Abstract
Background
Complex primary and revision THR requires comprehensive understanding of abnormal bony anatomy. Evaluation and classification of acetabular bone defects is essential to manage them appropriately. It is difficult to appreciate complex defects using conventional 2-Dimensional radiological modalities. 3D printed models can provide both visual and tactile reproduction of the bony anatomy, with potential for better pre-operative planning and making these complex surgeries more precise and accurate.
Materials and methods
Anatomical 3D models of pelvis and femur were made based on CT scans of 27 patients undergoing complex primary THR/Revision THR by FDM (Fusion Deposition Modeling) technology using Flash Forge–Dreamer 3D printer with ABS (plastic) material. Models were used for pre-operative planning and simulation of surgery. Aims of the study were to study the accuracy of 3D models in predicting the implant sizes, accuracy in evaluation of acetabular bone defects and validating the utility of 3 D models through surgeon feedback.
Results
The acetabular cup size and placement was accurate in 25 (92.6%) patients. Preoperative acetabular bone defect was accurately estimated in all the patients. There were no neurovascular complications at early and 1-year follow-up in this case series. Model realism and reliability survey response from five surgeons was graded, with average overall usefulness of 3D models of 4.86/5, average model realism was 4.9/5, average usefulness for planning was 4.74/5 and usefulness for teaching was 5/5.
Conclusion
3D models are accurate and help in assessing acetabular bone deficiencies reliably in complex and revision THR. Anatomical models help in surgical planning and simulation, enabling surgeons in predicting the correct implant sizes and importantly placement of acetabular cup and for management of bone defects. The safe trajectory of acetabular screws can be simulated and determined, thereby avoiding penetration into pelvis and neuro-vascular injuries.
Keywords: 3D-printing, Total hip arthroplasty, Planning, Revision arthroplasty, Pre-operative evaluation, Bone defects
1. Introduction
Pre-operative planning for total hip replacement (THR) is essential1 in complex primary (dysplastic hips, ankylosing spondylitis post-traumatic arthritis), and in revision/re-revision total hip arthroplasty, which are associated with acetabular and femoral bone deficiency.
The indications for Revision Total Hip Arthroplasty (R-THA) are varied and some of the common causes are aseptic loosening (50%), instability (16%), infection (15%), debilitating pain, periprosthetic fractures, or component failure.2,3 The incidence of revision THA has increased substantially during the last decade and is projected to nearly double by 2026.4 In R-THA severe acetabular defects are frequently encountered necessitating structural bone grafting, metal augments and even custom implants.5 This complicated articular reconstructive procedure requires a comprehensive understanding of the abnormal bony anatomy. Evaluation and classification of acetabular bone defects is essential to manage them appropriately.
Sengodan et al.6 performed a anthropometric analysis of the hip joint in South Indian population and reported significant differences in the size of acetabulum and proximal femora as compared to the Caucasian population. In many complex primary etiologies like dysplasia, ankylosed hip and post acetabular fractures, hip surgeons are often faced with challenges of size mismatch between the native acetabuli and the smaller implant sizes available. Templating on plain radiographs gives a rough estimate of component sizing and positioning.
Further evaluation of complex primary and revision hip surgery cases includes CT (Computed Tomography) scanning with 3D image rendering. However, this is a 2-dimensional representation of a complex 3-dimensional problem. Appreciation of this abnormality in 3D images on 2D screen is incomplete. Often, 3D images are studied closely, but, as mentioned above, appreciation of the abnormality in question may not always be obtained on a 2D screen. In revision scenario the utility may be limited by implant related artifacts. Life-size 3D printed models of pelvis and femur can be made from CT scans of patients with complex acetabular problems prior to THR/Revision THR by FDM (Fusion deposition modeling) technology. These 3D printed models have potential to provide both visual and tactile reproduction of the abnormal bony anatomy, with excellent accuracy.7
Though 3D printed patient specific custom implants are ideal in these types of cases, for THA using standard available implants 3D printed models are of great help in determining the size, augments and position of implant.
The aim of this study was to evaluate the accuracy of 3D-printing, by comparison of planned implant sizes and final implants used at the time of surgery. The secondary objectives of the study were to study:
-
a.
Accuracy of 3D printed models in the assessment acetabular bone-loss pre-operatively
-
b.
Evaluation of surgeon feedback on their experience using 3D printed models for complex primary and revision THA
2. Material and methods
This study was a retrospective study of patients who underwent total hip arthroplasty (THA) for complex primary or revision etiology, at a single institute between June 2015 to October 2019. Institutional Ethics Committee (IEC) approval was obtained for this study (SS/2015/IEC 193). Inclusion criteria-all patients who underwent complex primary or revision THA, with pre-operative 3D-modeling for planning and simulation of surgery. Twenty-seven patients were included in the study.
The 3D-printed models were assessed by the primary surgeon prior to surgery and the procedure was simulated on the models. The following parameters were evaluated during the simulation- Acetabular bone defect classification based on the Paprosky system, planned sizes of the acetabular reamers, acetabular and femoral component sizes. Accuracy of planned component sizing was evaluated against the actual components implanted during surgery.
