Background:
Postoperative nursing can improve the quality of life (QoL) and functional prognosis for lung cancer patients. The purpose of this study was to evaluate the effects of high-quality nursing on inflammation and prognosis in postoperative patients with advanced nonsmall cell lung cancer (NSCLC).
Methods:
A total of 372 patients with NSCLC were enrolled between the May 2014 and June 2016. Patients were randomly received high-quality nursing (n = 192) or normal nursing (n = 180). Symptom management, QoL, hospital stay, inflammatory score, survival time, recurrence rate, symptoms, anxiety, depression scale and psychological distress were assessed at baseline and 5-year follow up.
Results:
High-quality nursing significantly shortened hospital stay, improved postoperative inflammation, symptom management, QoL compared to patients received normal nursing. Compare with normal nursing, high-quality nursing decreased anxiety, depression scale and psychological distress for postoperative patients with advanced NSCLC. Outcomes showed that high-quality nursing increased the survival time and decreased recurrence rate for postoperative patients with advanced NSCLC.
Conclusion:
In conclusion, data in the current study indicate that high-quality nursing can decrease inflammation and improve prognosis for the postoperative patients with NSCLC.
Keywords: High-quality nursing, nonsmall cell lung cancer, quality of life, recurrence, survival
1. Introduction
Lung cancer approximately accounts for one third of all cancer-related deaths that is more seriously threat for human health than other cancers including colon cancer, breast, prostate and liver cancer.[1] The median survival of patients with advanced nonsmall cell lung cancer (NSCLC) has historically been poor and the 5-year survival rate is very low.[2] The prognosis of patients with advanced NSCLC is also unsatisfactory, despite many therapeutic strategies have been applied for clinical patients.[3–5]
Nursing is an essential model of clinical intervention, which strengthens the significance of clinical nursing activities for patients with cancer.[6] An integrated nursing can effectively relieve the patient’s negative feelings, improve their self-management ability, reduce the burden of family care and improve the satisfaction with nursing activities for lung cancer patients.[7] Appropriate care provided by nurses contributes to decreasing of anxiety, depression scale, and monitor for possible complications.[8] Comprehensive nursing is a preferable technique for acute psoriasis to improve clinical symptoms, enhance immune function and diminish inflammatory factor levels, thereby optimizing the quality of life (QoL) in cancer patients.[9] Nursing plays a pivotal role in the treatment course of cancer patients because nursing care can observe and inquiry the early recognition of the signs and symptoms of side effects, which will help improve the outcomes of the cancer patients.[10] Nursing of follow-up of cancer patients during the postoperative period are feasible and effective in improving the QoL, postoperative symptoms, and distress for NSCLC patients.[11] It is therefore important to analyze the relationship between nursing and prognosis of NSCLC patients.
In the present study, effects of high-quality nursing on symptom management, QoL, hospital stay, inflammatory score, symptoms, anxiety, depression scale and psychological distress were assessed at baseline and 5-year for postoperative patients with advanced NSCLC. The aim of the present study was also to investigate the effects of high-quality nursing on survival time and recurrence rate in postoperative patients with advanced NSCLC.
2. Materials and Methods
2.1. Patients
A total of 394 patients with advanced NSCLC were enrolled in the Hongqi Hospital Affiliated to Mudanjiang Medical College from May 2014 to June 2016. Diagnosis of advanced NSCLC was confirmed by 3 radiologists. All patients were received normal nursing group (n = 202) or high-quality nursing group (n = 192). Patients with advanced NSCLC are assessed over a 5-year follow-up period beginning at the end of surgery.
2.2. Inclusion and exclusion criteria
Eligibility criteria were as follow: histologically confirmed advanced NSCLC after surgery; scheduled for adjuvant chemotherapy; age > 18 years; body mass index (BMI) > 18 kg/m2; follow the study protocol. Patients were excluded: (1) had cancer history; (2) concurrent surgery; (3) congestive heart disease; (4) depression; (5) pregnant woman; (6) patients with a history of childhood trauma. The study protocol was approved by the Ethical committee Red Flag Hospital affiliated to Mudanjiang Medical College (Mudanjiang, China).
