Background:
To explore the risk factors of bile duct injury in laparoscopic cholecystectomy (LC) in China through meta-analysis.
Methods:
The study commenced with a search and selection of case–control studies on the risk factors for bile duct injury in LC in China using the following databases: PubMed, EMBASE, ScienceNet.cn, CNKI, Wanfang Data, and VIP. Data were extracted from the collected documents independently by 2 researchers, following which a meta-analysis of these data was performed using Revman 5.3.
Results:
The compilation of all data from a total of 19 case–control studies revealed that among 41,044 patients, 458 patients experienced bile duct injury in LC, accounting for the incidence rate of 1.12% for bile duct injury. The revealed risk factors for bile duct injury were age (≥40 years) (odds ratio [OR] = 6.23, 95% CI [95% confidence interval]: 3.42–11.33, P < .001), abnormal preoperative liver function (OR = 2.01, 95% CI: 1.50–2.70, P < .001), acute and subacute inflammation of gallbladder (OR = 8.35, 95% CI: 5.32–13.10, P < .001; OR = 4.26, 95% CI: 2.73–6.65, P < .001), thickening of gallbladder wall (≥4 mm) (OR = 3.18, 95% CI: 2.34–4.34, P < .001), cholecystolithiasis complicated with effusion (OR = 3.05, 95% CI: 1.39–6.71, P = .006), and the anatomic variations of the gallbladder triangle (OR = 11.82, 95% CI: 6.32–22.09, P < .001). However, the factors of gender and overweight (body mass index ≥ 25 kg/m2) were not significantly correlated with bile duct injury in LC.
Conclusions:
In the present study, age (≥40 years), abnormal preoperative liver function, gallbladder wall thickening, acute and subacute inflammation of the gallbladder, cholecystolithiasis complicated with effusion, and anatomic variations of the gallbladder triangle were found to be closely associated with bile duct injury in LC.
Keywords: bile duct injury, China, laparoscopic cholecystectomy, risk factors
1. Introduction
Cholecystolithiasis (gallstones) is a common surgical disease, with a high incidence rate of up to 10.1% in China, where diet and the living habits of people change continually. Cholesterol stones are the main type of gallstones. Laparoscopic cholecystectomy (LC) is becoming increasingly popular in China. Since its inception in the early the 1990s in China, LC has developed for more than 2 decades and is now used widely at all levels in the hospitals of the country. Moreover, advancements in laparoscopic techniques and equipment allow surgeries with a small wound, slight pain, and little interference to the abdominal viscera as well as rapid recovery, enabling LC to gradually surpass open cholecystectomy and open minicholecystectomy to become the preferred choice for gallbladder removal.
Cholecystectomy, once considered to have several risk factors, mainly dangerous pathology, dangerous anatomy, and dangerous surgery, is currently the most common iatrogenic factor for bile duct injury. Most bile duct injuries occur in LC.[1] The reported rate of occurrence of bile duct injuries in LC is approximately 0.5% to 0.85%,[2–4] which is 2 to 3 times greater than that in open cholecystectomy. Bile duct injuries may lead to biliary peritonitis, traumatic bile duct strictures, recurrent cholangitis, biliary cirrhosis, portal hypertension, and even liver failure, and could prove to be fatal in extreme cases.[5] Despite the evident advantages of LC, such accompanying damage cannot be ignored. In certain cases, multiple operations and endoscopic therapy still cannot treat bile duct injury, which not only reduces the patients’ quality of life, increases their economic burden, and often leads to doctor-patient disputes and medical lawsuits. Indeed, the prevention of iatrogenic bile duct injury is an inevitable eternal area of concern in the clinical field of hepatobiliary surgery, for which the analysis of the risk factors for bile duct injury in LC is of great significance.
In China, LC is used widely in hospitals at provincial, municipal, and county levels. However, the incidence of bile duct injury reported by hospitals at all levels is quite different. The units that have recently introduced LC should attach great importance to the safety issue of bile duct injury. The present study involved a meta-analysis of the reported risk factors for bile duct injuries in LC in China to provide evidence for corresponding prevention.
2. Methods
2.1. Search strategy
A systematic search for studies in the literature was performed in PubMed, EMBASE, ScienceNet.cn, CNKI, Wanfang Data, and VIP databases. The search was performed independently by 2 researchers by using the following keywords: LC, bile duct injury, risk factors, and China. All the studies retrieved from these databases were included in the present study irrespective of the publication date.
2.2. Study criteria and selection
Inclusion criteria: All published studies on the risk factors for bile duct injuries in LC in China; The study subjects were patients who had experienced bile duct injuries in the LC; and The study was designed as a case–control or randomized controlled study of the included works of the literature. Exclusion criteria: Repeatedly published documents; Documents with incomplete data; or Reviews, conference abstracts, basic research documents, and documents in which research objects were not Chinese people. Studies that fulfilled any of these exclusion criteria were not included in the present study. Two researchers independently screened and selected the suitable research papers with integrated data, first by title and abstract, then through full text, and finally through manual retrieval. Whether to include a paper in the present study was decided after deliberation and discussion. In case of disagreement on the decision between the 2 researchers, a third senior researcher was requested to participate in the discussion and undertake the final decision. The study protocol was approved by the Ethics Committee of the Second Affiliated Hospital of Kunming Medical University.
2.3. Data extraction and literature quality assessment
Two researchers independently searched for and extracted data in accordance with the inclusion and exclusion criteria. Any disagreement was resolved through mutual discussion or discussion with a third senior researcher. The extracted data included the first author, sample size, publication date, and the risk factors for bile duct injuries in LC. Each study was assessed for quality and rated by assigning stars in each domain in accordance with the guidelines of the Newcastle-Ottawa Scale (NOS). The studies that received 5 or more stars out of 9 stars on the NOS scale were included in the present study.
