Purpose:
This study investigated the effect of real-time feedback on the restoration of spontaneous circulation, survival to hospital discharge, and favorable functional outcomes after hospital discharge.
Methods:
PubMed, ScienceDirect, and China National Knowledge Infrastructure databases were searched to screen the relevant studies up to June 2020. Fixed-effects or random-effects model were used to calculate the pooled estimates of relative ratios (RRs) with 95% confidence intervals (CIs).
Results:
Ten relevant articles on 4281 cardiac arrest cases were identified. The pooled analyses indicated that real-time feedback did not improve restoration of spontaneous circulation (RR: 1.13, 95% CI: 0.92–1.37, and P = .24; I2 = 81%; P < .001), survival to hospital discharge (RR: 1.27, 95% CI: 0.90–1.79, and P = .18; I2 = 74%; P < .001), and favorable neurological outcomes after hospital discharge (RR: 1.09, 95% CI: 0.87–1.38; P = .45; I2 = 16%; P = .31). The predefined subgroup analysis showed that the sample size and arrest location may be the origin of heterogeneity. Begg’s and Egger’s tests showed no publication bias, and sensitivity analysis indicated that the results were stable.
Conclusion:
The meta-analysis had shown that the implementation of real-time audiovisual feedback was not associated with improved restoration of spontaneous circulation, increased survival, and favorable functional outcomes after hospital discharge.
Keywords: cardiac arrest, chest compression, feedback
1. Introduction
Chest compressions are an essential part of efficient cardiopulmonary resuscitation (CPR). Early implementation of high-quality chest compressions reduces mortality and improves favorable neurological outcomes.[1,2] High-quality chest compressions depend on appropriate rate and depth, full chest recoil, and minimal interruptions during chest compressions. However, numerous studies have demonstrated poor compliance with the recommended targets and wide variability in the quality of CPR in clinical practice.[3–5]
Real-time audiovisual feedback technology can provide information about the quality of chest compression components during training and in clinical practice, thus enhancing chest compression performance to meet the guidelines. In addition, training using a mannequin equipped with a computer-based real-time audiovisual feedback system improves the retention of CPR skills.[6]
Although real-time feedback was associated with greater ability to maintain high-quality chest compressions in simulation studies, the effect of real-time feedback on patient outcomes and survival after cardiac arrest remained controversial.[7,8] Several articles reported the effect of real-time feedback on patient outcomes and survival after cardiac arrest, but they varied in study designs, recruitment, and exclusion criteria and measurements.[9–18] Therefore, this study systematically evaluated the efficacy of feedback on patient outcomes and survival after cardiac arrest to provide an optimal plan for resuscitation.
2. Methods
2.1. Study design
This study was performed in accordance with the preferred reporting items for systematic reviews[19] and registered it in PROSPERO (CRD42020198279). Ethical approval and informed consent of patients are not required because this study was based on published studies and did not involve patients directly.
2.2. Literature search
PubMed, ScienceDirect, and China National Knowledge Infrastructure databases were searched to screen the relevant studies up to June 2020. The following keywords were used: “feedback” and “cardiac arrest” or “resuscitation.” In addition, we manually scanned the reference lists of several relevant reviews to select additional studies.
All included studies should meet the following criteria: evaluated the effect of feedback on the quality of chest compression; contained sufficient data for the assessment of relative ratios (RRs) with 95% confidence intervals (CIs). The exclusion criteria were as follows: duplicate reports, conference reports, theses, review papers, or animal studies and posters; repeated or overlapping publications.
2.3. Data extraction and quality assessment
Two reviewers independently performed data extraction from all the eligible publications using a redesigned form. The extracted information included the following: first author, year of publication, study design, study country, sample size, arrest location such as out-of-hospital cardiac arrest (OHCA) or in-hospital cardiac arrest (IHCA), monitoring equipment, and CPR providers. If the required data were missing, we attempted to contact the literature authors to ensure the accuracy of relevant information. Any disagreement was resolved by discussion or by consultation with a third author.
The quality of included studies was assessed using the Cochrane risk of bias tool for randomized controlled trials and Newcastle–Ottawa Scale for observational studies. All differing views was resolved by a third reviewer through discussion.
