Abstract
Acute respiratory tract infections pose a serious threat to the health of children worldwide, with viral infections representing a major etiology of this type of disease. Protective measures such as mask-wearing, social distancing, and hand hygiene can be effective in curbing the spread of severe acute respiratory syndrome coronavirus 2. These precautions may also have an impact on the spread of other respiratory viruses. In this study, we retrospectively compared the respiratory virus infections of children in Southwest China before and after the outbreak of COVID-19. Nasopharyngeal swabs were collected from 1578 patients under 14 years old with acute respiratory tract infection symptoms before and after COVID-19 pandemic. Nine common respiratory viruses including human bocavirus, human rhinoviruses, human coronaviruses, human adenoviruses, human metapneumovirus, respiratory syncytial virus, influenza A virus, influenza B virus, and parainfluenza virus were measured by advanced fragment analysis. The respiratory virus infection rates among children of all ages and genders in Southwest China under the precautions against COVID-19 pandemic were significantly lower than that of the same period before the pandemic. Our findings indicate that public health measures implemented during the COVID-19 pandemic, including strict mask-wearing, social distancing, and hand hygiene, may be effective in preventing the transmission of other respiratory viruses in children, thereby controlling the spread of infections.
Keywords: advanced fragment analysis, children, COVID-19, infection, public health, respiratory viruses
1. Introduction
Acute respiratory tract infections (ARTI) are divided into 2 categories, lower and upper respiratory tract infections, which seriously threaten the health of children worldwide.[1,2] Lower respiratory tract infections cause more deaths than any other infections in some countries, while upper respiratory tract infections usually lead to relatively mild symptoms but are widespread and account for the majority of respiratory infections.[3,4] Although bacteria, fungi, and mycoplasmas can lead to ARTI, viruses are the most common causative pathogens.[5,6] In recent years, viruses that cause ARTI mainly include human bocavirus (HBoV), human rhinoviruses (HRV), human coronaviruses (HCoV), human adenoviruses (HAdV), human metapneumovirus (HMPV), respiratory syncytial virus (RSV), influenza viruses, and parainfluenza virus (PIV). The accumulated data indicate that controlling the spread of respiratory viruses is beneficial to the growth and development of children. Because the immune and respiratory systems of infants and preschoolers are still immature, early-life respiratory infections may have a direct effect on lung development and increase the risk of asthma.[7,8] Additionally, early identification of respiratory viruses is also important. Due to the wide variation in treatment options for different respiratory pathogens, inappropriate medication may result in virus escape, mutation, and development of drug resistance.[9] Therefore, interrupting the transmission of respiratory viruses and early diagnosis of virus types with rapid molecular test platforms will be crucial in reducing unnecessary use of antibiotics and length of hospital stay, which can help ensure the health of children.[10,11]
Over the last few decades, routine clinical laboratory testing for respiratory viruses has largely been conducted using immunofluorescence assays for the detection of antigen or antibody. Given the poor sensitivity and labor-intensity involved, these methods have been gradually replaced by nucleic acid amplification tests.[12] Molecular assays have improved the detection rate of respiratory infections and also shorten the detection time dramatically.[13] With the rapid development of molecular techniques, multiplex polymerase chain reaction (PCR) has been increasingly used for the diagnosis of infectious diseases in recent years, due to its high efficiency.[14,15] The advanced fragment analysis (AFA) method perfectly combines multiple PCR amplification and capillary electrophoresis, allowing it possible to detect dozens of pathogenic genes simultaneously in a single analysis.[16] In view of these advantages, AFA was utilized in this study to simultaneously detect 9 common respiratory viruses from nasopharyngeal swabs of children.
The public health guidance for COVID-19 compiled by the Chinese Center for Disease Control and Prevention (briefly as China CDC) were published at the end of January 2020. Guidelines state that the public should wear surgical masks or N95 masks in public places, maintain hand hygiene, and keep distance from others (at least 1 m). Gatherings were prohibited or restricted. The effectiveness of China’s protective measures against the spread of severe acute respiratory syndrome coronavirus 2 was clearly evident. By the end of March, China had successfully controlled the epidemic.[17] In this study, we retrospectively compared the situation of respiratory virus infections among children in Southwest China before and after the COVID-19 pandemic, and analyzed whether the public health protection measures adopted by the Chinese government can effectively control the transmission of various respiratory viruses among children.