2.4. Meta-analysis
The meta-analysis was performed for eligible studies using Review Manager 5.3 (International Cochrane Collaboration, Northern Europe), with the dichotomous variables expressed as odds ratio (OR) with 95% CI (95% confidence interval). Furthermore, Cochran Q test and I2 test were performed to assess heterogeneity across the included studies. In the test results, P > .1 and I2 < 50% indicated little heterogeneity among the studies; therefore, a fixed-effects model was preferred, while P < .1 and I2 > 50% indicated a statistically significant heterogeneity and a random-effects model was adopted. Finally, a funnel plot symmetry test was performed to assess the possibility of publication bias in the meta-analysis.
3. Results
3.1. Search results
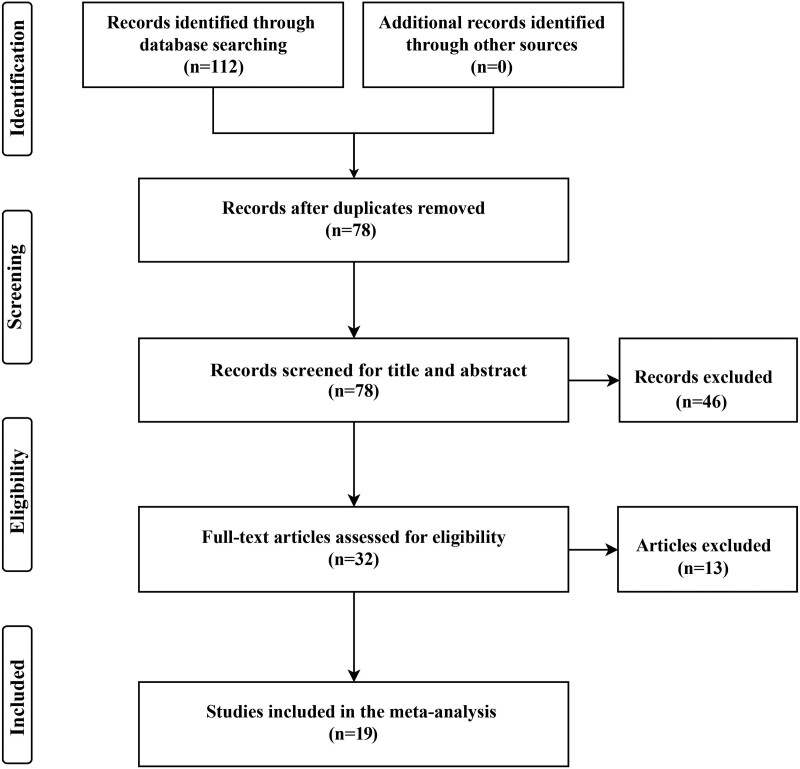
The database search with keywords retrieved 112 documents, including 34 duplicates that were filtered later. Among the remaining 78 documents, 32 documents that matched the quality filter were selected first by screening the titles and abstracts and, subsequently, the full texts, providing 19 studies that were finally included in the meta-analysis. These studies involved 41,044 patients, among which 458 patients had experienced bile duct injuries in LC, accounting for a prevalence of 1.12% for bile duct injuries. Figure 1 illustrates the process of selection of the 19 studies, which were all case–control studies published between 1992 and 2019. The literature quality assessment rated 1 paper with 5 stars, 4 papers with 6 stars, 5 papers with 7 stars, 6 papers with 8 stars, and 3 papers with 9 stars. Refer to Table 1 for the included papers.
Figure 1.
Literature search flow chart.
Table 1.
Characteristics of the included studies.
| Author/year | Article number | Study design | Sample (B/T) | Study start and end date | Risk factors | NOS scores |
|---|---|---|---|---|---|---|
| Chen, 2013[22] | 1671-8194 (2013) 09-0227-02 | C | 29/1612 | 2000.10–2011.12 | ①④⑤⑧ | 7 |
| He, 2019[8] | 10.3760/cma.j.issn.1674-4756.2019.04.008 | C | 50/7984 | 2010.02–2018.02 | ①⑤⑧ | 7 |
| Jiang, 2016[23] | 1674-361X (2016) 10-0063-02 | C | 8/1350 | 2007.03–2016.03 | ①②⑦ | 6 |
| Jin, 2017[24] | 10.19528/j.issn.1003-3548.2017.09.040 | C | 34/568 | 2011.07–2016.07 | ①②④⑦⑧ | 8 |
| Li, 2016[25] | Not mentioned | C | 21/383 | 2013.01–2015.05 | ①②④⑦⑧ | 8 |
| Long, 2015[26] | 10.3969/j.issn.1671-8348.2015.02.027 | C | 16/1244 | 2003.12–2013.12 | ①④⑥⑦⑧ | 8 |
| Peng, 2019[27] | 10.3969/j.issn.2095-140X.2019. 07. 016 | C | 36/800 | 2014.05–2018.07 | ①②③④⑥⑦⑧ | 9 |
| Sun, 2011[28] | 1009-9905(2011)11-0902-02 | C | 14/799 | 2005.01–2011.01 | ①⑦ | 6 |
| Tong, 2012[29] | 1674-4721(2012)04(a)-0039-02 | C | 16/160 | 2010.02–2011.10 | ① | 5 |
| Wang, 2011[14] | 1005-2208(2011)07-0591-03 | C | 41/4531 | 1999.10–2010.12 | ①④⑤⑧ | 9 |
| Wang, 2015[30] | 1673-016X (2015)06-0077-03 | C | 16/2541 | 2010.01–2014.02 | ①⑤⑧ | 7 |
| Wang, 2017[31] | 1671-0126(2017)01-0032-03 | C | 6/764 | 2006.03–2016.06 | ①⑤⑥⑧ | 7 |
| Wang, 2018[32] | 1009-6612(2018)12-0898-03 | C | 28/608 | 2010.01–2016.12 | ①③⑥⑧ | 8 |
| Wang, 2020[7] | 10.14163/j.cnki.11-5547/r.2020.06.023 | C | 40/300 | 2016.07–2019.09 | ①④⑥⑦⑧ | 8 |
| Wu, 2013[33] | 1674-4721(2013)08(a)-0185-02 | C | 25/859 | 2008.01–2012.12 | ①②⑦ | 6 |
| Yang, 2017[34] | 10.15887/j.cnki.13-1389/r.2017.20.118 | C | 6/300 | 2014.08–2015.08 | ①②⑥⑦ | 6 |
| Yuan, 2013[35] | 1007-1989(2013)05-0492004 | C | 12/985 | 2005-2012 | ①⑧ | 7 |
| Zhong, 2019[36] | 1009-5519(2019)06-0833-04 | C | 15/4013 | 2013.01–2018.01 | ①⑤⑥⑧ | 8 |
| Zhou, 2016[6] | 10.3760/cma.j.issn.1007-8118.2016.09.010 | C | 45/11,243 | 1992.10–2013.12 | ①③⑥⑧ | 9 |
Risk factors = ① Gender; ② Age; ③ BMI; ④ Liver function; ⑤ Cholecystitis; ⑥ Gallbladder wall thickness; ⑦ Cholecystolithiasis with effusion; ⑧ Anatomical variation of the gallbladder triangle.
