Background:
This study was designed to compare effect of combined use of dexamethasone and honey versus each agent alone in controlling complications associated with removal of impacted mandibular third molar.
Methods:
This randomized clinical study included patients suffering from impacted mandibular wisdom teeth. Patients were divided randomly into 4 groups. Group I, control, group II, received dexamethasone injection preoperatively, group III, received honey locally in the wound after extraction, and group IV, received dexamethasone injection preoperatively and topical honey application. All patients were evaluated preoperatively and postoperatively to assess facial edema, interincisal distance, pain, and total analgesic dose used.
Results:
Significant edema developed in group I than other groups and improved significantly in group II and III on seventh postoperative day, and tenth postoperative day in group I. Insignificant edema developed in group IV. Significant decrease in interincisal distance occurred in all groups on third postoperative day that improved significantly on seventh postoperative days in all groups except group I, it improved on tenth postoperative day. Pain was significantly minimum in group IV than other groups and its maximum degree was in group I.
Conclusion:
Both dexamethasone and honey are an effective way of minimizing swelling, pain, and trismus after removal of impacted lower third molars. Both agents either alone or in combination provide simple, safe, painless, and cost-effective method to eliminate postoperative discomfort. However, dexamethasone or honey can decrease complications related to surgical extraction of mandibular third molar, the simultaneous application of both agents is more effective method in this regard.
Keywords: complication, dexamethasone, honey, impacted, postoperative, third molar
1. Introduction
Surgical removal of an impacted mandibular third molar is one of the most common procedures in oral and maxillofacial surgery. The inflammatory response to surgical trauma is associated with edema, discomfort, dehiscence, and trismus and these factors may affecting the patient’s everyday life.[1–3] Also, complications such as dry socket and postoperative infection after surgical removal of impacted molars have been recorded and contributed in worsening of the patient’s condition.[4,5]
An appropriate anti-inflammatory drug is necessary to reduce postoperative inflammation and associated problems.[6] Corticosteroids are employed to prevent oedema and trismus associated with surgical extraction of impacted third molar.[7] Different studies showed that corticosteroids were effective in lowering postoperative pain and oedema in patients undergoing dental operations.[7,8] A number of recent investigations studied the analgesic benefit of a single perioperative dosage of dexamethasone, but the results have been inconsistent.[8,9]
Since ancient times, honey has been one of the most regularly employed agents in alternative medicine.[10,11] There is enough data to support the use of honey in treatment of wounds and burns.[1,12,13] Honey’s therapeutic benefits have been linked to its antimicrobial, anti-inflammatory and antioxidant properties.[14] When applied to wounds and burns, honey has been shown soothing effect and superior efficacy than povidone iodine dressing in reducing pain and increasing comfort in chronic wound patients.[15] Also, honey reducing acute postoperative pain and analgesic requirements in tonsillectomy patients.[16,17] Furthermore, Honey could also be utilized to treat the pain associated with alveolar osteitis.[18]
This study was designed to compare the effect of combined use of dexamethasone and natural honey versus each agent alone in controlling complications associated with surgical extraction of impacted mandibular third molars.
2. A novel therapeutic approach for reducing postoperative inflammatory complications after impacted mandibular third molar removal
2.1. Study design
This study was a prospective, randomized clinical trial that performed according to CONSORT 2010. The study was performed according to rules of ethics declared by Helsinki. An ethical approval (no. 21-5\1) was obtained from the institutional ethics committee. All patients included in this study signed an informed consent. The study duration was from January 2021 until June 2021 and ended as planned in the suggested study’s protocol. This study was registered under www.ClinicalTrial.gov (study no. NCT04848259 -14 \ 4 \ 2021).
In this study, to investigate the effect of natural honey and dexamethasone on postoperative complications of impacted third molar removal, the patients were divided into 4 groups that included control, dexamethasone, honey, and combined honey-dexamethasone groups.
2.2. Sample size calculation
In the current study, the minimum sample size required of subjects was 69 using G*Power version 3.1.92, where the effect size was 0.40 (chosen as an above medium value)[19] with alpha error 0.05 and a power level of 0.80. Considering that some patients could be lost during postoperative follow up periods, 80 subjects were finally included.
2.3. Inclusion and exclusion criteria
Patients were included in this investigation if they had no systemic disease, no history of smoking, their age ranged 20 to 35 years old, and suffering from mesioangular impacted mandibular third molar. Regarding the vertical position of an impacted tooth, only Pell and Gregory class B impaction (The occlusal plane of an impacted tooth is between the occlusal plane and the cervical line of a second molar) was included. Also, regarding horizontal relation of an impacted tooth to mandibular ramus, only Pell and Gregory class 2 impaction (half of the crown of an impacted tooth is covered by a mandibular ramus) was included in this study.
