Background:
Glenoid baseplate failure is one of the causes of revision and poor outcomes in reverse shoulder arthroplasty (RSA). The objective of this study was to determine whether alterations in surgical technique can improve time-zero fixation of the baseplate in varying bone densities. A secondary objective was to identify whether preoperative radiographic glenoid sclerosis width was associated with the implementation of these techniques.
Methods:
This study included a biomechanical analysis and a retrospective radiographic review. The biomechanical portion describes 2 alterations to the standard surgical technique (under-preparation [A1] or over-preparation [A2] of the central screw pilot hole) and determined their torque-compression relationship via bone-substitute blocks with varying densities. Patients who underwent the described technical alterations were identified from a registry database of primary RSAs performed between 2007 and 2020. These patients were matched to patients who underwent the standard surgical technique, and preoperative radiographs were compared. Interrater reliability testing was performed to determine reproducibility.
Results:
With respect to the biomechanical arm, the average compressive force of the baseplate in the low-density block model when using the standard technique was 112 N compared with 300 N for the A1 technique (p = 0.01). In the high-density bone model, the standard technique resulted in failure to seat the baseplate, or screw breakage. Performing the A2 technique, the baseplate was seated without failure, with an average compressive force of 450 N. In the clinical arm, retrospective intraoperative video review for use of the alternative techniques found 20 shoulders in the “low-density” cohort and 21 in the “high-density” cohort. There was a significant difference in the glenoid sclerosis thickness between the experimental and matched control groups in our “high-density” cohort (p = 0.0014). The interrater reliability coefficient was found to be 0.69 for the “low-density” glenoid sclerosis thickness measurement and 0.92 for the “high-density” measurement.
Conclusions:
In low- and high-density bone models, alterations in surgical technique significantly improved compression and improved the ability to successfully seat the glenoid baseplate. Preoperative radiographs can assist in indicating the alternative technique in the sclerotic glenoid.
Clinical Relevance:
Utilization of these techniques intraoperatively will improve time-zero fixation of the glenoid baseplate and potentially avoid failure of fixation.
Early in the history of reverse shoulder arthroplasty (RSA), glenoid-sided complications were an often-cited cause of failure1-6. However, with improved implant design, baseplate failure has decreased, going from one of the most common types of failure to one of the least common7,8. Nevertheless, baseplate failure has not been completely eliminated. A recent meta-analysis evaluating aseptic loosening of the glenoid baseplate demonstrated that the complication occurred in 1.16% of all RSAs9. Although the rate of glenoid-sided failure is low, continued attention should be directed to improving baseplate integrity given the potentially devastating consequences of failure10.
Glenoid baseplate failure occurs because of a lack of osseous ingrowth about the baseplate. This lack of ingrowth leads to micromotion about the implant-bone interface and increased stress, which may lead to implant failure and, oftentimes, the need for revision surgery11. In a study of failed RSAs, Frankle and Pupello utilized a scanning electron microscope and found that a lack of osseous ingrowth on the underside of the baseplate was associated with failure11. Proper osseous ingrowth depends on the stability of initial fixation of the baseplate. Extensive work has been devoted to elucidating the optimal implant design to maximize initial stability12-18. Implants that utilize a central screw enable the assessment of initial fixation via the required torque to fully seat the screw. Therefore, emphasis on the required torque to generate sufficient fixation to avoid mechanical failure has been of interest.
The quality of implant fixation is affected by different bone densities19-21, with greater bone densities allowing for fixation methods that differ from those for glenoids that are less dense22. This difference is seen during glenoid fixation of a baseplate with a central screw, where variations to surgical technique have been implemented for varying bone densities to increase time-zero stability. The decision to employ these variations in the past was made intraoperatively based on time-zero perception of bone quality, such as the resistance to the drill, the torque when inserting the tap, and the torque when seating the baseplate. However, variation in surgical technique to improve the initial fixation of a baseplate with a central screw has not clearly been described.
The primary objective of the current study was to determine whether alterations in surgical technique can improve time-zero fixation of the glenoid baseplate in varying bone densities. The secondary objective was to identify whether glenoid sclerosis width on preoperative radiographs was associated with the implementation of these techniques. To determine the efficacy of these novel techniques, a previously described testing methodology for assessing the torque-compression relationship was utilized with a bone surrogate testing model including 3 densities to mimic low-, normal-, and high-density bone23. In addition, we sought to identify a cohort of patients among whom an alteration in the standard technique of bone preparation for baseplate insertion had occurred. Within this cohort, we sought to determine whether differences in preoperative radiographic glenoid sclerosis width could be utilized to aid in the surgeon’s decision to utilize an alternative technique for glenoid baseplate insertion.