B = bile duct injury, BMI = body mass index, C = case–control study, NOS = Newcastle-Ottawa Scale, T = total cases.
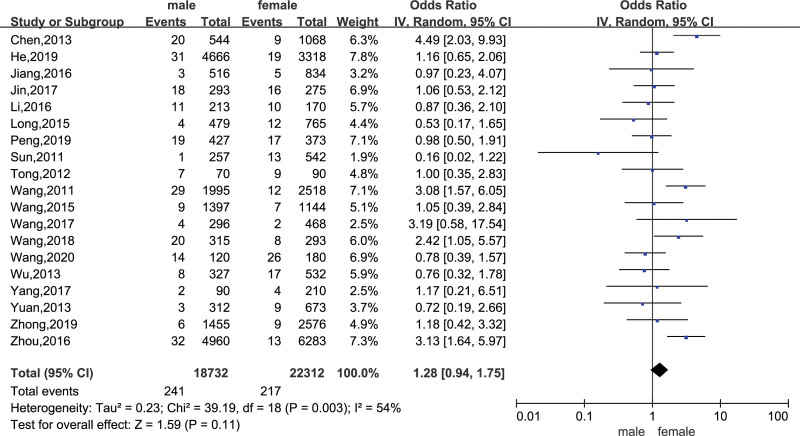
3.2. Gender
There are 19 studies reporting the influence of sex on bile duct injury during LC, including 41,044 patients. The heterogeneity test I2 = 54%, P = .003. It is considered that there is heterogeneity among the groups included in the study; therefor, a random-effects model combined analysis was adopted. The results suggest that the gender difference is not related to the occurrence of bile duct injury in LC (OR = 1.28, 95% CI: 0.94–1.75, P = .11) (Fig. 2).
Figure 2.
A forest plot of meta-analysis of the correlation between gender and bile duct injury in LC. CI = confidence interval, LC = laparoscopic cholecystectomy, OR = odds ratio.
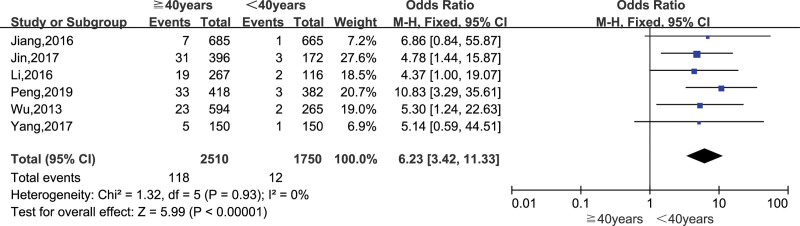
3.3. Age
There are 6 literature reports on the influence of age (≥40 years) on bile duct injury in LC. The heterogeneity test I2 = 0%, P = .93, indicating that there was no heterogeneity among the studies, and the fixed-effects model was used for combined analysis. The results suggest that patients over 40 years of age have an increased risk of bile duct in LC (OR = 6.23, 95% CI: 3.42–11.33, P < .001) (Fig. 3).
Figure 3.
A meta-analysis forest plot of the correlation between age and bile duct injury in LC. CI = confidence interval, LC = laparoscopic cholecystectomy, OR = odds ratio.
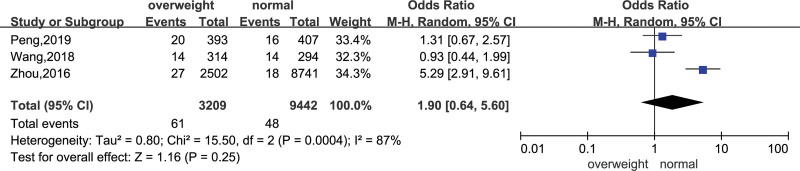
3.4. Overweight
There are 3 papers analyzed the influence of overweight (body mass index (BMI) ≥ 25 kg/m2) on bile duct injury during LC, including 12,651 patients. Heterogeneity test I2 = 87%, P = .001. It is considered that there is heterogeneity among the studies. And use random-effects model to merge analysis. The results suggest that being overweight (BMI ≥ 25 kg/m2) is not related to the occurrence of bile duct injury in LC (OR = 1.90, 95% CI: 0.64–5.60, P = .25) (Fig. 4).
Figure 4.
