Abstract
Study Design:
Controlled laboratory study using a single cohort design.
Objectives:
To determine if balance in older adults could be significantly improved with foot orthotic intervention.
Background:
Poor balance has been associated with risk for falls. Limited evidence exists indicating that foot orthoses influence balance.
Methods:
Thirteen individuals older than 65 who reported at least 1 unexplained fall during the past year and who demonstrated poor balance participated in the study. Subjects were tested for one-leg stance, tandem stance, tandem gait, and alternating step tests during the first (SCREEN) and second (PRE) sessions prior to foot orthotic intervention. Tests were repeated during the second testing session immediately after custom foot orthotic intervention (POST), and 2 weeks following foot orthotic use (FU). SCREEN and PRE measures were compared for stability using absolute difference computations and Friedman’s rank test. PRE, POST, and FU data were analyzed using the Friedman’s rank test (alpha = 0.05) with Bonferroni correction for multiple post-hoc comparisons.
Results:
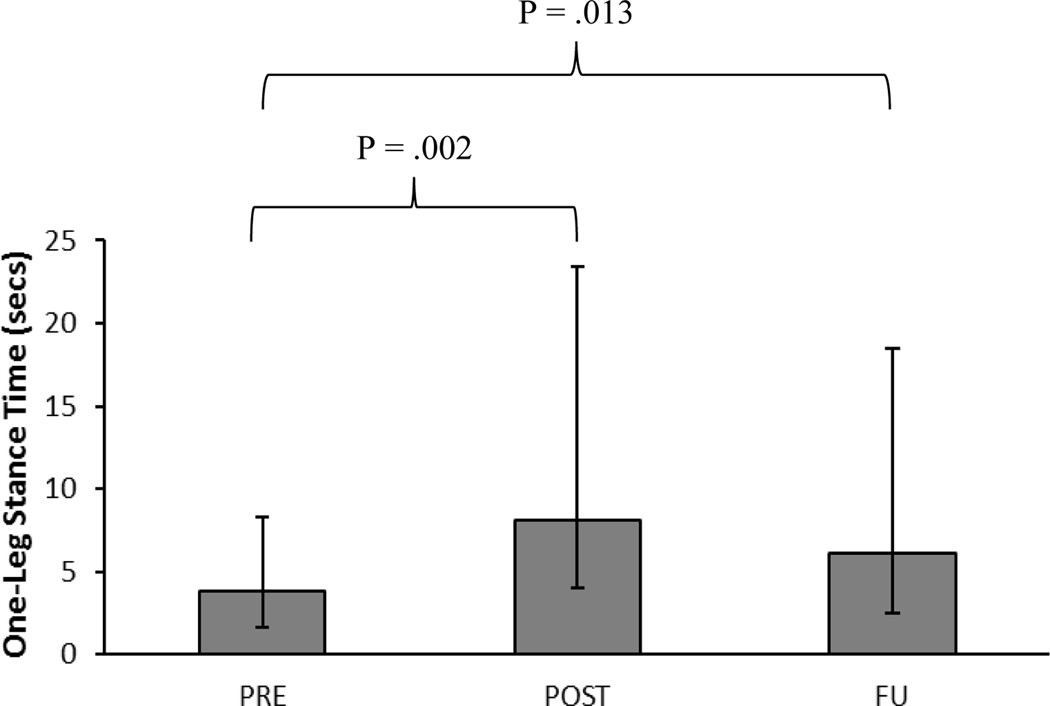
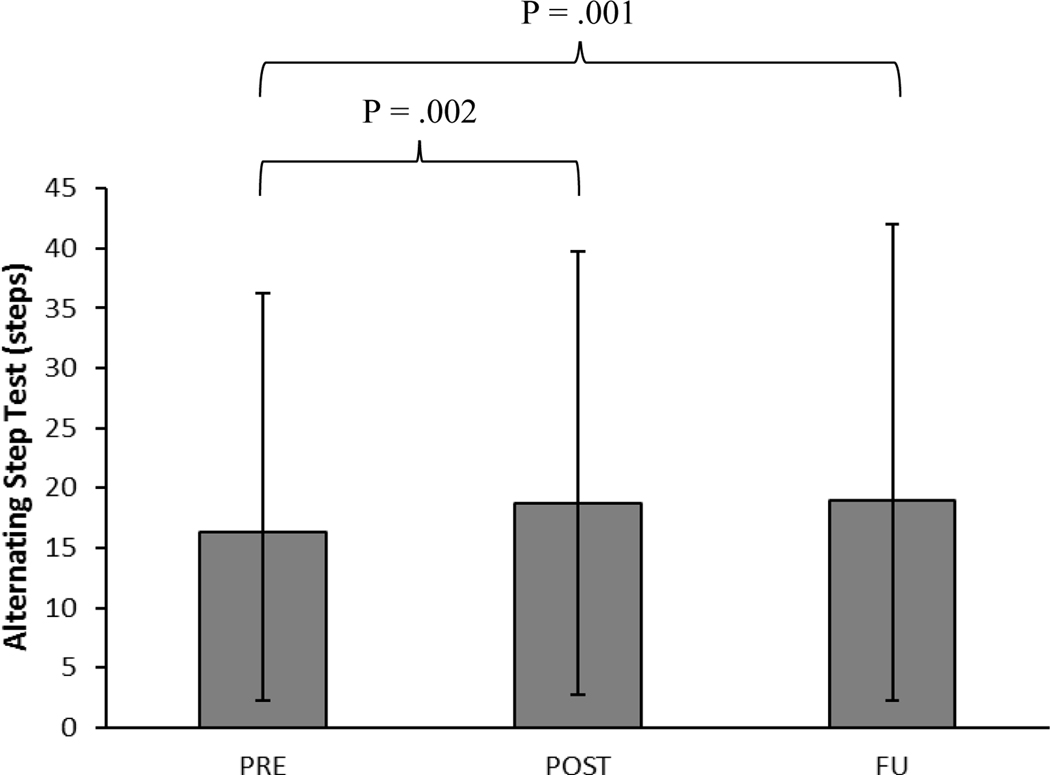
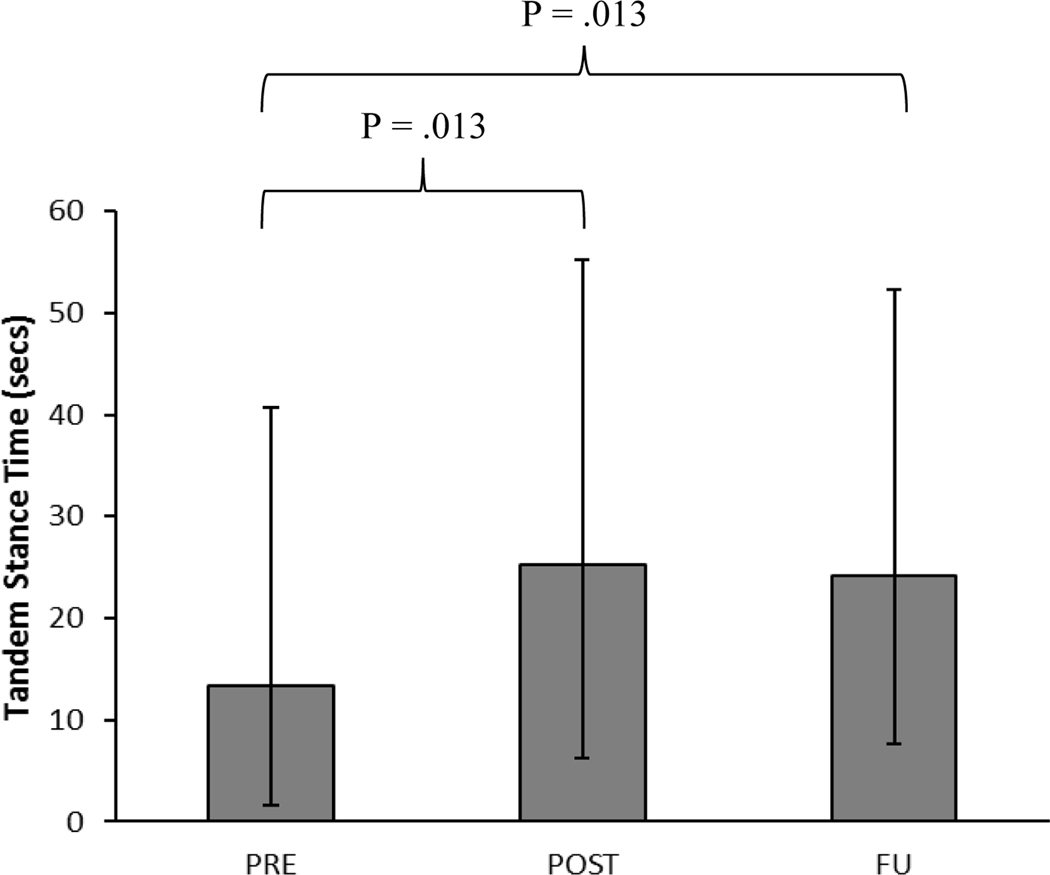
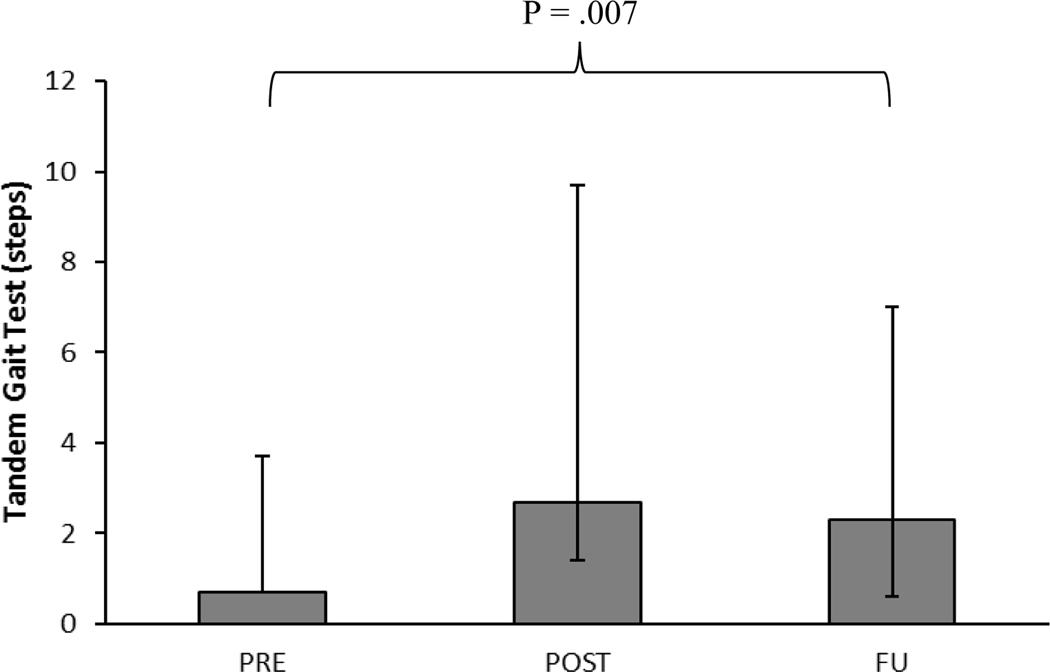
Each balance measure was statistically equivalent between the SCREEN and PRE measurements. One-leg stance times for PRE were significantly less than POST (P = .002) and FU (P = .013) measurements. Tandem stance times for PRE were significantly less than POST (P = .013) and FU (P = .013) measurements. Steps taken for the tandem gait test during the PRE measurements were significantly fewer than steps taken for the FU test (P = .007). Steps taken during the alternating step test for the PRE test were significantly fewer than steps taken during the POST (P = .002) and FU (P =.001) tests. POST and FU measurements were not significantly different for any of the 4 outcome measures.
Conclusions:
The results provide preliminary evidence that foot orthoses can effect improvement in balance measures for older adults.
Keywords: Postural Control, Stability, Geriatrics, Orthoses, Falls