Materials and Methods
Biomechanical
In this study, we utilized a monoblock RSA glenoid baseplate with a central 6.5 × 30-mm compression screw (RSP [Reverse Shoulder Prosthesis]; DJO Global). Porous polyurethane bone-substitute blocks (Pacific Research Laboratories) were used as bone surrogates, with 3 varying densities to represent low-density bone (20 PCF, density 0.32 g/cm3; model #1522-12), normal-density bone (30 PCF, density 0.48 g/cm3; model #1522-04), and high-density bone (50 PCF, density 0.8 g/cm3; model #1522-27). This bone substitute has been studied previously and determined to have modulus, density, and strength similar to their appropriate cancellous bone (low-, normal-, and high-density bone)24,25. An epoxy resin sheet (model #3401-03; Pacific Research Laboratories), which was reamed to match the radius of curvature for the glenoid baseplate, was utilized to mimic contact between the undersurface of the baseplate and the surface of the glenoid.
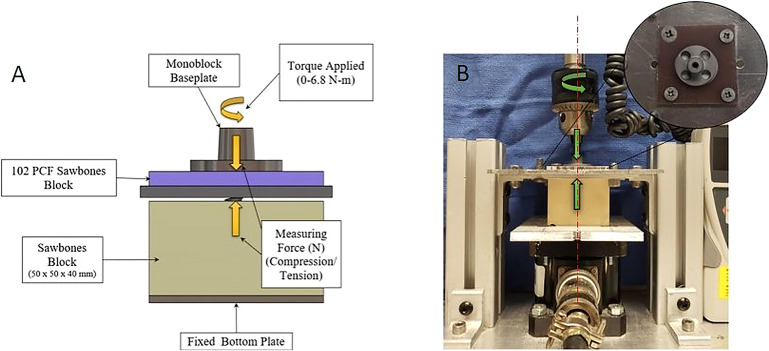
A total of 35 bone-substitute blocks were utilized. Block sizes were all standardized to a size of 50 × 50 × 40 mm, and the central pilot hole was placed directly in the center of the block with the use of a drill press. The test was repeated 5 times per technique per bone group. The alternative technique for low-density bone (A1) and the standard technique were performed on the low-density 20-PCF bone block. The alternative technique for high-density bone (A2) and the standard technique were performed on the high-density 50-PCF bone block. All 3 techniques were also performed on the normal-density, 30-PCF bone block. A previously published model (Fig. 1) was utilized to measure compression via a 6-DOF (degrees of freedom) load cell apparatus (MC3A-1,000 lb; 0.2% accuracy; AMTI Transducers)23,26-29.
Fig. 1.
A detailed illustration of the biomechanical testing model (Fig. 1-A) and the actual experimental setup (Fig.1-B) are shown. Tension forces equate inversely in a 1:1 fashion to compression forces via the third law of Newtonian physics. The digital torque meter (HTGS-85, 0.5% accuracy; Imada) was used to measure torque while seating the glenoid baseplate. Torque and compression were noted at increments of 1.1 Nm (10 in-lbf) to a maximum torque of 6.8 Nm (60 in-lbf). This end point was chosen on the basis of previous in vivo studies of surgeon-experienced tactile feedback while implanting this glenoid baseplate1,30. Datapoints were collected via a custom program in LabVIEW (National Instruments). Gross material deformation (“stripping”), screw breakage, and implant seating were noted; final compression and torque were recorded when there was failure to achieve the end point of 6.8 Nm (60 in-lbf). (Reproduced, with modification from, Diaz MA, Garrigues GE, Ricchetti ET, Gutierrez S, Frankle MA. Relationship between insertion torque and compression strength in the reverse total shoulder arthroplasty baseplate. J Orthop Res. 2020 Apr;38[4]:871-9. Epub 2019 Nov 25. © 2019 Orthopaedic Research Society. Published by Wiley Periodicals, Inc. Reproduced with permission.)
Standard and Alternative Techniques
The standard technique utilized for implanting the chosen glenoid baseplate was that according to the manufacturer’s surgical technique guide (DJO Global). This standard technique was employed for all 3 bone-surrogate densities.