While, patients were excluded from this study, if they were suffering from pericoronitis before the surgery, have taken antibiotic or anti-edematous drugs 2 weeks before the surgery, suffering from concurrent periodontal disease and patients presented with contraindications to drugs used in this study.
2.4. Patient grouping
Patients were divided randomly (using online software (https://www.randomizer.org) into 4 groups, each group contained 20 patients. In group I, after extraction of an impacted third molar a wound irrigated by normal saline before closure. In group II, dexamethasone 2 % (8 mg/2 mL, Sigma, KSA) at dose 0.2 mg/kg was injected intravenously (IV) half an hour before the surgery. In group III, 2 mL natural honey was placed in the socket after tooth extraction while, in group IV dexamethasone 2% at dose 0.2 mg/kg was injected IV half an hour before the surgery and 2 mL natural honey was placed in a socket after tooth extraction before closure.
Before the commencement of the study the honey was obtained from the Cooperative association of Beekeepers in Madina munawarah and submitted for chemical analysis, to ensure that its chemical composition be adherent to Codex Alimentarius[20] and Saudi standard specifications,[21] in (Food and environment laboratories, Quality Agency, Municipality of Al-Madinah Al-Munawwarah Region) form number: 42002206.
2.5. Surgical protocol
All patients underwent the surgery under inferior alveolar and buccal nerve blocks using 2% lidocaine with 1:200,000 epinephrine solution. Dexamethasone 2% at dose 0.2 mg/kg was injected half an hour IV before surgery in group II and IV. A modified ward flap was raised to access the surgical field, buccal and distal bone was removed around the impacted tooth using surgical burs rotate at low speed under copious saline irrigation, then the tooth was sectioned. Once the tooth was extracted, the bone edge was smoothed by a bone file, socket was irrigated with sterile saline solution to eliminate debris. After that, 2 mL of natural honey was applied in group III and IV (Fig. 1). Then, the flap was closed was with 3–0 silk. All patients were instructed to take Augmentin 1g/12 h for 7 days, Ibuprofen 400 mg tablet on demand and received a written postoperative instruction.
Figure 1.
Honey application after extraction of impacted third molar.
2.6. Patient evaluation
All patients were submitted to preoperative and postoperative evaluation that included assessment of mandibular function, pain level on visual analogue scale (VAS), total amount of the used analgesic dose, and facial edema. Postoperative evaluation was performed on the first, second, third, seventh and tenth postoperative day.
Mandibular function was evaluated by measuring an interincisal distance (IID) between upper and lower anterior teeth. Pain intensity was evaluated by using a 10-point VAS, with the patient marking a mark on the scale to refer the pain level from no pain “0” to severe pain “10.” Total amount of the used analgesic dose was calculated after surgery by asking each patient to report each analgesic dose that was used postoperatively. Finely, facial edema was evaluated by using a modification of the tape measure method described by Gabka and Matsumara.[22] The points of this measurement include angle of mandible (AM), tragus (T), pogonion (P), corner of mouth (CM), ala of nose (AN) and lateral canthus of eye. Following measurements were recorded D1: AM-P; D2: AM-CM; D3 AM-AN; D4: AM-lateral canthus of eye; D5: T-P; D6: T-CM and D7: T-AN. After recording of these measurements, the mean values of (D1–D4), (D5–D7), and (D1–D7) were calculated and compared among the groups.
2.7. Statistical analysis
It was carried out using SPSS computer package version 25.0 (IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp., USA). For descriptive statistics: the means, standard deviations, and 95% confidence intervals were used for quantitative variables. For analytic statistics: A repeated measures ANOVA with a Greenhouse-Geisser correction test was applied to assess differences in means of quantitative variables within the same group at different time periods with Bonferroni post hoc correction to determine where the significance specifically exist. Kruskal–Wallis test was used to assess differences in means of quantitative variables between the groups at each time period. The statistical methods were verified, assuming a significant level of P < .05 and a highly significant level of P < .001.[21]
3. Results
This study was conducted on 80 patients, 43 females and 37 males, with mean age 25.025. The mean patients’ age was 27.20 ± 7.13, 28.20 ± 7.82, 28.20 ± 8.33, and 28.50 ± 6.41 for groups I, II, III, and IV, respectively. Each of group II and group III contained 12 female patients while, group I and group IV contained 10 and 9 female patients, respectively.
There was no statistically significant difference among groups regarding mean age and sex distribution. In addition, there was no statistical difference among groups regarding all evaluated parameters at the preoperative period. All patients showed uneventful wound healing and no infection or wound dehiscence was reported.
In this study, there was statistically significant facial edema appeared on the third postoperative day in all groups, except group IV. Significant improvement in the edema begins to appear on the seventh postoperative day in groups II and group III. While significant improvement appeared on the tenth postoperative day in groups I. At all intervals, group IV showed non-significant development of the edema.