Falls among the elderly constitute a significant problem in terms of potential injuries, adverse consequences on quality of life, and costs to the individual and society. Perhaps more significantly, falls are the leading cause of accidental death among the elderly.27 More than 1.6 million older individuals were treated by emergency room personnel for fall related injuries in 2001.4 Approximately 20–30% of the injuries that occur from falls are severe injuries such as hip fracture or head injury.37 Such injuries may have deleterious effects on mobility and quality of life. For those elders who incur a hip fracture, 25% will die within 6 months of the injury, and those who survive will have a 10–15% reduction in their life expectancy.45 Costs for medical care for fall injuries are substantial because approximately 50% of individuals who require hospitalization for injuries incurred from a fall are then discharged to nursing home care.34 By 2020, the total cost of falls among older adults is projected to be $43 billion.38 Even in the absence of physical injury, a history of falls may induce fear of falling, self-imposed decreased activity levels, functional dependence on others, social isolation, depression, and reduced quality of life.9,21
Numerous investigators have demonstrated that balance impairment is a significant contributor to falls among the elderly.3,7,30,41 Several balance performance measures have been associated with falls history, including the one-leg stance test and the balance section of the Performance Oriented Mobility Assessment.40 A variation of the one-leg stance test has been described by Toulotte et al,42 who reported that older individuals with a history of falls touched the non-weight bearing foot to the ground 3 times more often than older individuals with no history of falls during 30 seconds of unilateral standing. Lord et al20 also have documented that 50 older adults who incurred an injurious fall had significantly poorer performance for static standing balance and dynamic balance while walking in place compared with a group of age and sex matched controls.