2. Materials and Methods
2.1. Participants
A total of 1578 children who visited the West China Second University Hospital were included in this study, including 784 children from January to June 2019 (Before COVID-19) and 794 children from January to June 2020 (After COVID-19). They were all under 14 years old and showed signs of ARTI, such as fever, sore throat, cough, sneezing, runny nose, and nasal congestion. Clinically collected nasopharyngeal swabs were stored at 4°C with viral storage solution and tested within 24 hours. Severe acute respiratory syndrome coronavirus 2 nucleic acid test for patients with fever or respiratory symptoms was required since January 2020 in our hospital, and all included children were negative. The study was conducted under the supervision of the Ethics Committee of West China Second University Hospital.
2.2. Advanced fragment analysis
In this study, the AFA method was used to detect 9 respiratory viruses commonly found in the upper respiratory tract of children, including HBoV, HRV, HCoV, HAdV, HMPV, RSV, influenza A virus, influenza B virus, and PIV. In brief, the multiplex PCR amplification experiment was carried out on Veriti thermal cycler platform using the multiplex PCR commercial kit (Health Gene Technologies, Ningbo, China). Subsequently, capillary electrophoresis was performed on a Dx3500 Series Genetic Analyzer (Life Technologies, Carlsbad, CA). The fragments were then analyzed by GeneMapperTM software (Applied Biosystems, Foster City, CA) and the cutoff value was set to 500. Besides the detection of specific viral nucleic acids, human DNA/RNA and reference genes were also tested to ensure that the entire process of sampling, extraction, and amplification was in control.
2.3. Statistical analysis
Infection rates were compared using the chi-squared test. All statistical analyses were performed using SPSS 19.0 (IBM, Armonk, NY). A P value of <.05 was considered to be statistically significant.
3. Results
3.1. The incidence of respiratory virus infections in children before and after the outbreak of COVID-19
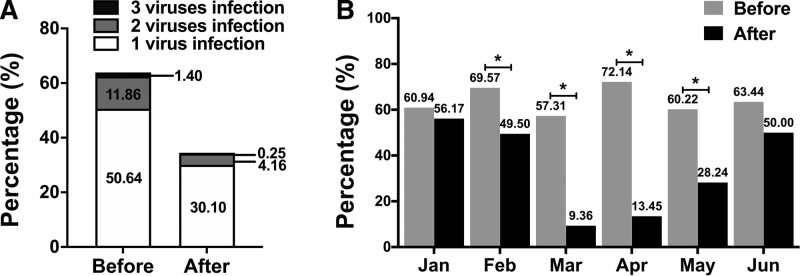
The characteristics of the children enrolled in this study are summarized in Table 1. As we can see in Figure 1A, the positive rate of respiratory virus infections was 63.90% (501/784) from January to June in the year before the COVID-19 outbreak, and 34.51% (274/794) in the same period after the pandemic. In addition, the prevalence of multiple respiratory virus in children was higher with a percentage of 13.27% (104/784) before COVID-19, while the multiple infection rate in children after the onset of COVID-19 was only 4.41% (35/794). The above data indicated that after the outbreak of COVID-19, the rate of respiratory virus infections and the rate of multiple respiratory virus infections in children in Southwest China decreased significantly (P < .001). Notably, the proportion of symptomatic patients who were undiagnosed in the 2 study periods was 36.10% and 65.49%, respectively. This may be due to the limited variety of pathogens detected by AFA. In terms of monthly infection data, the rate of respiratory virus infection in children was lower in each month from January to June after the outbreak than in the corresponding period before the outbreak (Fig. 1B). This phenomenon may be closely related to implementation of the national policies on mask-wearing, social distancing, and practicing good hand hygiene during the COVID-19 pandemic.
Table 1.
