Abstract
Liver hanging maneuver (LHM) is now a safe, accurate, and well established technique for various kinds of hepatic resections. But because of technical difficulty and limited experience, there have been very few reports of hepatic resection using LHM in children as compared to adults. We hereby report a case of extended right hepatectomy with part of caudate lobectomy using LHM in an 8-month-old infant for a large hepatoblastoma in Kidwai Memorial Institute of Oncology, a regional cancer center in south India. LHM facilitates major hepatectomy with “anterior approach,” reducing several risks caused by liver mobilization: bleeding, rupture of the tumor, tumor cell dissemination, hemodynamic instability, and post op liver failure. This technique is very useful and safe for bulky pediatric hepatic tumors.
Keywords: Liver resection, Hanging maneuver, Hepatoblastoma
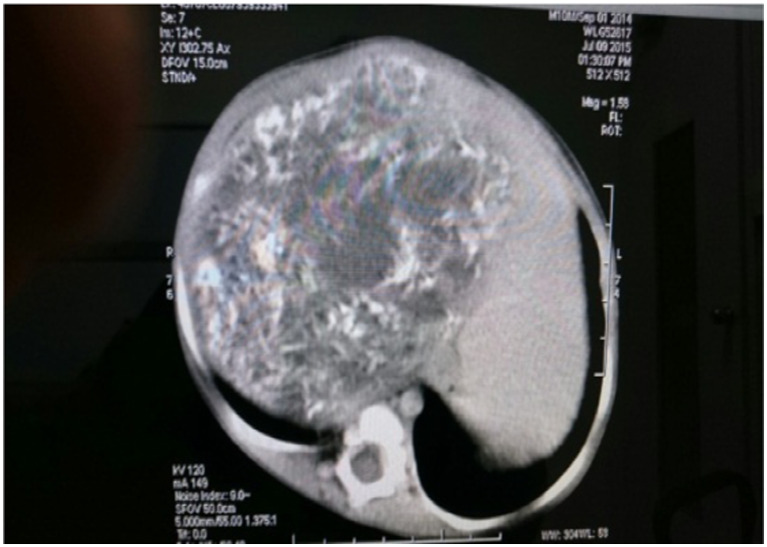
An 8-month male child presented to our department with complaints of a large mass in the abdomen, which the parents noticed first at 4 months of age and which progressively increased over the period. The patient was investigated and diagnosed as hepatoblastoma by FNAC. Serum AFP was elevated (1000 ng/ml). CECT abdomen and pelvis showed a 10.2 × 9.3 × 9.5 cm mass in the right lobe liver splaying RHV and MHV, abutting and displacing the right kidney (Fig. 1). Hepatic veins and intrahepatic IVC are normal. Because of a large size, NACT was planned and 5 cycles carboplatin-adriamycin were given. Postchemotherapy CT abdomen showed no significant interval reduction in the size of lesion (stable disease).
Fig. 1.
CECT abdomen showing a 10.2 × 9.3 × 9.5 cm mass in the right lobe liver splaying RHV and MHV
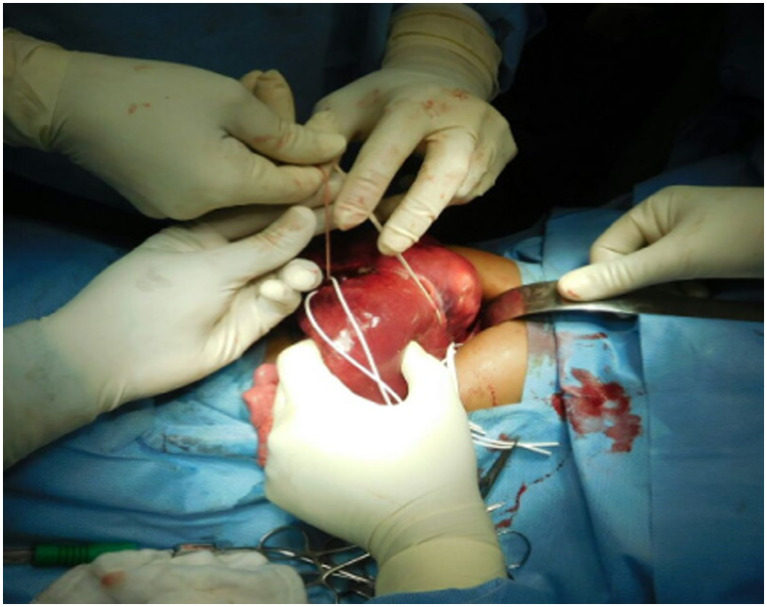
Hence, the patient was planned for surgery and he underwent right extended hepatectomy with part of caudate lobectomy by liver hanging maneuver (LHM). The abdomen was opened by right subcostal transverse incision extending about 3–4 cm across midline. The falciform ligament was divided and suprahepatic IVC was exposed. Fibrous tissue between liver and anterior surface of IVC was dissected with the help of right angled forceps. Liver parenchyma was dissected and confluence of the middle and left hepatic vein was identified. Then, dissection started at the porta hepatis. The hepatic pedicle was retracted to the left and segment I was lifted from IVC. The anterior aspect of the infrahepatic IVC was dissected and short hepatic veins were ligated and divided. A long curved Kelly clamp was inserted behind the caudate lobe just to left of the right inferior hepatic vein (RIHV) and passed cranially along the anterior surface of IVC between 10 and 11 o’clock positions towards space between the previously dissected middle and left hepatic veins. After complete dissection, hepatic parenchyma was looped up with an umbilical tape. During parenchymal transection, continuous upwards traction was applied on tape by holding both its ends together (Fig. 2). Occlusion of one or two of three Glisson’s pedicles, which enter a part of the liver to be resected, revealed a demarcation line on the liver surface.
Fig. 2.
Hanging maneuver with an umbilical tape passed through a tunnel created between 9 and 10 o’clock position anterior to IVC and passed between the middle and left hepatic vein