The testing of balance performance should take into consideration that the central nervous system uses different strategies for maintaining balance, depending on whether the task is static or dynamic. Maintenance of balance in quiet standing is an example of a static task, which involves integration of sensory information as part of a closed-loop (feedback) system.28 In quiet standing, whether the stance position is bipedal or unipedal, the line of gravity remains within the base of foot support.12 However, maintenance of balance during dynamic tasks, such as walking, requires use of feed forward control.13 When an individual is walking or changing from one position to another, the line of gravity may move outside the base of foot support. A distinction between static and dynamic balance performance in community-dwelling older adults is supported by the finding that scores on static and dynamic balance tests are only moderately correlated.35 Because static and dynamic tasks challenge different aspects of balance control, balance assessment should include performance under both types of conditions.
Previous investigators have manipulated the interface between the foot and walking support surface in an attempt to improve balance and, therefore, possibly reduce the risk of falling. Several investigators have documented that balance in older individuals is better with walking shoes compared with shoes with elevated heels.1,22,39 Balance also is poorer when shoe sole material is softer than normal,22 sole surface area is smaller,39 when shoes are not worn or only socks are worn,11, 17, 24 or when shoes have absent fixation (straps or laces) or are made of flexible material.24,36
Other investigators have examined the influence of shoe inserts on balance based on the concept of attempts to enhance somatosensory stimulation of the skin on the plantar aspect of the foot. Perry et al31 reported that an insole designed to facilitate foot-sole sensation with a ridge around the periphery of the insert resulted in greater lateral stability and reduced the number of falls in their sample of community-dwelling older adults. Fifty percent of the sample assigned to wear the special insole, however, reported initial discomfort on wearing the insole and 1 of the participants refused to wear the insole because of this discomfort. Vibration has also been used to promote somatosensory stimulation of the plantar aspect of the foot. Priplata et al,32,33 in 2 separate studies, have documented that placement of vibrating gel-based insoles in the shoes of elderly subjects resulted in significant reduction in sway parameters for quiet standing. The cost and feasibility of this instrumentation, however, may preclude widespread use among the elderly.
Another approach in the area of shoe inserts has been the use of custom or semi-custom arch supports to influence postural control. Our clinical experience indicates that custom foot orthotics improve postural stability for individuals who have either excessively supinated or pronated foot structure. In the case of the supinated (high arched foot) foot, postural control may be challenged because the individual has a relatively small base of support between the foot and the support surface. In contrast, postural control deficits for individuals with excessively pronated (collapsed arch) foot structure may be attributed to hypermobile/unstable function of joints within the foot. These insoles also may stimulate the plantar aspect of the foot over a larger surface area, thereby providing greater sensory input that can be used to adjust for changes in the center-of-pressure imposed on the plantar aspect of the foot. Custom foot orthoses have been used previously to improve standing balance for samples of younger subjects.5,29 In the only study we identified involving a sample of older adults, semi-custom arch supports effected significant improvements in the Berg Balance Scale and the Timed Up and Go Test for 67 older adults.26 The investigators, however, did not document the stability of their measures prior to the intervention and did not have a control group.
The purpose of the current study, therefore, was to determine if custom foot orthoses would improve static and dynamic measures of balance older adults who reported at least 1 unexplained fall during the year prior to enrollment in the study and who demonstrated poor balance on the one-leg stance test. We hypothesized that custom foot orthoses would improve performance on the following balance measures: one-leg stance test, tandem stance test, tandem gait test, and the alternating step test.
METHODS
Subjects
Potential subjects were recruited by posting fliers at local retirement communities and senior centers. Subjects for this study were men and women older than 65 who reported at least 1 unexplained fall during the 1 year preceding enrollment in the study. A fall was defined as an unexpected event in which the subject lost their balance, slipped, or tripped and landed on the floor or ground or a lower level.19 Subjects also had to demonstrate poor balance on the one-leg stance test. Poor balance was defined as the inability to stand in single leg stance for 5 or more seconds. Subjects had to be able to walk independently at least 10 meters on a level surface without the use of any assistive device. All subjects were able to read and understand English, and were able to follow all instructions and perform all study procedures. Subjects had to demonstrate at least 20/40 vision with any correction from glasses they wore based on testing with a Snellen Eye Chart so that performance on the balance tests would not be impaired by poor vision. We arbitrarily selected this visual criterion to insure that subjects would be able to see the step being used for the alternating step test and would be able to see the lines used for the tandem gait task.
Individuals with moderate or severe dementia, as determined by a Six-Item Screener score of 3 or less2 were excluded from the study. Individuals who had had any type of lower extremity amputation, any lower extremity surgery during the previous year, or any other type of surgery during the previous 6 months were excluded from the study. Individuals were also excluded if they: had been diagnosed with any neurological or vestibular disorder; reported that they regularly became dizzy or weak when they rose to standing from a seated or lying position; were using foot orthotics; or had ingested any substance that might affect postural control (e.g., alcohol, sedatives, cold remedies, stimulants, etc.) within the 24 hours that preceded testing. Subjects also reported that they were not taking any narcotic medicines or tricyclic anti-depressants such as Elavil or Imipramine, because these medicines may influence balance. Subjects were asked to not engage in exercise or training that emphasized balance training (e.g., Tai Chi, etc.) during their involvement in the study. Informed consent was obtained by the principal investigator and the rights of the subjects were protected at all times. The study protocol for this work was approved by the Biomedical IRB of the Office of Human Research Ethics at the University of North Carolina at Chapel Hill, Chapel Hill, NC.
