Highlights
-
•
Digital physical therapy may be a solution for continuity during lockdown, yet its development appears complex.
-
•
Implementation difficulties seem to relate to physical, attentional, and training factors.
-
•
Technological accessibility, adaptation of the therapist and involvement of the whole family appear to be facilitators.
-
•
Future possibilities may support a better follow-up with fluid communication between families and therapists.
Keywords: COVID-19, Early intervention, Physical therapy modalities, Qualitative research, Telehealth
Abstract
Background
Digital physical therapy was performed within early intervention sessions for children with developmental disorders during the COVID-19 pandemic. There is no known qualitative study that addresses the perspectives of parents with digital practice for early intervention.
Objective
To describe the parents' experiences with digital physical therapy for early intervention in children during COVID-19 lockdown.
Methods
A qualitative phenomenological study. Purposive sampling was conducted, including 16 parents of the children participating in the early intervention program. Data were collected through semi-structured interviews and researchers' field notes. An inductive analysis was performed.
Results
Four themes emerged: a) ambivalent experiences about digital physical therapy: telehealth can be a good solution in times of COVID-19, however, it was also perceived as difficult and insufficient; b) barriers encountered for its implementation: describing factors related to physical aspects, training, and time, and difficulties maintaining the child's attention; c) perceived facilitators during its use: based on digital accessibility, availability, and adaptability of the therapist and the rest of the family; d) future possibilities of digital physical therapy: suggested uses for after the lockdown, such as a complement that facilitates communication and as a follow-up with older children.
Conclusions
Our findings help shed light on the possible benefits of digital physical therapy in children with developmental disorders, considering the perspectives of families. However, there are several difficulties to be overcome to successfully implement this type of therapy and optimize its future possibilities.
Introduction
Early intervention (EI) programs are understood as the group of services, such as physical therapy, aimed at young children from 0 to 6 years old, their families, and their close environment. The objective of EI services is to respond as soon as possible to the needs of children with developmental disorders (i.e., motor, cognitive, sensory, or language developmental disorders) or who are at risk for such disorders (developmental delay).1
The goals of physical therapy in EI are: primary prevention, informing the general population about motor development and warning signs; and secondary and tertiary prevention, through quantitative and qualitative assessment, intervention, training, and research.2 In recent years, therapeutic interventions in pediatrics have been oriented towards everyday settings (homes, infant schools, care services, or playgrounds).3 This implies a paradigm shift, progressively transforming from a child-centered model to a type of intervention in which the child, the family, and the environment are actively involved.4,5
From March 12, 2020, EI Centers in Spain were closed due to Covid-19.6,7 In addition, mandatory home lockdown was implemented for all persons, with the exception of essential services.8 In those families in which a child had motor impairments or was at risk due to developmental disorders, this situation may have had an even greater impact due to increased levels of stress, depression,9 and family concern.10 The absence of rehabilitation can lead to soft tissue contractures, bone deformities, regression in motor milestones, dysphagia, and respiratory difficulties, etc.11
The COVID-19 lockdown has also had a major impact on physical therapy services worldwide,12 especially in the care of chronically ill patients12 and parents of children with physical disabilities who experienced a major interruption of rehabilitation services.13 Consequently, the World Physiotherapy organization12 proposed that investment in and recognition of digital physical therapy practice (synchronous and asynchronous delivery) could be an effective way to address the challenges and needs of the population to access the services of physical therapists. Digital practice was included as a modality for conducting EI sessions using communication technologies, favoring access to the virtual home in real time to optimize the monitoring of functional objectives.14,15
Following the COVID-19 lockdown, numerous studies have examined telehealth services in pediatrics including children under six years of age with motor impairments.16, 17, 18 A recent systematic review focusing on telehealth in children with neurodevelopmental disorders19 concluded that the services offered were equivalent to or better than face-to-face services and were a potential emerging resource. Questionnaires have also been used to gage caregivers' satisfaction and perceptions regarding this intervention, suggesting possibilities for the future.20,21 In addition, guidelines have been developed,22, 23, 24 complementing those existing to date25 and supporting all professionals in this field with new innovative strategies. Rosenbaum et al.26 suggested that telehealth could continue to be a treatment alternative after the pandemic is over because it provides the ability to see children in their natural environments.26
To date, there is no known qualitative study that addresses the perspectives of parents on digital practice in EI. Therefore, the aim of this study was to describe the experience of parents when using digital physical therapy for children in EI during the COVID-19 lockdown.