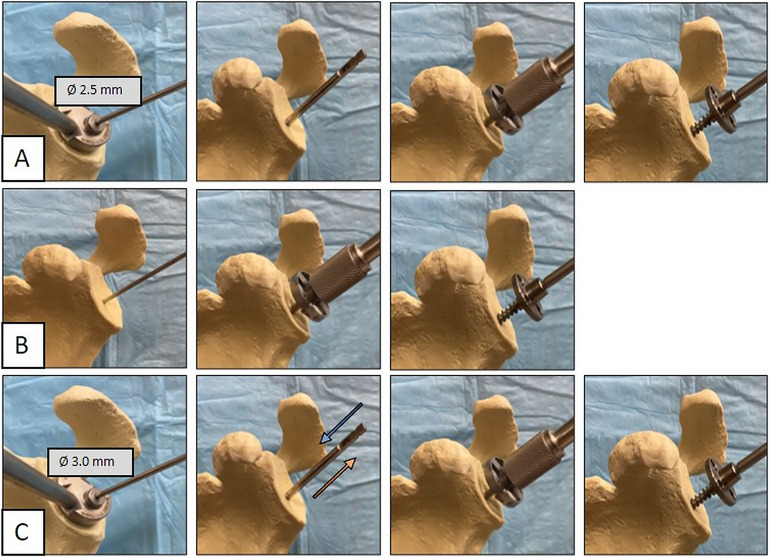
Alternative techniques were developed for low-density and high-density bone quality. See Figure 2 for details of all 3 techniques.
Fig. 2.
Standard and alternative techniques. Fig. 2-A The standard technique involves the insertion of a 2.5-mm guidewire for the central pilot hole to a depth of 30 mm, followed by use of a 6.5-mm guide-tap, reaming of the glenoid, and finally, insertion of a monoblock baseplate. Fig. 2-B The low-density alteration (A1) also begins with the use of a 2.5-mm guidewire for the pilot hole. The glenoid is then reamed over the guidewire, and the monoblock baseplate is inserted without the use of a guide-tap. Fig. 2-C The high-density alteration (A2). This follows the steps of the standard technique, but a 3.0-mm drill is used for the pilot hole, and the guide-tap is passed (inserted and removed) a total of 3 times.
Clinical
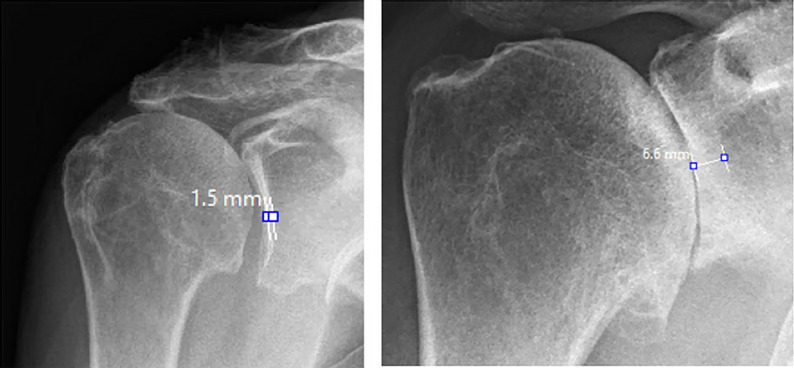
Institutional review board approval was acquired prior to the initiation of the study. Patients were selected from a registry database of primary RSAs performed over a 13-year period (January 2007 to May 2020) at a single tertiary referral center. Exclusion criteria were revision shoulder arthroplasty, the absence of an intraoperative video, and unavailable preoperative imaging. The 2 groups were selected among patients with a preoperative diagnosis of osteoarthritis, rotator cuff tear arthropathy, and fracture sequelae. The 2 patient groups were categorized as “low-density” and “high-density.” Intraoperative videos for each patient were reviewed in real time. Utilization of the standard technique for implantation of the glenoid baseplate, alteration in surgical technique as shown in Figure 2, and aberration in the surgical procedure leading to the alternative technique being utilized (screw stripping, screw breakage) were recorded. Preoperative Grashey-view radiographs of the operative shoulder were reviewed, and glenoid sclerosis thickness was measured via the picture archiving and communication system (PACS, MedVIEW; Aspyra). At the midway point of the glenoid, the subchondral sclerosis thickness was measured as the distance from the articular margin to the point where the opacity of the sclerotic margin diminished to that of the uniform glenoid vault (Fig. 3). The glenoid sclerosis thickness measurement was repeated by a second reviewer for reliability testing. An age and sex-matched control group from the registry for whom the standard technique was successfully utilized was created for comparison.
Fig. 3.
Measurement of subchondral sclerosis thickness about the midportion of the glenoid on preoperative radiographs.