Characteristics of included children.
| Characteristics | COVID-19 outbreak | |
|---|---|---|
| Before | After | |
| Sex, n (%) | ||
| Male | 432 (55.10%) | 481 (60.58%) |
| Female | 352 (44.90%) | 313 (39.42%) |
| Age group (year), n (%) | ||
| <1 | 387 (49.36%) | 298 (37.53%) |
| ≥1 to <3 | 167 (21.30%) | 157 (19.77%) |
| ≥3 to <6 | 108 (13.78%) | 123 (15.49%) |
| ≥6 to <14 | 122 (15.56%) | 216 (27.20%) |
| Ethnicity (Han Chinese), n (%) | 784 (100%) | 794 (100%) |
The characteristics of children aged 0 to 14 years with respiratory tract infection symptoms in the first half of 2019 and 2020 (corresponding to Before and After in the table, respectively).
Figure 1.
Precautions for COVID-19 may effectively reduce respiratory virus infections in children. (A) The total respiratory virus infection rate was 63.90% (501/784) before COVID-19 outbreak, and 34.51% (274/794) after COVID-19 outbreak. For multiple viral infections, which were 13.27% (104/784) before COVID-19 outbreak, and then fell to 4.41% (35/794) after COVID-19 outbreak. (B) Compared to the same period before the COVID-19 outbreak, the infection rate decreased in each month from January to June after the outbreak, and the difference was statistically significant from February to May. These results indicated significant decline in respiratory virus infection rates as well as the prevalence of multiple viral infections among children in Southwest China after the outbreak of COVID-19.
3.2. The characteristics of respiratory virus infections in children before and after the outbreak of COVID-19
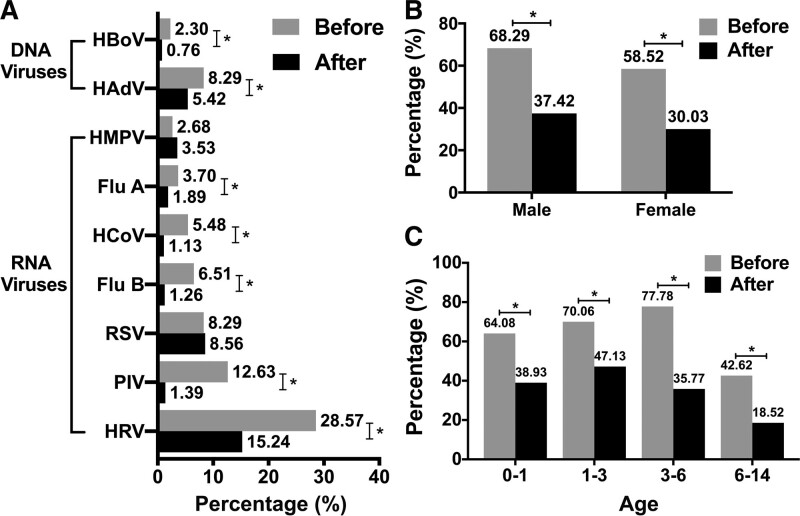
Among the types of respiratory virus infections in children, HRV was the most common virus detected in nasopharyngeal swab samples before and after the COVID-19 outbreak. The infection rates of HBoV and HAdV, 2 DNA viruses, have decreased significantly since the COVID-19 outbreak (P < .05). Among RNA viruses, only influenza A virus, HCoV, influenza B virus, PIV, and HRV showed a significant decline after the pandemic (P < .05) (Fig. 2A). For the gender analysis in Figure 2B, the data showed higher positive rates of respiratory virus infections in boys than in girls both before and after the pandemic, suggesting that boys are more susceptible to respiratory virus infections. The results may be linked to boys’ more outdoor activity. In detail, the positive rate of respiratory virus infections in boys before and after COVID-19 was 68.29% (295/432) and 37.42% (180/481), respectively. With regard to girls, the detection rate was 58.52% (206/352) and 30.03% (94/313), respectively. According to the age analysis in Figure 2C, the positive rates of virus in the 4 age groups of 0 to1, 1 to 3, 3 to 6, and 6 to 14 years old after the outbreak of COVID-19 decreased compared to that before the outbreak of the pandemic. Both before and after the onset of COVID-19, the rates of respiratory virus infection children aged 6 to 14 years old were significantly lower than that in younger age groups. These results indicated that under the strict public health measures of COVID-19, the infection rates of both DNA and RNA viruses have decreased, and the prevalence rates of children of different genders and ages have also decreased significantly. Therefore, the precautions against COVID-19 may effectively reduce the transmission of other respiratory virus infections among children in Southwest China.
Figure 2.