A meta-analysis forest plot of the correlation between BMI and bile duct injury in LC. BMI = body mass index, CI = confidence interval, LC = laparoscopic cholecystectomy, OR = odds ratio.
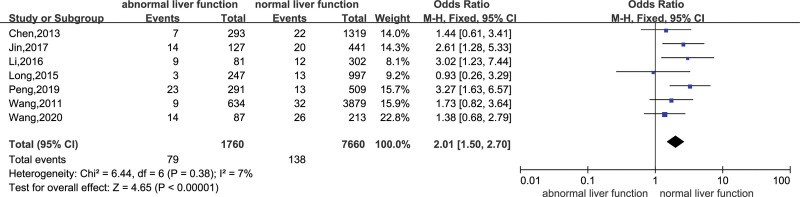
3.5. Abnormal preoperative liver function
Seven studies reported on the relationship between preoperative liver function and LC bile duct injury. Heterogeneity test I2 = 7%, P = .38. It is considered that the heterogeneity between the studies was small, and the fixed-effects model was used for combined analysis. The results suggest that patients with abnormal liver function before surgery have an increased risk of bile duct injury in LC (OR = 2.01, 95% CI: 1.50–2.70, P < .001) (Fig. 5).
Figure 5.
Forest plot of meta-analysis of the correlation between preoperative liver function and bile duct injury in LC. CI = confidence interval, LC = laparoscopic cholecystectomy, OR = odds ratio.
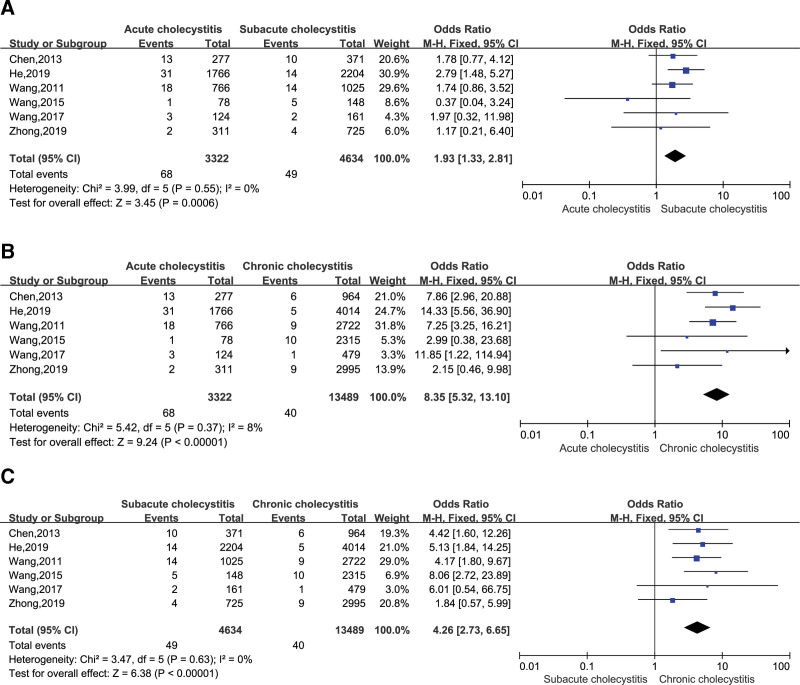
3.6. Cholecystitis
There are 6 literature reports on the relationship between the stages of gallbladder inflammation (acute, subacute, chronic) and bile duct injury in LC. Compared with the acute and subacute phases, the heterogeneity between studies was small (I2 = 0%, P = .55), using a fixed-effect model combined analysis, the acute phase increased the risk of bile duct injury in LC (OR = 1.93, 95% CI: 1.33–2.81, P < .001) (Fig. 6A). Compared with the acute phase and the chronic phase, the heterogeneity among the studies was small (I2 = 8%, P = .37). The fixed-effect model was used for the combined analysis. The acute phase increased the risk of bile duct injury in LC (OR = 8.35, 95% CI: 5.32–13.10, P < .001) (Fig. 6B). Compared with the subacute and chronic phases, the heterogeneity among the studies was small (I2 = 0%, P = .63). The fixed-effect model was used for the combined analysis. The subacute phase increased the risk of bile duct injury in LC (OR = 4.26, 95% CI: 2.73–6.65, P < .001) (Fig. 6C).
Figure 6.
(A) Comparing acute cholecystitis with subacute cholecystitis, meta-analysis forest diagram of the correlation between acute cholecystitis and bile duct injury in LC. CI = confidence interval, LC = laparoscopic cholecystectomy, OR = odds ratio. (B) Comparing acute cholecystitis with chronic cholecystitis, a forest plot of meta-analysis of the relationship between acute cholecystitis and bile duct injury in LC. CI = confidence interval, LC = laparoscopic cholecystectomy, OR = odds ratio. (C) Comparison of subacute cholecystitis and chronic cholecystitis, forest plot of meta-analysis of the relationship between subacute cholecystitis and in LC. CI = confidence interval, LC = laparoscopic cholecystectomy, OR = odds ratio.
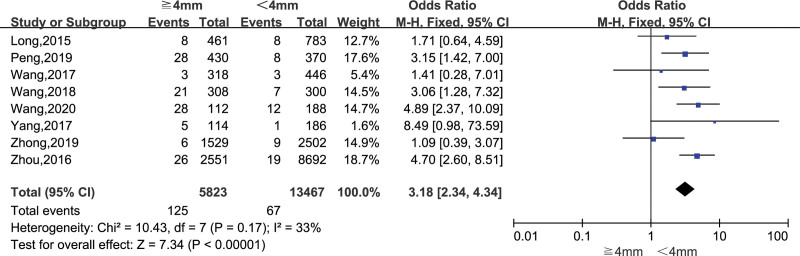
3.7. Thickening of gallbladder wall
Eight papers analyzed the relationship between gallbladder wall thickness (≥4 mm) and bile duct injury during LC. Heterogeneity test I2 = 33%, P = .17. It is considered that the heterogeneity between the studies is small, and a fixed effect is adopted. The results suggest that when the gallbladder wall thickens ≥4 mm, the risk of bile duct injury in LC is increased (OR = 3.18, 95% CI: 2.34–4.34, P < .001) (Fig. 7).