2.3. Type of interventions
In the control group, normal nursing for the management of symptoms condition in patients with advanced NSCLC will be included. Normal nursing included routine nursing, diet nursing, symptom nursing and other postoperative nursing. In the experimental group, all types of high-quality nursing include the normal nursing and additional care. Additional care included postoperative complications care, postoperative mental communication, and medication reminder in patients with advanced NSCLC.
2.4. Clinical assessment
Quality of life was evaluated using the Dutch version of the World Health Organization QoL assessment instrument (WHOQOL-100).[12] Satisfaction of patients was accessed by the “satisfaction with provider” item (question 18) of the validated Consumer Assessment of Healthcare Providers and Systems General Survey. Physical function assessment was analyzed using The World Health Organization’s International Classification of Functioning, Disability and Health.[13] Depression was measured using the 20-item Center for Epidemiologic Studies Depression scale (CES-D). Cognitive function was accessed using the trail-making-test. Anxiety of patients was determined by the Dental Anxiety Scale (DAS). The systemic inflammation score (SIS) score was measured from the results of the blood test (serum albumin level and LMR) as described previously.[14]
2.5. Data analysis
Data are expressed as mean ± standard deviation (SD) or number (%). Data are analyzed using SPSS19.0 (IBM Corp., Armonk, NY) statistical software. Unpaired Student t test or Mann–Whitney U test was used for the comparison between the 2 groups. Kaplan–Meier method was used to assess the relationship between the survival time of patient and the nursing. A P < .05 was considered significant.
3. Results
3.1. Characteristics of the postoperative patients with advanced NSCLC
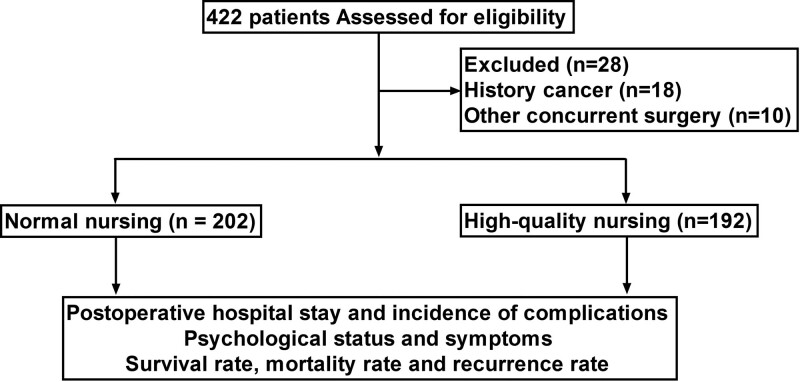
Patients with advanced NSCLC were divided into high-quality nursing group (n = 192) and normal nursing group (n = 202). Advanced NSCLC patients were determined by the current Diagnosis-Specific Graded Prognostic Assessment (DS-GPA). All patients were grade III or IV NSCLC. Characteristics of advanced NSCLC patient are summarized in Table 1. Figure 1 showed participant flow from recruitment to follow-up for patients with advanced NSCLC.
Table 1.
Baseline characteristics of patients.
| Characteristic | Normal nursing care | High-quality nursing care | P value |
|---|---|---|---|
| Number | 202 | 192 | 0.87 |
| Gender (no. in %) | |||
| Female | 92 (45.5%) | 87 (45.3%) | 0.92 |
| Male | 110 (54.5%) | 105 (54.7%) | 0.85 |
| Smoking history (no. in %) | 32 (15.8%) | 27 (14.1%) | 0/82 |
| Pathological type (no. in %) | |||
| Adenocarcinoma | 112 (55.4%) | 107 (55.7%) | 0.90 |
| Squamous carcinoma | 90 (44.6%) | 85 (44.3%) | 0.82 |
| Stage (no. in %) | |||
| III | 146 (72.3%) | 142 (74.0%) | 0.86 |
| IV | 56 (27.7%) | 50 (26.0%) | 0.88 |
| Chemotherapy state (no. in %) | |||
| First-line chemotherapy | 88 (43.6%) | 84 (43.8%) | 0.93 |
| Second-line chemotherapy | 114 (56.4%) | 108 (56.2%) | 0.92 |
Data are shown as n (%).