Methods
Design
A descriptive phenomenological approach was used27, 28, 29 based on Husserl's framework.30,31 In the field of qualitative studies, phenomenology attempts to understand other people's lived experiences.32 The aim of phenomenology is the study of phenomena as they appear to arrive at an essential understanding of human experience.31 To consider subjective experiences, the researcher assumes a certain attitude of attentive openness and readiness for a proper understanding of the unique meaning of participants’ lived experiences.30,31 This experience always has a meaning for the person who has undergone the same, and thus, phenomenological research uses first-person narratives from the participants themselves as a data source.30 The study followed the Standards for Reporting Qualitative Research (SRQR)33 and the Consolidated Criteria for Reporting Qualitative Research (COREQ).34 In accordance with the SRQR33 and COREQ34 criteria, the description of the research team and reflexivity35 have been included in Supplementary Material 1. This study was approved by the Ethics Committee of CEU San Pablo University (code 467/20/TFM) and by the management of the EI Center where the study was conducted (www.citocentro.org).
Participant recruitment
A purposive sampling method was used to recruit parents who had experience with the application of digital physical therapy to children in EI.36 Sampling and data collection continued until the ongoing analysis revealed information redundancy, at which point no new information emerged from the data analysis.36 Extended information about the recruitment process is shown in Supplementary Material 2. No parents withdrew from the study.
The inclusion criteria were: 1) parents of children, irrespective of their developmental disorder diagnosis; 2) integrated within the EI service at the time of COVID-19 lockdown; 3) who had received a minimum of five digital physical therapy sessions during the lockdown period (from 12 March to June 2020); 4) and who agreed to participate in the study after signing the informed consent form.
Data collection
Based on the phenomenological design of this study, first person data collection tools (in-depth interviews) and researcher's field notes were used.30 Semi-structured interviews were conducted using open-ended questions to capture the lived experience of each participant (Table 1).32,36 The question guide was developed based on a literature review and previous experiences of researchers. Subsequently, the researchers listened carefully, noting the key words and topics identified in the participants’ responses and using their answers to ask further questions for clarification. In this manner, relevant information was collected from the participants’ perspective.35 In addition, during the face-to-face interviews, researchers used prompts: (a) to encourage participants to provide more details, (b) to encourage participants to continue talking, and (c) to resolve confusion. The interviews were conducted during the month of March 2021 by 1 of the investigators (A.C-B.) through the Zoom platform (www.zoom.us), San Diego, CA, USA).37 Permission to record the audio and video was obtained from the participants using an informed digital consent form. To guarantee confidentiality, each participant was assigned an alpha-numeric code. During the interviews, data collection was complemented by researcher field notes.
Table 1.
Semi-structured interview question guide.
| Aspects to be researched | Questions to ask in the field |
|---|---|
| The meaning of digital physical therapy | What does digital physical therapy mean to you? How would you define or explain this intervention according to your lived experience? |
| Knowledge and accessibility to technology | Before lockdown, what was your knowledge about the different ways or means of performing online physical therapy? How was your accessibility to the means necessary for the use of technology? What means were available to you? What devices and apps have you used? |
| Adaptation to change | How did you experience the process of switching to online therapy? What about the rest of the family? What about your child?" How did you feel about the physical therapist's adaptation and involvement in relation to this change? |
| Experiences | What were the digital physical therapy sessions like? What feelings surfaced for you during these sessions? "And after them? What has digital physical therapy done for you? What aspects made it relevant for you to do? What do you think has been the benefit of participating in these sessions? In what aspects of the child have you noticed changes? |
| Attitude towards technology | How do you currently conduct physical therapy sessions? What means do you use? What is your experience regarding the use/maintenance of digital practice in the physical therapy setting? |
| Needs of the family | What are your current needs in relation to your child? What do you think your physical therapist can help you with? What would you consider to be the ideal form of treatment and accompaniment in physical therapy? What is most relevant to you? |
Data analysis
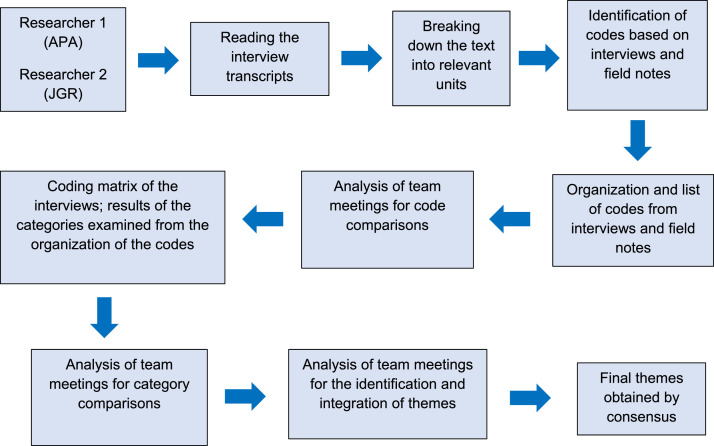
All interviews were transcribed verbatim (A.P-A.) and supplemented with the researchers' field notes. Subsequently, the interview transcript was sent by e-mail to each participant so that they could add or clarify any aspect they considered appropriate. Finally, an inductive analysis was performed by two researchers (A.P-A., J.G-R),35,38 consisting of successive reading and fragmentation of the participants' narratives, with representative codes being assigned independently by each researcher, which were then categorized into the different themes by consensus (Fig. 1). No qualitative data analysis software was employed. For the analysis, the Microsoft Excel ® program was used to organize and share the coding process.