Figure 7.
Forest plot of meta-analysis of the relationship between gallbladder wall thickness and bile duct injury in LC. CI = confidence interval, LC = laparoscopic cholecystectomy, OR = odds ratio.
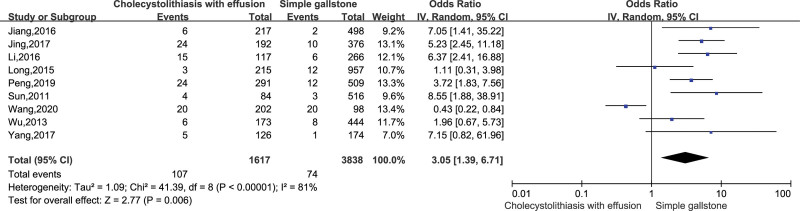
3.8. Cholecystolithiasis complicated with effusion
There are 9 literature reports on the effect of simple gallbladder stones and gallbladder stones combined with fluid accumulation on bile duct injury in LC. The heterogeneity test I2 = 81% and P < .001, indicating that the heterogeneity between studies was relatively large, and the random effect model was adopted to combine the effect amount and analyze. The results showed that patients with gallbladder stones and fluid accumulation increased the risk of intraoperative bile duct injury (OR = 3.05, 95% CI: 1.39–6.71, P = .006) (Fig. 8).
Figure 8.
A forest plot of meta-analysis of the correlation between gallbladder stones and fluid accumulation and bile duct injury in LC. CI = confidence interval, LC = laparoscopic cholecystectomy, OR = odds ratio.
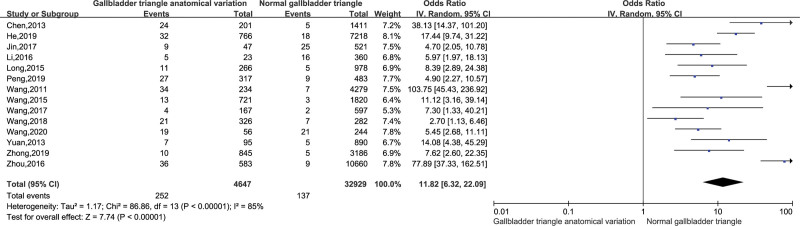
3.9. Anatomical variation of the gallbladder triangle
There are 14 papers analyzing the influence of the anatomical variation of the gallbladder triangle on bile duct injury during LC. The heterogeneity test I2 = 85%, P < .001. It is considered that there is heterogeneity among the studies, and the random-effects model is used for combined analysis. The results suggest that the anatomical variation of the gallbladder triangle increases the risk of bile duct injury in LC (OR = 11.82, 95% CI: 6.32–22.09, P < .001) (Fig. 9).
Figure 9.
Forest plot of meta-analysis on the relationship between gallbladder triangle anatomic variation and bile duct injury in LC. CI = confidence interval, LC = laparoscopic cholecystectomy, OR = odds ratio.
3.10. Sensitivity test
The sensitivity test showed that research data of Zhou DJ[6] showed the greatest heterogeneity in the meta-analysis of the influence of overweight (BMI ≥ 25 kg/m2) on bile duct injury during LC. After excluding the research data, the effect size was recombined. The final result did not substantially change, but the heterogeneity decreased significantly (I2 = 0%, P = .51). The research data of Wang JG[7] has the greatest heterogeneity in the meta-analysis of the correlation between gallbladder stones with effusion and bile duct injury in LC. After excluding the research data, the effect size was recombined. The final results did not change, but the heterogeneity significantly decreased (I2 = 19%, P = .28). In the meta-analysis of the impact of cholecystitis on bile duct injury in LC, the acute phase increased the risk of bile duct injury in LC compared with the subacute phase (OR = 1.93, 95% CI: 1.33–2.81, P < .001). However, after eliminating the research data of He YP[8] to merge effect quantity, acute cholecystitis did not increase the risk of bile duct injury (OR = 1.54, 95% CI: 0.96 2.48, P = .07). Therefore, comparing acute cholecystitis with subacute cholecystitis, we cannot conclude that acute cholecystitis increases the risk of bile duct injury in LC.
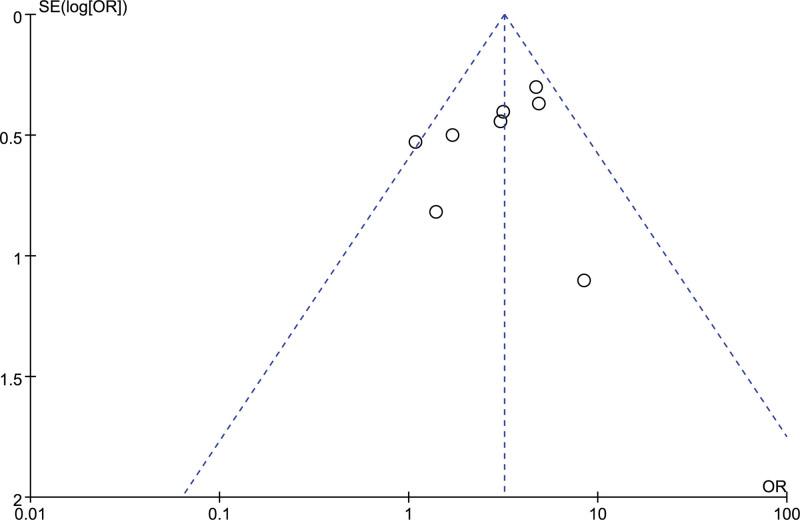
3.11. Publication bias
Based on the thickness of the gallbladder wall to evaluate the publication bias of the included studies and draw a funnel chart, the images are basically symmetrical, indicating that the meta-analysis results are less likely to have publication bias, so the conclusions obtained are relatively reliable (Fig. 10).