Characteristics of respiratory virus infections in children before and after COVID-19 outbreak. (A) HBoV, HAdV, Flu A, HCoV, Flu B, PIV, and HRV infection rates were significantly lower after the COVID-19 outbreak. (B) Respiratory viral infections in both boys and girls decreased significantly since the COVID-19 outbreak. For male participants, the total viral detection rate was higher than that of girls. (C) There was a significant decline in respiratory virus infection rates in all age groups of children since the outbreak of COVID-19. These results indicated that under the strict public health measures for COVID-19 prevention and control, the infection rates of both DNA and RNA viruses decreased, and the prevalence rates of children of different genders and ages also decreased significantly. Flu A = influenza A virus, Flu B = influenza B virus, HAdV = human adenovirus, HBoV = human bocavirus, HRV = human rhinovirus, PIV = parainfluenza virus.
4. Discussion
Respiratory diseases associated with viral infections pose a major threat to human health, with pediatric respiratory infections placing a huge burden on health care infrastructure.[9,18] Studies have shown that children are the main victims of respiratory infections, so particular attention is needed.[19,20] Although the clinical characteristics of respiratory virus infections vary around the world, the routes of transmission remain consistent, primarily through droplets but also through direct or indirect contact. This study compared the prevalence of respiratory virus infections among children in Southwest China before and after the outbreak of COVID-19, aiming to analyze whether the public health protection measures adopted by the Chinese government can effectively control the spread of various respiratory viruses among children.
It is worth mentioning that this study was conducted in the context of the COVID-19 in China. At the start of the COVID-19 outbreak in January 2020, the Chinese government instructed all citizens to strictly wear masks, maintain social distancing, and practice instant hand hygiene. Entrances to scenic spots, schools, hospitals, markets, and other public places have been equipped with special personnel for supervision and inspection. Disinfectants are provided free of charge in all public places to ensure timely hand hygiene is available to all. In Southwest China, where our research institute is located, the government controlled large gatherings of more than 50 people and urged people to cancel unnecessary daily gatherings. Our findings indicated that the incidence of respiratory virus infections was significantly reduced in children of all genders and ages following government public health measures. These measures reduce the spread of the viruses from person to person through droplets, as well as direct or indirect contact. A study conducted by Ma et al suggested that mask-wearing and instant hand hygiene can slow the exponential spread of avian influenza virus.[21] According to Chiu et al, when the physical distance between people is greater than 1 m, the possibility of virus transmission is low, and this possibility decreases with increasing distance.[22] Our results are consistent with these findings. Notably, in Figure 1B, there was no significant decrease in the rate of respiratory virus infections in January and June after the outbreak of COVID-19. We speculate that the reason for this phenomenon is that January was the beginning of the COVID-19 outbreak and people gradually adapted to a series of precautions. And in June, when COVID-19 was well contained in China, less stringent precautions might have been taken. As shown in Figure 2A, the infection rates for 7 common seasonal respiratory viruses declined significantly after the COVID-19 outbreak. However, HMPV and RSV infection rates did not decrease significantly after the outbreak. Further analysis revealed that HMPV and RSV infections were concentrated in January and February after the outbreak of COVID-19, while no positive samples for either virus were found in March to June. It is worth mentioning that before the outbreak, HMPV and HRV positive samples were found every month. Therefore, COVID-19 preventive measures also have a role in blocking HMPV and HRV transmission. Our data are similar to accumulated data showing that infants and young children under 6 years of age are more susceptible to respiratory viruses than children between 6 and 14 years of age, mainly due to physiological differences in the respiratory tract and immaturity of the immune system.[9,23] In terms of gender, our study found that boys were more likely to be infected with respiratory viruses, which is consistent with previous reports.[24,25]
The study still has some limitations. Firstly, at present there is no consensus for single and multiple viral infections. Some studies suggest that multiple viral infections are closely related to high hospitalization rate and clinical disease severity.[26,27] Other studies found no significant differences in clinical severity, outcome, and patient management between single and multiple viral infections.[13,28,29] Therefore, whether concurrent multiple viral infections are related to the severity of disease needs further study. Secondly, the population immunization against COVID-19 vaccine was introduced in 2021. Therefore, the effect of vaccination was not included in this study. However, we will consider the role of the vaccine in future studies. Finally, some studies suggest that boys have a higher risk of primary infections leading to hospitalization and a higher mortality rate than girls.[30–32] Further studies are necessary to fully elucidate the mechanisms of gender differences in respiratory virus infections.