Figure 1.
Study flowchart.
3.2. Comparison of postoperative hospital stay and incidence of complications
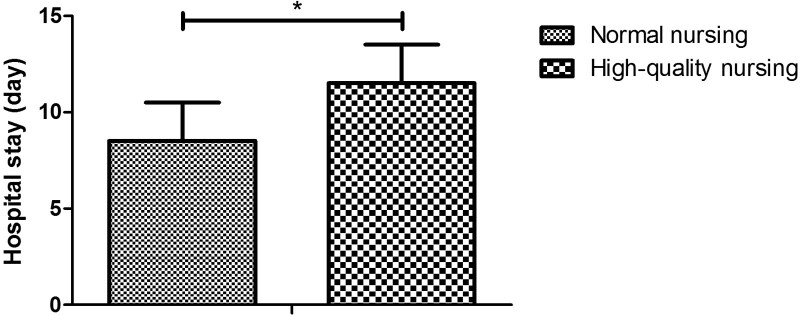
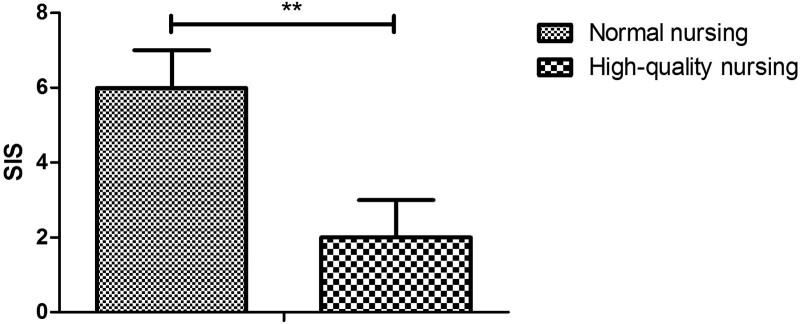
As shown in Figure 2, high-quality nursing decreased hospital stay compared with normal nursing (8.5 days vs 11.5 days; P < .05). Data demonstrated that incidence of complications during hospitalization were decreased by high-quality nursing compared to normal nursing (Table 2). The SIS of patients in high-quality nursing group was lower than patients in normal nursing group (Fig. 3).
Figure 2.
Analysis of postoperative hospital stay and incidence of complications between high-quality nursing and normal nursing group. *P < .05 vs normal nursing.
Table 2.
Incidence of complications were decreased by high-quality nursing care compared to normal nursing care.
| Complications | Normal nursing care | High-quality nursing | P value |
|---|---|---|---|
| Pneumonia | 3 (1.5%) | 1 (0.5%) | 0.042 |
| Atelectasis | 5 (2.5%) | 2 (1.0%) | 0.035 |
| Hypoxia | 6 (3.0%) | 2 (1.0%) | 0.010 |
| Empyema/pleuritis | 4 (2.0%) | 1 (0.5%) | 0.012 |
| Interstitial pneumonitis | 4 (2.0%) | 1 (0.5%) | 0.012 |
| Respiratory failure | 2 (1.0%) | 1 (0.5%) | 0.042 |
| Pulmonary edema | 2 (1.0%) | 1 (0.5%) | 0.072 |
| Asthma attack | 3 (1.5%) | 1 (0.5%) | 0.042 |
| Bronchitis | 4 (2.0%) | 2 (1.0%) | 0.045 |
| Atrial fibrillation | 5 (2.5%) | 2 (1.0%) | 0.037 |
| Delirium | 0 | 0 | - |
| Chylothorax | 2 (1.0%) | 1 (0.5%) | 0.042 |
| Bleeding (reoperation) | 3 (1.5%) | 1 (0.5%) | |
| Bronchial fistula | 4 (2.0%) | 2 (1.0%) | 0.048 |
| Cerebral infarction | 0 | 0 | - |
| Urinary tract infection | 0 | 0 | - |
| Lung herniation | 4 (2.0%) | 1 (0.5%) | 0.030 |
| Gastric dyskinesia | 0 | 0 | - |
| Sepsis | 0 | 0 | - |
| Angina | 0 | 0 | - |
| Heart failure | 0 | 0 | - |
| Middle lobe rotation | 1 (0.5%) | 0 | - |
| Transient ischemic attack | 0 | 0 | - |
Data are shown as n (%).