Neurovascular complications in the immediate post-operative period and follow-up were obtained from case records and out-patient records.
3. 3D printing technique
All patients underwent pre-operative radiological evaluation with computed tomography scanning (CT) of pelvis and hips with 0.6 mm thickness CT slices (Siemens™ Somatom Perspective™ 64-slice CT scan system) and 3D models are printed in-house by the author according to the standard STL-based medical modeling protocol developed in the institute.
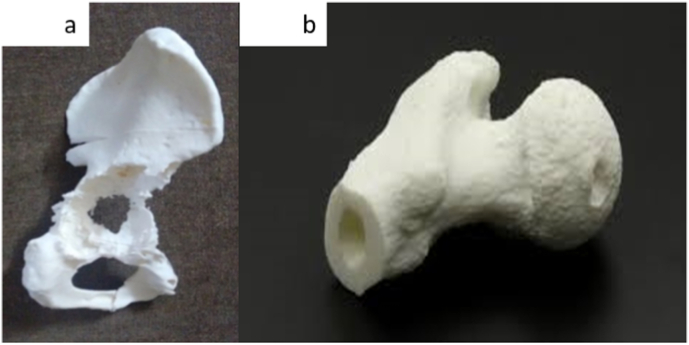
After CT scanning was completed, CT scan Digital Imaging and Communication in Medicine (DICOM) files were imported and 3D representation of the bone models was generated using InVesalius™ Software (Version 3.0.0. beta 5 software, Centre for Information Technology Renato Archer, Campinas, SP, Brazil). This software does automatic segmentation and converts DICOM files to STL (Standard Triangulation Language) file format using thresholding technique. STL file is a standard file format which is supported by almost all Rapid-Prototyping (RP) platforms, for medical modeling. The STL files were refined and cleaned using Mesh Laboratory – advanced 3D mesh processing software (Meshlab version 1.1.0, ISTI-CNR) and individual STL files were made. Slicing of these files is done using Slic3r™ slice engine with standard resolution (layer height 0.2 mm, shells 3, infill 20%, print speed 60 mm/s, travel speed 80 mm/s, extruder temperature 230°, platform temperature 110° and finally written in g-code file and transferred to printer. 3D models were printed using FlashForge Dreamer 3D printer (FlashForge Dreamer Dual Extruder) with 1.75 mm Acrylonitrile Butadiene Styrene (ABS) plastic filament. All the models are printed in-house by the author. The 3D printed models (Fig. 1) are anatomically accurate in size for templating.7
Fig. 1.
a–b: 3D printed hemi-pelvis and Femur.
4. Simulation of surgery on the 3D-models
The primary surgeon was able to plan and simulate a safe, successful surgical strategy on the models first. Templating was carried out by the surgeon in the weeks prior to surgery, and the implants were chosen accordingly. Preoperative bone loss was classified by the Paprosky8 system and was the grade of defect was confirmed based on intraoperative findings. Anatomical landmarks were marked on the pelvis. Acetabular cup size, augments, and buttress sizes, as well as cage dimensions, were selected and trialed in advance. The intraoperative size was compared to the planned preoperative size on the 3-D models. The models were durable to a degree that allowed preoperative surgical simulation of acetabular reaming, drill trajectory and screw positioning in cortical bone. Screw trajectory simulation was carried out on the models, allowing for improved accuracy and thus reducing the chance of intraoperative penetration into the pelvis, thereby reducing chances of neurovascular injury when screws were required outside the Lewinnek safe-zone. The models were also sterilized by Ethylene Oxide (ETO) and used for intra-operative reference.
5. Surgical technique
All 27 patients underwent primary or revision THA through the standard posterior approach in the lateral decubitus position.
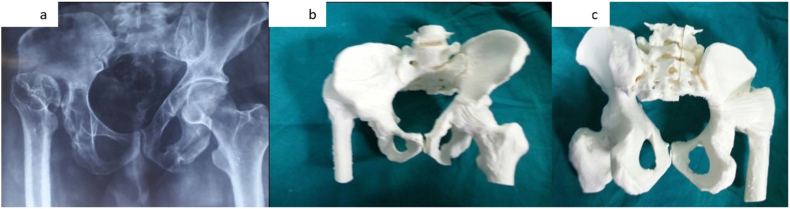
Case example 1: We illustrate a case of a 25-years old Female patient with a dysplastic right hip, Crowe Type IV. Fig. 2a–c shows the pre-operative radiograph and the corresponding 3D-printed model.
Fig. 2.
a–c: Fig. 2a. Pre-operative radiograph of the pelvis with both hips, showing Crowe Type IV dysplastic Right Hip; 2b: 3D printed model of the pelvis with both hips, life-size (Viewed from the front); 2c: 3D printed model of the pelvis with both hips, life-size (Viewed from behind).