Statistical Analysis
Using the pilot data, a large effect size (1.5) was used for an a priori power analysis. A total sample size of 35 (5 blocks per testing group) was necessary to power the study at 0.86 (G*Power, version 3.1.9.2; Heinrich Heine Universität Düsseldorf).
Normality was tested with a Shapiro-Wilk test, and subsequently, parametric tests were used to analyze data. A paired t test was used within each bone-block model to compare alternative techniques. For the clinical evaluation, independent t tests were performed (alpha = 0.05). The reliability of the radiographic measurements of glenoid sclerosis thickness was assessed using the intraclass correlation coefficient. Data are presented as the mean and standard deviation (SD). All statistical operations were performed using SPSS (version 22; IBM).
Source of Funding
No funding was received for this project.
Results
Biomechanical Arm
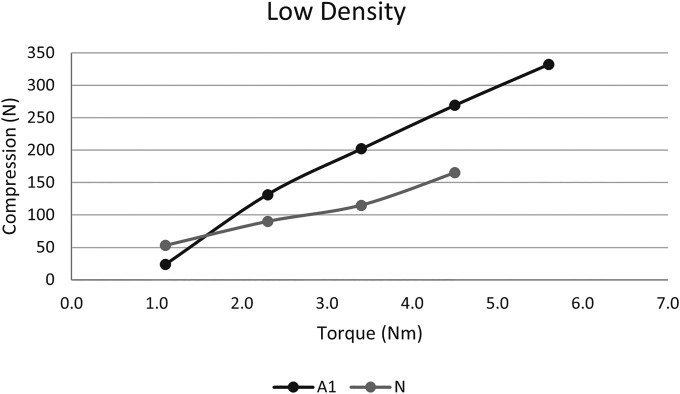
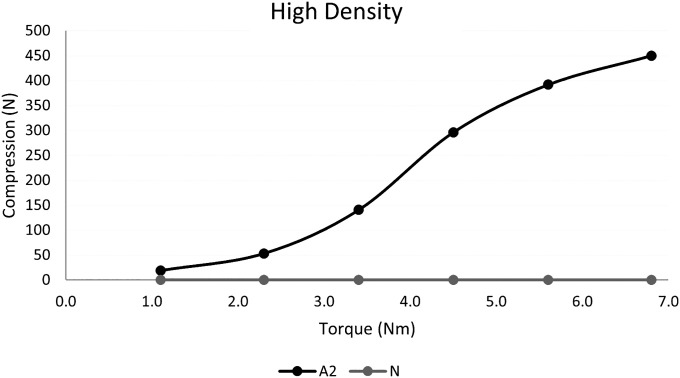
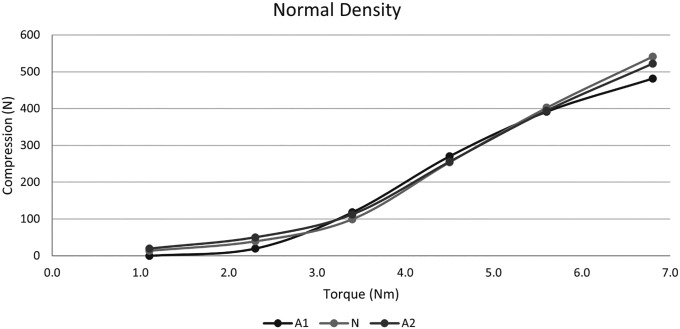
In the low-density bone-block model, the average compressive force of the baseplate when using the standard technique was 112 N compared with 300 N when the alternative technique for low-density bone (A1) was utilized (p = 0.01). All baseplates stripped prior to achieving the final torque goal of 6.8 Nm (60 in-lbf). The average torque prior to stripping was 3.8 Nm (34 in-lbf) for the standard technique and was 5.8 Nm (51 in-lbf) when A1 was utilized (p = 0.001). In the high-density bone block model, failure to seat the glenoid baseplate was noted for all specimens when the standard technique was utilized. Gross failure with screw breakage occurred in 3 specimens, and failure to completely seat the baseplate at the torque end point occurred in 1 specimen. This arm of the study was ceased after 4 seating attempts because of a lack of remaining implants due to the previously mentioned gross failure of the central screw in the 3 available baseplates. When the alternative technique (A2) was performed, the baseplate was seated without failure, with an average compressive force of 450 N. In the standard-density bone block, the average compressive force for the standard technique was 541 N; for the A1 technique, it was 481 N (p = 0.106); and for the A2 technique, 522 N (p = 0.314). The average torque-compression relationships at 1.1-Nm (10-in-lbf) intervals can be found in Figures 4, 5, and 6.