Figure 3.
Analysis of the systematic inflammation score between high-quality nursing and normal nursing group. *P < .05 vs normal nursing.
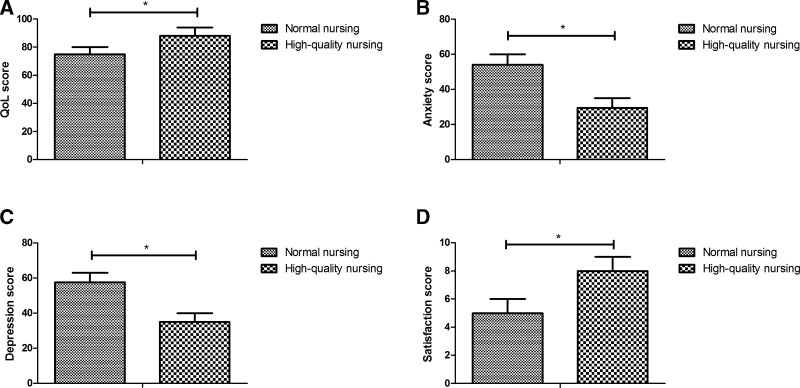
3.3. Comparison of psychological status
The satisfaction with care quality was reported in postoperative patients with advanced NSCLC between high-quality nursing and normal nursing groups. As shown in Figure 4A, patient physical QoL had a significant improvement in high-quality nursing group compared to normal nursing group. As shown in Figure 4B–C, high-quality nursing significantly decreased anxiety and depression scale for postoperative patients with advanced NSCLC compared to patients in normal nursing group. As shown in Figure 4D, the high-quality nursing increased the satisfaction of NSCLC patient compared to patients in the normal nursing group. The parameters of psychological status of postoperative patients with advanced NSCLC were shown in Table 3.
Figure 4.
Analysis of psychological status in postoperative patients with advanced NSCLC between high-quality nursing and normal nursing group. (A) Patient physical QoL; (B) anxiety of patients; (C) depression of patients; (D) the satisfaction of patients. *P < .05 vs normal nursing.
Table 3.
Comparison of QoL in postoperative patients with advanced NSLCL between 2 groups.
| Outcome | Normal nursing care | High-quality nursing | P value |
|---|---|---|---|
| Quality of life-EORTC QLQ30 (scale 0–100) | |||
| Global QoL | 72 ± 8 | 86 ± 8 | 0.032 |
| Physical function | 52 ± 10 | 68 ± 11 | 0.040 |
| Emotional function | 42 ± 8 | 56 ± 10 | 0.048 |
| Role function | 65 ± 12 | 74 ± 14 | 0.045 |
| Cognitive function | 45 ± 11 | 54 ± 10 | 0.034 |
| Social function | 62 ± 13 | 75 ± 14 | 0.026 |
| Depression-CES-D (scale 0-100) | |||
| Depression score | 54 ± 6 | 34 ± 6 | 0.025 |
| Anxiety(scale 0–100) | |||
| Anxiety score | 55 ± 5 | 30 ± 5 | 0.022 |
Data are shown as mean ± SD.
3.4. Comparison of cancer-related symptoms
The effects of nursing care on symptom management were investigated in postoperative patients with advanced NSCLC. As shown in Table 4, high-quality nursing could alleviate symptoms including pain, fatigue, sleep disturbance, nausea, shortness of breath, sadness, poor appetite, dry mouth, difficulty remembering, distress, drowsiness, vomiting and numbness. We found that high-quality nursing had a significant improvement of emotional problems in patients with advanced NSCLC compared to those in the normal nursing group.