Figure 10.
Funnel chart for meta-analysis.
4. Discussion
Advanced laparoscopic equipment and sophisticated surgical techniques have enabled LC to become the preferred choice of surgery for gallbladder removal among Chinese people. However, an increasing number of bile duct injuries reported in LC is a major concern. The incidence of bile duct injury in China in this study was 1.12%, which is much higher than that reported in Belgium (0.37%)[9] and Italy (0.42%).[10] Therefore, bile duct injury represents one of the most severe complications of LC, and if not managed effectively, may progress into a condition requiring liver transplantation rather than a simple cholecystectomy.[11] Halbert et al[12] reported that 0.8% of patients with bile duct injuries after LC require liver transplantation, causing great inconvenience to the patients and possible disputes with the doctors. In this context, identification and analysis of the risk factors for bile duct injuries in LC is of great significance. The meta-analysis conducted in the present study revealed age (≥40 years), gallbladder wall thickening (≥4 mm), abnormal preoperative liver function, gallbladder inflammation, gallbladder stone with effusion, and anatomic variations of the gallbladder triangle as the risk factors for bile duct injury in LC, while the factors of gender and overweight (BMI ≥ 25 kg/m2) were not associated with such associations.
The meta-analysis did not reveal any significant difference in the incidence of bile duct injuries in LC between men and women (OR = 1.28, 95% CI: 0.94–1.75, P = .11), which was inconsistent with the findings of previous studies. Grönroos et al[13] had reported that the probability of women experiencing bile duct injuries was higher as their abdominal organs and tissues exhibit better elasticity and relaxation compared to those of men. In female patients undergoing LC, the gallbladder is pulled to bring the common bile duct to the risk area and place it parallel to the cystic duct. In this process, the common bile duct may be easily mistaken to be a continuation of the cystic duct and be removed. On the contrary, other studies[14] have suggested a higher probability of injuries in men as the majority of them are reluctant to undergo surgery until they have had several episodes of acute inflammation, which might be followed by thickening of the gallbladder wall and severe cholecystitis adhesion, ultimately increasing the incidence of bile duct injuries in LC. This view was corroborated by the findings of Giger et al,[15] who reported “male gender” as an independent risk factor for bile duct injury. Moreover, older age (≥40 years) was reported to increase the risk of LC-related bile duct injuries (OR = 6.23, 95% CI: 3.42–11.33, P < .001). In China, most individuals aged above 40 perform heavy work, meanwhile failing to receive timely medical treatment when cholecystolithiasis with acute cholecystitis occurs, or even when they are diagnosed with cholecystolithiasis through a physical examination and have indications for surgery, early surgery is not performed until the disease worsens and leads to a higher risk of intraoperative bile duct injuries. The afore-stated study included 3 research papers that reported the influence of the overweight factor (BMI ≥ 25 kg/m2) on bile duct injuries among 12,651 patients who underwent LC, demonstrating independence between the 2 (OR = 1.90, 95% CI: 0.64–5.60, P = .25). Generally, there is an increase in the amount of adipose tissue in the gallbladder triangle of overweight subjects, which may be the reason for the increased amount of bleeding and interference in surgical exposure. However, with the proficiency of laparoscopic operation, the increase of adipose tissue at the gallbladder triangle did not increase the incidence of bile duct injury in LC.
The present study revealed that patients exhibiting abnormal liver function prior to LC were at a higher risk of bile duct injury (OR = 2.01, 95% CI: 1.50–2.70, P < .001), and that the abnormal preoperative liver function might be a result of cholecystolithiasis with acute cholecystitis or Mirrizi syndrome, which were also reported to be associated with an increased risk of bile duct injury in LC. The degree of abnormality of preoperative liver function reflected the severity of cholecystolithiasis with acute cholecystitis or Mirrizi syndrome. Therefore, it is necessary to monitor the changes in preoperative liver function value and to spread awareness among people regarding the risk associated with it. Cholecystitis, an independent risk factor for bile duct injury in LC,[16] may lead to adhesion at the gallbladder triangle and disorder of the local anatomical structure. Söderlund et al[17] conducted a prospective study and reported an increased risk of bile duct injuries in patients with acute cholecystitis. In a study, Blohm et al[18] suggested that the optimal time to receive LC for acute cholecystitis was within 2 days upon admission. The study was fundamentally consistent with the study by Söderlund and suggested that, in comparison to chronic inflammation, acute and subacute inflammation of gallbladder led to a higher probability of experiencing bile duct injuries following LC. The present study, together with several previous studies, concluded that the optimal duration for gallbladder removal is chronic inflammation of the gallbladder or within 2 days upon admission for acute cholecystitis. In addition, the anatomic variations of the gallbladder triangle were recognized as a risk factor for LC-related bile duct injury.[19,20] Approximately 70% to 80% of iatrogenic bile duct injuries occur because of the incorrect identification of biliary tract anatomical structure,[21] and anatomic variations render it difficult to distinguish between the cystic duct, the common hepatic duct, and the common bile duct. Bile duct variations are diverse, with the parallel or spiral confluence of the cystic duct and the common hepatic duct being the most common cause of bile duct injury. The meta-analysis results revealed that the risk of bile duct injuries in LC was increased by 11.82 folds in patients with anatomic variations of the gallbladder triangle, compared to those without anatomic variations (OR = 11.82, 95% CI: 6.32–22.09, P < .001). Therefore, anatomic variations of the gallbladder triangle should be considered an important factor in this regard. The thickness of the gallbladder wall is another factor that reflects the severity of gallbladder inflammation. With an increase in the thickness of the gallbladder wall, the severity of congestion and edema increases, and the use of electrocoagulation hemostasis and electrocoagulation separation becomes longer, leaving the patient at a higher risk of thermal injury to the bile duct and its vessels. The present study confirmed that gallbladder wall thickening (≥4 mm) increased the risk of bile duct injury in LC (OR = 3.18, 95% CI: 2.34–4.34, P < .001). Furthermore, it was revealed that patients with cholecystolithiasis complicated with effusion might be at a higher risk of bile duct injury in LC than in those with simple cholecystolithiasis (OR = 3.05, 95% CI: 1.39–6.71, P = .006). This may have occurred because, in cholecystolithiasis complicated with effusion, the gallbladder is enlarged, and the stones may be located in the cystic duct or incarcerated in the Hartmann bag, predisposing the patients to damage in the common liver duct or the right hepatic duct.