In conclusion, the positive detection rate of respiratory virus in children has decreased significantly since the outbreak of COVID-19. This achievement may be attributed to the implementation of national policies on mask-wearing, social distancing, and good hand hygiene during the COVID-19 pandemic. In the context of the COVID-19 pandemic and the absence of vaccine during the study periods, our findings suggest that preventive measures to block the route of transmission of the respiratory viruses are effective. This research may have some guiding significance for the prevention and control of other possible pathogen pandemics in the future.
Author contributions
Conceptualization: Ting Liu.
Data curation: Shu-Yu Lai, Yan-Ling Liu, Yong-Mei Jiang.
Formal analysis: Shu-Yu Lai, Ting Liu.
Project administration: Ting Liu.
Visualization: Shu-Yu Lai, Ting Liu.
Writing – original draft: Shu-Yu Lai, Yan-Ling Liu, Yong-Mei Jiang.
Writing – review & editing: Ting Liu.
Abbreviations:
- AFA =
- advanced fragment analysis
- ARTI =
- acute respiratory tract infections
- HAdV =
- human adenovirus
- HBoV =
- human bocavirus
- HCoV =
- human coronavirus
- HMPV =
- human metapneumovirus
- HRV =
- human rhinovirus
- PCR =
- polymerase chain reaction
- PIV =
- parainfluenza virus
- RSV =
- respiratory syncytial virus.
This work was supported by the National Natural Science Foundation of China (No.81801628) and the Clinical Research Foundation of West China Second University Hospital (KL076).
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
How to cite this article: Lai S-Y, Liu Y-L, Jiang Y-M, Liu T. Precautions against COVID-19 reduce respiratory virus infections among children in Southwest China. Medicine 2022;101:37(e30604).
Contributor Information
Shu-Yu Lai, Email: shuyulai@126.com.
Yan-Ling Liu, Email: liuting88823@163.com.
Yong-Mei Jiang, Email: jiangym_scu@163.com.
References
- [1].Monto AS. Studies of the community and family: acute respiratory illness and infection. Epidemiol Rev. 1994;16:351–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Shi T, Arnott A, Semogas I, et al. The etiological role of common respiratory viruses in acute respiratory infections in older adults: a systematic review and meta-analysis. J Infect Dis. 2020;222(Supplement_7):S563–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Jain N, Lodha R, Kabra SK. Upper respiratory tract infections. Indian J Pediatr. 2001;68:1135–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Mizgerd JP. Acute lower respiratory tract infection. N Engl J Med. 2008;358:716–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Doan Q, Enarson P, Kissoon N, et al. Rapid viral diagnosis for acute febrile respiratory illness in children in the emergency department. Cochrane Database Syst Rev. 2014:9:CD006452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Yen CY, Wu WT, Chang CY, et al. Viral etiologies of acute respiratory tract infections among hospitalized children – a comparison between single and multiple viral infections. J Microbiol Immunol Infect. 2019;52:902–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chan JY, Stern DA, Guerra S, et al. Pneumonia in childhood and impaired lung function in adults: a longitudinal study. Pediatrics. 2015;135:607–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Johnston ID, Strachan DP, Anderson HR. Effect of pneumonia and whooping cough in childhood on adult lung function. N Engl J Med. 1998;338:581–7. [DOI] [PubMed] [Google Scholar]
- [9].Tregoning JS, Schwarze J. Respiratory viral infections in infants: causes, clinical symptoms, virology, and immunology. Clin Microbiol Rev. 2010;23:74–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Brendish NJ, Clark TW. Antiviral treatment of severe non-influenza respiratory virus infection. Curr Opin Infect Dis. 2017;30:573–8. [DOI] [PubMed] [Google Scholar]