Fig. 4.
Torque-compression relationship for the alternative (A1) and standard/normal (N) techniques for the low-density blocks at 1.1-Nm (10-in-lbf) intervals.
Fig. 5.
Torque-compression relationship for the standard/normal (N) and alternative (A2) techniques for the high-density blocks at 1.1-Nm (10-in-lbf) intervals.
Fig. 6.
Torque-compression relationship for the alternative (A1 and A2) and standard/normal (N) techniques for the normal-density blocks at 1.1-Nm (10-in-lbf) intervals.
Radiographic Arm
A total of 379 intraoperative videos were available for review. Of these, 20 shoulders (20 patients) were included in the “low-density” cohort, and 21 shoulders (19 patients) were included in the “high-density” cohort. The average age at the time of surgery for the low-density cohort was 73 years (range, 60 to 87 years). In the low-density group, 15 patients had a preoperative diagnosis of rotator cuff tear arthropathy, and 5 had a preoperative diagnosis of fracture sequelae. Nine of the patients were female, and 11 were male. The average age for the high-density cohort was 63 years (range, 41 to 78 years). All of these patients had a preoperative diagnosis of osteoarthritis, and all were male.
The mean subchondral thickness was 1.7 mm (SD, 0.56 mm) in the low-density cohort and was 5.3 mm (SD, 1.3 mm) in the high-density cohort. The mean subchondral thickness in the respective matched control groups was 1.9 mm and 3.8 mm (Table I). In the low-density cohort, there was no significant difference between the experimental and matched control groups (p = 0.45). There was a significant difference in the measurement of glenoid sclerosis thickness between the experimental and control groups in our high-density cohort (p < 0.0014). The interrater reliability coefficient was found to be 0.69 for the low-density glenoid sclerosis measurement and 0.92 for the high-density glenoid sclerosis measurement (Table II).
TABLE I.
Glenoid Sclerosis Thickness
| Group | Mean Sclerosis Width (mm) |
|---|---|
| High-density bone | 5.3 |
| Low-density bone | 1.7 |
| High-density bone: matched control | 3.8 |
| Low-density bone: matched control | 1.9 |
TABLE II.
ICC for Radiographic Glenoid Sclerosis Measurement*
| Bone Density | ICC | 95% CI |
|---|---|---|
| Low density | 0.69 | −0.45 to 0.93 |
| High density | 0.92 | 0.82 to 0.98 |
ICC = intraclass correlation coefficient, and CI = confidence interval.
Discussion
To our knowledge, this is the first study to demonstrate alterations in surgical technique for glenoid baseplate insertion to improve implant compression. In the biomechanical model with bone substitutes, we demonstrated improvement in the insertional torque-compression relationship compared with the standard technique in low-density and high-density bone quality. Additionally, we were able to identify that the assessment of preoperative radiographic sclerosis may aid in the decision-making process to utilize these techniques in sclerotic bone.
Our biomechanical arm provided evidence of greater compression when the alternative techniques were utilized for high- and low-density bone. Greater compression about the bone-implant interface is theorized to provide greater stability, decrease micromotion, and improve osseous ingrowth. In the dental literature, a direct relationship between increasing insertional torque and decreased micromotion of the implant has been demonstrated27. Intuitively, this concept should translate to the glenoid-baseplate interface.
The basic principles of screw performance rely heavily on their general purpose and application. The overall goal is to achieve optimal fixation within the given medium by improving thread engagement. Thread features and design variables (geometry, pitch, thread angle, etc.) affect screw performance and can be altered to improve screw purchase. Alternatively, the preparation of the medium can be altered to improve thread engagement. In general, the size of the pilot hole created is related to the major diameter of the screw to allow an appropriate amount of thread engagement and clearing of debris during tapping to create smooth threads. In dense material (bone), tapping is advantageous if debris can be properly cleared, preventing bone chips from wedging into thread formation. These bone chips can increase friction and lead to screw failure. Similarly, if the pilot hole is not large enough, the increased resistance can also lead to shearing under torque. In low-density bone, the bone-chip debris could offer an advantage by compressing into threads and adding support; however, tapping may remove much material from the screw hole, reducing thread engagement. The AO/ASIF (Association of the Study of Internal Fixation) technique manual recommends not tapping in cancellous bone because it is thought that inserting a screw without tapping compresses trabeculae and gives better holding power31,32. Moreover, the quality of threads and the ability to retain fixation in low-density bone may be worse compared with denser bone. Both alternative techniques presented were shown to improve thread engagement.
