudes of the respondents. Sperman and one-way ANOVA test were used to assess the significant difference in each item on the three scales that assess stigma towards depression patients and social distance scale among different demographic variables (gender, major, educational level, and school level) in the proportion of agreement. Multiple logistic regression was conducted to study the predicted relationship between the three scales and other demographic variables. We considered the response with half of the total score or under equal 0 value, but the answer with above half of the total score equals 1vaule. The value of p was set at <0.05 for statistical significance.
Results
Demographic baseline characteristics of the study sample
Out of 1259 distributed questionnaires, four questionnaires have refused to complete the survey. The baseline characteristics of the participants are shown in Table 1. The average age of the respondents was 22.4± 3.85 (mean ± SD). The ratio of gender (male 26%: female 74%) was approximately 1:3, which may be attributed to the already imbalanced gender ratio in Syrian schools. To explore the difference in stigmatizing attitudes between medical and non-medical students, we have classified students’ majors into medical majors (34.8%) and non-medical majors (65.2%). About 43.1% of students were working during their educational lives. More than half of respondents (58.2%) have reported a positive history of mental health disease, but only (7%) are under psychological treatment.
Table 1. Baseline characteristics of the participants.
| N = 1259 | ||
|---|---|---|
| n | % | |
| Age (Mean/SD) | 22.4/3.85 | |
| Gender | ||
| Male | 327 | 26.0% |
| Female | 932 | 74.0% |
| Social status | ||
| Single | 1095 | 87.0% |
| Married | 125 | 9.9% |
| Divorced | 23 | 1.8% |
| Widower | 16 | 1.3% |
| Major section | ||
| Medical student | 438 | 34.8% |
| Non-medical student | 821 | 65.2% |
| Economic level | ||
| Bad | 105 | 8.3% |
| Middle | 748 | 59.4% |
| Good | 363 | 28.8% |
| High | 43 | 3.4% |
| The University stage | ||
| 1ST year | 229 | 18.2% |
| 2nd year | 216 | 17.2% |
| 3rd year | 204 | 16.2% |
| 4th year | 262 | 20.8% |
| 5th year | 186 | 14.8% |
| 6th year | 162 | 12.9% |
| Region | ||
| City | 890 | 70.7% |
| Rural | 369 | 29.3% |
| Occupation status | ||
| Worker | 542 | 43.1% |
| Non-Worker | 717 | 56.9% |
| Live with | ||
| Family | 1051 | 83.5% |
| With father | 27 | 2.1% |
| With mother | 103 | 8.2% |
| With friends | 78 | 6.2% |
| Immigrant status | ||
| Yes | 560 | 44.5% |
| No | 699 | 55.5% |
| History of Mental Health Disease | ||
| Yes | 733 | 58.2% |
| No | 526 | 41.8% |
| Current psychological treatment | ||
| Yes | 88 | 7.0% |
| No | 1171 | 93.0% |
| Current pharmacological treatment | ||
| Yes | 174 | 7.0% |
| No | 1085 | 93.0% |
Personal stigma
In Table 2, we collected the gender differences and medical and non-medical significant differences in the percentage of participants who held stigma attitudes toward the person with depression. About 47.80% of respondents agreed that depressed people could snap out of the problem; most were females. 14.60% stated that depression is not even an actual medical illness. Surprisingly enough, 2% of medical background respondents thought that as well. As for more extreme stigmatization, 16.80% of respondents considered depressed people as dangerous people. 19.50% will tend to avoid people with depression, and 5.20% of medical background respondents will also prevent these people. Approximately 18.80% of respondents won’t tell anyone if they suffer from depression. Only a small portion of respondents won’t hire anyone with depression (6.90%) or elect a politician suffering from depression (8.40).
Table 2. Percentage of participants who “agree” or “strongly agree” with about personal stigma towards depression patient scale statements.
| Statement about personal belief | Total (N = 935) | Gender | Major section | Region | Economic level | Occupation status | ||||||||||||||||||||
| n | Male (n = 327) | Female (n = 932) | Medical (n = 438) | Non-Medical (n = 821) | City (n = 890) | Rural region (n = 369) | Low (n = 105) | Moderate (n = 748) | Good (n = 363) | High (n = 43) | Worker (n = 542) | Non-worker (n = 717) | ||||||||||||||
| % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||
| The person could snap out of the problem | 602 | 47.80% | 115 | 9.20% | 477 | 38.2%** | 179 | 14.30% | 413 | 33.1%** | 421 | 33.70% | 171 | 13.70% | 37 | 3.00% | 370 | 29.60% | 171 | 13.70% | 14 | 1.1%* | 247 | 19.80% | 345 | 27.60% |
| Problem is a sign of personal weakness | 149 | 11.80% | 48 | 3.90% | 86 | 6.9%* | 30 | 8.40% | 104 | 2.4%** | 80 | 6.40% | 54 | 4.3%* | 17 | 8.40% | 77 | 6.20% | 35 | 2.80% | 5 | 0.40% | 62 | 5.00% | 72 | 5.85 |
| Problem is not a real medical illness | 184 | 14.60% | 55 | 4.40% | 111 | 8.9%* | 25 | 2.00% | 141 | 11.4%** | 101 | 8.10% | 65 | 5.2%* | 22 | 1.80% | 107 | 8.60% | 34 | 2.70% | 3 | 0.2%* | 72 | 7.60% | 94 | 5.80% |
| People with this problem are dangerous | 211 | 16.80% | 57 | 4.60% | 154 | 12.40% | 74 | 5.90% | 137 | 11.00% | 148 | 11.90% | 63 | 5.10% | 19 | 1.50% | 130 | 10.50% | 53 | 4.30% | 9 | 0.70% | 97 | 9.20% | 114 | 7.80% |