Testing Procedures
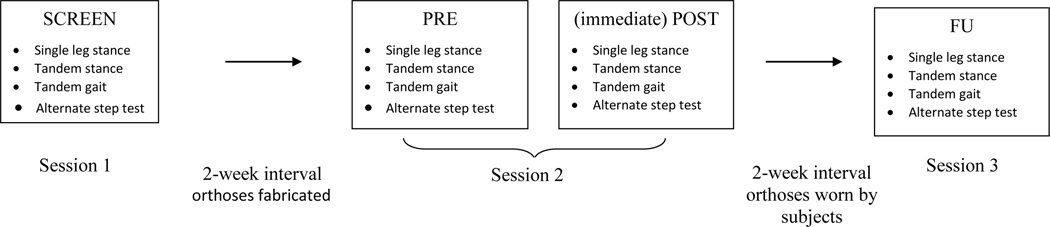
Subjects were tested on 3 occasions, each separated by approximately 2 weeks, and wore the same shoes for all testing sessions (FIGURE 1). Subjects were asked to wear laced walking or athletic shoes that they usually wore for a majority of the day. During the initial testing session (SCREEN), subjects were assessed for cognition using the Six-Item Screener test.2 If the potential subject made fewer than 3 errors on the Six-Item Screener test, they were then tested for the one-leg stance test. The subject wore a standard safety belt for all balance testing and the principal investigator lightly held the safety belt during testing to insure subject safety. For the one-leg stance test, the subject was asked to stand on the lower extremity of their preference and bend the knee of the other lower extremity, attempting to stand for as long as possible on the stance limb. Standing time was recorded with a stop watch to the nearest tenth of a second. The mean of 3 trials was used to determine if the subject was unable to stand for a minimum of 5 seconds. Timing stopped when the subject moved the stance foot (e.g., hopping movement), touched down with the other leg, contacted any other external support, or needed assistance from the investigator to prevent loss of balance. Individuals who were able to stand for more than 5 seconds were dismissed from the study.
FIGURE 1.
Schematic that details the 4 times of measurement over 3 testing sessions.
If the subject met the inclusion criterion for the one-leg stance test, testing proceeded and height, weight, age, and gender were recorded. The one-leg stance test was completed for the other lower extremity, again computing the mean of 3 trials. If the subject was able to stand on the second test limb for more than 5 seconds they were dismissed from the study. The average of the mean test time for the right limb and the mean test time for the left limb was used for data analysis.
Subjects then performed the tandem stance test.44 The subject stood with one foot directly in front of the other with the heel of the front foot touching the toe of the back foot and the feet forming a straight line with no angulation. The subject assumed this position while holding on to the back of a chair and then was asked to release their contact with the chair and stand in this position as long as possible with eyes open and arms in their preferred position, for a maximum of 30 seconds. Standing time was recorded with a stop watch to the nearest tenth of a second. Timing stopped if the subject contacted any other external support (e.g., the chair), changed foot position, or needed assistance from the investigator to maintain balance. The mean of 3 trials was computed. The test was then repeated reversing the front and rear foot positions, again computing the mean of 3 trials for data analysis. The average of the 2 means was used for data analysis.
The subject then performed the tandem gait test.44 The subject was asked to walk with eyes open at a comfortable pace in a straight line, heel to toe, between 2 strips of tape that were 12 cm apart. The number of properly placed steps was counted, up to a maximum of 20 steps. The counting of successful steps ended when the first step was taken resulting in faults such as feet not in alignment, or the heel of the front foot was not touching the toe of the other foot. The mean of 3 trials was used for data analysis.
The final balance measure was the alternating step test. This is a dynamic stepping task that is a modification of the alternating step test item from the Berg Balance Scale (BBS),25 for which performance is categorically rated on a scale from 0–4. A rating of 4 on the BBS indicates that an individual is able to make 8 alternating foot placements in 20 seconds. Pilot data indicated that subjects we would be testing would likely be able to make many more than 8 foot placements during a 20 second period of time. A rating of 4, therefore, would not be helpful in differentiating balance capability among these individuals and would not be sensitive to any improvement in balance resulting from an intervention. The modified alternating step test we used involved counting the actual number of alternating steps taken during a 20 second test period as the outcome measure, similar to a test described by Isles et al.15 The subject performed this test by standing with both feet initially positioned 5 cm from a 7.5 cm high platform. The subject was asked to place the entire plantar surface of one foot onto the platform and then bring the foot back to the starting position. The subject then placed the other foot up onto the platform and back to the starting position. This alternating pattern was repeated as many times as possible during a 20 second test period. The number of completed steps up onto the step and down to the starting position was counted. The mean of 3 trials was used for data analysis.15
Our purpose in using the mean performance of both lower extremities was to obtain a more complete representation of the each subject’s balance capability. Daily functional movements require that individuals balance either statically or dynamically on each of their lower extremities, and we did not want to represent an individual’s balance only by the performance of a preferred test limb.
When balance testing was concluded, the principal investigator examined each subject for structural alignment of the lower extremity. Structural exam items noted were: cavus/planus foot structure during unilateral stance, forefoot to rearfoot alignment, passive dorsiflexion available in prone position with the knee extended, tibial varum in standing, limb length inequality, and foot equinus.10 The principal investigator, who has 24 years of experience fabricating custom foot orthoses, then molded foot orthotic materials to the subject’s feet with the subject in the seated position prior to the end of the subject’s first testing session. The principal investigator then fabricated the subject’s foot orthoses between the first and second testing session. The fabrication of these semi-rigid orthoses is described in another publication,14 and involves the use of thermal cork for rearfoot posting and filling in of the arch space, as well as 0.375 mm thick nickleplast (Alimed Corp, Dedham, MA) for fabrication of forefoot posts, rearfoot posts, and heel lift. A 0.375 mm (1/8 inch) medial forefoot post was incorporated into the orthoses if the subject appeared to have more than 5 degrees of forefoot varus. Forefoot varus is a malalignment that can cause foot pronation, and the addition of the medial forefoot post was designed to limit the foot pronation that would occur.10 A 0.375 mm heel lift was added to the foot orthoses if the subject did not have passive dorsiflexion beyond neutral dorsiflexion/plantar flexion. Inadequate dorsiflexion at the talocrural joint can cause foot pronation and inadequate length of the triceps surae could pull an individual’s center of mass posteriorly toward the heel, thereby creating instability.10 Heel lift was added to limit these effects. A medial rearfoot post ranging from 0 to 0.375 was added to the orthoses if the subject demonstrated tibial varum or other malalignments (e.g., genu varus) making the distal 1/3 of the leg be inclined medially away from the true vertical during single limb stance. Such a malalignment could result in foot pronation to bring the medial aspect of the heel to the ground.10 A medial rearfoot post was added to limit this influence. If the subject had more than 0.375 mm of limb length inequality in standing while wearing shoes, then the principal investigator provided several pieces of 0.375 mm heel lift material so that the subject could report the magnitude of heel lift that produced greatest comfort. This amount of heel lift was then added to the undersurface of the foot orthosis for the shorter lower extremity. Custom filling of the arch space was provided for all subjects, and a metatarsal pad was placed if the subject reported that the plantar surface of 1 or more metatarsal heads was experiencing uncomfortable pressure after initial fitting of the orthoses (during the second test session). Subjects’ structural exam characteristics and the construction features of their foot orthoses were recorded (TABLE 1).