In the setting of individuals with low-density bone, our alternative technique not only increased the compression that could be achieved but also increased the insertional torque prior to screw stripping. Screw stripping is a major concern because of its effect of compromising fixation due to failure of the bone-implant interface. When this event is encountered in our practice, the baseplate is immediately revised to guarantee ideal time-zero fixation. The decreased incidence of stripping and increased compression provided by the alternative technique for low-density bone are theorized to occur because of less trabecular bone disruption when the 6.5-mm tap is not utilized. This greater remnant of bone stock allows for a wedging effect about the glenoid baseplate when inserted and provides greater resistance to stripping and improved compression. Given less stripping, greater torque, and improved compression, we employ this technique regularly. Although preoperative radiographic glenoid sclerosis was not significantly different between the experimental and matched control groups, we recommend utilization of this technique in individuals with minimal glenoid sclerosis (<2 mm) on preoperative radiographs and individuals with large glenoid vault cavities in whom we anticipate the central screw will not achieve bicortical fixation in the scapular vault wall.
The alternative technique for sclerotic bone provided more than just increased compression. When this alternative technique was utilized, we did not experience any catastrophic implant failures or inability to fully seat the implant. This is in stark contrast to the testing of our standard technique, in which 3 of the 4 implants broke mid-implantation at the midportion of the screw, and the fourth was unable to be fully seated prior to meeting the 60 in-lbf end point. These findings are similar to those of a study by Diaz et al. that evaluated differing implant central screw designs in high- and low-density bone23. In their high-density group, they observed lower compression forces during implantation. This was theorized to be due to wedging of the implant during insertion. In our practice, the ideal candidate for utilization of the alternative technique is an individual with osteoarthritis and a large sclerotic glenoid rim (>5 mm) that makes passing the 6.5-mm guide tap intraoperatively difficult.
Other than improving compression, implant breakage, and screw stripping, an additional major strength of the described alternative techniques is their feasibility of use. They require little to no alteration in instrumentation or prosthesis design and can be employed with the addition of a 3.0-mm drill and a 2.5-mm guide. For this reason, the transition to incorporating these techniques into our practice has been seamless.
One potential limitation of this study was the utilization of polyurethane blocks as a bone surrogate. Ideally the biomechanical arm would have been performed in human cadaveric glenoids. However, reproducibility and uniform density of the substrate were required. To maximize the quality of our study, we utilized bone-substitute polyurethane blocks based on the American Society for Testing and Materials Standard F183933. The modulus of elasticity, density, and strength of the utilized foam blocks are similar to the material properties of cancellous glenoid bone24,34. Additionally, there exist numerous previously published RSA biomechanical studies utilizing similar bone substitutes20,23,30,35,36. Another limitation of the study is that these alternative techniques are only applicable to baseplates with a monoblock central screw and may not be generalizable to modular or central-peg implants. However, the concept of under-preparation of osteoporotic bone to enhance fixation is generalizable to all modes of fixation, as is over-preparation of dense sclerotic bone to avoid fracture or implant failure. One further limitation of the study that was not investigated is the relationship of peripheral screws to baseplate stability. The primary aim of the study was to determine improvement in initial compressive forces with the alternative techniques. We chose not to address the peripheral screws in this study given that, for this baseplate design, the peripheral screws would not have changed the compressive force since they are all locking screws. An additional limitation is the lack of an established relationship of glenoid baseplate compression and bone-implant micromotion. However, we theorize that the increased compression about the glenoid interface will provide improved stability. Whether this theoretical improvement is enough to lessen the rate of glenoid component failure has still to be determined. Given this, we recommend further investigation into compression and micromotion, as well as clinical outcomes, when these techniques are utilized.
Conclusion
Alterations in surgical technique for implanting the glenoid baseplate with a central screw design increase time-zero fixation in varying bone densities. Preoperative radiographs can assist in identifying patients for whom these techniques may be useful.
Footnotes
Investigation performed at the Florida Orthopaedic Institute and the Foundation for Orthopaedic Research and Education (F.O.R.E.), Tampa, Florida
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A409).