| Avoid people with this problem | 245 | 19.50% | 56 | 4.50% | 189 | 15.20% | 65 | 5.20% | 180 | 14.5%** | 179 | 14.40% | 66 | 5.30% | 24 | 1.90% | 139 | 11.20% | 76 | 6.10% | 6 | 0.50% | 120 | 9.70% | 125 | 10.15 |
| People with this problem are unpredictable | 399 | 31.70% | 91 | 7.40% | 308 | 25%* | 127 | 10.30% | 272 | 22.10% | 287 | 23.30% | 112 | 9.10% | 37 | 3.00% | 241 | 19.50% | 115 | 9.30% | 6 | 0.5%* | 157 | 12.70% | 242 | 19.6%* |
| If I had this problem, I would not tell anyone | 237 | 18.80% | 71 | 5.70% | 166 | 13.40% | 63 | 5.10% | 174 | 14%** | 171 | 13.80% | 66 | 5.30% | 24 | 1.90% | 142 | 11.40% | 59 | 4.80% | 12 | 1.00% | 98 | 11.20% | 139 | 7.90% |
| I would not employ someone with this problem | 87 | 6.90% | 27 | 2.20% | 60 | 4.80% | 24 | 1.90% | 63 | 5.10% | 65 | 5.20% | 22 | 1.80% | 15 | 1.20% | 47 | 3.80% | 19 | 1.50% | 6 | 0.5%* | 42 | 3.40% | 48 | 3.60% |
| I would not vote for a politician with this problem | 106 | 8.40% | 33 | 2.70% | 73 | 5.90% | 38 | 3.10% | 68 | 5.5%** | 75 | 6.00% | 31 | 2.50% | 9 | 0.70% | 58 | 4.70% | 32 | 2.60% | 7 | 0.60% | 53 | 4.30% | 53 | 4.30% |
| DPSS total score (mean ± SD) | 1.74 | 1.4 | 1.6 | 1.4 | 1.7 | 1.4 | 1.4 | 1.2 | 1.8 | 1.5 | 1.7 | 1.4 | 1.7 | 1.4 | 1.9 | 1.5 | 1.7 | 1.4 | 1.6 | 1.3 | 1.6 | 1.7 | 1.7 | 1.4 | 1.7 | 1.4 |
| Statement about personal belief | Total (N = 935) | Gender | Major section | Region | Economic level | Occupation status | ||||||||||||||||||||
| n | Male (n = 327) | Female (n = 932) | Medical (n = 438) | Non-Medical (n = 821) | City (n = 890) | Rural region (n = 369) | Low (n = 105) | Moderate (n = 748) | Good (n = 363) | High (n = 43) | Worker (n = 542) | Non-Worker (n = 717) | ||||||||||||||
| % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||
| The person could snap out of the problem | 602 | 47.80% | 115 | 9.20% | 477 | 38.2%** | 179 | 14.30% | 413 | 33.1%** | 421 | 33.70% | 171 | 13.70% | 37 | 3.00% | 370 | 29.60% | 171 | 13.70% | 14 | 1.1%* | 247 | 19.80% | 345 | 27.60% |
| Problem is a sign of personal weakness | 149 | 11.80% | 48 | 3.90% | 86 | 6.9%* | 30 | 8.40% | 104 | 2.4%** | 80 | 6.40% | 54 | 4.3%* | 17 | 8.40% | 77 | 6.20% | 35 | 2.80% | 5 | 0.40% | 62 | 5.00% | 72 | 5.85 |
| Problem is not a real medical illness | 184 | 14.60% | 55 | 4.40% | 111 | 8.9%* | 25 | 2.00% | 141 | 11.4%** | 101 | 8.10% | 65 | 5.2%* | 22 | 1.80% | 107 | 8.60% | 34 | 2.70% | 3 | 0.2%* | 72 | 7.60% | 94 | 5.80% |
| People with this problem are dangerous | 211 | 16.80% | 57 | 4.60% | 154 | 12.40% | 74 | 5.90% | 137 | 11.00% | 148 | 11.90% | 63 | 5.10% | 19 | 1.50% | 130 | 10.50% | 53 | 4.30% | 9 | 0.70% | 97 | 9.20% | 114 | 7.80% |
| Avoid people with this problem | 245 | 19.50% | 56 | 4.50% | 189 | 15.20% | 65 | 5.20% | 180 | 14.5%** | 179 | 14.40% | 66 | 5.30% | 24 | 1.90% | 139 | 11.20% | 76 | 6.10% | 6 | 0.50% | 120 | 9.70% | 125 | 10.15 |
| People with this problem are unpredictable | 399 | 31.70% | 91 | 7.40% | 308 | 25%* | 127 | 10.30% | 272 | 22.10% | 287 | 23.30% | 112 | 9.10% | 37 | 3.00% | 241 | 19.50% | 115 | 9.30% | 6 | 0.5%* | 157 | 12.70% | 242 | 19.6%* |
| If I had this problem, I would not tell anyone | 237 | 18.80% | 71 | 5.70% | 166 | 13.40% | 63 | 5.10% | 174 | 14%** | 171 | 13.80% | 66 | 5.30% | 24 | 1.90% | 142 | 11.40% | 59 | 4.80% | 12 | 1.00% | 98 | 11.20% | 139 | 7.90% |
| I would not employ someone with this problem | 87 | 6.90% | 27 | 2.20% | 60 | 4.80% | 24 | 1.90% | 63 | 5.10% | 65 | 5.20% | 22 | 1.80% | 15 | 1.20% | 47 | 3.80% | 19 | 1.50% | 6 | 0.5%* | 42 | 3.40% | 48 | 3.60% |
| I would not vote for a politician with this problem | 106 | 8.40% | 33 | 2.70% | 73 | 5.90% | 38 | 3.10% | 68 | 5.5%** | 75 | 6.00% | 31 | 2.50% | 9 | 0.70% | 58 | 4.70% | 32 | 2.60% | 7 | 0.60% | 53 | 4.30% | 53 | 4.30% |
| DPSS total score (mean ± SD) | 1.74 | 1.4 | 1.6 | 1.4 | 1.7 | 1.4 | 1.4 | 1.2 | 1.8 | 1.5 | 1.7 | 1.4 | 1.7 | 1.4 | 1.9 | 1.5 | 1.7 | 1.4 | 1.6 | 1.3 | 1.6 | 1.7 | 1.7 | 1.4 | 1.7 | 1.4 |
Perceived stigma
Participants’ agreements about the items reflecting other people’s beliefs are shown in Table 3. Half of the respondents were most likely to agree that most other people would think that people with depression can snap out of it if they wanted to. When comparing perceived stigma (Table 3) to personal stigma questionnaires (Table 2), About 37.80% of respondents thought that other people consider depression a sign of weakness. In contrast, only 11.80% believed so when expressing their personal belief in this regard. A quarter of non-medical respondents thought most people would not treat depression as a medical illness, and 17.7% believed that most people would consider depressed people dangerous. 38.60% of respondents estimated that most people would find it best for themselves to avoid depressed people in order not to be depressed. In addition, 31.90% thought that most people wouldn’t employ or elect a person with depression. According to Table 2, a far less portion of people will tend to act that way.