Table 4.
Effects of high-quality nursing care on cancer-related symptoms in postoperative patients with advanced NSLCL.
| Symptoms | Normal nursing care | High-quality nursing | P value |
|---|---|---|---|
| Pain | 16 (7.9%) | 7 (3.6%) | 0.40 |
| Fatigue | 24 (11.9%) | 18 (9.4%) | 0.50 |
| Sleep disturbance | 32 (15.8%) | 20 (10.4%) | 0.37 |
| Nausea | 25 (12.4%) | 17 (8.9%) | 0.44 |
| Shortness of breath | 22 (10.9%) | 13 (6.8%) | 0.34 |
| Poor appetite | 40 (19.8%) | 30 (15.6%) | 0.27 |
| Dry mouth | 35 (17.3%) | 26 (13.5%) | 0.20 |
| Difficulty remembering | 10 (4.9%) | 5 (2.6%) | 0.26 |
| Distress | 17 (8.4%) | 10 (5.2%) | 0.18 |
| Drowsiness | 34 (16.8%) | 21 (10.9%) | 0.10 |
| Vomiting | 37 (18.3%) | 19 (9.9%) | 0.08 |
| Numbness | 16 (7.9%) | 11 (5.7%) | 0.45 |
Data are shown as n (%).
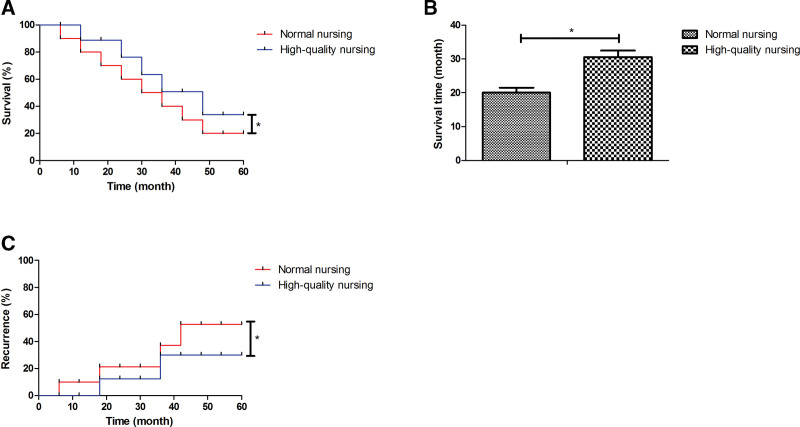
3.5. Comparison of survival rate, survival time and recurrence rate
The survival time, mortality and recurrence rate of postoperative patients with advanced NSCLC were compared between high-quality nursing and normal nursing group. As shown in Figure 5A–B, high-quality nursing had higher survival rate and survival time for postoperative patients with advanced NSCLC than patients received normal nursing. As shown in Figure 5C, high-quality nursing decreased mortality rate of postoperative patients with advanced NSCLC compared to those in the normal nursing group (P < .05). Data also found that patients with advanced NSCLC in the high-quality nursing had lower recurrence rate than those in the normal nursing group (P < .05).
Figure 5.
Analysis of the survival rate, survival time and recurrence rate between high-quality nursing and normal nursing group. (A) Kaplan–Meier curves for survival of patients with advanced NSCLC. (B) Survival time of postoperative patients with advanced NSCLC. (C) Recurrence rate of patients with advanced NSCLC. *P < .05 vs normal nursing.
4. Discussion
Despite most patients with advanced NSCLC receive surgery and other treatments, the overall survival and 5-year survival rate is unsatisfactory.[15] In this study, we investigated the effect of high-quality nursing on survival rate and recurrence rate in postoperative patients with advanced NSCLC. After receiving high-quality nursing, postoperative patients with advanced NSCLC experienced significantly increased the overall survival, less pain, and better preserved QoL than patients who received normal nursing. However, the patients with advanced NSCLC did not experience an emotional benefit from high-quality nursing compared to those in the normal nursing group.