References
- 1.Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The Reverse Shoulder Prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am. 2005. Aug;87(8):1697-705. [DOI] [PubMed] [Google Scholar]
- 2.Baulot E, Chabernaud D, Grammont PM. Results of Grammont’s inverted prosthesis in omarthritis associated with major cuff destruction. Apropos of 16 cases. Acta Orthop Belg. 1995;61(Suppl 1):112-9. [PubMed] [Google Scholar]
- 3.Seebauer L. Reverse prosthesis through a superior approach for cuff tear arthropathy. Tech Shoulder Elbow Surg. 2006;7(1):13-26. [Google Scholar]
- 4.Werner CML, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005. Jul;87(7):1476-86. [DOI] [PubMed] [Google Scholar]
- 5.Seebauer L, Walter W, Keyl W. Reverse total shoulder arthroplasty for the treatment of defect arthropathy. Oper Orthop Traumatol. 2005. Feb;17(1):1-24. [DOI] [PubMed] [Google Scholar]
- 6.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004. Apr;86(3):388-95. [DOI] [PubMed] [Google Scholar]
- 7.Cheung E, Willis M, Walker M, Clark R, Frankle MA. Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2011. Jul;19(7):439-49. [PubMed] [Google Scholar]
- 8.Cuff D, Pupello D, Virani N, Levy J, Frankle M. Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Joint Surg Am. 2008. Jun;90(6):1244-51. [DOI] [PubMed] [Google Scholar]
- 9.Rojas J, Choi K, Joseph J, Srikumaran U, McFarland EG. Aseptic glenoid baseplate loosening after reverse total shoulder arthroplasty: A systematic review and meta-analysis. JBJS Rev. 2019. May;7(5):e7. [DOI] [PubMed] [Google Scholar]
- 10.Casagrande D, Harmsen S, Norris TR. Glenosphere and baseplate failure in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(6):E181-2. [DOI] [PubMed] [Google Scholar]
- 11.Frankle M, Pupello D. Rationale and Biomechanics of the Reverse Shoulder Prosthesis: The American Experience. In: Frankle MA, Gumpert EE, editors. Rotator Cuff Deficiency of the Shoulder. Thieme Medical Publishers; 2008.
- 12.Chae SW, Kim SY, Lee H, Yon JR, Lee J, Han SH. Effect of baseplate size on primary glenoid stability and impingement-free range of motion in reverse shoulder arthroplasty. BMC Musculoskelet Disord. 2014. Dec 9;15:417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chou J, Malak SF, Anderson IA, Astley T, Poon PC. Biomechanical evaluation of different designs of glenospheres in the SMR reverse total shoulder prosthesis: range of motion and risk of scapular notching. J Shoulder Elbow Surg. 2009. May-Jun;18(3):354-9. [DOI] [PubMed] [Google Scholar]
- 14.James J, Huffman KR, Werner FW, Sutton LG, Nanavati VN. Does glenoid baseplate geometry affect its fixation in reverse shoulder arthroplasty? J Shoulder Elbow Surg. 2012. Jul;21(7):917-24. [DOI] [PubMed] [Google Scholar]
- 15.Virani NA, Harman M, Li K, Levy J, Pupello DR, Frankle MA. In vitro and finite element analysis of glenoid bone/baseplate interaction in the reverse shoulder design. J Shoulder Elbow Surg. 2008. May-Jun;17(3):509-21. [DOI] [PubMed] [Google Scholar]
- 16.Gutiérrez S, Greiwe RM, Frankle MA, Siegal S, Lee WE, 3rd. Biomechanical comparison of component position and hardware failure in the reverse shoulder prosthesis. J Shoulder Elbow Surg. 2007. May-Jun;16(3)(Suppl):S9-12. [DOI] [PubMed] [Google Scholar]
- 17.James J, Allison MA, Werner FW, McBride DE, Basu NN, Sutton LG, Nanavati VN. Reverse shoulder arthroplasty glenoid fixation: is there a benefit in using four instead of two screws? J Shoulder Elbow Surg. 2013. Aug;22(8):1030-6. [DOI] [PubMed] [Google Scholar]
- 18.Hopkins AR, Hansen UN, Bull AMJ, Emery R, Amis AA. Fixation of the reversed shoulder prosthesis. J Shoulder Elbow Surg. 2008. Nov-Dec;17(6):974-80. [DOI] [PubMed] [Google Scholar]
- 19.Chebli C, Huber P, Watling J, Bertelsen A, Bicknell RT, Matsen F, 3rd. Factors affecting fixation of the glenoid component of a reverse total shoulder prothesis. J Shoulder Elbow Surg. 2008. Mar-Apr;17(2):323-7. [DOI] [PubMed] [Google Scholar]