Table 3. Percentage of participants who “agree” or “strongly agree” with about perceived stigma towards depression patient scale statements.
| Statement about Perceived belief | Total (N = 935) | Gender | Major section | Region | Economic level | Occupation status | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Male (n = 327) | Female (n = 932) | Medical (n = 438) | Non-Medical (n = 821) | City (n = 890) | Rural region (n = 369) | Low (n = 105) | Moderate (n = 748) | Good (n = 363) | High (n = 43) | Worker (n = 542) | Non-worker (n = 717) | ||||||||||||||
| % | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | N | % (95% CI) | ||
| Most people belive that people with depression could snap out of it if they wanted | 632 | 50.20% | 132 | 11.30% | 500 | 42.9%** | 235 | 20.20% | 397 | 34.00% | 452 | 38.80% | 180 | 15.40% | 51 | 4.40% | 376 | 32.20% | 187 | 16.00% | 18 | 1.50% | 273 | 23.40% | 359 | 30.80% |
| Most people believe that Depression is a sign of personal weakness. | 476 | 37.80% | 107 | 9.40% | 369 | 32.3%* | 228 | 20.00% | 248 | 21.7%** | 356 | 31.20% | 120 | 10.5%* | 36 | 3.20% | 295 | 25.90% | 128 | 11.20% | 17 | 1.50% | 207 | 18.10% | 269 | 23.60% |
| Most people believe that Depression is not a medical illness. | 518 | 41.10% | 118 | 10.50% | 400 | 35.5%* | 231 | 20.50% | 287 | 25.5%** | 375 | 33.30% | 143 | 12.70% | 41 | 3.60% | 313 | 27.80% | 146 | 13.00% | 18 | 1.60% | 229 | 20.30% | 289 | 25.60% |
| Most people believe that people with Depression are dangerous. | 353 | 28.00% | 74 | 6.60% | 279 | 24.8%** | 154 | 13.70% | 199 | 17.7%** | 257 | 22.90% | 96 | 8.50% | 27 | 2.40% | 211 | 18.80% | 101 | 9.00% | 14 | 1.20% | 150 | 13.40% | 203 | 18.10% |
| Most people believe that it is best to avoid people with Depression so that you don’t become depressed yourself. | 486 | 38.60% | 99 | 8.80% | 387 | 34.5%** | 213 | 19.00% | 273 | 24.3%** | 364 | 32.40% | 122 | 10.9%* | 34 | 3.00% | 284 | 25.30% | 155 | 13.80% | 13 | 1.20% | 209 | 18.60% | 277 | 24.70% |
| Most people believe that people with Depression are unpredictable. | 361 | 28.70% | 84 | 7.50% | 277 | 24.9%* | 124 | 11.10% | 237 | 21.3%** | 254 | 22.80% | 107 | 9.60% | 29 | 2.60% | 221 | 19.80% | 98 | 8.80% | 13 | 1.20% | 162 | 14.50% | 199 | 17.90% |
| If they had Depression most people would not tell anyone. | 513 | 40.70% | 113 | 10.10% | 400 | 35.8%** | 216 | 19.30% | 297 | 26.6%** | 371 | 33.20% | 142 | 12.75 | 37 | 3.30% | 306 | 27.40% | 153 | 13.70% | 17 | 1.50% | 220 | 19.70% | 293 | 26.20% |
| Most people would not employ someone they knew had been affected with Depression | 402 | 31.90% | 84 | 7.50% | 318 | 28.4%** | 186 | 16.60% | 216 | 19.3%** | 300 | 26.80% | 102 | 9.1%* | 30 | 2.70% | 234 | 20.90% | 122 | 10.90% | 16 | 1.40% | 179 | 16.00% | 223 | 19.90% |
| Most people would not vote for a politician they knew had been affected with Depression | 401 | 31.90% | 79 | 7.10% | 322 | 28.8%** | 178 | 15.90% | 223 | 19.9%** | 289 | 25.80% | 112 | 10.00% | 33 | 3.00% | 235 | 21.00% | 118 | 10.60% | 15 | 1.30% | 178 | 15.90% | 223 | 19.90% |
| DPSS total score (mean ± SD) | 3.7 | 2.90 | 2.9 | 2.70% | 3.9 | 2.9%** | 4.2 | 3 | 3.3 | 2.7** | 3.8 | 2.9 | 3.4 | 2.8 | 3.4 | 2.9 | 3.7 | 2.8 | 3.6 | 2.9 | 3.4 | 3.4 | 3.6 | 2.8 | 3.7 | 2.8 |
Social distance
Participants’ endorsements for "probably unwilling" or "definitely unwilling" to have contact with the depressed person are shown in Table 4. In general, more than half of respondents won’t live next door to depressed people if they had to choose, more than half won’t work close to them, 36.90% won’t make friends with them. More than 90% won’t marry one of them.
Table 4. Percentage of participants who “probably unwilling” or “definitely unwilling” to have contact with depression patient.