- [11].van Houten CB, Cohen A, Engelhard D, et al. Antibiotic misuse in respiratory tract infections in children and adults-a prospective, multicentre study (TAILORED treatment). Eur J Clin Microbiol Infect Dis. 2019;38:505–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Zhang Y, Cao L, Xu Z, et al. Evaluation of a multiplex PCR assay for detection of respiratory viruses and mycoplasma pneumoniae in oropharyngeal swab samples from outpatients. J Clin Lab Anal. 2020;34:e23032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Asner SA, Rose W, Petrich A, et al. Is virus coinfection a predictor of severity in children with viral respiratory infections? Clin Microbiol Infect. 2015;21:264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Wang S, Yang F, Li D, et al. Clinical application of a multiplex genetic pathogen detection system remaps the aetiology of diarrhoeal infections in Shanghai. Gut Pathog. 2018;10:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Vallieres E, Renaud C. Clinical and economical impact of multiplex respiratory virus assays. Diagn Microbiol Infect Dis. 2013;76:255–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zhang H, Cheng H, Wang Q, et al. An advanced fragment analysis-based individualized subtype classification of pediatric acute lymphoblastic leukemia. Sci Rep. 2015;5:12435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Liu J, Zhang L, Yan Y, et al. Excess mortality in Wuhan city and other parts of China during the three months of the covid-19 outbreak: findings from nationwide mortality registries. BMJ. 2021;372:n415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Monick MM, Yarovinsky TO, Powers LS, et al. Respiratory syncytial virus up-regulates TLR4 and sensitizes airway epithelial cells to endotoxin. J Biol Chem. 2003;278:53035–44. [DOI] [PubMed] [Google Scholar]
- [19].Galanti M, Birger R, Ud-Dean M, et al. Longitudinal active sampling for respiratory viral infections across age groups. Influenza Other Respir Viruses. 2019;13:226–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Toivonen L, Karppinen S, Schuez-Havupalo L, et al. Burden of recurrent respiratory tract infections in children: a prospective cohort study. Pediatr Infect Dis J. 2016;35:e362–9. [DOI] [PubMed] [Google Scholar]
- [21].Ma QX, Shan H, Zhang HL, et al. Potential utilities of mask-wearing and instant hand hygiene for fighting SARS-CoV-2. J Med Virol. 2020;92:1567–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Chiu NC, Chi H, Tai YL, et al. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: retrospective national epidemiological surveillance study. J Med Internet Res. 2020;22:e21257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Harless J, Ramaiah R, Bhananker SM. Pediatric airway management. Int J Crit Illn Inj Sci. 2014;4:65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wang H, Zheng Y, Deng J, et al. Prevalence of respiratory viruses among children hospitalized from respiratory infections in Shenzhen, China. Virol J. 2016;13:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Zhang D, He Z, Xu L, et al. Epidemiology characteristics of respiratory viruses found in children and adults with respiratory tract infections in southern China. Int J Infect Dis. 2014;25:159–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Chauhan JC, Slamon NB. The impact of multiple viral respiratory infections on outcomes for critically ill children. Pediatr Crit Care Med. 2017;18:e333–8. [DOI] [PubMed] [Google Scholar]
- [27].Cilla G, Onate E, Perez-Yarza EG, et al. Viruses in community-acquired pneumonia in children aged less than 3 years old: high rate of viral coinfection. J Med Virol. 2008;80:1843–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Scotta MC, Chakr VC, de Moura A, et al. Respiratory viral coinfection and disease severity in children: a systematic review and meta-analysis. J Clin Virol. 2016;80:45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Wishaupt JO, van der Ploeg T, de Groot R, et al. Single- and multiple viral respiratory infections in children: disease and management cannot be related to a specific pathogen. BMC Infect Dis. 2017;17:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Boonyaratanakornkit J, Englund JA, Magaret AS, et al. Primary and repeated respiratory viral infections among infants in rural Nepal. J Pediatric Infect Dis Soc. 2020;9:21–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Haerskjold A, Kristensen K, Kamper-Jorgensen M, et al. Risk factors for hospitalization for respiratory syncytial virus infection: a population-based cohort study of Danish children. Pediatr Infect Dis J. 2016;35:61–5. [DOI] [PubMed] [Google Scholar]
- [32].Chen J, Hu P, Zhou T, et al. Epidemiology and clinical characteristics of acute respiratory tract infections among hospitalized infants and young children in Chengdu, West China, 2009-2014. BMC Pediatr. 2018;18:216. [DOI] [PMC free article] [PubMed] [Google Scholar]