2.4. Statistical analysis
All statistical analyses were carried out using the Stata version 14 (StataCorp., College Station, TX), and the significance threshold was a 2-sided P < .05. The dichotomous variables were odds ratios with 95% CIs as effect indicators. Heterogeneity among the studies was tested by I2 statistic percentages and the Cochran Q chi-squared test. A random-effects model was used when P < .05 and I2 > 50%; otherwise, a fixed-effect model was applied. Subgroup analysis was used to explore the sources of heterogeneity. Sensitivity analysis was conducted to examine the robustness and stability of study findings. Publication and selection bias were investigated through funnel plots.
3. Results
3.1. Literature search
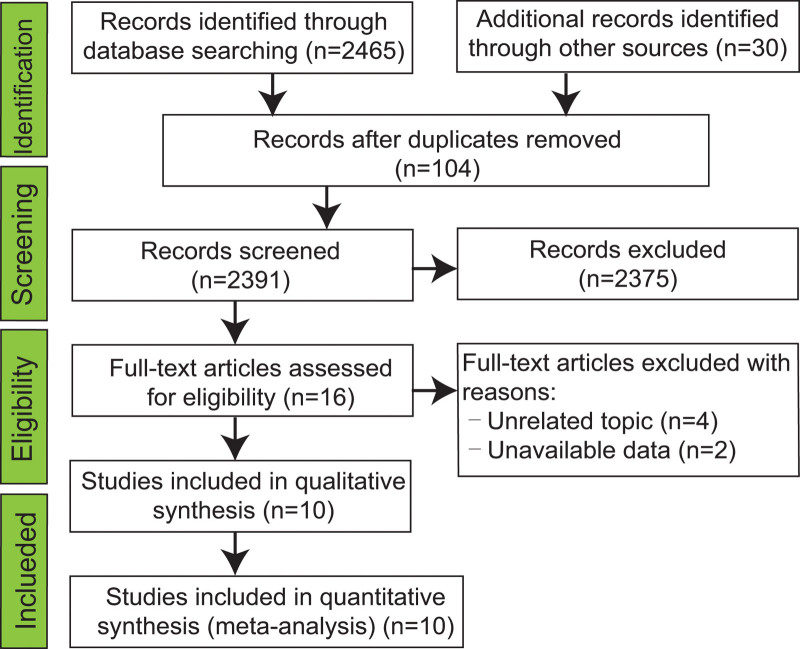
Figure 1 shows the specific procedure of article selection. In total, 2495 studies were searched for evaluation initially. After scanning the titles and abstracts, 104 duplicate and 2375 unrelated studies were excluded. The full texts of the remaining 16 articles were read, and 10 articles were finally enrolled in this meta-analysis.[9–18]
Figure 1.
Summary of the study selection process.
3.2. Characteristics of the included studies and quality assessment
Table 1 presents the characteristics of the included studies. Four studies were conducted in North America,[9,10,12,14] 4 in Europe,[11,15–17] and 2 in Asia.[13,18] Among the 10 studies, 9 reported the incidence of restoration of spontaneous circulation,[9–14,16–18] 9 assessed the rate of survival to discharge,[9–15,17,18] and 4 investigated the neurological outcomes after hospital discharge.[10,11,14,17] Quality assessment was performed based on the Cochrane risk of bias tool for randomized controlled trials. The Newcastle–Ottawa Scale results for the observational studies are presented in Tables S1–S3, Supplemental Digital Content 1, http://links.lww.com/MD/H253.
Table 1.
Characteristics of the included studies.
| Author (Year) | Study country | Study design | Sample size | Arrest location | Monitoring equipment | CPR providers |
|---|---|---|---|---|---|---|
| Abella et al, 2007 | USA | Historical case-control study | 156 | IHCA | Laerdal QCPR | Hospital resuscitation team |
| Bobrow et al, 2013 | USA | Prospective cohort study | 484 | OHCA | ZOLL E Series Defibrillator | Emergency medical technician |
| Couper et al, 2015 | United Kingdom | Prospective cohort study | 291 | IHCA | Phillips MRx QCPR defibrillator | Emergency medical technician |
| Crowe et al, 2015 | USA | Prospective cohort study | 101 | IHCA and OCHA | ZOLL R Series Defibrillator | Clinicians |
| Goharani et al, 2019 | Iran | Randomized controlled study | 900 | IHCA | Cardio first angel | Hospital resuscitation teams |
| Hostler et al, 2011 | USA and Canada | Randomized controlled study | 1586 | OCHA | Philips MRx QCPR defibrillator | Emergency medical service providers |
| Kramer-Johansen et al, 2006 | Norway, Sweden, and UK | Prospective cohort study | 241 | OCHA | Laerdal QCPR | Emergency medical service providers |
| Lakomek et al, 2020 | Germany | Prospective cohort study | 198 | OCHA | corpuls3 defibrillator | Emergency medical service providers |
| Sainio et al, 2013 | Finland | Prospective cohort study | 185 | OCHA | Philips MRx QCPR defibrillator | Helicopter emergency medical service providers |
| Vahedian-Azimi et al, 2020 | Iran | Randomized controlled study | 22 | IHCA | Cardio first angel | ICU nurses |
CPR = cardiopulmonary resuscitation, ICU = intensive care unit, IHCA = in-hospital cardiac arrest, OHCA = out-of-hospital cardiac arrest.