| Statement about personal belief (SDS) | Total (N = 1259) | Gender | Major section | Region | Economic level | Occupation status | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Male (n = 327) | Female (n = 932) | Medical (n = 438) | Non-Medical (n = 821) | City (n = 800) | Rural region (n = 369) | Low (n = 105) | Moderate (n = 748) | Good (n = 363) | High (n = 43) | Worker (n = 542) | Non-Worker (n = 717) | ||||||||||||||
| % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||
| Live next door | 669 | 53.10% | 179 | 14.00% | 496 | 40.00% | 250 | 20.20% | 419 | 33.8%* | 477 | 32.20% | 171 | 15.50% | 55 | 4.40% | 378 | 30.50% | 208 | 16.80% | 28 | 2.3%* | 401 | 24.40% | 268 | 21.6%** |
| Spend the evening socializing | 487 | 38.70% | 135 | 10.90% | 352 | 28.40% | 204 | 16.50% | 283 | 22.9%** | 345 | 27.90% | 142 | 11.50% | 40 | 3.20% | 282 | 22.80% | 145 | 11.70% | 20 | 1.60% | 274 | 22.10% | 213 | 17.20% |
| Make friends | 465 | 36.90% | 133 | 10.80% | 332 | 26.90% | 172 | 13.90% | 293 | 23.80% | 328 | 26.60% | 137 | 11.10% | 43 | 3.50% | 278 | 22.50% | 126 | 10.20% | 18 | 1.50% | 270 | 21.90% | 195 | 15.80% |
| Work closely | 675 | 53.60% | 176 | 14.30% | 499 | 40.40% | 228 | 18.50% | 447 | 36.20% | 474 | 38.40% | 201 | 16.30% | 55 | 4.50% | 391 | 31.70% | 201 | 16.30% | 28 | 2.30% | 413 | 33.50% | 262 | 21.2%** |
| Marry into family | 1134 | 90.10% | 304 | 24.70% | 830 | 67.30% | 398 | 32.30% | 736 | 59.70% | 808 | 65.50% | 326 | 26.40% | 96 | 7.80% | 669 | 54.30% | 332 | 26.90% | 37 | 3.00% | 645 | 52.30% | 489 | 39.70% |
| DSS total score (mean ± SD) | 2.7 | 1.30% | 2.8 | 1.30% | 2.7 | 1.30% | 2.8 | 1.40% | 2.7 | 1.3%* | 2.7 | 1.30% | 2.7 | 1.30% | 2.7 | 1.30% | 2.7 | 1.30% | 2.8 | 1.30% | 3 | 1.40% | 2.6 | 1.30% | 2.8 | 1.40% |
Predictors for stigma and social distance by multiple linear regression analysis
We performed multiple logistic regression to analyze the predicted relationship between the three scales and other demographic variables. We found that almost variables couldn’t be linked in a statistically significant expected test for all scales, except the significant section (Medical student or non-medical student) on three scales, sex variable in depression perceived stigma scale, and the current region or location according to social distance scale. The adjusted R square values for DPSS, DPSS*, and SDS were 0.19, 0.050, and 0.005, respectively (Table 5).
Table 5. Predictors for stigma and social distance by multiple linear regression analysis.
| Dependent variable | Predictors | B | t | P* | R | R2 | Adj.R2 |
|---|---|---|---|---|---|---|---|
| DPSS | 0.165 | 0.24 | 0.19 | ||||
| Gender | 0.02 | 0.2 | 0.83 | ||||
| Age | 0.01 | 0.9 | 0.33 | ||||
| Major section | 0.44 | 4.9 | 0.00 | ||||
| Economic level | -0.06 | -1.06 | 0.28 | ||||
| Region settings | -0.02 | -0.23 | 0.81 | ||||
| Occupation status | -0.056 | -0.6 | 0.54 | ||||
| DPSS* | 0.23 | 0.056 | 0.050 | ||||
| Gender | 1.12 | 5.6 | 0.000 | ||||
| Age | 0.01 | 0.85 | 0.3 | ||||
| Major section | -1.06 | -5.7 | 0.000 | ||||
| Economic level | -0.17 | -1.3 | 0.18 | ||||
| Region settings | 0.14 | 0.78 | 0.43 | ||||
| Occupation status | -0.15 | -0.76 | 0.44 | ||||
| SDS | 0.09 | 0.01 | 0.005 | ||||
| Gender | -0.11 | -1.27 | 0.2 | ||||
| Age | -0.005 | -0.43 | 0.6 | ||||
| Major section | -0.14 | -1.6 | 0.09 | ||||
| Economic level | 0.05 | 0.94 | 0.3 | ||||
| Region settings | -0.17 | -2.1 | 0.03 | ||||
| Occupation status | 0.28 | 0.32 | 0.7 | ||||
Participants’ usual sources of mental health knowledge
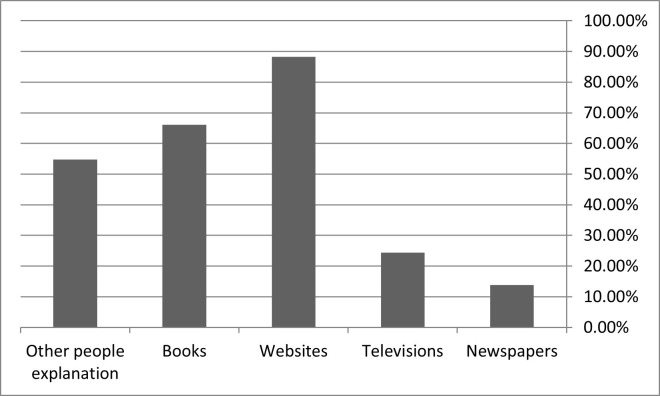
Showing in Fig 1, the most dependent source of information towards mental health knowledge was internet websites (85.80%). Books (64.40%), people explanation (53.10%), television (23.90%), and newspapers (11.30%) were also reliable sources of information, respectively.
Fig 1. Participants’ usual sources of mental health knowledge.
In Table 6, we asked the respondents about people, medications, and other interventions that they might find helpful for depressed people. Regarding most beneficial people, 79.3% agreed that a psychiatrist would greatly assist such mental health issues. About 59.8% thought that help from a close family member would be beneficial, and 59.3% consented to pray to God as a helpful solution.
Table 6. Recommended helpful interventions by the participants.