Comparison among groups showed that, on the third postoperative day there was significant increased edema in group I than other groups. While, on the seventh postoperative day there was significant improvement in the edema in group IV than group I (Table 1).
Table 1.
Comparing facial swelling values at different follow up interval in all groups.
| Variables in different groups | Preoperative | Postoperative | P value1 | ||||
|---|---|---|---|---|---|---|---|
| First day | Second day | Third day | Seventh day | Tenth day | |||
| Mean (D1 to D4) | |||||||
| Group I | 9.87 ± .82 | 10.91 ± .77 | 11.13 ± .74 | 11.31 ± .78 | 11.2 ± .81 | 9.92 ± .76 | <.001* |
| Group II | 9.82 ± .4 | 10.21 ± .68 | 10.33 ± .47 | 10.45 ± .41 | 9.97 ± .76 | 9.8 ± .78 | .028* |
| Group III | 9.77 ± .88 | 10.42 ± .84 | 10.5 ± .8 | 10.78 ± .72 | 9.94 ± .84 | 9.8 ± 1.06 | .003* |
| Group IV | 9.74 ± .62 | 9.85 ± .53 | 9.88 ± .59 | 10.01 ± .67 | 9.74 ± .76 | 9.8 ± .59 | .935 |
| P value2 | .502 | .004 | <.001 | <.001 | .279 | .674 | |
| Mean (D5 to D7) | Immediate | 2nd day | 3rd day | 7th day | 10th day | ||
| Group I | 11.82 ± 1.64 | 12.7 ± 1.71 | 13.23 ± 1.66 | 13.69 ± 1.56 | 12.58 ± 1.66 | 11.91 ± 1.69 | .005* |
| Group II | 12.03 ± 1.01 | 12.36 ± 1.08 | 12.79 ± 1.06 | 12.84 ± 1.02 | 12.23 ± 1.07 | 12.1 ± 1.16 | .035* |
| Group III | 11.93 ± .95 | 12.26 ± 1.06 | 12.5 ± .99 | 12.92 ± .97 | 12.01 ± .95 | 11.95 ± 1.01 | .031* |
| Group IV | 11.85 ± .51 | 12.11 ± .53 | 12.24 ± .51 | 12.31 ± .55 | 11.99 ± .62 | 11.91 ± .58 | .287 |
| P value | .102 | .247 | .290 | .102 | .046* | .228 | |
| Mean (D1 to D7) | Immediate | 2nd day | 3rd day | 7th day | 10th day | ||
| Group I | 10.76 ± 1.14 | 11.72 ± 1.14 | 11.93 ± 1.11 | 12.16 ± 1.09 | 10.99 ± 1.12 | 10.81 ± 1.06 | <.001* |
| Group II | 10.8 ± .61 | 11.23 ± .72 | 11.84 ± .64 | 11.2 ± .64 | 10.96 ± .83 | 10.83 ± .73 | .029* |
| Group III | 10.76 ± .85 | 11.3 ± .93 | 11.37 ± .89 | 11.71 ± .84 | 10.85 ± .9 | 10.73 ± 1.01 | .023* |
| Group IV | 10.69 ± .53 | 10.82 ± .47 | 10.85 ± .51 | 10.9 ± .52 | 10.74 ± .62 | 10.7 ± .56 | .625 |
| P value | .563 | .101 | .010* | .004* | .910 | .532 | |
1: Significance. P value in row indicates significance between groups.
2: Significance P value in column indicates significance at different follow up period in each group.
D1 = distance from angle of mandible to pogonion, D4 = distance from angle of mandible to lateral canthus of eye, D5: distance from tragus to pogonion, D7 = distance from angle of mandible to ala of nose.
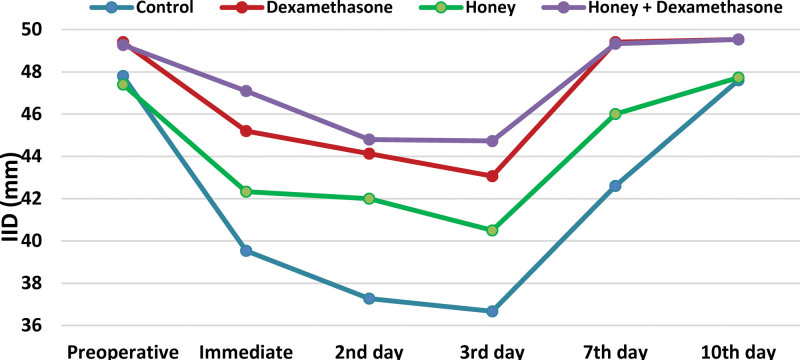
Significant decreased IID was reported on the second postoperative day in groups I and IV and on the third postoperative day in all groups. Significant improvement in IID was reported on the seventh and tenth postoperative day in all groups except group I, the improvement occurred on the tenth postoperative day. From the first to tenth postoperative days, significant decreased IID was observed in group I than groups II and IV (Fig. 2).