3.3. Restoration of spontaneous circulation
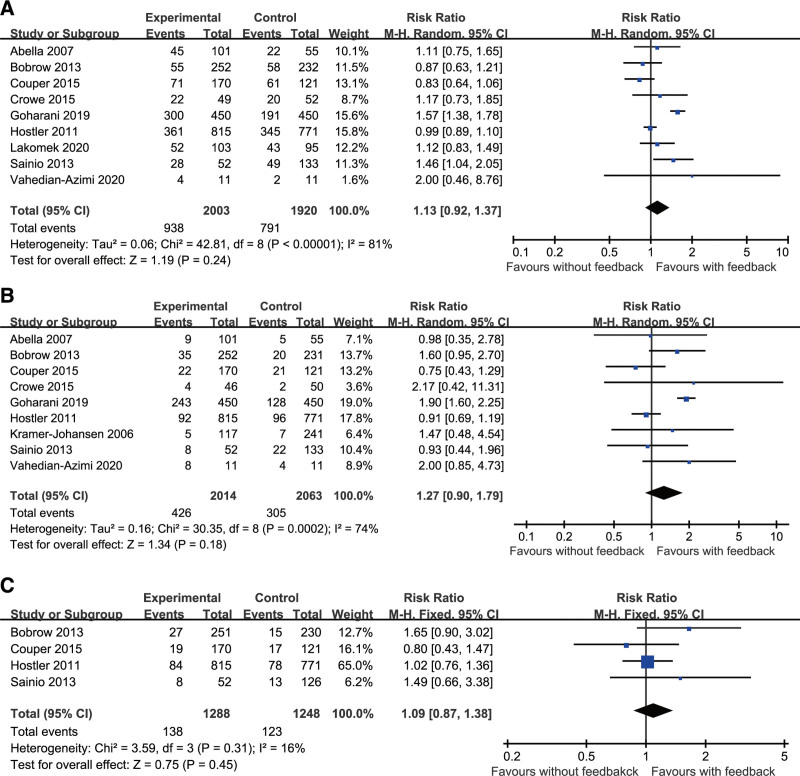
Heterogeneity (I2 = 81%, P < .001) was revealed in the 9 studies,[9–14,16–18] and in the random effects model, real-time feedback did not improve restoration of spontaneous circulation (RR: 1.13, 95% CI: 0.92–1.37; P = .24; Fig. 2A).
Figure 2.
Forest plot of studies reporting (A) restoration of spontaneous circulation, (B) survival to hospital discharge, and (C) favorable neurological outcomes after hospital discharge.
3.4. Survival to hospital discharge
Nine studies that enrolled 4077 patients evaluated the association of real-time feedback with survival to hospital discharge in cardiac arrest.[9–15,17,18] The forest plot with a random-effects model (I2 = 74%, P < .001) indicated that real-time feedback was not associated with survival to hospital discharge (RR: 1.27, 95% CI: 0.90–1.79; P = .18; Fig. 2B).
3.5. Favorable neurological outcome after hospital discharge
No evident heterogeneity (I2 = 16%; P = .31) was observed among the 4 studies.[10,11,14,17] The result obtained with a fixed-effect model indicated that real-time feedback was not associated with favorable neurological outcome after hospital discharge (RR: 1.09, 95% CI: 0.87–1.38; P = .45; Fig. 2E).
4. Subgroup analysis
Subgroup analysis was performed based on the severity of sample size and arrest location to identify the possible sources of heterogeneity (Table 2). Sample size and arrest location were causes of heterogeneity in the subgroup analysis.
Table 2.