| People who can help | ||
| A typical GP or family doctor | 575 | 45.9% |
| A pharmacist | 140 | 11.2% |
| A counsellor | 349 | 27.9% |
| A social worker | 335 | 26.7% |
| A telephone counselling service | 126 | 10.1% |
| A psychiatrist | 994 | 79.3% |
| A psychiatric nurse | 418 | 33.4% |
| A clinical psychologist | 704 | 56.2% |
| Help from close family | 749 | 59.8% |
| Help from close friends | 849 | 67.8% |
| An herbalist | 42 | 3.4% |
| Pray to god for help | 743 | 59.3% |
| Medication which can help | ||
| Vitamins and mineral | 562 | 47.5% |
| Laxatives such as lactulose or Senna | 22 | 1.9% |
| Tonics or herbal medicines | 157 | 13.3% |
| Antibiotics | 86 | 7.3% |
| Antidepressants | 897 | 75.8% |
| Pain relievers such as aspirin or acetaminophen | 112 | 9.5% |
| Sleeping pills | 188 | 15.9% |
| Antipsychotics | 172 | 14.5% |
| Tranquillizer such as diazepam | 331 | 28% |
| Anxiolytics | 662 | 55.9% |
| Other Inventions | ||
| Becoming physically more active, such as playing more sports, or doing a lot more walking or gardening. | 1013 | 82% |
| Undergoing electro-convulsive therapy. | 690 | 55.9% |
| Getting out more. | 819 | 66.3% |
| Staying at home and resting. | 213 | 17.2% |
| Having an occasional alcoholic drink to relax. | 68 | 5.5% |
| Psychotherapy | 794 | 64.3% |
| Attending courses or relaxation, stress management, meditation, or yoga | 552 | 44.7% |
| Cutting out alcohol altogether. | 68 | 5.5% |
| Massage to relax. | 352 | 28.5% |
| Acupuncture therapy. | 71 | 5.7% |
| Being admitted to a psychiatric hospital. | 103 | 8.3% |
| Reading about people with similar problems and how they have dealt with them. | 690 | 55.9% |
| Going on a special diet or avoiding certain foods. | 352 | 28.5% |
| Aromatic therapy. | 94 | 7.6% |
| Hypnosis | 103 | 8.3% |
| Being admitted to a psychiatric ward or general hospital. | 117 | 9.5% |
| Help methods | ||
| Encourage the person to seek help. | 705 | 59.1% |
| Accompany the person to professional help. | 666 | 54.4% |
| Contact professional help on the person`s behalf. | 133 | 10.9% |
| Listen with the person | 723 | 59.1% |
| Encourage the person to see a community physician. | 313 | 25.6% |
| Encourage the person to see a counsellor. | 319 | 26.1% |
| Encourage the person to see psychiatrist. | 768 | 62.7% |
| Give advice. | 629 | 51.4% |
| Encourage the person to go to hospital. | 126 | 10.3% |
| Encourage the person to see psychologist. | 651 | 53.2% |
| Encourage the person to go to a mental health clinic. | 164 | 13.4% |
| Ask if the person wants help | 615 | 50.2% |
| Assess the problem/risk of harm. | 310 | 25.3% |
| Do an intervention. | 123 | 10% |
| Cheer the person up/boost the person`s confidence. | 755 | 61.7% |
| Tell the person`s parents or family. | 325 | 26.6% |
| Seek information for the person. | 547 | 46.9% |
| Help the person make new friends. | 599 | 48.9% |
| Help with chores/work. | ||
| Provide general support (e.g. practical emotional). | 638 | 52.1% |
| Spend time/socialize with the person. | 681 | 55.6% |
| Encourage the person to become physically active. | 699 | 57.1% |
Antidepressants (75.8%), anxiolytics (55.9%), and vitamins (47.5%) were the top three medications that respondents chose and thought to be most helpful, respectively.
Out of all the activities that have been suggested to aid depression, encouraging physical activity was chosen to be the most helpful intervention (82%). On the other hand, most respondents didn’t think cutting out alcohol would benefit much (5.5%).
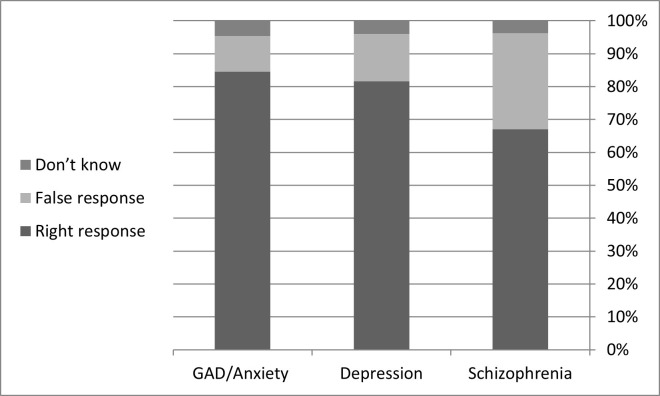
Finally, we reported good percentages of the correct knowledge responses toward diagnosing three selected psychiatric disorders. 14.30%, 15.20%, and 27.90% were the percentages of the incorrect answers in awareness of diagnosis Anxiety, Depression, and Schizophrenia, respectively (Fig 2).
Fig 2. Supporting information: (Knowledge towards the three mental disorders) [depression].
Discussion
To our knowledge, this is the first study to use a case vignette to investigate gender (male and female), major (medical and non-medical), region (rural and city), occupation (worker and non-worker), and economic status (low, moderate, good, high) differences in Syrian students’ stigma attitudes toward people with depression and the desire for social distancing. In each result, we attempted to investigated enough similar papers with close questionnaires, and discussed the similarities and the differences. However, we did not discuss studies that involved Syrians in asylum countries [32, 33].
The study found a higher level of stigma and desire for social distance among Syrian students toward depressive people than in other studies like muzzling et al. [40], where Italian people who experienced depression either directly or indirectly hold less stigmatizing attitudes. The percentage of the respondents who agreed that “depressive people are dangerous” was higher in China (60%) [41], Qatar (60%) [42], brazil (56%) [43], Italy (27%) [37] and united states (33%) [44] than in the present study (18.8%) and this may be because the onset of depression is due mainly to stressful life conditions other than hereditary causes [40]. A low percentage of the respondents (18.8%) stated that “if I have this problem, I will not tell anyone,” compared to a widespread belief among the Italian population (75%) who tend to hold their condition in solitude [40] and this in line with Australian people who have the belief of helpfulness of self-reliance [45]. Compared to the non-medical students (2.4%), medical students (8.4%) agreed more that “depression is a sign of personal weakness,” and this is in line with He et al. [41], where medical students (50%) agreed more about that subscale than non-medical (38%). This may be due to the that psychiatric education focuses mainly on professional knowledge for diagnosis and treatment but neglects the humanistic and emotional concerns that reduce the stigma towards the mentally ill patients [41] and may be associated with their belief that depressive patients are unpredictable, dangerous, and find it hard to control themselves [46].