Parenchymal transection was done with the help of bipolar electrocautery and harmonic scalpel. Smaller vessels (<3 mm) were coagulated and larger ones were ligated. After parenchymal transection, occluded Glisson’s pedicle was divided after being dissected into its artery, portal vein, and bile duct. Draining hepatic vein was divided. IRHV was divided between vascular clamps and oversewn.
Operating time was 210 min with about 100 ml blood loss. Postoperative recovery was uneventful and the patient was discharged on postoperative day 9.
Final HPR showed a 16 × 14.5 × 8 cm hepatoblastoma with mixed epithelial-mesenchymal component with areas of focal necrosis and small foci of residual viable epithelial component (10 %), margins free of tumor. The patient was followed up at regular intervals with continuation of adjuvant chemotherapy.
Discussion
Complete liver mobilization and extrahepatic vascular control for right hepatectomy was first described by Lortat-Jacob and Robert in 1952. This technique increased safety of major hepatectomies, hence was adopted by most hepatic surgeons as conventional approach to right hepatic resection [1].
Over the years, some drawbacks of liver mobilization have emerged: (i) high risk of hemorrhage because of difficult right-sided mobilization, especially for huge tumors that invades surrounding structures; (ii) manipulation of tumor with risk of tumor rupture or systemic dissemination of cancer cells; (iii) intraoperative systemic hemodynamic instability caused by twisting and compression of IVC; and (iv) damage to remnant liver caused by mechanical compression of parenchyma and inflow reduction by pedicle torsion.
To circumvent these problems, the “anterior approach” (AA) was proposed by Ozawa in 1992 and later developed by practitioners in Hong Kong (Lai et. al) [2, 3]. This unconventional approach consisted of parenchymal transection without prior mobilization of the liver. The advantages of this approach are decreased intraoperative blood loss and transfusion requirements, “no-touch” technique—hence decreased tumor cell dissemination with increased cumulative disease free survival, and decreased post op liver failure because of less intraoperative ischemia to remnant liver.
The drawbacks of anterior approach were difficulty in visualization of deeper parenchymal plane and bleeding control during deeper parenchymal dissection. To overcome these drawbacks, Jacques Belghiti in 2001 proposed the concept of liver hanging maneuver (LHM) [4]. The advantages of LHM are as follows:
Facilitates control of bleeding at the deeper parenchymal plane
Guides the direction of anatomic parenchymal transection
Facilitates major hepatectomy with “anterior approach”
Provides traction and facilitates dissection in deeper plane
Reduces several risks caused by liver mobilization like bleeding, rupture of the tumor, tumor cell dissemination, hemodynamic instability, and post op liver failure
The critical step of liver mobilization is dissection between the liver and anterior surface of IVC. The anatomical basis for which is formed by existence an avascular plane from 10 to 11 o’clock position on the anterior surface of IVC. Dissection should be done in this plane.