Fig. 1.
Inductive analysis process. Phases of the inductive analysis process from the independent reading of the transcripts by each researcher, to the final themes obtained by consensus.35,38
Rigor and trustworthiness
To ensure the rigor and methodological quality of this study, the Lincoln and Guba Trustworthiness Criteria39 for Credibility, Transferability, Dependability or Consistency, and Confirmability were followed (Table 2).
Table 2.
Trustworthiness criteria.
| Criteria | Techniques and application procedures |
|---|---|
| Credibility | Researcher triangulation: each interview was analyzed by two researchers. Subsequently, team meetings were held in which the analyses were compared, and themes were identified. Triangulation of participants: the study included participants with different diagnoses, however, all required digital practice. Thus, multiple perspectives were obtained with a common link (the digital physical therapy experience). Triangulation of data collection methods: semi-structured interviews were conducted, and field notes were taken by the researcher. Participant validation: this consisted of asking participants to confirm the data obtained during the data collection and analysis phases. |
| Transferability | In-depth descriptions of the study were made, providing details on the characteristics of the researchers, the participants, the context, the sampling strategies, and the data collection and analysis procedures. |
| Dependence or consistency |
Exhaustive description of the analysis process performed. Researcher triangulation. |
| Confirmability | Researcher triangulation, participant triangulation, data collection triangulation. Researcher reflexivity was encouraged through reflective reporting and description of the rationale for the study. |
Results
In total, 15 families (16 participants) participated in this study. The 16 participants, mean age 41 ± 4.9 years, were parents (15 mothers and one father). Both the father and the mother were invited to participate, however M6 and F6 were the only family where both parents agreed to participate. The 15 children (six girls and nine boys), mean age 3.43 ± 1.2 years, had different diagnoses. The characteristics of the parents and children are shown in Supplementary Material 3 and 4, respectively.
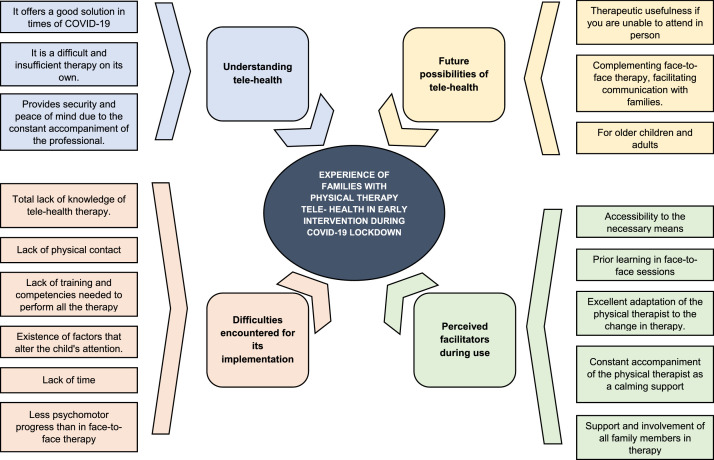
Based on the 43 categories and 17 sub-themes that emerged, four main themes were identified: a) ambivalent experiences about digital physical therapy; b) barriers encountered for its implementation; c) perceived facilitators during use; d) future possibilities. Fig. 2 shows the conceptual map of the study findings. A detailed summary of the themes, subthemes, and categories is provided in Supplementary Material 5. For illustrating quotes, see Supplementary Material 6.
Fig. 2.
Conceptual map of the study findings. Conceptual map reflecting the experience of parents with physical therapy telehealth in early intervention of their children during COVID-19 lockdown.
Ambivalent experiences about digital physical therapy
The first theme describes the significance of digital practice for families who experienced this physical therapy service in EI during COVID-19 lockdown. Participants reported that digital practice appeared to be a good solution given the impossibility of face-to-face treatment, which offered them the opportunity to continue their child's treatment during lockdown.
In addition, they appreciated the monitoring by the digital physical therapists as a guide who supported and helped them to identify progress or setbacks in the evolutionary development of their children.
The experience of the lockdown together with the application of digital practice during the session generated many different emotions among the participants. Parents felt accompanied by the physical therapists, who were able to resolve doubts quickly through fluid communication and gave them the opportunity to feel happy and fulfilled as parents when performing the session with their children.