To be more specific, respondents disagreed that “live next door to depressive neighbor” (50%), “spending the event socializing with depressive ones” (38.7%), “make depressive people close friends” (36.9%), “marry into a family with a history of depression” (90%) and “work closely with mentally ill people” (53.6%). This are line in with other studies like He et al. [41], where (71.1%) of the respondents agreed that they would not marry someone who is depressed, and (45.1%) of them would not work closely with them. The results are line in with other studies like He et al. [41] and Anosike et al. [47]. For example, a study in Nigeria found that 49% of the undergraduate students agreed that “I would be against any daughter of mine marrying a man who had been to the hospital to see a psychiatrist about mental problems.”The cause of keeping social distance may be due to the belief That depressive people are dangerous [41]. A line of research studies that also suggest that people with depression (or other mental illnesses) are difficult seems to generate increased social distancing [48, 49].
Most of the respondents (79.5%) hold the belief that mentally-ill people would gain great assistance from the psychiatrists, which is in line with other studies such as Holzinger et al. [50] and muzzling et al. [40], which reported that in Italy most of the respondents hold the attitude of seeking professional help as a first choice and this is compared to Ibrahim et al. [51] which reported that most of the students with mental health problems seek support first from non-medical personal such as peers and family. This indicates that social support represents a cornerstone step in achieving professional support in the future. Avoiding seeking professional help may be due to considering that as a threat to self-esteem, a sign of weakness, acceptance of failure, and the fear of being labeled as a mentally ill patient [51–53]. In addition to the previous causes, Özmen et al. [54] reported that respondents agreed that psychological counseling and social support for mentally ill patients are more effective than treatment by medications considered harmful and addictive.
In this study female students hold higher level of stigmatization and social distance atitude in all subscales than the male students compared to Anderson et al. [48] which reported that male students were more unwilling to work closely with depressive people, Korszun et al. [55] reported that female students hold a greater sympathy towards mentally ill patients than male students and He et al. which reported that male students holds higher stigamtizating and social distance attitude than female students in all subscales except “work closely” and “marry” with depressive person subscales (40.3% vs 47.5% and 68.5% vs 72.5% respectively). This may be attributed to the already imbalanced gender ratio in Syrian schools and that female students and the fact that females hold better knowledge about mental illness and subsequentaly more kind towards mentally ill patients [55].
Oliveira et al. [56] reported that the more the contact with mentally ill people, the lower the stigma. Unlike other physicians, psychiatrists and physicians with a relative of mental illness show lower stigma and higher scores on pity and help. This is explained by contact hypothesis and the fact that other specialities may contact the mentally ill patient in more serious conditions in the emergency room in virtue of their mental illness. As regard the students, the study reported that the more the education in psychiatry, the less the stigma. The level of the stigma has decreased significantly between the students after taking the psychiatry rotation which managed to change their thoughts and beliefs about the mantally ill patients.The study limitations include small sample size, the cross sectional design of the study doesn’t allow the follow up to observe the change in beliefs towards the mentally ill patient overtime and the old version of the AQ-27 in Portuguese.
He et al. [41] investigated the gender and tha major differences among college students in tha attitude towards depressive people. The study stated that unlike female students, male students agreed more that if they had depression, they wouldn’t tell anyone.With female predominence, Most of the respondents would be unwilling to marry or work with depressive peoples. The respondents thought that depressive people are ineloquent, unpredictable, danger and couldn’t control their behavoir. Thus they hold social distance attitude towards mentally ill patients. The study also reported that psychiatric education focused mainly on professional knowledge acquisition like how to diagnose and treat mentally ill patients but neglect the correction of the negative attitudes towards the patients and lack the humanistic and emotional concerns may contribute to the stigma.
Wu et al. [57] investigated the attitude towards depressive patients among the non-mental health professionals and reported that they are unwilling to hire a relative or marry someone with mental health problems like schizophrenia, depression or GAD (generalized anxiety disorder). They believe that they are dangerous, unpredicable and may hurt themselfies and others.The participants admitted that they gained such negative attitude through the socail media mainly from newspapers.
Palou et al. [58] reported that over the training course of the undergraduate nursing students in the mental health field, their attitudes towards mentally ill patients were significantly improved. It was also found that psychiatric education including the issues of stigmatization is associated with better knowledge acquisition and positive attitudes towards the people with mental health problems. The study has some limitations such as it included only the students so the results cannot be generalizable and not all socioeconomic characteristics of the participants were considered.
Dey et al. [59] found that males are more stigmatizing than females towards their peers with mental health problem. This may be due to the fact that males consider the mental health problem a sign of weakness not sickness and the fact that males should be able to manage their psychiatric problems on their owns. For the “unpredictible and dangerous” factor, authors stated that the cause of such attitude is likely due to the stereotypical image of masculinity. Males with mental health problems are more stigmatized than females. This may be due to the methodological design of the used survey that makes the character’s gender of the vignette was similar to the gender of the participants.
The limitations
The stigmatizing attitudes were investigated in the view of hypothetical scenarios, not towards real-life people, and no causal conclusion could be withdrawn as the study design is cross-sectional, not all social characteristics of the Syrian population were considered, and the people of the study are only students so the results cannot be generalized. In addition, Depression Stigma Scales and Social distance scale have not been validated in Arab populations.
Conclusion
A significant proportion of the Syrian students have a high level of stigma attitudes towards depressed persons. But massive numbers of Syrian students are willing to deal with these persons in their lives. Multiple recommendations should be made to improve the public health attitudes towards these patients, incredibly depressed persons. Campaigns are required to invest more efforts into wider areas of the country; this includes schools, universities, health centers, and hospitals. Now, It is more important than ever to start looking for more appropriate methods to implement anti-stigma ideologies into the community. It is also clear now that planning on increasing the psychological health workers capacity is vital for overall mental health issues in Syria. One of the most causes may be the deteriorated situation in Syria after the humanity war for 11 years. The leaders of the global humanitarian organizations should support the mental health psychiatry in Syria through awareness programs for suitable dealing with mental health patients, improving the current infrastructures of the psychiatric hospitals, and supporting mental centers.