Figure 2.
IID in all groups along different follow up intervals. ID = interincisal distance.
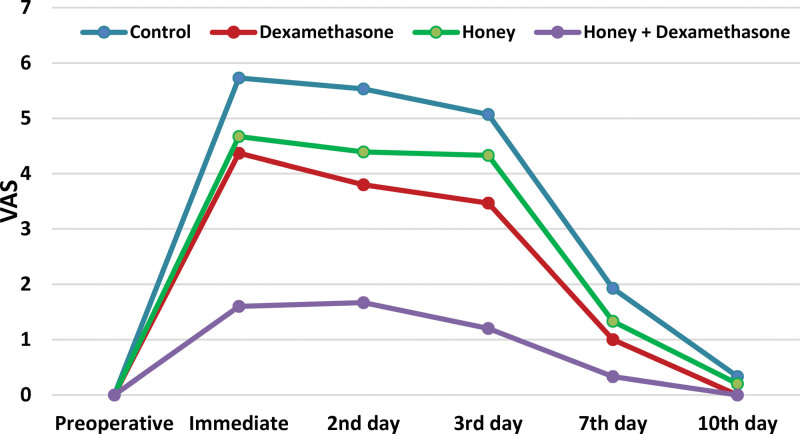
Regarding pain score on VAS, this study showed that pain was reported in all groups on the first postoperative day and continued to the third postoperative day. Then, the pain was significantly decreased on the seventh postoperative days in all groups. Comparison among groups showed that in all postoperative follow up periods, the pain was significantly minimum in group IV than other groups and its maximum degree was in group I. Also, there was no statistically significant difference between group I and group III on the first and third postoperative periods (Fig. 3).
Figure 3.
Pain score on VAS in all groups along different follow up intervals. VAS = visual analogue scale.
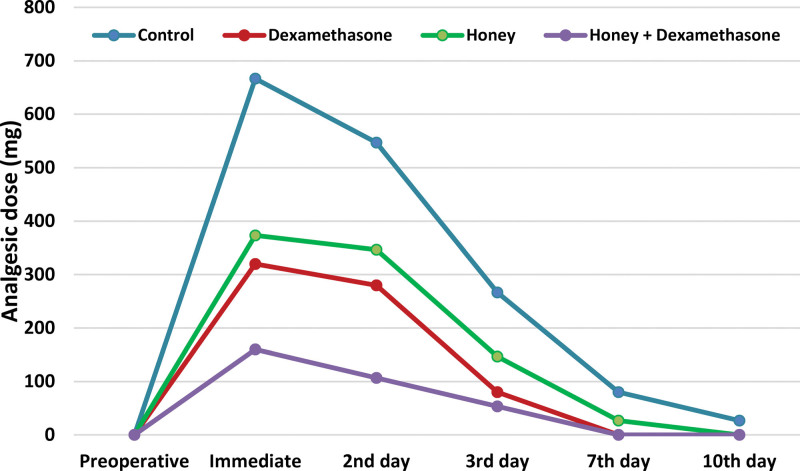
The results of this study showed that, during the first postoperative day, the maximum used analgesic dose was reported in group I while, the minimum dose was reported in group IV. In all groups, significant reduction in the used analgesic dose was recorded on the third postoperative day. The dose was stopped on the seventh postoperative days in groups II and IV and stopped on the tenth postoperative day in group III (Fig. 4).
Figure 4.
Total analgesic dose used at different follow up periods in all groups.
4. Discussion
Edema, discomfort, and trismus are common complications associated with oral surgery, which have a substantial impact on a patient’s quality of life. Prevention of postoperative discomfort that happen after removal of an impacted third molar is usually a better patient care method than treating the disease after appearance of symptoms. Many clinicians have successfully employed anti-inflammatory drugs, such as steroids, for this purpose. Dexamethasone is a synthetic glucocorticoid with anti-inflammatory, long-acting, high-potency and immunosuppressive properties. It has at least 25 times the glucocorticoid action of hydrocortisone. However, unlike hydrocortisone, it has only a minor mineralocorticoid action.[24,25]
Because of side effects of synthetic medications, particularly steroids,[26] researchers are focusing more on plant-based drugs. Honey, a natural ingredient that has been utilized for therapeutic purposes since ancient times, in addition to plant-based medications. Honey is now accepted as a novel effective therapy for different disorders, thanks to the validation of ethnopharmacological claims.[27]
To evaluate quality of honey and ensuring that it is free from any foreign bodies or any concomitant, a sample of honey was subjected for chemical analysis. The chemical analysis included presence of strange smell, foreign matter, fermentation, and level of acidity. Also, moisture, sugars content (fructose, glucose, and sucrose) and percent of hydroxymethylfurfural were determined. A sample was considered of good quality and safe if it meets Codex Alimentarius[20] and Saudi standard specification for hone.[21]
Aim of this current study was to increase postoperative satisfaction of oral surgery patients through comparing the effect of combined use of preoperative dexamethasone injection and local honey placement in the wound after extraction versus solely preoperative IV dexamethasone injection or local honey placement.