Several clinical studies found that high-quality nursing has been utilized to manage patients with cancer.[16–18] The implementation of the new advanced cancer nursing role may have contributed to important improvements of QoL for cancer patients with gynaecological, haematological, Head & Neck and upper gastrointestinal cancers.[19] Consistently, outcomes in the current study demonstrated that high-quality nursing efficiently improved QoL and significantly decreased anxiety and depression scale for postoperative patients with advanced NSCLC. Oncology nurses must obtain knowledge and skills in primary palliative care to provide comprehensive cancer care, which may improve satisfaction and survival for cancer patients.[20] In this study, we observed that high-quality nursing contributed to the improvements of hospital stay and incidence of complications, as well as inflammation.
A study showed that comprehensive nursing is superior compared to the conventional nursing for patients with liver cancer.[21] Another study demonstrated that high-quality nursing alleviates adverse reactions and cancer pain for patients with lung cancer during the perioperative period.[16] Outcomes in this study found that high-quality nursing increased survival time and decreased mortality for NSCLC patients. The potential reasons to support a high-quality nursing could be related to the fact that nursing improved psychological states, which might lead to longer survival. Notably, high-quality nursing may be an efficient strategy, which might have significant clinical implication in the future for postoperative patients with advanced NSCLC.
5. Conclusion
In conclusion, the current analysis demonstrated that high-quality nursing significantly decreased postoperative hospital stay, incidence of complications, anxiety, and depression in postoperative patients with advanced NSCLC. Notably, high-quality nursing improved symptoms including pain, dyspnea and physical symptom burden and postoperative quality of life, survival rate, mortality rate and recurrence rate in postoperative patients with advanced NSCLC. However, the other benefits of high-quality nursing should further be confirmed in larger populations based on patients with advanced NSCLC.
Author contributions
MH W, YS and MH Z summarized experimental data, conducted data analysis and wrote the manuscript. RY Z and JF designed this study and revised manuscript. All authors read and approved the final manuscript.
Abbreviations:
- BMI =
- body mass index
- CES-D =
- Center for Epidemiologic Studies Depression scale
- DAS =
- Dental Anxiety Scale
- DS-GPA =
- Diagnosis-Specific Graded Prognostic Assessment
- NSCLC =
- nonsmall cell lung cancer
- QoL =
- assessment instrument
- QoL =
- quality of life
- SD =
- standard deviation
- SIS =
- The systemic inflammation score
- WHOQOL-100 =
- World Health Organization
How to cite this article: Wang M, Sun Y, Zhang M, Yu R, Fu J. Effects of high-quality nursing care on quality of life, survival, and recurrence in patients with advanced nonsmall cell lung cancer. Medicine 2022;101:37(e30569).
Funding: Not applicable.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate: The study was approved by the Ethical Community, Nursing School of Qiqihar Medical University. Informed consent was obtained from all participants. All methods were performed in accordance with relevant guidelines and regulations.
The authors declare that they have no competing interests.
Contributor Information
Minghuan Wang, Email: 377042531@qq.com.
Yang Sun, Email: sunyang@163.com.
Meihui Zhang, Email: meihuizhang@163.com.
Renzhi Yu, Email: zhang_sunclinical@163.com.