TABLE 1 –
Subjects’ structural and foot orthotic characteristics
| Subject | Exam Characteristics | Foot Orthotic Architecture* |
|---|---|---|
| 1 | Neutral foot, callus left 2nd metatarsal head | Metatarsal pad |
| 2 | Forefoot varus, limited ankle dorsiflexion | Medial forefoot post, heel lift |
| 3 | Forefoot varus | Medial forefoot post |
| 4 | Forefoot varus, limited ankle dorsiflexion | Medial forefoot post, heel lift |
| 5 | Neutral foot. | Orthoses with no corrective features |
| 6 | Forefoot Equinus, cavus, limited ankle dorsiflexion | Heel lift |
| 7 | Cavus foot, limited ankle dorsiflexion | Heel lift |
| 8 | Neutral foot | Orthoses with no corrective features |
| 9 | Forefoot varus, limited ankle dorsiflexion | Medial forefoot post, heel lift |
| 10 | Tibial varum | Medial rearfoot post |
| 11 | Forefoot varus, 1.125 mm (3/8 in) limb length inequality | Medial forefoot post, 1.125 mm heel lift correction |
| 12 | Forefoot varus, limited ankle dorsiflexion | Medial forefoot post, heel lift |
| 13 | Forefoot varus, limited ankle dorsiflexion | Medial forefoot post, heel lift |
All foot orthoses had a custom filling-in of the arch space.
The subject returned to the testing site approximately 2 weeks following the first testing session (FIGURE 1). Prior to trying their foot orthoses, the subjects completed all of the balance tests (PRE) to determine how stable their performance was on these measures compared with the screening exam tests (SCREEN). Then the subjects were provided their foot orthoses and were asked to walk for several minutes with the foot orthoses in their shoes to determine if any adjustments needed to be made to address comfort issues. Once the subject reported that the foot orthoses were comfortable, testing of all balance measures was repeated (POST) to determine if there was any immediate effect of the intervention. Subjects were asked to wear their foot orthoses as much as possible between the end of this session and the final testing session. Subjects completed a daily log to report the estimated number of hours that the foot orthoses were worn. They also were asked to contact the principal investigator immediately if any discomforts arose from wearing the foot orthoses so that modification of the orthoses could be made as needed.
The subject returned to the test facility for the third and final testing session approximately 2 weeks following the second testing session (FIGURE 1). Testing on all balance measures was repeated for the last time (FU). Daily orthotic wear logs were collected. Each subject also was asked to report any adverse experiences from wearing the foot orthoses.
Data Analysis
Descriptive statistics were generated for the subjects and aspects of their participation in the study. An analysis for normality using the Kolmogorov-Smirnov test indicated that the data for 2 of the 4 balance measures were not normally distributed at some of the times of measurement (TABLE 2). This analysis, combined with the low number of subjects, prompted the use of nonparametric data analyses. The data for SCREEN and PRE measurement sessions were compared for test-retest stability by computing median absolute differences and using the Friedman’s rank test for correlated samples (alpha =.05). The Friedman’s rank test was also used to determine if subject performance was significantly different across the following 3 times of measurement: pre-intervention assessment during the second test session (PRE), post-intervention assessment during the second test session (POST), and the follow-up assessment during the third test session (FU). Post-hoc testing to determine which pairwise contrasts were significantly different was also accomplished with the Friedman’s rank test with Bonferroni correction using an alpha level of 0.017. Raw data were stored in Microsoft Excel (Redmond, WA) and all statistical analyses were conducted using SAS Statistical Software (Cary, NC).
TABLE 2 –
Descriptive Statistics for Balance Measures*
| Time of Measurement | One-Leg Stance Test (secs) | Tandem Stance Test (secs) | Tandem Gait Test (steps) | Step Test (steps) | |
|---|---|---|---|---|---|
| SCREEN | Median | 3.3 | 15.8 | 1.0 | 14.7 |
| IQR | 2.2 – 4.0 | 9.3 – 18.1 | 0.3 – 1.7 | 12.7 – 17.7 | |
| K-S | P = .777 | P = .874 | P = .252 | P = .547 | |
| PRE | Median | 3.8 | 13.3 | 0.7 | 16.3 |
| IQR | 2.2 – 4.5 | 11.7 – 27.4 | 0.0 – 3.0 | 14.0 – 20.0 | |
| K-S | P = .133 | P = .025 | P = .003 | P = .556 | |
| POST | Median | 8.1 | 25.3 | 2.7 | 18.7 |
| IQR | 4.1 – 15.3 | 19.0 – 29.9 | 1.3 – 7.0 | 16.0 – 21.0 | |
| K-S | P = .057 | P = .264 | P = .001 | P = .986 | |
| FU | Median | 6.1 | 24.2 | 2.3 | 19.0 |
| IQR | 3.6 – 12.4 | 16.5 – 28.1 | 1.7 – 4.7 | 16.7 – 23.0 | |
| K-S | P = .232 | P = .437 | P = .049 | P = .546 |
SCREEN = assessment at first screening visit, PRE = pre-intervention assessment at second visit, POST = post-intervention assessment at second visit, and FU = follow-up assessment at third visit. IQR = interquartile range and K-S = Kolmogorov-Smirnov test for normal distribution.
RESULTS
Seven women and 6 men with mean ± SD age of 81.4 ± 5.9 (range = 70–90) years participated in the study. The 7 women in the study had a mean ± SD height of 159.1 ±7.6 cm and a mass of 63.1 ± 10.9 kg. The 6 men in the study had a mean ± SD height of 178.1 ± 4.6 cm and a mass of 88.0 ± 11.4 kg. The mean ± SD number of correct responses on the Six-Item Screener test for intact cognition was 5.7 ± 0.4. Mean ± SD number of falls during the past year was 11.2 ± 28.2 (range 1–104). Most subjects reported falling fewer than 4 times during the preceding year, but 2 subjects reported falling approximately once a month and 1 subject reported falling approximately twice a week. Subjects reported wearing their foot orthoses an average ± SD of 10.2 ±4.0 hours per day after being fitted during the second testing session. The number of days between the first 2 testing sessions was 16.2 ± 4.6 days, and the number of days between the last 2 testing sessions was 14.4 ±1.3 days. Subject characteristics identified during the structural alignment examination, as well as the architectural features of the subjects’ foot orthoses are detailed in TABLE 1. One subject returned for a slight modification of her orthoses (pressure relief). No other adverse consequences from foot orthotic use were reported by subjects.
Median, interquartile range, and normality values for the 4 balance measures for the 4 times of measurement are provided in TABLE 2. The data for all balance tests between SCREEN and PRE measurements were statistically equivalent (P > .05; TABLE 3). Median and interquartile range values for the absolute difference between paired SCREEN and PRE values are presented in TABLE 3. The initial Friedman’s rank test analysis indicated that significant differences (P < .05) existed across the PRE, POST, and FU times of measurement for the 4 balance measures (TABLE 4 and FIGURES 2–5). Post-hoc analyses indicated that POST and FU measures were statistically equivalent (P > .017) for the 4 balance measures (TABLE 4 and FIGURES 2–5). With 1 exception, the POST and FU measurements were significantly greater than the PRE measurements for all variables (P < .017). Although the median value for the tandem gait test at the POST time of measurement (2.7 steps) was more than 3 times greater than the median value at the PRE time of measurement (0.7 steps), this difference was not considered statistically significant (P = .034) based on our adjusted alpha level of 0.017.