Subgroup analysis.
| Heterogeneity factors | No. of studies | RR (95% CI) | P value | I2 (P value) | ||
|---|---|---|---|---|---|---|
| For ROSC | Sample size | ≥400 | 3 | 1.12 (0.78 − 1.62) | .532 | 94.0% (<.001) |
| <400 | 6 | 1.11 (0.91 − 1.35) | .323 | 39.5% (.142) | ||
| Arrest location | OHCA | 3 | 0.99 (0.90 − 1.09) | .868 | 0.0% (.541) | |
| OHCA/IHCA | 6 | 1.23 (0.93 − 1.62) | .151 | 77.2% (.001) | ||
| For survived to hospital discharge | Sample size | ≥400 | 3 | 1.40 (0.82 − 2.40) | .222 | 90.6% (<.001) |
| <400 | 6 | 1.05 (0.74 − 1.48) | .785 | 0.0% (.432) | ||
| Arrest location | OHCA | 4 | 1.09 (0.80 − 1.49) | .591 | 27.2% (.247) | |
| OHCA/IHCA | 5 | 1.39 (0.84 − 2.30) | .205 | 65.3% (.021) | ||
CI = confidence intervals, IHCA = in-of-hospital cardiac arrest, OHCA = out-of-hospital cardiac arrest, ROSC = restoration of spontaneous circulation, RR = relative ratio.
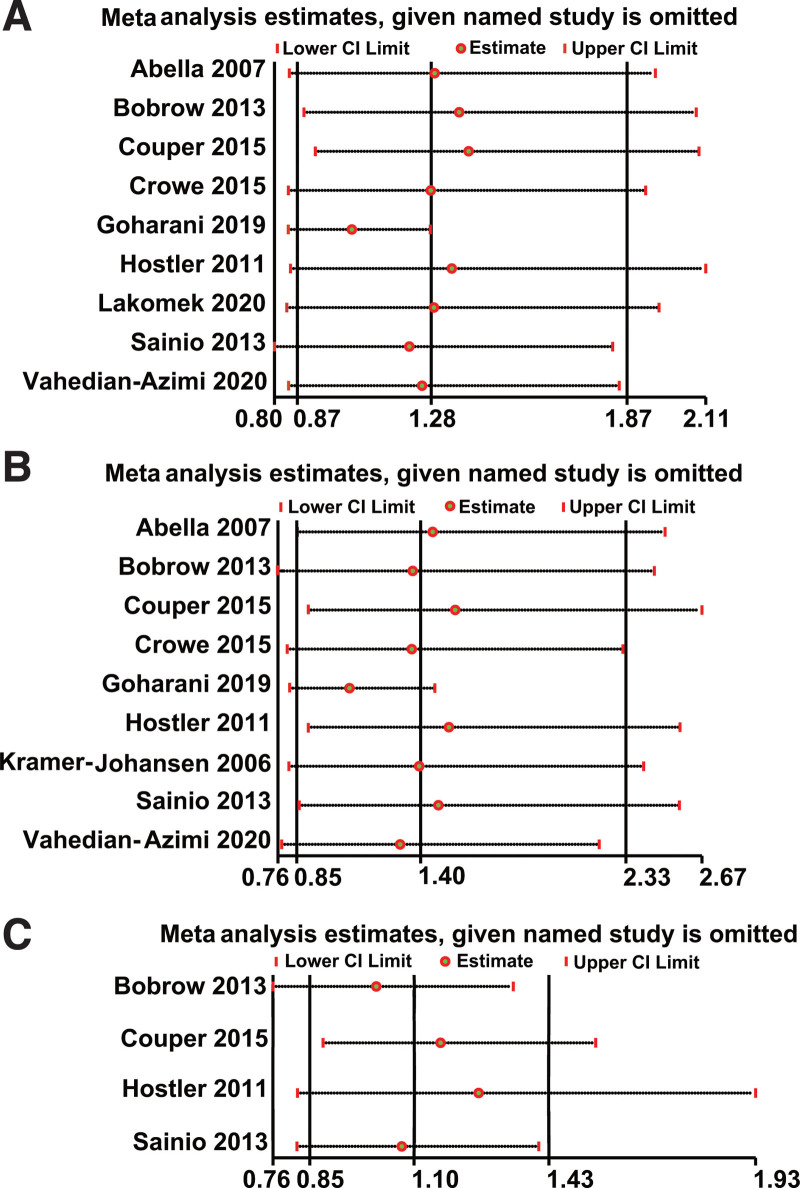
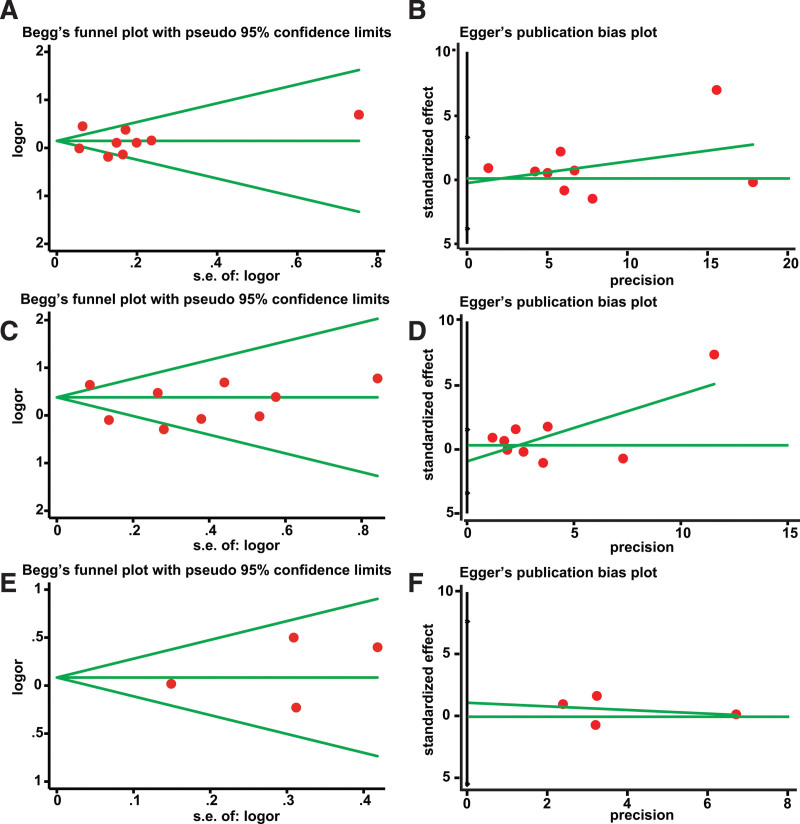
5. Sensitivity analysis and publication bias
To further confirm the robustness of the results, we conducted a sensitivity analysis, but no significant changes were observed in the outcomes (Fig. 3). Begg’s and Egger’s tests showed no publication bias for restoration of spontaneous circulation (P = .175, Fig. 4A; P = .873, Fig. 4B), survival to hospital discharge (P = .602, Fig. 4C; P = .404, Fig. 4D), and favorable neurological outcome after hospital discharge (P = 1.00, Fig. 4C; P = .558, Fig. 4F).
Figure 3.
Sensitivity analysis of pooled hazard ratios. (A) Restoration of spontaneous circulation, (B) survival to hospital discharge, and (C) favorable neurological outcomes after hospital discharge.
Figure 4.
Funnel plot of publication bias. (A) Restoration of spontaneous circulation, (B) survival to hospital discharge, and (C) favorable neurological outcomes after hospital discharge.
6. Discussion
The current systematic review and meta-analysis present the most recent and updated work summarizing the evidence for clinical outcomes with real-time feedback during chest compression. The meta-analysis had shown that implementation of real-time audiovisual feedback device was not associated with improved restoration of spontaneous circulation, increased survival, and favorable functional outcomes after hospital discharge, consistent with the results of a prior meta-analysis.[7]
Contrary to our findings, 2 previous studies demonstrated that real-time feedback was associated with improved CPR quality, increased survival, and favorable functional outcomes.[10,13] The observed effect of real-time feedback was verified, but they were caused by factors external to the interventions. First, the implementation of unfamiliar compression feedback device required training by a clinical resuscitation provider for its usage. We cannot rule out the possibility of feedback-off to feedback-on training effect, especially in a before-after study. Second, compression feedback device studies are blind to clinical resuscitation providers. Awareness of the monitoring of chest compression performance might have resulted in better effect than the actual results obtained without supervision.