In addition, some participants also felt insecure during these sessions, perceiving the digital physical therapy practice as complicated and, at times, insufficient, which, together with the stress of lockdown, led to feelings of discomfort.
Barriers for its implementation
Participants described different barriers they encountered during the sessions. First, the total lack of knowledge regarding digital physical therapy, as it was a modality which was never offered or deemed necessary prior to the pandemic.
Along with the initial lack of knowledge, participants described several fundamental factors that impacted the treatment of their children through digital practice. These included the lack of physical contact and the lack of training and skills necessary to develop the therapy, feeling that they did not have the necessary knowledge and resources, having to perform the work of a physical therapist without training or experience, and assuming a change of role during the sessions, as they went from parents to physical therapists.
In addition, participants described the existence of distractors that altered the child's attention and the lack of time as barriers to the implementation of digital physical therapy. Among the factors that distracted their attention, they identified that the children's attitude was different as they felt that both the therapy and their daily routines had been altered. Participants also observed that the children became less collaborative with the parents than with the physical therapists and that they behaved differently when in front of a camera.
In terms of lack of time, participants reported that during lockdown they had to continue working and doing household chores, and therefore they perceived the therapy as an extra workload.
All these barriers seemed to be perceived as factors that had an impact on their children's psychomotor progress, or even regression, during these months, compared to the in-person therapy.
Perceived facilitators during use
Participants also described different facilitators that helped them implement the digital practice. Along with the accessibility that all parents had to the technology needed to conduct the therapy at home (good internet connection and a computer with a camera), participants felt that it was very helpful to have learned what to observe in face-to-face sessions prior to the pandemic.
In addition, concerning facilitators, they spoke of the physical therapists' ability to adapt to the change of modality, which also implied performing the digital physical therapy with the materials they had at home. Consequently, they emphasized the importance of the human nature of the physical therapists, also highlighting the flexibility of their schedules to adapt to their needs as a family and the wide availability shown by the professionals. Finally, participants described how by being confined, the rest of the family also helped in the day-to-day sessions, which reduced the workload.
Future possibilities
After experiencing it first-hand, the participants described that, from their perspective, digital practice can be a future option for occasional sessions that cannot be attended in person, either because they live in geographical areas far from the EI center, or because of occasional illnesses of the child or other personal restrictions that do not allow travel. However, they continue to prefer face-to-face sessions, identifying digital physical therapy as a complement to these sessions, which also seems to facilitate communication with families, helping to improve their training and the resolution of doubts.
Furthermore, the participants described that if the child were older, it would be easier to perform the digital practice, therefore, in the future, it could be potentially used in these cases.
Discussion
This study described parents’ experiences of digital physical therapy in EI services during COVID-19 lockdown. The results seemed to reveal benefits of digital practice in children with developmental disorders. Several difficulties were highlighted, together with the perceived facilitators, from the parents’ point of view. Finally, the future possibilities were also underlined to further optimize the use of digital physical therapy practice.
Parents perceived digital practice as a very useful and practical option in COVID-19 circumstances, mainly due to the possibility of continuing with the treatment. This finding is consistent with those of several previous studies, which show continuity to be a positive factor inherent to telehealth in times of COVID-19.21,26,40,41 With digital physical therapy, parents also felt guided and supported at times when face-to-face attendance was not possible, allowing them to improve their own skills and understanding of how to help their child. Both the families42 as well as the professionals43 see greater ease in terms of family training and empowerment using this medium.26,44 Wallish et al.,45 described the empowerment of parents of children with developmental disorders in their phenomenological study. Parents felt more confident following the telehealth intervention, offering them greater insight into their children's behaviors. In our study, parents felt security and peace of mind due to the constant presence of the professional.
Our results, however, also seemed to show that for parents, digital physical therapy was a complicated therapy to perform, due to their lack of knowledge regarding this novel service, among others. In a recent study, school-based occupational therapists determined that there is a lack of understanding of telehealth in the services.46 Camden and Silva47 already indicated the need to prioritize training in telehealth for both therapists and parents because it is a novel, reliable, and beneficial therapy for all. Moreover, parents pointed to the lack of physical contact with the therapists as a major drawback; an aspect previously observed by parents26,48 and by occupational therapists46 as an indisputable barrier that was difficult to solve. In addition, the lack of knowledge made them feel afraid of having to assume all the responsibility, not feeling competent or confident at certain times, as previous authors have also indicated,26 which made it difficult to perform the sessions at home following the therapist's instructions.49 A clinical implication of this finding could be to provide specific training for both parents and therapists on privacy and security in the use of technology, skills to conduct these sessions remotely, or time management and availability. This suggestion should be considered for improving digital physical therapy practice in the future to make it easier to deal with these technical elements. 41
Our results reflect the numerous distractors that children face during digital physical therapy practice, consistent with what has been described by professionals46 and parents.26 Both the parents in our study and those in Camden and Silva's47 study commented that the asynchronous exchange of videos and photos was a good way to communicate. Another suggestion on how to improve digital physical therapy practice in the future could be to promote the asynchronous use of videos and photos in those children whose behavior was more altered by the camera or those with short attention spans. Parents did not have to manage their child and could focus on the therapists during the session.