Direct invasion of tumor to distal major hepatic veins, diaphragm, and retroperitoneum, cirrhosis, large tumor size, preoperative TACE, and/or portal vein embolization were earlier considered as contraindication for major liver resection. Several studies have shown that these conditions are not contraindications and LHM can be done safely. The only contraindication for LHM at present is infiltration of the avascular plane by liver lesion.
Complication during LHM is mainly vascular in nature, which occurs due to dissection into subcapsular plane (MC), injury to SHV, and injury to MRHV and IRHV. The reported incidence of bleeding has been found to be 0 to 6 %. No death has been reported till date due to bleeding.
Other studies conducted by Kokudu et al. [5], Ettore et al. [6], and Suzuki et al. [7] have established the safety and feasibility of LHM for various kinds of liver resections. [Table 1] shows a brief review of literature with comparison.
Table 1.
Studies that have established the safety and feasibility of LHM for various kinds of liver resections
| Study | Indications | Planed | Done | Feasibility | Intra-op bleeding | Bleeding-related interruption |
|---|---|---|---|---|---|---|
| Belghiti 2001 | 32 RH | 32 | 30 | 93.5 % | 2(6 %) | 2 |
| Kokudo 2003 | 37 RH, 8 RHM, 20 LH, 6RLS | 71 | 70 | 98.5 % | 1(1.40 %) | 1 |
| Susuki 2004 | 5 RH | 5 | 5 | 100 % | 0 | 0 |
| Ettorre 2004 | 26 RH | 26 | 24 | 92.3 % | 1(4 %) | 0 |
| Belghiti 2007 | 159 RH, 28 RHM, 9 LH, 5 ELH | 228 | 201 | 88 % | 5(2 %) | 0 |
| Ettorre 2007 | 45 RH, 34 LH, 1 CH | 49 | 47 | 96 % | 1(2 %) | 0 |
Although we have performed a number adult hepatectomies using hanging technique, this is the first time we have performed it in an infant. Very few case reports are there in world literature and none has been reported in India of using hanging technique in infant.
Conclusion
Hepatectomies in pediatric patients are difficult and challenging, and hanging technique can be extremely useful in performing it easily and safely.
Contributor Information
C. Ramachandra, Email: ramachandrac@yahoo.com
Sharma Vikas, Email: dr.vs8070@gmail.com.
S. Krishnamurthy, Email: krishnamuthys@yahoo.com
S. Ramesh, Email: doctorsramesh@gmail.com
L. Appaji, Email: lappaji@yahoo.com
Rekha V. Kumar, Email: rehkavkumar@gmail.co.in
References
- 1.Lortat-Jacob JL, Robert HG. Well defined technique for right hepatectomy. Presse Med. 1952;60:549–551. [PubMed] [Google Scholar]
- 2.Ozawa K. Hepatic function and liver resection. J Gastroenterology Hepatology. 1990;5:296–309. doi: 10.1111/j.1440-1746.1990.tb01632.x. [DOI] [PubMed] [Google Scholar]
- 3.Lai EC, Fan ST, Lo CM, et al. Anterior approach for difficult major right hepatectomy. World J Surg. 1996;20:314–317. doi: 10.1007/s002689900050. [DOI] [PubMed] [Google Scholar]
- 4.Belghiti J, Guevara OA, Noun R, et al. Liver hanging maneuver: a safe approach to right hepatectomy without liver mobilization. J Am Coll Surg. 2001;193:109–111. doi: 10.1016/S1072-7515(01)00909-7. [DOI] [PubMed] [Google Scholar]
- 5.Kokudo N, Sugawara Y, Imamura H, Sano K, Makuuchi M. Sling suspension of the liver in donor operation: a gradual tape-repositioning technique. Transplantation. 2003;76:803–807. doi: 10.1097/01.TP.0000080982.03297.A7. [DOI] [PubMed] [Google Scholar]
- 6.Ettorre GM, Douard R, Corazza V, Santoro R, Vennarecci G, Santoro E. Anatomical basis of liver hanging manoeuvre: a clinical and anatomical in vivo study. Am Surg. 2007;73:1193–1196. [PubMed] [Google Scholar]
- 7.Suzuki M, Unno M, Katayose Y, Takeuchi H, Rikiyama T, Onogawa T, et al. Hepatic resection through an anterior approach employing a modified liver hanging manoeuvre in patients with a massive liver tumour severely oppressing the inferior vena cava. Hepato-Gastroenterology. 2004;51:1459–1463. [PubMed] [Google Scholar]