Nevertheless, the present study had certain limitations. First, the study included only published Chinese literature, so there is a possibility of selection bias. Second, the eligible studies were of low quality. Third, all the included studies were case–control studies and may, therefore, present publication bias. Therefore, careful interpretation of the results of the present study is recommended. In addition, high-quality and randomized controlled trials with large sample sizes are required for further confirmation of these results.
5. Conclusion
The meta-analysis revealed age (≥40 years), abnormal preoperative liver function, gallbladder wall thickening, acute and subacute inflammation of the gallbladder, cholecystolithiasis complicated with effusion, and anatomic variations of the gallbladder triangle were found to be closely associated with bile duct injury in LC. Early identification of these risk factors is necessary to increase awareness of the risk associated with surgery and prevent the incidence of bile duct injury. However, despite the above-stated advantages, the present study had certain limitations. For example, the study was supported by inadequate research evidence on the risk factors for bile duct injury in LC. Since the conclusions may include bias errors, further research is required to verify the correlation of these risk factors with bile duct injury in LC.
Author contributions
Conceptualization: Shaohua Yang, Xiaohui Gu, Xiaowen Zhang.
Data curation: Shaohua Yang, Sheng Hu, Xiaohui Gu.
Formal analysis: Shaohua Yang, Xiaowen Zhang.
Funding acquisition: Xiaowen Zhang.
Writing – original draft: Shaohua Yang, Xiaohui Gu, Xiaowen Zhang.
Writing – review & editing: Shaohua Yang, Xiaohui Gu, Xiaowen Zhang.
Abbreviations:
- 95% CI =
- 95% confidence interval
- LC =
- laparoscopic cholecystectomy
- OR =
- odds ratio
The datasets generated during and/or analyzed during the current study are publicly available.
This research was supported by the Yunnan Provincial “Famous Doctors” Training Fund Project (Human Resources and Social Security Department of Yunnan Province [2018] No. 73).
The authors have no conflicts of interest to disclose.
How to cite this article: Yang S, Hu S, Gu X, Zhang X. Analysis of risk factors for bile duct injury in laparoscopic cholecystectomy in China: A systematic review and meta-analysis. Medicine 2022;101:37(e30365).
Contributor Information
Shaohua Yang, Email: kunyiysh@163.com.
Sheng Hu, Email: hushengkunyi@163.com.
Xiaohui Gu, Email: guxiaohuikunyi@163.com.
References
- [1].Feng X, Dong J. Surgical management for bile duct injury. Biosci Trends. 2017;11:399–405. [DOI] [PubMed] [Google Scholar]
- [2].Mangieri CW, Hendren BP, Strode MA, et al. Bile duct injuries (BDI) in the advanced laparoscopic cholecystectomy era. Surg Endosc. 2019;33:724–30. [DOI] [PubMed] [Google Scholar]
- [3].Lau WY, Lai EC, Lau SH. Management of bile duct injury after laparoscopic cholecystectomy: a review. ANZ J Surg. 2010;80:75–81. [DOI] [PubMed] [Google Scholar]
- [4].Zhao YP, Jiang HC. General Surgery. Version 2. Beijing, China: People’s Medical Publishing House[M], 2014:264. [Google Scholar]
- [5].Bauer TW, Morris JB, Lowenstein A, et al. The consequences of a major bile duct injury during laparoscopic cholecystectomy. Gastrointest Surg. 1998;2:61–6. [DOI] [PubMed] [Google Scholar]
- [6].Zhou DJ, Bai FJ, Han BQ, et al. Risk factors associated with bile duct injury after laparoscopic cholecystectomy (in Chinese). Chin J Hepatobiliary Surg. 2016;22:614–7. [Google Scholar]
- [7].Wang JG, Gong GJ, Sun LX. Study on risk factors of bile duct injury in patients with laparoscopic cholecystectomy (in Chinese). China Prac Med. 2020;15:52–4. [Google Scholar]
- [8].He YP, Di WD. Analysis of risk factors for bile duct injury after laparoscopic cholecystectomy (in Chinese). Chin J Pract Med. 2019;46:25–7. [Google Scholar]
- [9].Van de Sande S, Bossens M, Parmentier Y, et al. National survey on cholecystectomy related bile duct injury--public health and financial aspects in Belgian hospitals--1997. Acta Chir Belg. 2003;103:168–80. [DOI] [PubMed] [Google Scholar]
- [10].Nuzzo G, Giuliante F, Giovannini I, et al. Bile duct injury during laparoscopic cholecystectomy: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg. 2005;140:986–92. [DOI] [PubMed] [Google Scholar]
- [11].Parrilla P, Robles R, Varo E, et al. Liver transplantation for bile ductinjury after open and laparoscopic cholecystectomy. Br J Surg. 2014;101:63–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Halbert C, Altieri MS, Yang J, et al. Long-term outcomes of patients with common bile duct injury following laparoscopic cholecystectomy. Surg Endosc. 2016;30:4294–9. [DOI] [PubMed] [Google Scholar]