In this study, only mesioangular, Pell and Gregory class B (vertical position), and Pell and Gregory class 2 (horizontal position) impactions were included. All surgeries were performed by the same surgeon and the same surgical protocol was used for all patients in order to eliminate bias associated to intraoperative trauma. Additionally, a modified ward flap was used to get access to the surgical field, as it was determined that both ward’s flap and modified ward’s flaps give good efficacy while, the modified ward’s flaps having much less duration of surgery and postoperative pain.[28]
In the current study, dexamethasone was used through IV rout as it provides stable blood levels just prior to surgical trauma. While, oral route efficacy is dependent on patient compliance, and a repeated oral dose is necessary to maintain an adequate blood level. Ability of oral corticosteroid to reduce postoperative sequelae is debatable. Regarding intramuscular route, it has a larger risk of adrenal suppression.[29]
Dexamethasone was administered preoperatively, as it is only effective in controlling edema if given prior to tissue damage.[30]
For controlling postoperative pain, Ibuprofen was used. However, the Ibuprofen has analgesic and anti-inflammatory properties but, it did not affect the results of this study because all patients, in all groups, were prescribed to take Ibuprofen on demand. Therefore, its effect was present and neutralized in all groups.
There was no statistically significant difference between groups in terms of age and sex distribution. In addition, there was no change in any outcome factors in any group during the preoperative period. This guarantees that the results are more consistent.
Regarding postsurgical edema, the maximum mean level of edema was significantly observed on the third postoperative day in all groups (P < .05), except group IV that, showed insignificant (P ˃ 0.05) edema during different postoperative periods. Significant improvement (P < .05) (decrease in edema level when compared to its maximum increase at on the third postoperative day) occurred on the tenth postoperative day in group I that nearly subsided to its preoperative level, while it improved significantly on the seventh postoperative day in both group II and group III.
These results are in agreement with study of Raakesh N et al,[22] and Berine and Hollander,[31] who reported a significant improvement in postoperative edema in dexamethasone than control group. Also, in accordance with Elbagoury E et al,[32] who stated that after surgical removal of impacted third molar there was less swelling in honey group than in control group. While, the current study is in disagreement with Kang et al,[33] who reported that there was no significant effect appeared on facial swelling after giving the patients one preoperative dose of prednisolone at 10 or 20 mg orally before mandibular third molar surgery. The different result between both studies may be attributed to difference in rout of drug administration and different dose.
This result can be attributed to the anti-inflammatory effect of dexamethasone and its ability to decrease capillary permeability[34] and decrease prostaglandins E2 and thromboxane B2 levels.[35] Also, the ability of honey to decrease fluid transudation and inflammatory mediators’ level and elevating nitric oxide end products can explain its anti-edematous effect.[13]
Result of this study showed that, a significant decreased IID was reported in control than other groups during the first 3 days postoperative. While significant improvement reported on the seventh postoperative day in all groups except group I where, significant improvement in IID was reported on the tenth postoperative. This is in accordance with Raakish N,[22] El Hag et al,[36] and Graziani et al,[37] who reported that significant reduction in mouth opening in dexamethasone than control group. This may be due to anti-inflammatory action of dexamethasone and honey and ability of honey to stimulate tissue repair.[15] This result is in contrast to with Kang et al,[33] who reported that there was no significant effect on mandibular movement after giving the patients single preoperative dose of prednisolone at 10 or 20 mg orally before mandibular third molar surgery. As mentioned previously the difference rout of drug administration and different dose may be responsible for different results.
When comparing 4 groups, there was significant (P < .05) less pain in group IV than other groups, and there was a significant less pain in group II and group III than group I, while there was non-significant (P ˃ 0.05) difference between group II and group III. The lower pain level in group II and group III compared to the control group is consistent with Raakish N,[22] Nuraldeen M, and Al-Moudallal Y.[38] The former reported less pain in dexamethasone group and the later reported less pain in honey group than the control. This result is in disagreement with Kang et al,[33] who found that there was no significant effect on postoperative pain after giving the patients single preoperative dose of prednisolone at 10 or 20 mg orally before extracting the third molar. As mentioned previously the difference in rout of drug administration and different dose may be responsible for different results.