Lack of time and feelings of stress also appeared to be notable difficulties described by parents when providing therapy. Schiariti and McWilliam22 already reflected that adults often had no rest, being forced to be constantly at home with their children without additional help, an aspect that was more complex if the children had a disability. Cankurtaran et al.,50 also observed that parents' physical and mental quality of life declined during the pandemic. In addition, families reported feeling additional responsibilities and a heavier workload.26 Conversely, in several studies prior to the pandemic,42,51 families highlighted the reduction in the number of trips to specialized centers as a great advantage; an aspect that did not appear in the present study. This may be because our study deals exclusively with the period of lockdown due to COVID-19, during which no one was able to travel.
The participants in our study described the belief that the child would progress faster during face-to-face therapy, consistent with statements of parents included in the Camden and Silva study,47 as they were afraid of losing the progress made in face-to-face therapy during the online therapy. In addition, some parents even observed a worsening or a halt in the child's progress, similar to the results of Cankurtaran et al.,50 in which most parents reported that their children's condition worsened during lockdown. However, in the study by Krasovsky et al.,21 parents found that telehealth during COVID-19 prevented functional decline.
Our results suggest different facilitators perceived by parents, such as technological accessibility. However, different studies26,43,49,52 highlighted the concern that telehealth does not reach people due to the lack of access to technology (especially in rural settings)26,52 or due to technological problems of internet connection, use of hardware or software.43,49 This contrast with previous studies in different settings may be due to the fact that all the participants in our study belonged to the same geographical context in a city with a good socioeconomic level, and therefore they all had good internet connections and easy access to technological means.
Other facilitators identified in our study are the parents' learning to manage their children in face-to-face sessions prior to the digital physical therapy practice, a finding that is consistent with the study by Gardner et al.,53 or the constant accompaniment, the availability and adaptation of the physical therapist, in aspects such as the timetable or the materials used, in accordance with previous studies,26,43 this is a source of peace of mind for parents.51 Finally, our findings also described the support and involvement of the whole family as another favorable factor, as shown in the study by Rosenbaum et al.,26 and that of Cole et al.,43 from the professionals' perspective.
Regarding the future possibilities of digital practice for pediatric physical therapy in EI, professionals and parents had already suggested that it may be an alternative in child disability services after the pandemic,26 consistent with our results. Havenga et al.,54 found that parents also mentioned this possibility in situations where distance prevented transportation to the treatment site. However, Bova et al.,14 argued that the new telehealth approach can be a valid alternative for the care and treatment of children with neurological disorders, however, it cannot be allowed to become a generalized and definitive model of care, consistent with the results of our study, which shows a clear preference for face-to-face therapy, which is similar to findings of other authors who also explored the families' perspective.41,45 The hybrid model, which combines face-to-face and telehealth services, is an option worth considering.47 A possible future clinical application is to enable physical therapists to gain insight into the child's natural environment (home, school, or park) in cases when travel to the community may not be feasible.
A strength of our study is that it is the first to our knowledge to describe the application of digital practice during COVID-19 lockdown in children with developmental disorders, from the parents’ perspectives. The limitation of this study is that these results cannot be extrapolated to all families who underwent digital physical therapy practice in EI during lockdown, due to the nature of the research question and the qualitative design selected.
Conclusions
This study may help to better understand the concerns, thoughts, and feelings that families have had with digital physical therapy, thus determining the possible benefits/limitations and its future possibilities. Digital practice was perceived as a good response to the COVID-19 lockdown, mainly due to the possibility of continuity of treatment. It allowed parents to feel supported and accompanied by their physical therapist, who helped them feel safer and reassured. However, several barriers related to lack of information and previous training, as well as physical and attentional factors were encountered. It is necessary to continue studying digital practice and its future possibilities in the field of physical therapy in EI and even at later ages to value and understand all the opportunities that new technologies can provide us in this field.
Declaration of Competing Interest
None.
Acknowledgments
The authors thank all the families and children who have made this study possible, sharing their experiences related to digital physical therapy during a difficult and unexpected experience, such as the COVID-19 lockdown.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.bjpt.2022.100445.