- [13].Grönroos JM, Hämäläinen MT, Karvonen J, et al. Is male gender a risk factor for bile duct injury during laparoscopic cholecystectomy. Langenbecks Arch Surg. 2003;388:261–4. [DOI] [PubMed] [Google Scholar]
- [14].Wang H, Luo JG, Liang P, et al. Analysis of risk factors for bile duct injury during laparoscopic cholecystectomy (in Chinese). Chin J Pract Surg. 2011;31:591–3. [Google Scholar]
- [15].Giger U, Ouaissi M, Schmitz SF, et al. Bile duct injury and use of cholangiography during laparoscopic cholecystectomy. Br J Surg. 2011;98:391–6. [DOI] [PubMed] [Google Scholar]
- [16].Georgiades CP, Mavromatis TN, Kourlaba GC, et al. Is inflammation a significant predictor of bile duct injury during laparoscopic cholecystectomy? Surg Endosc. 2008;22:1959–64. [DOI] [PubMed] [Google Scholar]
- [17].Söderlund C, Frozanpor F, Linder S. Bile duct injuries at laparoscopic cholecystectomy: a single-institution prospective study. Acute cholecystitis indicates an increased risk. World J Surg. 2005;29:987–93. [DOI] [PubMed] [Google Scholar]
- [18].Blohm M, Österberg J, Sandblom G, et al. The sooner, the better? The importance of optimal timing of cholecystectomy in acute cholecystitis: data from the national Swedish registry for gallstone surgery, GallRiks. J Gastrointest Surg. 2017;21:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Vidrio Duarte R, Martínez Martínez AS, Ortega León LH, et al. Transillumination of Calot’s triangle on laparoscopic cholecystectomy: a feasible approach to achieve a critical view of safety. Cureus. 2020;12:e9113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Shang P, Liu B, Li X, et al. A practical new strategy to prevent bile duct injury during laparoscopic cholecystectomy. A single-center experience with 5539 cases. Acta Cir Bras. 2020;35:e202000607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Chehade M, Kakala B, Sinclair JL, et al. Intraoperative detection of aberrant biliary anatomy via intraoperative cholangiography during laparoscopic cholecystectomy. ANZ J Surg. 2019;89:889–94. [DOI] [PubMed] [Google Scholar]
- [22].Chen LF. Analysis of influencing factors of bile duct injury in laparoscopic cholecystectomy (in Chinese). Guide China Med. 2013;11:227–8. [Google Scholar]
- [23].Jiang DC. Observation on the risk factors of bile duct injury in laparoscopic cholecystectomy and prevention measures (in Chinese). China’s Rural Health. 2016;20:63–5. [Google Scholar]
- [24].Jin MM. Analysis of related risk factors for bile duct injury during laparoscopic cholecystectomy (in Chinese). Clin Med. 2017;37:79–81. [Google Scholar]
- [25].Li RK, Li BJ, Wu BB. Analysis of risk factors for bile duct injury caused by laparoscopic cholecystectomy (in Chinese). Jilin Med J. 2016;37:1360–2. [Google Scholar]
- [26].Long SL, Yang H, Gu C, et al. Study on related risk factors of bile duct injury in laparoscopic cholecystectomy (in Chinese). Chongqing Med. 2015;44:224–225 + 228. [Google Scholar]
- [27].Peng XR, Wang P, Jiang YM, et al. Analysis of risk factors for bile duct injury after laparoscopic cholecystectomy (in Chinese). Med Pharm J Chin PLA. 2019;31:68–71. [Google Scholar]
- [28].Sun K. Analysis of factors related to biliary tract injury in laparoscopic cholecystectomy (in Chinese). Chin J Curr Adv Gen Surg. 2011;14:902–3. [Google Scholar]
- [29].Tong Q. Analysis of related factors of bile duct injury caused by cholecystectomy (in Chinese). China Modern Med. 2012;19:39–41. [Google Scholar]
- [30].Wang TM, Cao JW, Li DL, et al. Analysis of factors affecting bile duct injury during laparoscopic cholecystectomy and prevention strategies (in Chinese). J Hunan Normal Univ (Med Sci). 2015;12:77–9. [Google Scholar]
- [31].Wang B. Analysis of risk factors for bile duct injury during laparoscopic cholecystectomy (in Chinese). J Shanxi Med College Continuing Educ. 2017;27:32–4. [Google Scholar]
- [32].Wang JJ, Xie H. Risk factors of bile duct injury after laparoscopic cholecystectomy (in Chinese). J Laparoscopic Surg. 2018;23:898–900. [Google Scholar]
- [33].Wu W. Analysis of risk factors related to bile duct injury in laparoscopic cholecystectomy (in Chinese). China Modern Med. 2013;20:185–6. [Google Scholar]
- [34].Yang B. Analysis of related risk factors affecting bile duct injury during laparoscopic cholecystectomy (in Chinese). Chin J Clin Rational Drug Use. 2017;10:172–3. [Google Scholar]
- [35].Yuan DH, Chen YJ, Wei HB, et al. Analysis of risk factors for biliary tract injury induced by laparoscopic cholecystectomy (in Chinese). China J Endoscopy. 2013;19:492–5. [Google Scholar]
- [36].Zhong H, Wu XJ, Li SY, et al. Clinical study on diagnosis and treatment of iatrogenic bile duct injury related to laparoscopic cholecystectomy (in Chinese). 2019;35:833–836 + 840. [Google Scholar]