TABLE 3 –
Stability Analyses between SCREEN and PRE Data
| One-Leg Stance Test (secs) | Tandem Stance Test (secs) | Tandem Gait Test (steps) | Step Test (steps) | ||
|---|---|---|---|---|---|
| Absolute Differences | Median | 0.4 | 3.4 | 1.3 | 2.0 |
| Between SCREEN And PRE Data | IQR | 0.2 – 1.2 | 0.5 – 11.4 | 0.7 – 1.7 | 0.7 – 2.7 |
| Friedman’s Rank Test (df = 1) | χ 2F = 1.92 | χ 2F = 0.08 | χ 2F = 0.00 | χ 2F = 3.00 | |
| Comparing SCREEN and PRE Data | P = .166 | P = .782 | P = 1.000 | P = .083 | |
SCREEN = assessment at first screening visit, PRE = pre-intervention assessment at second visit, POST = post-intervention assessment at second visit, and FU = follow-up assessment at third visit. IQR = interquartile range.
TABLE 4 –
Nonparametric Test Results for Balance Measures
| One-Leg Stance Test (secs) | Tandem Stance Test (secs) | Tandem Gait Test (steps) | Step Test (steps) | ||
|---|---|---|---|---|---|
| Friedman’s Rank Test (df = 2) | χ 2F = 11.69 | χ 2F = 11.39 | χ 2F = 8.00 | χ 2F = 17.43 | |
| Comparing PRE, POST, and FU | P = .003 | P = .003 | P = .018 | P = .001 | |
| Post-hoc Friedman’s Rank Test | PRE vs POST | χ 2F = 9.31 | χ 2F = 6.23 | χ 2F = 4.45 | χ 2F = 19.31 |
| P = .002 | P = .013 | P = .034 | P = .002 | ||
| PRE vs FU | χ 2F = 6.23 | χ 2F = 6.23 | χ 2F = 7.36 | χ 2F = 12.00 | |
| P = .013 | P = .013 | P = .007 | P = .001 | ||
| POST vs FU | χ 2F = 0.08 | χ 2F = 3.60 | χ 2F = 0.08 | χ 2F = 2.27 | |
| P = .782 | P = .058 | P = .782 | P = .132 | ||
SCREEN = assessment at first screening visit, PRE = pre-intervention assessment at second visit, POST = post-intervention assessment at second visit, and FU = follow-up assessment at third visit. IQR = interquartile range.
FIGURE 2.
One-leg stance time (n = 13). Values represent median ± interquartile range. PRE = pre-intervention assessment at second visit, POST = post-intervention assessment at second visit, and FU = follow-up assessment at third visit. Values are significantly different (P = 0.003) across the 3 times of measurement. Brackets indicate significant pairwise contrasts with Bonferroni correction.
FIGURE 5.
Number of steps (median ± interquartile range) for alternating step test (n = 13). PRE = pre-intervention assessment at second visit, POST = post-intervention assessment at second visit, and FU = follow-up assessment at third visit. Values are significantly different (P = 0.001) across the 3 times of measurement. Brackets indicate significant pairwise contrasts with Bonferroni correction.
DISCUSSION
The results of this study provide preliminary evidence that custom foot orthoses can effect improvement in static and dynamic measures of balance for older adults with balance impairments and a history of unexplained falls. In most cases, these improvements were seen immediately after foot orthotic intervention and were maintained 2 weeks following the intervention.
We specifically recruited a sample of older adults who might be representative of individuals at risk for falls. Our subjects reported at least 1 fall during the year prior to enrollment in the study, indicating they could be classified as “fallers” who were at increased risk for additional falls simply because of their age and because of a history of a previous fall.43 We acknowledge that our subjects represent a biased sample and that other subject characteristics that we did not control may be related to risk for falling. The subjects’ inability to stand in one-leg stance for more than 5 seconds also suggests they were at risk for an injurious fall.43 Two normative studies indicate mean ± SD times for the one-leg stance test as 13.08 ± 11.1 seconds8 and 21.43 ± 10 seconds44 for samples of older adults in the eighth decade of life. Our subjects were only able to take fewer than 2 steps prior to the intervention for the tandem gait test, compared with 6.43 ± 3.1 steps8 and 14.1 ± 7 steps44 for samples of older adults in the eighth decade of life. Taken together, these data indicate our subjects had balance impairments and were at increased risk for falls.
Each balance measure was statistically equivalent between the SCREEN and PRE measurements and the median absolute differences between SCREEN and PRE measurements were relatively small in magnitude, indicating the stability of our balance measures prior to foot orthotic intervention. We selected our 4 outcome measures because we thought they would pose varying levels of difficulty for our subjects and because they represented both static and dynamic challenges to balance. Kornetti et al18 have documented that 3 of the measures we used (one-leg stance, tandem stance, and alternating step test) could be helpful in differentiating individuals who would be considered fallers versus non-fallers for their overall score on the Berg Balance Scale. The one-leg stance test and the tandem stance test represent static balance performance measures. The alternating step test and the tandem gait test, however, both require that the subject be able to maintain stable balance on 1 lower extremity while other body segments move through space and change the subject’s center of mass positions. Anecdotally, all of our subjects reported that the tandem gait task was the most challenging of the 4 physical performance measures included in the study. As an indicator of the difficulty of this test, 6 of our 13 subjects were unable to take a single step during their attempted performance of the tandem gait test either during the SCREEN or PRE testing sessions.
Foot orthotic intervention had an immediate significant effect on improving subjects’ balance performance for 3 of the 4 balance performance measures. The only balance measure for which this was not the case was the tandem gait test. Although not statistically significant, the median number of steps subjects took for this test during the POST time of measurement (2.7) was more than 3 times the number of steps taken during the PRE time of measurement (0.7). The FU measurements for all balance measures were statistically equivalent to the POST measurements and significantly improved compared with the PRE measurements. These results suggest that the foot orthotic intervention generally had an immediate effect in improving balance performance that was sustained at the time of the FU measurements. The follow-up period for testing in this study was relatively short. Additional research is needed to determine if the positive influence of the foot orthoses on balance can be maintained over longer periods of time and lead to improvement in functional mobility and reduction of falls.