Appendix. Supplementary materials
References
- 1.Federación Estatal de Asociaciones de Profesionales de Atención Temprana (GAT) Real Patronato sobre Discapacidad; Madrid: 2005. Libro Blanco de La Atención Temprana.http://gat-atenciontemprana.org/wp-content/uploads/2019/05/LibroBlancoAtenci%C2%A6nTemprana.pdf Available from: (accessed on 1 December 2021) [Google Scholar]
- 2.Macías L., Palomo R., Chillón R., et al. Documento marco fisioterapia en atención temprana. España. Consejo General de Colegios de Fisioterapeutas de España. 2021 https://www.consejo-fisioterapia.org/adjuntos/publicaciones/publicacion_1.pdf Available from: (accessed on 1 December 2021) [Google Scholar]
- 3.Ponte J. Contextos y entornos naturales. Alguna reflexión teórica y su aplicación práctica. La Rev d'Atenció Precoç. 2017;5:127–144. http://www.desenvolupa.net/index.php/Articles/Contextos-y-entornos-naturales.-Alguna-reflexion-teorica-y-su-aplicacion-practica-Jaime-Ponte-11-2017 Available from: (accessed on 1 December 2021) [Google Scholar]
- 4.Romero-Galisteo R.P., Barajas C., Monográfico Gálvez-Ruiz P. Perspectivas actuales de evaluación e intervención en Atención Temprana. Escritos Psicol - Psychol Writings. 2014;8:6–13. doi: 10.24310/espsiescpsi.v8i2.13231. [DOI] [Google Scholar]
- 5.Díaz C. Confederación Plena Inclusión España; España: 2019. Guía Básica De Atención Temprana y Transformación.https://www.plenainclusion.org/sites/default/files/atencion_temprana_bbppinteractivo.pdf Available from: (accessed on 1 December 2021) [Google Scholar]
- 6.Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO). Coronavirus disease (COVID-19) out-break and situation reports. 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- 8.Boletín Oficial de la Comunidad de Madrid. Orden 338/2020, de 9 de marzo de 2020, de la Consejería de Sanidad, por la que se adoptan medidas preventivas y recomendaciones de salud pública en la Comunidad de Madrid como consecuencia de la situación y evolución del coronavirus (COVID-19). Available from: https://www.comunidad.madrid/sites/default/files/doc/sanidad/bocm-20200310-1.pdf. (accessed on 1 December 2021).
- 9.Dhiman S., Sahu P.K., Reed W.R., Ganesh G.S., Goyal R.K., Jain S. Impact of COVID-19 outbreak on mental health and perceived strain among caregivers tending children with special needs. Res Dev Disabil. 2020;107:1–15. doi: 10.1016/j.ridd.2020.103790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grumi S., Provenzi L., Gardani A., et al. Rehabilitation services lockdown during the COVID-19 emergency: the mental health response of caregivers of children with neurodevelopmental disabilities. Disabil Rehabil. 2020;43:27–32. doi: 10.1080/09638288.2020.1842520. [DOI] [PubMed] [Google Scholar]
- 11.Ferreira A.L., Ferreira L.C. Impact of social isolation due to the COVID-19 pandemic in patients with pediatric disorders: rehabilitation perspectives from a developing country. Phys Ther. 2020;100:1910–1912. doi: 10.1093/ptj/pzaa152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Physiotherapy . World Physiotherapy; Londres: 2021. Impact of the COVID-19 Pandemic on Physiotherapy Services.https://world.physio/sites/default/files/2021-06/Covid-Report-March2021-FINAL.pdf Available from: (accessed on 1 December 2021) [Google Scholar]
- 13.Cacioppo M., Bouvier S., Bailly R., Houx L., Lempereur M., Mensah-Gourmel J., et al. Emerging health challenges for children with physical disabilities and their parents during the COVID-19 pandemic: the ECHO French survey. Ann Phys Rehabil Med. 2021;64(3) doi: 10.1016/j.rehab.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bova S.M., Basso M., Bianchi M.F., et al. Impact of COVID-19 lockdown in children with neurological disorders in Italy. Disabil Health J. 2021;14:1–9. doi: 10.1016/j.dhjo.2020.101053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mayston M. Telehealth for disability management: what really matters? Dev Med Child Neurol. 2021;63:124. doi: 10.1111/dmcn.14734. [DOI] [PubMed] [Google Scholar]
- 16.Molinaro A., Micheletti S., Pagani F., et al. Action observation treatment in a tele-rehabilitation setting: a pilot study in children with cerebral palsy. Disabil Rehabil. 2020;42:1–6. doi: 10.1080/09638288.2020.1793009. [DOI] [PubMed] [Google Scholar]