Supporting information
(DOCX)
(ZIP)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Richa C. and Doron T., Depression: symptoms, causes, diagnosis, and treatment. Depression, 2021. [Google Scholar]
- 2.Bains N. and Abdijadid S., Major depressive disorder, in StatPearls [Internet]. 2021, StatPearls Publishing. [PubMed] [Google Scholar]
- 3.Lim G., Prevalence of Depression in the Community from 30 Countries between 1994 and 2014. Sci. 2018, Rep. doi: 10.1038/s41598-018-21243-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mojtabai R., Olfson M., and Han B.J.P., National trends in the prevalence and treatment of depression in adolescents and young adults. 2016. 138(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bayram N., Bilgel N.J.S.p., and p. epidemiology, The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. 2008. 43(8): p. 667–672. doi: 10.1007/s00127-008-0345-x [DOI] [PubMed] [Google Scholar]
- 6.Ibrahim A.K., et al., A systematic review of studies of depression prevalence in university students. 2013. 47(3): p. 391–400. [DOI] [PubMed] [Google Scholar]
- 7.Lei X.-Y., et al., Prevalence of depression among Chinese University students: a meta-analysis. 2016. 11(4): p. e0153454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Otte C., et al., Major depressive disorder. 2016. 2(1): p. 1–20. [DOI] [PubMed] [Google Scholar]
- 9.Uher R., et al., Major depressive disorder in DSM‐5: Implications for clinical practice and research of changes from DSM‐IV. 2014. 31(6): p. 459–471. [DOI] [PubMed] [Google Scholar]
- 10.Laursen T.M., et al., Mortality and life expectancy in persons with severe unipolar depression. 2016. 193: p. 203–207. [DOI] [PubMed] [Google Scholar]
- 11.Rovner B.W., et al., Depression and mortality. 1991. 265(8): p. 993–996. [DOI] [PubMed] [Google Scholar]
- 12.Majeed H. and Lee J.J.T.L.P.H., The impact of climate change on youth depression and mental health. 2017. 1(3): p. e94–e95. [DOI] [PubMed] [Google Scholar]
- 13.Angst J., Angst F., and H.H.J.J.o.c.p. Stassen, Suicide risk in patients with major depressive disorder. 1999. 60(2): p. 57–62. [PubMed] [Google Scholar]
- 14.Rayner A.V. and O Brien J.G.J.M.P., Depression and medical illness. 2003. 23: p. 133–154. [Google Scholar]
- 15.Keller M.B. and Berndt E.R.J.P.B., Depression treatment: a lifelong commitment? 2002. 36: p. 133–141. [PubMed] [Google Scholar]
- 16.Yokoya S., et al., A brief survey of public knowledge and stigma towards depression. 2018. 10(3): p. 202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santos J.C., Barros S., and I.M.J.G.q.n.r. Santos, Stigma: The Perspective of Workers on Community Mental Health Services—Brazil. 2016. 3: p. 2333393616670442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lauber C., Stigma and discrimination against people with mental illness: a critical appraisal. Epidemiology and Psychiatric Sciences, 2008. 17(1): p. 10–13. [PubMed] [Google Scholar]
- 19.Corrigan P.W. and Watson A.C., Understanding the impact of stigma on people with mental illness. World psychiatry, 2002. 1(1): p. 16. [PMC free article] [PubMed] [Google Scholar]
- 20.Wood L., et al., Public perceptions of stigma towards people with schizophrenia, depression, and anxiety. 2014. 220(1–2): p. 604–608. [DOI] [PubMed] [Google Scholar]
- 21.Corrigan P., et al., An attribution model of public discrimination towards persons with mental illness. Journal of health and Social Behavior, 2003: p. 162–179. [PubMed] [Google Scholar]
- 22.Sartorius N., Stigma and mental health. Lancet (London, England), 2007. 370(9590): p. 810–811. doi: 10.1016/S0140-6736(07)61245-8 [DOI] [PubMed] [Google Scholar]
- 23.Alonso J., et al., Perceived stigma among individuals with common mental disorders. 2009. 118(1–3): p. 180–186. [DOI] [PubMed] [Google Scholar]
- 24.Lauber C. and W.J.I.r.o.p. Rössler, Stigma towards people with mental illness in developing countries in Asia. 2007. 19(2): p. 157–178. [DOI] [PubMed] [Google Scholar]
- 25.Henderson C., Evans-Lacko S., and Thornicroft G., Mental illness stigma, help seeking, and public health programs. American journal of public health, 2013. 103(5): p. 777–780. doi: 10.2105/AJPH.2012.301056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patten S.B., et al., Perceived stigma among recipients of mental health care in the general Canadian population. 2016. 61(8): p. 480–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Givens J.L. and J.J.A.m. Tjia, Depressed medical students’ use of mental health services and barriers to use. 2002. 77(9): p. 918–921. [DOI] [PubMed] [Google Scholar]
- 28.Musa A., et al., Depression severity and depression stigma among students: A survey of universities in five countries. 2020. 208(11): p. 884–889. [DOI] [PubMed] [Google Scholar]
- 29.Yang F., et al., Stigma towards depression in a community-based sample in China. 2020. 97: p. 152152. [DOI] [PubMed] [Google Scholar]
- 30.Cheng D.R., et al., Stigma and perception of psychological distress and depression in Australian-trained medical students: results from an inter-state medical school survey. 2013. 209(3): p. 684–690. [DOI] [PubMed] [Google Scholar]
- 31.Angermeyer M., Corrigan P., and Rüsch N., Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry, 2005. 20(8): p. 529–539. doi: 10.1016/j.eurpsy.2005.04.004 [DOI] [PubMed] [Google Scholar]
- 32.Bär J., Pabst A., Röhr S., Luppa M., Renner A., Nagl M., et al. (2021). Mental Health Self-Stigma of Syrian Refugees With Posttraumatic Stress Symptoms: Investigating Sociodemographic and Psychopathological Correlates. Frontiers in Psychiatry, 12, 1113. 10.3389/FPSYT.2021.642618/BIBTEX [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Renner A., Jäckle D., Nagl M., Hoffmann R., Röhr S., Jung F., et al. (2021). Predictors of psychological distress in Syrian refugees with posttraumatic stress in Germany. PLOS ONE, 16(8), e0254406. doi: 10.1371/journal.pone.0254406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alsubaie S., Almathami M., Alkhalaf H., Aboulyazid A., & Abuhegazy H. (2020). A Survey on Public Attitudes Toward Mental Illness and Mental Health Services Among Four Cities in Saudi Arabia. Neuropsychiatric Disease and Treatment, 16, 2467–2477. doi: 10.2147/NDT.S265872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abi Hana R., Arnous M., Heim E., Aeschlimann A., Koschorke M., Hamadeh R. S., et al. (2022). Mental health stigma at primary health care centres in Lebanon: qualitative study. International Journal of Mental Health Systems, 16(1), 1–14. 10.1186/S13033-022-00533-Y/FIGURES/1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al-Adawi S., Dorvlo A. S. S., Al-Ismaily S. S., Alghafry D. A., Al-Noobi B. Z., Al-Salmi A., et al. (2002). Perception of and attitude towards mental illness in Oman. The International Journal of Social Psychiatry, 48(4), 305–317. doi: 10.1177/002076402128783334 [DOI] [PubMed] [Google Scholar]