Because very limited evidence is available regarding the effects of foot orthoses and foot inserts on balance, the authors must speculate on the theoretical mechanism by which these devices influence human balance. Two of our subjects had rigid, supinated feet. These feet tend to have less plantar surface area of the foot in contact with the ground, thereby decreasing the base of support of the individual. Additionally, less motion is available throughout the joints of the foot to respond to perturbations in balance. Although the latter issue is not really addressed by foot orthoses, a custom filling in of the individual’s arch space with a custom foot orthosis increases the base of support between the contact surface and the plantar surface of the foot. Additionally, 7 of our subjects had limited ankle dorsiflexion and 1 of these subjects presented with forefoot equinus. Both musculoskeletal conditions tend to exert a posteriorly directed pull on the posterior leg as the ankle joints move into dorsiflexion. We addressed what we thought was a destabilizing influence in each of these cases by providing slight heel lift for these 7 subjects. Menz et al23 have supported this line of reasoning by documenting that reduced ankle flexibility was associated with poorer standing and leaning balance. The pronated foot is generally considered a hypermobile, unstable foot.6,14 The primary issues that we detected and thought were causing pronation were tibial varum, forefoot varus, and limited ankle dorsiflexion. We addressed these issues with medial rearfoot posting, medial forefoot posting, and heel lift, respectively, in an attempt to decrease the excessive pronation we qualitatively detected.
This research represents a relatively small pilot study and has a number of limitations. Although subjects wore the same shoes for all 3 test sessions, subjects all wore their own shoes and we did not control for shoe type other than asking subjects to wear laced athletic or walking shoes that they wore most of the time. We should note that light contact was made with the subjects during all balance testing by maintaining contact with the safety belt that they wore. This could have provided biased feedback during balance tests. Although visual acuity was assessed, other visual measures such as ambient peripheral vision, as well as measures of sensation, muscle performance, proprioception, and reaction time were not assessed. All of these factors may have had influence on the balance capability of our subjects. Additionally, our study did not include a control group or other comparison group, which limits the strength of the data in terms of clinical implications. We did not provide a practice period for any of the balance measures, but assessed the stability of our measures by performing assessment of each of the 4 balance measures on 2 separate occasions prior to foot orthotic intervention. Statistical analysis of these data indicated the measures were stable prior to the intervention.
One of the issues associated with custom foot orthotic intervention is the cost of these appliances. Future investigations could assess the efficacy of this intervention more completely, including the savings that may result from prevention of falls and the medical costs related to treatment of falls. These data could then be used to evaluate the efficacy of custom foot orthoses or non-custom arch supports that are appreciably less expensive than custom appliances. Finally, we are unable to say whether the statistically significant improvement we observed in the balance performance from foot orthotic intervention would translate into clinically meaningful differences such as reduced number of falls.
CONCLUSION
We observed immediate improvements in static and dynamic measures of balance in older adults following the placement of custom foot orthoses in their laced walking/athletic shoes. These improvements were maintained at 2 weeks following the intervention.
FIGURE 3.
Tandem stance time (n = 13). Values represent median ± interquartile range. PRE = pre-intervention assessment at second visit, POST = post-intervention assessment at second visit, and FU = follow-up assessment at third visit. Values are significantly different (P= 0.003) across the 3 times of measurement. Brackets indicate significant pairwise contrasts with Bonferroni correction.
FIGURE 4.
Number of steps (median ± interquartile range) for tandem gait test (n = 13). PRE = pre-intervention assessment at second visit, POST = post-intervention assessment at second visit, and FU = follow-up assessment at third visit. Values are significantly different (P = 0.018) across the 3 times of measurement. Brackets indicate significant pairwise contrasts with Bonferroni correction.
KEY POINTS.
Findings
The results of this study provide preliminary evidence that custom foot orthoses can effect improvement in static and dynamic measures of balance for older adults with balance impairments. In most cases, these improvements were seen immediately after foot orthotic intervention and were maintained 2 weeks following the intervention.
Implication
Clinicians may wish to consider custom foot orthotic intervention for older adults with balance impairments who are at risk for falls.
Caution
Additional studies are needed that involve control groups, blinding of investigators, longer follow-up, inclusion of mobility measures, and monitoring incidence of falls to justify widespread application of these findings.
Acknowledgments
This research was supported by Award Number UL1RR025747 from the National Center for Research Resources
The study protocol for this work was approved by the Biomedical IRB of the Office of Human Research Ethics at the University of North Carolina at Chapel Hill, Chapel Hill, NC.
The authors assert that they have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript, except as cited in the manuscript.
References
- 1.Arnadottir SA, Mercer VS. Effects of footwear on measurements of balance and gait in women between the ages of 65 and 93 years. Phys Ther. 2000;80(1):17–27. [PubMed] [Google Scholar]
- 2.Callahan CM et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40(9):771–781. [DOI] [PubMed] [Google Scholar]
- 3.Campbell AJ, Borrie MJ, Spears GF, et al. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing. 1990;19:136–141. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Web-based injury statistics query and reporting system (WISQARS). URL: www/cdc.gov/ncipc/wisqars 2003 [National Center for Injury].