Regarding total used analgesic dose, there was significant less used dose in group IV than other groups and there was significant less analgesic dose in group II and III than group I. Also, there was less analgesic dose in group II, and IV than group I on the seventh and tenth postoperative days. These results were in accordance with Raakish N[22] who reported less pain in dexamethasone than control group and Nuraldeen M and Al-Moudallal Y,[38] who found less analgesic dose used with honey group than the control. Honey decreases activity of cyclooxygenase-1 and cyclooxygenase-2, thus demonstrating anti-inflammatory effects and shows immunomodulatory effects.[38] As mentioned previously, the anti-inflammatory effects of dexamethasone and honey explain their role in reducing pain and analgesic dose after surgery.[33,38]
Generally, results of the current study may be attributed to the ability of dexamethasone to prevent conversion of phospholipid into arachidonic acid, therefore blocking formation of prostaglandins, leukotrienes and thromboxane A2 related substances. In addition to its ability to reduce capillary permeability.[34] Also, it has the potential to inhibit formation of pain mediators in traumatized area and reducing sensitization of central pain receptors by blocking nociceptors centrally and peripherally.[3,40,41] While, the ability of honey to reduce white blood cells in inflammatory media and decreasing prostaglandin levels and elevating nitric oxide end products can interpret its antiedematous effect.[13] The combined effect of preoperative administration of dexamethasone and topical application of honey in extraction site may result in insignificant postoperative sequalae in this group.
It is recommended that, a future study with evaluation of swelling using soft tissue images obtained by facial scanning that, can provide a more reliable evaluation in that regard.
5. Conclusion
The use of dexamethasone and natural honey can reduce the degree of swelling, trismus and pain after surgical removal of impacted third molar. In this prospective randomized clinical study, we conclude that preoperative administration of intravenous dexamethasone and topical application of natural honey is effective in combating postsurgical complication. Superior effects were seen in simultaneous use of preoperative dexamethasone and topical application of honey in extraction site.
Acknowledgments
All authors thank for Dr Mohamed Osama Nour, Assistant Professor at Department of Public Health and Community Medicine, Damietta Faculty of Medicine, Al-Azhar University, Egypt for his efforts in statistical analysis of this study.
Author contributions
Conceptualization: Alaa Abdelqader Altaweel, Abd El-Hamid Gaber, Mahmoud Z. Alnaffar.
Data curation: Alaa Abdelqader Altaweel, Mahmoud Z. Alnaffar, Abdulrahman S. Almowallad, Abeer S. Almuwallad, Rawan K. Alharbi.
Formal analysis: Alaa Abdelqader Altaweel.
Funding acquisition: Abd El-Hamid Gaber, Mahmoud Z. Alnaffar, Abdulrahman S. Almowallad, Mohamad H. Almech, Abeer S. Almuwallad, Wasan A. Arab.
Investigation: Alaa Abdelqader Altaweel, Mohamad H. Almech, Abeer S. Almuwallad, Rawan K. Alharbi.
Methodology: Alaa Abdelqader Altaweel, Abd El-Hamid Gaber, Mohamad H. Almech,
Project administration: Alaa Abdelqader Altaweel, Mahmoud Z. Alnaffar.
Resources: Abd El-Hamid Gaber, Mahmoud Z. Alnaffar, Abdulrahman S. Almowallad, Mohamad H. Almech, Abeer S. Almuwallad, Rawan K. Alharbi, Wasan A. Arab.
Software: Mahmoud Z. Alnaffar, Abdulrahman S. Almowallad, Mohamad H. Almech, Abeer S. Almuwallad, Wasan A. Arab.
Supervision: Alaa Abdelqader Altaweel.
Validation: Alaa Abdelqader Altaweel, Wasan A. Arab.
Visualization: Alaa Abdelqader Altaweel.
Writing – original draft: Alaa Abdelqader Altaweel, Abd El-Hamid Gaber.
Writing – review & editing: Alaa Abdelqader Altaweel, Abd El-Hamid Gaber.
Abbreviations:
- AM =
- angle of mandible
- AN =
- ala of nose
- CM =
- corner of mouth
- IID =
- interincisal distance
- IV =
- intravenous
- P =
- pogonion
- T =
- tragus
- VAS =
- visual analogue scale
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The work was done in Vision Colleges, Jeddah, Saudi Arabia.
The authors have no funding and conflicts of interest to disclose.
How to cite this article: Altaweel AA, El-Hamid Gaber A, Alnaffar MZ, Almowallad AS, Almech MH, Almuwallad AS, Alharbi RK, Arab WA. A novel therapeutic approach for reducing postoperative inflammatory complications after impacted mandibular third molar removal. Medicine 2022;101:37(e30436).
Contributor Information
Abd El-Hamid Gaber, Email: abdelhamidgaber@yahoo.com.
Abdulrahman S. Almowallad, Email: abeer.222009@hotmail.com.