References
- [1].Marasovic Susnjara I. Lung cancer incidence and mortality in Split-Dalmatia County, 2003-2012. Cent Eur J Public Health. 2020;28:59–64. [DOI] [PubMed] [Google Scholar]
- [2].Yang H, Yao Z, Zhou X, et al. Survival and prognostic factors of lung cancer patients with preexisting connective tissue disease: a retrospective cohort study. Annal Trans Med. 2020;8:1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Junger ST, Schodel P, Ruess D, et al. Timing of development of symptomatic brain metastases from non-small cell lung cancer: impact on symptoms, treatment, and survival in the era of molecular treatments. Cancers. 2020;12:3618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hagiwara K, Harimoto N, Araki K, et al. Long-term survival of two patients with pancreatic cancer after resection of liver and lung oligometastases: a case report. Surgical Case Rep. 2020;6:309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kuroda H, Nakada T, Oya Y, Takahashi Y, Matsusita H, Sakakura N. Clinical adjustability of radiological tools in patients with surgically resected cT1N0-staged non-small-cell lung cancer from the long-term survival evaluation. J Thoracic Dis. 2020;12:6655–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Agarwal R, Epstein AS. Advance care planning and end-of-life decision making for patients with cancer. Semin Oncol Nurs. 2018;34:316–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Long FJ, Chen H, Wang YF, et al. Research on the effect of health care integration on patients’ negative emotions and satisfaction with lung cancer nursing activities. World J Clin Cases. 2020;8:4059–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ozdemir Koken Z, Sezer R, Tosun K. Nursing care of the patient with neurogenic bladder after kidney transplantation: a case report. Transplant Proc. 2019;51:2501–2. [DOI] [PubMed] [Google Scholar]
- [9].Abbott M, Ustoyev Y. Cancer and the immune system: the history and background of immunotherapy. Semin Oncol Nurs. 2019;35:150923. [DOI] [PubMed] [Google Scholar]
- [10].Li P, Guo YJ, Tang Q, Yang L. Effectiveness of nursing intervention for increasing hope in patients with cancer: a meta-analysis. Rev Lat Am Enfermagem. 2018;26:e2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ferrell B, Sun V, Hurria A, et al. Interdisciplinary palliative care for patients with lung cancer. J Pain Symptom Manage. 2015;50:758–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Cardoso da SD, Schwarz K, Fontanari AM, et al. WHOQOL-100 before and after sex reassignment surgery in Brazilian male-to-female transsexual individuals. J Sex Med. 2016;13:988–93. [DOI] [PubMed] [Google Scholar]
- [13].Chen YC, Lin KC, Wu CY, et al. Determinants of quality of life in the older residents of long-term care facilities using the world health organization international classification of functioning, disability and health framework in Taiwan. Disabil Rehabil. 2019:42:1–9. [DOI] [PubMed] [Google Scholar]
- [14].Chang Y, An H, Xu L, et al. Systemic inflammation score predicts postoperative prognosis of patients with clear-cell renal cell carcinoma. Br J Cancer. 2015;113:626–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Cai Y, Wang Y, Sun J, et al. Successful treatment of a patient with NSCLC carrying uncommon compound EGFR G719X and S768I mutations using osimertinib: a case report. J Int Med Res. 2020;48:300060520928793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Yu X, Liu J. Effects of high-quality nursing care for patients with lung cancer during the perioperative period: a protocol of systematic review of randomized controlled trials. Medicine. 2019;98:e18132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Olling K, Nyeng D, Wee L. Predicting acute odynophagia during lung cancer radiotherapy using observations derived from patient-centred nursing care. Tech Innovations Patient Support Radiation Oncol. 2018;5:16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Cowley A, Evans C, Bath-Hextall F, Cooper J. Patient, nursing and medical staff experiences and perceptions of the care of people with palliative esophagogastric cancer: a systematic review of the qualitative evidence. JBI Database Syst Rev Implement Rep. 2016;14:134–66. [DOI] [PubMed] [Google Scholar]
- [19].Westman B, Ullgren H, Olofsson A, Sharp L. Patient-reported perceptions of care after the introduction of a new advanced cancer nursing role in Sweden. Eur J Oncol Nursing. 2019;41:41–8. [DOI] [PubMed] [Google Scholar]
- [20].Dahlin C. Palliative care: delivering comprehensive oncology nursing care. Semin Oncol Nurs. 2015;31:327–37. [DOI] [PubMed] [Google Scholar]
- [21].Gou Y, Yi J, Jiang M, Cao C. Analysis on effects of comprehensive nursing care applied in interventional therapy for patients with liver cirrhosis and liver cancer. Iran J Public Health. 2019;48:494–500. [PMC free article] [PubMed] [Google Scholar]