- 20.Lung TS, Cruickshank D, Grant HJ, Rainbow MJ, Bryant TJ, Bicknell RT. Factors contributing to glenoid baseplate micromotion in reverse shoulder arthroplasty: a biomechanical study. J Shoulder Elbow Surg. 2019. Apr;28(4):648-53. [DOI] [PubMed] [Google Scholar]
- 21.Stroud NJ, DiPaola MJ, Martin BL, Steiler CA, Flurin PH, Wright TW, Zuckerman JD, Roche CP. Initial glenoid fixation using two different reverse shoulder designs with an equivalent center of rotation in a low-density and high-density bone substitute. J Shoulder Elbow Surg. 2013. Nov;22(11):1573-9. [DOI] [PubMed] [Google Scholar]
- 22.Gorman RA, 2nd, Christmas KN, Simon P, Hess AV, 2nd, Brewley EE, Jr, Mighell MA, Frankle MA. Optimizing humeral stem fixation in revision reverse shoulder arthroplasty with the cement-within-cement technique. J Shoulder Elbow Surg. 2020. Jul;29(7S):S9-16. [DOI] [PubMed] [Google Scholar]
- 23.Diaz MA, Garrigues GE, Ricchetti ET, Gutierrez S, Frankle MA. Relationship Between Insertion Torque and Compression Strength in the Reverse Total Shoulder Arthroplasty Baseplate. J Orthop Res. 2020. Apr;38(4):871-9. Epub 2019 Nov 25. [DOI] [PubMed] [Google Scholar]
- 24.Patel PSD, Shepherd DET, Hukins DWL. Compressive properties of commercially available polyurethane foams as mechanical models for osteoporotic human cancellous bone. BMC Musculoskelet Disord. 2008. Oct 9;9:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shim V, Boheme J, Josten C, Anderson I. Use of Polyurethane Foam in Orthopaedic Biomechanical Experimentation and Simulation. In: Zafar F, Sharmin E, editors. Polyurethane. London: IntechOpen; 2012. p 171-200. [Google Scholar]
- 26.Friedrich Graef, Karl M, Winter W. Determination of Micromotion at the Implant Bone Interface - An In-Vitro Methodologic Study. Dentistry. 2015;5(4):1-5. [Google Scholar]
- 27.Trisi P, Perfetti G, Baldoni E, Berardi D, Colagiovanni M, Scogna G. Implant micromotion is related to peak insertion torque and bone density. Clin Oral Implants Res. 2009. May;20(5):467-71. [DOI] [PubMed] [Google Scholar]
- 28.Johnson KA, Smith FW. Axial compression generated by cortical and cancellous lag screws in the equine distal phalanx. Vet J. 2003. Sep;166(2):159-63. [DOI] [PubMed] [Google Scholar]
- 29.Ricci WM, Tornetta P, 3rd, Petteys T, Gerlach D, Cartner J, Walker Z, Russell TA. A comparison of screw insertion torque and pullout strength. J Orthop Trauma. 2010. Jun;24(6):374-8. [DOI] [PubMed] [Google Scholar]
- 30.Harman M, Frankle M, Vasey M, Banks S. Initial glenoid component fixation in “reverse” total shoulder arthroplasty: a biomechanical evaluation. J Shoulder Elbow Surg. 2005. Jan-Feb;14(1)(Suppl S):162S-7S. [DOI] [PubMed] [Google Scholar]
- 31.Schatzker J. Screws and Plates and Their Application. In: Müller M, Allgöwer M, Schneider R, Willenegger H, editors. Manual of Internal Fixation. 3rd ed. Springer; 1991. p 184.
- 32.Chapman JR, Harrington RM, Lee KM, Anderson PA, Tencer AF, Kowalski D. Factors affecting the pullout strength of cancellous bone screws. J Biomech Eng. 1996. Aug;118(3):391-8. [DOI] [PubMed] [Google Scholar]
- 33.ASTM. Standard Specification for Rigid Polyurethane Foam for use as a Standard Material for Testing Orthopaedic Devices and Instruments. ASTM International; 2014.
- 34.Anglin C, Tolhurst P, Wyss UP, Pichora DR. Glenoid cancellous bone strength and modulus. J Biomech. 1999. Oct;32(10):1091-7. [DOI] [PubMed] [Google Scholar]
- 35.Formaini NT, Everding NG, Levy JC, Santoni BG, Nayak AN, Wilson C. Glenoid baseplate fixation using hybrid configurations of locked and unlocked peripheral screws. J Orthop Traumatol. 2017. Sep;18(3):221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Formaini NT, Everding NG, Levy JC, Santoni BG, Nayak AN, Wilson C, Cabezas AF. The effect of glenoid bone loss on reverse shoulder arthroplasty baseplate fixation. J Shoulder Elbow Surg. 2015. Nov;24(11):e312-9. [DOI] [PubMed] [Google Scholar]