- 5.Cobb SC, Tis LL, Johnson JT. The effect of 6 weeks of custom-molded foot orthosis intervention on postural stability in participants with ≥ 7 degrees of forefoot varus. Clin J Sport Med. 2006;16(4):316–322. [DOI] [PubMed] [Google Scholar]
- 6.Donatelli RA. Normal anatomy and biomechanics. In: Donatelli RA, ed. The Biomechanics of the Foot and Ankle. Philadelphia, PA: F.A. Davis Company;1996;3–33. [Google Scholar]
- 7.Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol A Biol Sci Med Sci. 1990;45:M192–7. [DOI] [PubMed] [Google Scholar]
- 8.Giorgetti MM, Harris BA, Jette A. Reliability of clinical balance outcome measures in the elderly. Physiother Res Internat. 1998;4(4):274–283. [DOI] [PubMed] [Google Scholar]
- 9.Gregg EW, Pereira MA, Caspersen CJ. Physical activity, falls, and fractures among older adults: a review of the epidemiologic evidence. J Am Geriatr Soc. 2000;48:883–893. [DOI] [PubMed] [Google Scholar]
- 10.Gross MT: Lower quarter screening for structural malalignment- Suggestions for orthotics and shoewear. J Orthop Sports Phys Ther. 1995;21:389–405. [DOI] [PubMed] [Google Scholar]
- 11.Horgan NF, Crehan F, Bartlett E, et al. The effects of usual footwear on balance amongst elderly women attending a day hospital. Age Ageing. 2009;38(1):62–67. [DOI] [PubMed] [Google Scholar]
- 12.Horak FB. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing. 2006;35 Suppl 2:ii7-ii11. [DOI] [PubMed] [Google Scholar]
- 13.Horak FB, Nashner LM. Central programming of postural movements: Adaptation to altered support-surface configurations. J Neurophysiol. 1986;55(6):1369–1381. [DOI] [PubMed] [Google Scholar]
- 14.Hunt GC, Brocato RS. Gait and foot pathomechanics. In: Hunt GC, ed. Physical Therapy of the Foot and Ankle. New York, NY: Churchill Livingstone; 1988:39–57. [Google Scholar]
- 15.Isles RC, Choy NLL, Steer M, Nitz JC. Normal values of balance tests in women aged 20–80. J Am Geriatr Soc. 2004;62(8):1367–1372. [DOI] [PubMed] [Google Scholar]
- 16.Johnston LB, Gross MT: Effects of foot orthoses on quality of life for individuals with patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2004;34(8):440–448. [DOI] [PubMed] [Google Scholar]
- 17.Koepsell TD, Wolf ME, Buchner DM, et al. Footwear style and risk of falls in older adults. J Am Geriatr Soc. 2004;52(9):1495–1501. [DOI] [PubMed] [Google Scholar]
- 18.Kornetti DL, Fritz SL, Chiu Y-P et al. Rating scale analysis of the Berg Balance Scale. Arch Phys Med Rehabil. 2004;85:11–28-1135. [DOI] [PubMed] [Google Scholar]
- 19.Lamb SE et al. Development of a common outcome data set for fall injury prevention trials: The prevention of falls network Europe (ProFaNE) consensus. J Am Geriatric Soc. 2005;53:1618–162. [DOI] [PubMed] [Google Scholar]
- 20.Lord SR, McLean D, Stathers G. Physiological factors associated with injurious falls in older people living in the community. Gerontol. 1992;38(6):338–46. [DOI] [PubMed] [Google Scholar]
- 21.Lord SR, Sherrington C, Menz HB. Falls in Older People: Risk Factors and Strategies for Prevention. Cambridge: Cambridge University Press, 2000. [Google Scholar]
- 22.Menant JC, Perry SD, Steele JR, et al. Effect of shoe characteristics on dynamic stability when walking on even and uneven surfaces in young and older people. Arch Phys Med Rehabil 2008;89(10):1970–1976. [DOI] [PubMed] [Google Scholar]
- 23.Menz HB, Morris ME, Lord SR. Foot and ankle characteristics associated with impaired balance and functional ability in older people. J Gerontol A Biol Sci Med Sci. 2005;60(12):1546–52. [DOI] [PubMed] [Google Scholar]
- 24.Menz HB, Morris ME, Lord SR. Footwear characteristics and risk of indoor and outdoor falls in older people. Gerontology. 2006;52(3):174–180. [DOI] [PubMed] [Google Scholar]
- 25.Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: A prospective study. Phys Ther. 2008;88(4):449–459. [DOI] [PubMed] [Google Scholar]
- 26.Mulford C, Taggart HM, Nivens A, Payne C. Arch support use for improving balance and reducing pain in older adults. Appl Nurs Res. 2008;21:153–158. [DOI] [PubMed] [Google Scholar]
- 27.Murphy SL. Deaths: final data for 1998. National vital statistics reports, vol. 48, no. 11. Hyattsville (Md)7 National Center for Health Statistics; 2000. [PubMed] [Google Scholar]
- 28.Nashner LM. Adapting reflexes controlling the human posture. Exp Brain Res. 1976;26(1):59–72. [DOI] [PubMed] [Google Scholar]
- 29.Ochsendorf DT, Mattacola CG, Arnold BL. Effect of orthotics on postural sway after fatigue of the plantar flexors and dorsiflexors. J Athl Train. 2000;35(1):26–30. [PMC free article] [PubMed] [Google Scholar]
- 30.Overstall PW, Exton-Smith AN, Imms FJ, Johnson AL. Falls in the elderly related to postural imbalance. Br Med J. 1977;1:261–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perry SD, Radtke A, McIlroy WE, et al. Efficacy and effectiveness of a balance-enhancing insole. J Gerontol A Biol Sci Med Sci. 2008;63(6):595–602. [DOI] [PubMed] [Google Scholar]
- 32.Priplata AA, Niemi JB, Harry JD et al. Vibrating insoles and balance control in elderly people. Lancet. 2003;362:1123–1124. [DOI] [PubMed] [Google Scholar]
- 33.Priplata AA, Patritti BL, Niemi JB, et al. Noise-enhanced balance control in patients with diabetes and patients with stroke. Ann Neurol. 2006;59:4–12. [DOI] [PubMed] [Google Scholar]
- 34.Sattin RW, Lambert DA, DeVito CA, et al. The incidence of fall injury events among the elderly in a defined population. Am J Epidemiol. 1990;131:1028–37. [DOI] [PubMed] [Google Scholar]
- 35.Shubert TE, Schrodt LA, Mercer VS, Busby-Whitehead J, Giuliani CA. Are scores on balance screening tests associated with mobility in older adults? J Geriatr Phys Ther. 2006;29(1):35–39. [PubMed] [Google Scholar]
- 36.Sherrington C, Menz HB. An evaluation of footwear worn at the time of fall-related hip fracture. Age Ageing. 2003;32(3):310–314. [DOI] [PubMed] [Google Scholar]
- 37.Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma Inj Infect Crit Care. 2001;50:116–9. [DOI] [PubMed] [Google Scholar]
- 38.Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and nonfatal falls among older adults. Injury Prevention. 2006;12:290–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tencer AF, Koepsell TD, Wolf ME, et al. Biomechanical properties of shoes and risk of falls in older adults. J Am Geriatr Soc. 2004;52(11):1840–1846. [DOI] [PubMed] [Google Scholar]
- 40.Thomas JI, Lane JV. A pilot study to explore the predictive validity of 4 measures of falls risk in frail elderly patients. Arch Phys Med Rehabil. 2005;86:1636–40. [DOI] [PubMed] [Google Scholar]
- 41.Tinetti ME, Baker DI, McAvay G, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331:821–827. [DOI] [PubMed] [Google Scholar]
- 42.Toulotte et al. : Identification of healthy elderly fallers and non-fallers by gait analysis under dual-task conditions. Clin Rehab. 2006;20(3):269–276. [DOI] [PubMed] [Google Scholar]
- 43.Vellas BJ et al. One-leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc. 1997;45(6):735–8. [DOI] [PubMed] [Google Scholar]
- 44.Vereeck L, Wuyts F, Truijen S, Van de Heyning P. Clinical assessment of balance: Normative data, and gender and age effects. Internat J Audiology 2008;47:67–75. [DOI] [PubMed] [Google Scholar]
- 45.Weigelt JA. Trauma. In: Advanced Trauma Life Support for Doctors: ATLS. 6th ed. Chicago: American College of Surgeons, 1997, 26. [Google Scholar]