Mohamad H. Almech, Email: dentomech@hotmail.com.
Rawan K. Alharbi, Email: dr.rawan-kamal@hotmail.com.
Wasan A. Arab, Email: wasan.arab@hotmail.com.
References
- [1].Üstün Y, Erdoǧan O, Esen E, et al. Comparison of the effects of 2 doses of methylprednisolone on pain, swelling, and trismus after third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:535–9. [DOI] [PubMed] [Google Scholar]
- [2].McGrath C, Comfort MB, Lo ECM, et al. Changes in life quality following third molar surgery—the immediate postoperative period. Br Dent J. 2003;194:265–8; discussion 261. [DOI] [PubMed] [Google Scholar]
- [3].Kim K, Brar P, Jakubowski J, et al. The use of corticosteroids and nonsteroidal antiinflammatory medication for the management of pain and inflammation after third molar surgery: a review of the literature. Oral Surgery, Oral Med Oral Pathol Oral Radiol Endodontology. 2009;107:630–40. [DOI] [PubMed] [Google Scholar]
- [4].Ren YF, Malmstrom HS. Effectiveness of antibiotic prophylaxis in third molar surgery: a meta-analysis of randomized controlled clinical trials. J Oral Maxillofac Surg. 2007;65:1909–21. [DOI] [PubMed] [Google Scholar]
- [5].Blum IR. Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. Int J Oral Maxillofac Surg. 2002;31:309–17. [DOI] [PubMed] [Google Scholar]
- [6].Laureano Filho JR, Maurette PE, Allais M, et al. Clinical comparative study of the effectiveness of two dosages of Dexamethasone to control postoperative swelling, trismus and pain after the surgical extraction of mandibular impacted third molars. Med Oral Patol Oral Cir Bucal. 2008;13:129–32. [PubMed] [Google Scholar]
- [7].Piecuch JF. What strategies are helpful in the operative management of third molars? J Oral Maxillofac Surg. 2012;70(9 Suppl 1):S25–32. [DOI] [PubMed] [Google Scholar]
- [8].Fukami Y, Terasaki M, Okamoto Y, et al. Efficacy of preoperative dexamethasone in patients with laparoscopic cholecystectomy: a prospective randomized double-blind study. J Hepatobiliary Pancreat Surg. 2009;16:367–71. [DOI] [PubMed] [Google Scholar]
- [9].Tugsan Egemen BH, Ozer Z, Doruk N, et al. A comparative study of the antiemetic efficacy of dexamethasone, ondansetron, and metoclopramide in patients undergoing gynecological surgery. Med Sci Monit. 2010;16:336–41. [PubMed] [Google Scholar]
- [10].Molan PC, Betts JA. Clinical usage of honey as a wound dressing: an update. J Wound Care. 2004;13:353–6. [DOI] [PubMed] [Google Scholar]
- [11].Khan FR, Abadin ZU, Rauf N. Honey: nutritional and medicinal value. Int J Clin Pract. 2007;61:1705–7. [DOI] [PubMed] [Google Scholar]
- [12].Moore OA, Smith LA, Campbell F, et al. Systematic review of the use of honey as a wound dressing. BMC Complement Altern Med. 2001;1:2–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Al-Waili NS, Salom K, Al-Ghamdi AA. Honey for wound healing, ulcers, and burns; data supporting its use in clinical practice. Sci World J. 2011;11(June 2015):766–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Yaghoobi R, Kazerouni A, kazerouni O. Evidence for clinical use of honey in wound healing as an anti-bacterial, anti-inflammatory anti-oxidant and anti-viral agent: a review. Jundishapur J Nat Pharm Prod. 2013;8:100–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Gulati S, Qureshi A, Srivastava A, et al. A prospective randomized study to compare the effectiveness of honey dressing vs. povidone iodine dressing in chronic wound healing. Indian J Surg. 2014;76:193–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hwang SH, Song JN, Jeong YM, et al. The efficacy of honey for ameliorating pain after tonsillectomy: a meta-analysis. Eur Arch Oto-Rhino-Laryngology. 2016;273:811–8. [DOI] [PubMed] [Google Scholar]
- [17].Boroumand P, Zamani MM, Saeedi M, et al. Post tonsillectomy pain: can honey reduce the analgesic requirements? Anesth Pain Med. 2013;3:198–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Singh V, Pal U, Singh R, et al. Honey a sweet approach to alveolar osteitis: a study. Natl J Maxillofac Surg. 2014;5:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Erdfelder E, FAul F, Buchner A, et al. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60. [DOI] [PubMed] [Google Scholar]