The current guidelines[20,21] thus underline the importance of ensuring the adequate compression depth and fraction of time with active chest compression, because these factors are expected to lead to better hemodynamic perfusion and thus improve the patient outcomes.[22,23] A cluster randomized trial conducted by the Resuscitation Outcomes Consortium demonstrated that the use of real-time audiovisual feedback improved the mean compression depth by 2 mm and the chest compression fraction from 64% to 66%.[14] Thus, real-time audiovisual feedback induces changes in chest compression performance that may be extremely small to increase the chances of successful resuscitation.
Kramer–Johansen et al[15] reported the mostly positive rescuer comments on real-time feedback device; 89/103 (86%) of rescuers indicated that the device helped them perform CPR better. However, 18% of the CPR providers turned off the acoustic feedback because it was “distracting.” The psychological effects involved in CPR feedback are wide-ranging. Thus, the real-time feedback device must not be extremely complex.[24]
Notably, current scientific evidence alone is insufficient to support the complete abolition of the real-time feedback device. In a crowded setting of a cardiac arrest incident, the screen may be out of sight of the chest compression providers. Similarly, in the noisy setting of sudden emergency, the audio feedback information may not be heard by chest compression providers. In addition, we have limited knowledge about the effect of real-time feedback devices on mechanical injury, such as rib fractures, cardiac rupture, and hemopneumothorax, given the lack of reports in the included studies. Assessment of the capability of these real-time devices to improve patient outcomes should be withheld until the results of large randomized controlled trials become available.
Combining studies from different populations and backgrounds may have caused in some heterogeneity observed in this current meta-analysis. Specifically, this heterogeneity came from the OHCA/IHCA subgroup, which involved both patients who experienced IHCA or OHCA. The outcome of IHCA in general wards may differ from OHCA given the different clinical characteristics of these patient populations. In addition, small study effect has been reported earlier in the form of a larger and conforming association being reported in studies with smaller sample size, and increasing the sample size may produce different results. Although the heterogeneity existed between studies, the sensitivity analysis demonstrated that the results of our meta-analysis were stable.
Several limitations of our study should be mentioned. First, several small-sample-size studies were inevitably included in our analysis, which affected the credibility of the results. Second, the pooled data might be argued because all studies published in English. Third, all the studies were based on adult cardiac arrest. Although adult chest anatomy is similar to that of children, it is not exactly the same. Fourth, investigation of mechanical complications induced by chest compression should be encouraged.
7. Conclusion
Real-time feedback device does not ultimately translate to improved patient outcomes and survival after cardiac arrest. Certain doubts remain about the rationality of introducing such a system to clinical practice.
Author contributions
Conceptualization: Guang Wei Lv, Yong Li, Wen Jie Wang.
Data curation: Meng Zhang, Yi Zhang, Yuan Yuan Zhang.
Software: Shun Yi Feng.
Writing – original draft: Guang Wei Lv.
Writing – review & editing: Qing Chang Hu, Yong Li, Wen Jie Wang.
Supplementary Material
Abbreviations:
- CI =
- confidence interval
- CPR =
- cardiopulmonary resuscitation
- IHCA =
- in-hospital cardiac arrest
- OHCA =
- out-of-hospital cardiac arrest
- RR =
- relative ratio
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Supplemental Digital Content is available for this article.
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
How to cite this article: Lv GW, Hu QC, Zhang M, Feng SY, Li Y, Zhang Y, Zhang YY, Wang WJ. Effect of real-time feedback on patient’s outcomes and survival after cardiac arrest: A systematic review and meta-analysis. Medicine 2022;101:37(e30438).
Contributor Information
Guang Wei Lv, Email: lgw5726@hotmail.com.
Qing Chang Hu, Email: huqingchang20@126.com.
Meng Zhang, Email: crbyyhlb@sina.com.
Shun Yi Feng, Email: shunyi1058@hotmail.com.
Yong Li, Email: ly13333367871@hotmail.com.
Yi Zhang, Email: crbyyhlb@sina.com.
Yuan Yuan Zhang, Email: crbyyhlb@sina.com.