- 17.Beani E., Menici V., Ferrari A., Cioni G., Sgandurra G. Feasibility of a home-based action observation training for children with unilateral cerebral palsy: an explorative study. Front Neurol. 2020;11:1–17. doi: 10.3389/fneur.2020.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pietruszewski L., Burkhardt S., Yoder P.J., Heathcock J., Lewandowski D.J., Maitre N.L. Protocol and feasibility-randomized trial of telehealth delivery for a multicomponent upper extremity intervention in infants with asymmetric cerebral palsy. Child Neurol Open. 2020;7:1–9. doi: 10.1177/2329048×20946214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ellison K.S., Guidry J., Picou P., Adenuga P., Davis T.E. Telehealth and autism prior to and in the age of COVID-19: a systematic and critical review of the last decade. Clin Child Fam Psychol Rev. 2021;24:1–32. doi: 10.1007/s10567-021-00358-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tanner K., Bican R., Boster J., et al. Feasibility and acceptability of clinical pediatric telerehabilitation services. Int J Telerehabil. 2020;12:43–52. doi: 10.5195/ijt.2020.6336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krasovsky T., Silberg T., Barak S., et al. Transition to multidisciplinary pediatric telerehabilitation during the COVID-19 pandemic: strategy development and implementation. Int J Environ Res Public Health. 2021;18:1–13. doi: 10.3390/ijerph18041484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schiariti V., McWilliam R.A. Crisis brings innovative strategies: collaborative empathic teleintervention for children with disabilities during the COVID-19 lockdown. Int J Environ Res Public Health. 2021;18:1–10. doi: 10.3390/ijerph18041749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Plena Inclusión. Cómo Implementar La Teleintervención En La Atención Temprana. España: Plena Inclusión España; 2020. Available from: https://www.plenainclusion.org/sites/default/files/plena_inclusion._como_implementar_la_teleintervencion_en_la_atencion_temprana_0.pdf. (accessed on 1 December 2021).
- 24.Rabatin A.E., Lynch M.E., Severson M.C., Brandenburg J.E., Driscoll S.W. Pediatric telerehabilitation medicine: making your virtual visits efficient, effective and fun. J Pediatr Rehabil Med An Interdiscip Approach. 2020;13:355–370. doi: 10.3233/PRM-200748. [DOI] [PubMed] [Google Scholar]
- 25.Richmond T., Otr L., Peterson C., et al. American telemedicine association's principles for delivering telerehabilitation services. Int J Telerehabil. 2017;9:63–68. doi: 10.5195/ijt.2017.6232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosenbaum P.L., Silva M., Camden C. Let's not go back to ‘normal’! lessons from COVID-19 for professionals working in childhood disability. Disabil Rehabil. 2021;43:1022–1028. doi: 10.1080/09638288.2020.1862925. [DOI] [PubMed] [Google Scholar]
- 27.Cresswell J., Poth C. SAGE Publications Inc.; Thousand Oaks, California: 2018. Qualitative Inquiry and Research Design Choosing Among Five Approaches. [Google Scholar]
- 28.Korstjens I., Moser A. Series: practical guidance to qualitative research. Part 2: context, research questions and designs. Eur J Gen Pract. 2017;23:274–279. doi: 10.1080/13814788.2017.1375090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neubauer B.E., Witkop C.T., Varpio L. How phenomenology can help us learn from the experiences of others. Perspect Med Educ. 2019;8:90–97. doi: 10.1007/s40037-019-0509-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Norlyk A., Harder I. What makes a phenomenological study phenomenological? An analysis of peer-reviewed empirical nursing studies. Qual Health Res. 2010;20:420–431. doi: 10.1177/1049732309357435. [DOI] [PubMed] [Google Scholar]
- 31.Dowling M. From Husserl to van Manen. A review of different phenomenological approaches. Int J Nurs Stud. 2007;44:131–142. doi: 10.1016/j.ijnurstu.2005.11.026. [DOI] [PubMed] [Google Scholar]
- 32.Klem N.R., Shields N., Smith A., Bunzli S. Demystifying qualitative research for musculoskeletal practitioners part 4: a qualitative researcher's toolkit-sampling, data collection methods, and data analysis. J Orthop Sports Phys Ther. 2022;52(1):8–10. doi: 10.2519/jospt.2022.10486. [DOI] [PubMed] [Google Scholar]
- 33.O'Brien B.C., Harris I.B., Beckman T.J., Reed D.A., Cook D.A. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89:1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 34.Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Heal Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 35.Carpenter C., Suto M. Black-Well Publishing; Oxford: 2008. Qualitative Research For Occupational and Physical therapists: a Practical Guide. [Google Scholar]