- [20].Standard for honey, CXS 12-19811 adopted in 1981. Revised in 1987, 2001. Amended in 2019
- 21.Mesallam AS, El-Shaarawy MI. Quality attributes of honey in Saudi Arabia, Food Chem. 1987;25:1–11. [Google Scholar]
- [22].Gabka M. [Measuring techniques and clinical testing of an anti-inflammatory agent (tantum)]. Munch Med Wochenschr. 1971;113:198–203. [PubMed] [Google Scholar]
- [23].Chiang CL. Statistical Methods of Analysis by Chin Long Chiang. Trade Paperback, 2003. [Google Scholar]
- [24].Raakesh N, Ravi V, Ushass P, et al. Role of corticosteroids in reducing postoperative swelling, pain, and trismus following surgical extraction of impacted mandibular third molars. Int J Oral Care Res. 2017;5:265–9. [Google Scholar]
- [25].Bartlett R, Hartle AJ. Routine use of dexamethasone for postoperative nausea and vomiting: the case against. Anaesthesia. 2013;68:892–6. [DOI] [PubMed] [Google Scholar]
- [26].Nesbitt LT. Minimizing complications from systemic glucocorticosteroid use. Dermatol Clin. 1995;13:925–39. [PubMed] [Google Scholar]
- [27].Arawwawala M, Hewageegana S. Health benefits and traditional uses of honey: a review. J Apitherapy. 2017;2:9. [Google Scholar]
- [28].Kumar A, Memon A, Panjabi SK, et al. Flap design: comparison of ward’s flap versus modified ward’s flap in surgical extraction of impacted mandibular third molar. Prof Med J. 2019;26:1323–7. [Google Scholar]
- [29].Montgomery MT, Hogg JP, Roberts DL, et al. The use of glucocorticosteroids to lessen the inflammatory sequelae following third molar surgery. J Oral Maxillofac Surg. 1990;48:179–87. [DOI] [PubMed] [Google Scholar]
- [30].James H, Tucker M, Edward E. Contemporary Oral and Maxillofacial Surgery. Elsevier: Mosby, Inc.2018. [Google Scholar]
- [31].Beirne OR, Hollander B. The effect of methlyprednisolone on pain, trismus, and swelling after removal of third molars. Oral Surgery, Oral Med Oral Pathol. 1986;61:134–8. [DOI] [PubMed] [Google Scholar]
- [32].Elbagoury E, Fayed N. Application of “natural honey” after surgical removal of impacted lower third molar. Egypt Dent J. 1985;31:203–11. [PubMed] [Google Scholar]
- [33].Kang SH, Choi YS, Byun IY, et al. Effect of preoperative prednisolone on clinical postoperative symptoms after surgical extractions of mandibular third molars. Aust Dent J. 2010;55:462–7. [DOI] [PubMed] [Google Scholar]
- [34].Ata-Ali J, Ata-Ali F, Peñarrocha-Oltra D, et al. Corticosteroids use in controlling pain, swelling and trismus after lower third molar surgery. J Clin Exp Dent. 2011;3:469–75. [Google Scholar]
- [35].Dionne RA, Gordon SM, Rowan J, et al. Dexamethasone suppresses peripheral prostanoid levels without analgesia in a clinical model of acute inflammation. J Oral Maxillofac Surg. 2003;61:997–1003. [DOI] [PubMed] [Google Scholar]
- [36].Elhag M, Coghlan K, Christmas P, et al. The anti-inflammatory effects of dexamethasone and therapeutic ultrasound in oral surgery. Br J Oral Maxillofac Surg. 1985;23:17–23. [DOI] [PubMed] [Google Scholar]
- [37].Graziani F, D’Aiuto F, Arduino PG, et al. Perioperative dexamethasone reduces post-surgical sequelae of wisdom tooth removal. A split-mouth randomized double-masked clinical trial. Int J Oral Maxillofac Surg. 2006;35:241–6. [DOI] [PubMed] [Google Scholar]
- [38].Al-Khanati NM, Al-Moudallal Y. Effect of intrasocket application of manuka honey on postsurgical pain of impacted mandibular third molars surgery: split-mouth randomized controlled trial. J Maxillofac Oral Surg. 2019;18:147–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Markelov VV, Trushin MV. Bee venom therapy and low dose naltrexone for treatment of multiple sclerosis. Nepal J Neurosci. 2006;3:71–7. [Google Scholar]
- [40].Kaczmarzyk T, Wichlinski J, Stypulkowska J, et al. Preemptive effect of ketoprofen on postoperative pain following third molar surgery. A prospective, randomized, double-blinded clinical trial. Int J Oral Maxillofac Surg. 2010;39:647–52. [DOI] [PubMed] [Google Scholar]
- [41].Ong CKS, Seymour RA, Chen FG, et al. Preoperative ketorolac has a preemptive effect for postoperative third molar surgical pain. Int J Oral Maxillofac Surg. 2004;33:771–6. [DOI] [PubMed] [Google Scholar]