References
- [1].Sasson C, Rogers MA, Dahl J, et al. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. [DOI] [PubMed] [Google Scholar]
- [2].Gallagher EJ, Lombardi G, Gennis P. Effectiveness of bystander cardiopulmonary resuscitation and survival following out-of-hospital cardiac arrest. JAMA. 1995;274:1922–5. [PubMed] [Google Scholar]
- [3].Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293:305–10. [DOI] [PubMed] [Google Scholar]
- [4].Niles DE, Duval-Arnould J, Skellett S, et al. Characterization of pediatric in-hospital cardiopulmonary resuscitation quality metrics across an international resuscitation collaborative. Pediatr Crit Care Med. 2018;19:421–32. [DOI] [PubMed] [Google Scholar]
- [5].JamaKim HT, Kim JG, Jang YS, et al. Comparison of in-hospital use of mechanical chest compression devices for out-of-hospital cardiac arrest patients: AUTOPULSE vs LUCAS. Medicine (Baltim). 2019;98:e17881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Wik L, Myklebust H, Auestad BH, et al. Twelve-month retention of CPR skills with automatic correcting verbal feedback. Resuscitation. 2005;66:27–30. [DOI] [PubMed] [Google Scholar]
- [7].Kirkbright S, Finn J, Tohira H, et al. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation. 2014;85:460–71. [DOI] [PubMed] [Google Scholar]
- [8].An M, Kim Y, Cho WK. Effect of smart devices on the quality of CPR training: a systematic review. Resuscitation. 2019;144:145–56. [DOI] [PubMed] [Google Scholar]
- [9].Abella BS, Edelson DP, Kim S, et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007;73:54–61. [DOI] [PubMed] [Google Scholar]
- [10].Bobrow BJ, Vadeboncoeur TF, Stolz U, et al. The influence of scenario-based training and real-time audiovisual feedback on out-of-hospital cardiopulmonary resuscitation quality and survival from out-of-hospital cardiac arrest. Ann Emerg Med. 2013;62:47–56.e1. [DOI] [PubMed] [Google Scholar]
- [11].Couper K, Kimani PK, Abella BS, et al. The system-wide effect of real-time audiovisual feedback and postevent debriefing for in-hospital cardiac arrest: the cardiopulmonary resuscitation quality improvement initiative. Crit Care Med. 2015;43:2321–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Crowe C, Bobrow BJ, Vadeboncoeur TF, et al. Measuring and improving cardiopulmonary resuscitation quality inside the emergency department. Resuscitation. 2015;93:8–13. [DOI] [PubMed] [Google Scholar]
- [13].Goharani R, Vahedian-Azimi A, Farzanegan B, et al. Real-time compression feedback for patients with in-hospital cardiac arrest: a multi-center randomized controlled clinical trial. J Intensive Care. 2019;7:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hostler D, Everson-Stewart S, Rea TD, et al. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. BMJ. 2011;342:d512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kramer-Johansen J, Myklebust H, Wik L, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71:283–92. [DOI] [PubMed] [Google Scholar]
- [16].Lakomek F, Lukas RP, Brinkrolf P, et al. Real-time feedback improves chest compression quality in out-of-hospital cardiac arrest: a prospective cohort study. PLoS One. 2020;15:e0229431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Sainio M, Kämäräinen A, Huhtala H, et al. Real-time audiovisual feedback system in a physician-staffed helicopter emergency medical service in Finland: the quality results and barriers to implementation. Scand J Trauma Resusc Emerg Med. 2013;21:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Vahedian-Azimi A, Rahimibashar F, Miller AC. A comparison of cardiopulmonary resuscitation with standard manual compressions versus compressions with real-time audiovisual feedback: a randomized controlled pilot study. Int J Crit Illn Inj Sci. 2020;10:32–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Escobedo MB, Aziz K, Kapadia VS, et al. 2019 American Heart Association focused update on neonatal resuscitation: an update to the American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2019;140:e922–30. [DOI] [PubMed] [Google Scholar]
- [21].Panchal AR, Berg KM, Hirsch KG, et al. 2019 American heart association focused update on advanced cardiovascular life support: use of advanced airways, vasopressors, and extracorporeal cardiopulmonary resuscitation during cardiac arrest: an update to the American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2019;140:e881–94. [DOI] [PubMed] [Google Scholar]
- [22].Edelson DP, Abella BS, Kramer-Johansen J, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006;71:137–45. [DOI] [PubMed] [Google Scholar]
- [23].Vadeboncoeur T, Stolz U, Panchal A, et al. Chest compression depth and survival in out-of-hospital cardiac arrest. Resuscitation. 2014;85:182–8. [DOI] [PubMed] [Google Scholar]
- [24].Bohn A, Gude P. Feedback during cardiopulmonary resuscitation. Curr Opin Anaesthesiol. 2008;21:200–3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.