- 37.Griffiths K.M., et al., Effect of web-based depression literacy and cognitive–behavioural therapy interventions on stigmatising attitudes to depression: Randomised controlled trial. 2004. 185(4): p. 342–349. [DOI] [PubMed] [Google Scholar]
- 38.Zhu L., et al., Psychometric properties of the Depression Stigma Scale (DSS) in Chinese cancer patients: a cross-sectional study. 2019. 9(7): p. e028429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Link B.G., et al., Public conceptions of mental illness: labels, causes, dangerousness, and social distance. 1999. 89(9): p. 1328–1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Munizza C., et al., Public beliefs and attitudes towards depression in Italy: a national survey. PLoS One, 2013. 8(5): p. e63806. doi: 10.1371/journal.pone.0063806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.He H., et al., Stigmatizing Attitudes Toward Depression Among Male and Female, Medical and Non-medical Major College Students. Front Psychol, 2021. 12: p. 648059. doi: 10.3389/fpsyg.2021.648059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zolezzi M., et al., Stigma associated with mental illness: perspectives of university students in Qatar. Neuropsychiatr Dis Treat, 2017. 13: p. 1221–1233. doi: 10.2147/NDT.S132075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Peluso Ede T. and Blay S.L., Public stigma in relation to individuals with depression. J Affect Disord, 2009. 115(1–2): p. 201–6. doi: 10.1016/j.jad.2008.08.013 [DOI] [PubMed] [Google Scholar]
- 44.Link B.G., et al., Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am J Public Health, 1999. 89(9): p. 1328–33. doi: 10.2105/ajph.89.9.1328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jorm A.F., et al., Belief in dealing with depression alone: results from community surveys of adolescents and adults. J Affect Disord, 2006. 96(1–2): p. 59–65. doi: 10.1016/j.jad.2006.05.018 [DOI] [PubMed] [Google Scholar]
- 46.Suwalska J., et al., Medical students and stigma of depression. Part I. Stigmatization of patients. Psychiatr Pol, 2016. 51(3): p. 495–502. [DOI] [PubMed] [Google Scholar]
- 47.Anosike C., Aluh D.O., and Onome O.B., Social Distance Towards Mental Illness Among Undergraduate Pharmacy Students in a Nigerian University. East Asian Arch Psychiatry, 2020. 30(2): p. 57–62. doi: 10.12809/eaap1924 [DOI] [PubMed] [Google Scholar]
- 48.Anderson K.N., et al., How people evaluate others with social anxiety disorder: A comparison to depression and general mental illness stigma. Am J Orthopsychiatry, 2015. 85(2): p. 131–8. doi: 10.1037/ort0000046 [DOI] [PubMed] [Google Scholar]
- 49.Angermeyer M.C. and Matschinger H., Public beliefs about schizophrenia and depression: similarities and differences. Soc Psychiatry Psychiatr Epidemiol, 2003. 38(9): p. 526–34. doi: 10.1007/s00127-003-0676-6 [DOI] [PubMed] [Google Scholar]
- 50.Holzinger A., Matschinger H., and Angermeyer M.C., What to do about depression? Help-seeking and treatment recommendations of the public. Epidemiol Psychiatr Sci, 2011. 20(2): p. 163–9. doi: 10.1017/s2045796011000266 [DOI] [PubMed] [Google Scholar]
- 51.Ibrahim N., et al., Do depression literacy, mental illness beliefs and stigma influence mental health help-seeking attitude? A cross-sectional study of secondary school and university students from B40 households in Malaysia. BMC Public Health, 2019. 19(4): p. 544. doi: 10.1186/s12889-019-6862-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Corrigan P., How stigma interferes with mental health care. Am Psychol, 2004. 59(7): p. 614–625. doi: 10.1037/0003-066X.59.7.614 [DOI] [PubMed] [Google Scholar]
- 53.Hammer J.H., Parent M.C., and Spiker D.A., Mental Help Seeking Attitudes Scale (MHSAS): Development, reliability, validity, and comparison with the ATSPPH-SF and IASMHS-PO. J Couns Psychol, 2018. 65(1): p. 74–85. doi: 10.1037/cou0000248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Özmen E., et al., Public opinions and beliefs about the treatment of depression in urban Turkey. Social Psychiatry and Psychiatric Epidemiology, 40, 869–876. Social psychiatry and psychiatric epidemiology, 2005. 40: p. 869–76. doi: 10.1007/s00127-005-0985-x [DOI] [PubMed] [Google Scholar]
- 55.Korszun A., et al., Medical student attitudes about mental illness: does medical-school education reduce stigma? Acad Psychiatry, 2012. 36(3): p. 197–204. doi: 10.1176/appi.ap.10110159 [DOI] [PubMed] [Google Scholar]
- 56.Oliveira A.M., et al., Stigmatizing Attitudes Toward Patients With Psychiatric Disorders Among Medical Students and Professionals. Front Psychiatry, 2020. 11: p. 326. doi: 10.3389/fpsyt.2020.00326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wu Q., et al., Stigmatizing Attitudes Towards Mental Disorders Among Non-Mental Health Professionals in Six General Hospitals in Hunan Province. Front Psychiatry, 2019. 10: p. 946. doi: 10.3389/fpsyt.2019.00946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Giralt Palou R., et al., Analysis of Stigma in Relation to Behaviour and Attitudes towards Mental Health as Influenced by Social Desirability in Nursing Students. Int J Environ Res Public Health, 2022. 19(6). doi: 10.3390/ijerph19063213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dey M., et al., Stigmatizing attitudes of Swiss youth towards peers with mental disorders. PloS one, 2020. 15(7): p. e0235034–e0235034. doi: 10.1371/journal.pone.0235034 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(ZIP)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.