- 36.Moser A., Korstjens I. Series: practical guidance to qualitative research. Part 3: sampling, data collection and analysis. Eur J Gen Pract. 2018;24:9–18. doi: 10.1080/13814788.2017.1375091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Archibald M.M., Ambagtsheer R.C., Casey M.G., Lawless M. Using zoom videoconferencing for qualitative data collection: perceptions and experiences of researchers and participants. Int J Qual Methods. 2019;18:1–8. doi: 10.1177/1609406919874596. [DOI] [Google Scholar]
- 38.Braun V., Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 39.Lincoln Y., Guba E. SAGE Publications Inc.; California: 1985. Naturalistic Inquiry. [Google Scholar]
- 40.Assenza C., Catania H., Antenore C., et al. Continuity of care during COVID-19 lockdown: a survey on stakeholders’ experience with telerehabilitation. Front Neurol. 2021;11:1–14. doi: 10.3389/fneur.2020.617276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dantas L.O., Barreto R.P.G., Ferreira C.H.J. Digital physical therapy in the COVID-19 pandemic. Braz J Phys Ther. 2020;24(5):381–383. doi: 10.1016/j.bjpt.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Salomone E., Maurizio Arduino G. Parental attitudes to a telehealth parent coaching intervention for autism spectrum disorder. J Telemed Telecare. 2017;23:416–420. doi: 10.1177/1357633×16642067. [DOI] [PubMed] [Google Scholar]
- 43.Cole B., Pickard K., Stredler-Brown A. Report on the use of telehealth in early intervention in Colorado: strengths and challenges with telehealth as a service delivery method. Int J Telerehabil. 2019;11:33–40. doi: 10.5195/ijt.2019.6273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Camden C., Pratte G., Fallon F., Couture M., Berbari J., Tousignant M. Diversity of practices in telerehabilitation for children with disabilities and effective intervention characteristics: results from a systematic review. Disabil Rehabil. 2020;42:3424–3436. doi: 10.1080/09638288.2019.1595750. [DOI] [PubMed] [Google Scholar]
- 45.Wallisch A., Little L., Dunn W. Parent perspectives of an occupational therapy telehealth intervention. Int J Telerehabil. 2019;11:15–22. doi: 10.5195/ijt.2019.6274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rortvedt D., Jacobs K. Perspectives on the use of a telehealth service-delivery model as a component of school-based occupational therapy practice: designing a user-experience. Work. 2019;62:125–131. doi: 10.3233/WOR-182847. [DOI] [PubMed] [Google Scholar]
- 47.Camden C., Silva M. Pediatric teleheath: opportunities created by the COVID-19 and suggestions to sustain its use to support families of children with disabilities. Phys Occup Ther Pediatr. 2021;41:1–17. doi: 10.1080/01942638.2020.1825032. [DOI] [PubMed] [Google Scholar]
- 48.Tenforde A.S., Hefner J.E., Kodish-Wachs J.E., Iaccarino M.A., Paganoni S. Telehealth in physical medicine and rehabilitation: a narrative review. PM&R. 2017;9:51–58. doi: 10.1016/j.pmrj.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 49.Provenzi L., Grumi S., Gardani A., et al. Italian parents welcomed a telehealth family-centred rehabilitation programme for children with disability during COVID-19 lockdown. Acta Paediatr Int J Paediatr. 2021;110:194–196. doi: 10.1111/apa.15636. [DOI] [PubMed] [Google Scholar]
- 50.Cankurtaran D., Tezel N., Yildiz S.Y., Celik G. Unlu Akyuz E. Evaluation of the effects of the COVID-19 pandemic on children with cerebral palsy, caregivers’ quality of life, and caregivers’ fear of COVID-19 with telemedicine. Ir J Med Sci. 2021;190:1–8. doi: 10.1007/s11845-021-02622-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Buono S., Città S. Tele-assistance in intellectual disability. J Telemed Telecare. 2007;13:241–245. doi: 10.1258/135763307781458903. [DOI] [PubMed] [Google Scholar]
- 52.Rideout V., Katz V.S. Joan Ganz Cooney Center at Sesame Workshop; New York: 2016. Opportunity For all? Technology and Learning in Lower-Income Families.https://joanganzcooneycenter.org/publication/opportunity-for-all-technology-and-learning-in-lower-income-families/ Available from: (accessed on 1 December 2021) [Google Scholar]
- 53.Gardner K., Bundy A., Dew A. Perspectives of rural carers on benefits and barriers of receiving occupational therapy via Information and communication technologies. Aust Occup Ther J. 2016;63:117–122. doi: 10.1111/1440-1630.12256. [DOI] [PubMed] [Google Scholar]
- 54.Havenga E., Swanepoel D.W., Le Roux T., Schmid B. Tele-intervention for children with hearing loss: a comparative pilot study. J Telemed Telecare. 2017;23:116–125. doi: 10.1177/1357633×15617886. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.