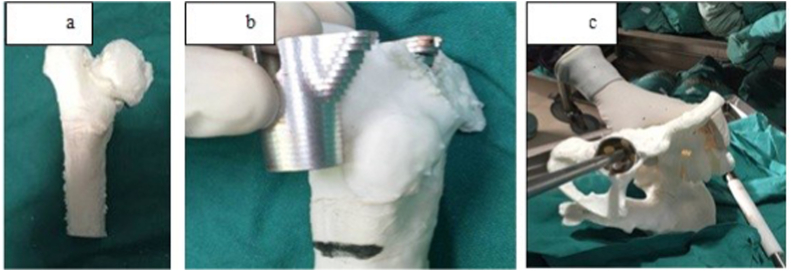
After adequate exposure, the surgeon proceeded with the preparation of the acetabular socket and femur. During concentric reaming of the acetabulum, the final reamer size was selected and reaming stopped based on pre-operative 3D-model simulation. Sizing of the components recorded during simulation on the 3D model were chosen and compared to the original anatomy of the patient and were found to be matching accurately (Fig. 3a–d).
Fig. 3.
a–c: Fig. 3a. 3D model of abnormal femur; 3b-sizing of DePuy Synthes S-Rom Metaphyseal sleeve on the model; 3c- Reaming and acetabular cup sizing on the model.
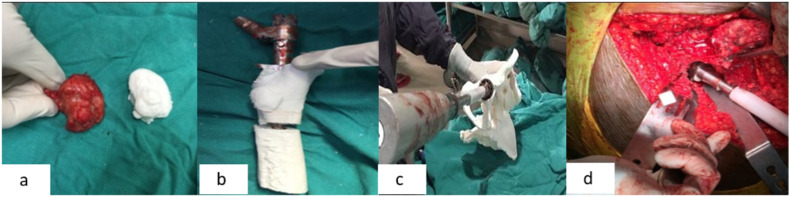
The anatomical sizing of the 3D model can be appreciated with the comparison of the deformed dysplastic femoral head and the model (Fig. 4a). The models were available on-table to evaluate and document accuracy of models used in templating and simulation, with native anatomy (Fig. 4b–d).
Fig. 4.
a–d: Fig. 4a Accurate size correlation between the 3D printed femoral head and the native femoral head; Fig.4b- Trialing of S-Rom sleeve and stem on the 3D model; Fig.4c- Reamer diameter first assessed on the 3D model intra-operatively and confirmed with the native acetabulum before preparation (Fig. 4d).
After completion of trialing based on the sizing of 3D models, stability of the hip was confirmed and final implantation was done. The post-operative radiograph shows appropriate sizing of components, restoration of limb-length and correct trajectory of screws placed (Fig. 5).
Fig. 5.
Post-operative radiograph after complex primary THA showing restoration of the hip centre, appropriate screw placement.
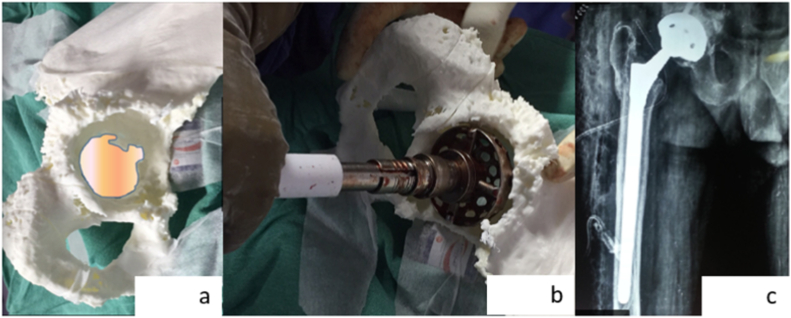
Case example 2: Revision total hip replacement surgery performed on a 72-year old male who had undergone primary THA five years before presenting to us, with significant pain in his right hip. The pre-operative radiograph shows obvious loosening of the acetabular component with high-grade protrusio (Fig. 6). CT scans were obtained and 3D model was printed for the pelvis, which showed a large medial defect but the columns were intact (Fig. 7a). The surgeon was able to size the acetabular reamer and component accurately (Fig. 7b), assess the bone defects and proceed with reconstruction. Reconstruction was successful with defect addressed adequately (Fig. 7c).
Fig. 6.
Pre-operative radiograph showing acetabular component loosening and high-grade protrusion of the acetabulum.
Fig. 7.
a–c: Fig. 7a. 3D printed model showing medial defect; 7b-accurate sizing of the reamer and component; 7c-post-operative radiograph showing hip restoration.
A survey was conducted to evaluate model realism, usefulness in planning and execution of surgery. Responses were obtained from five hip arthroplasty surgeons, who used these 3D-Models for THR.
6. Results
Of the 27 patients included in this study, there were 17 males (63%) and 10 (37%) females, with an average age of 43 years (Range 30–75 years). The mean follow-up duration was 14 months (±8.4 months). 17 (63%) patients underwent revision THA and 10 (37%) underwent complex primary THA. The indications for surgery are summarized in Table .1.
Table 1.
Summary of indications for surgery.
| Indication | Number (%) |
|---|---|
| Revision THA | 17 (63%) |
| Dysplastic Hips | 5 (18.5%) |
| Ankylosing spondylitis | 2 (7.4%) |
| Heterotopic Ossification of Hip | 1 (3.7%) |
| Post-Acetabular Fracture with arthritis | 2 (7.4%) |
| Total | 27 |
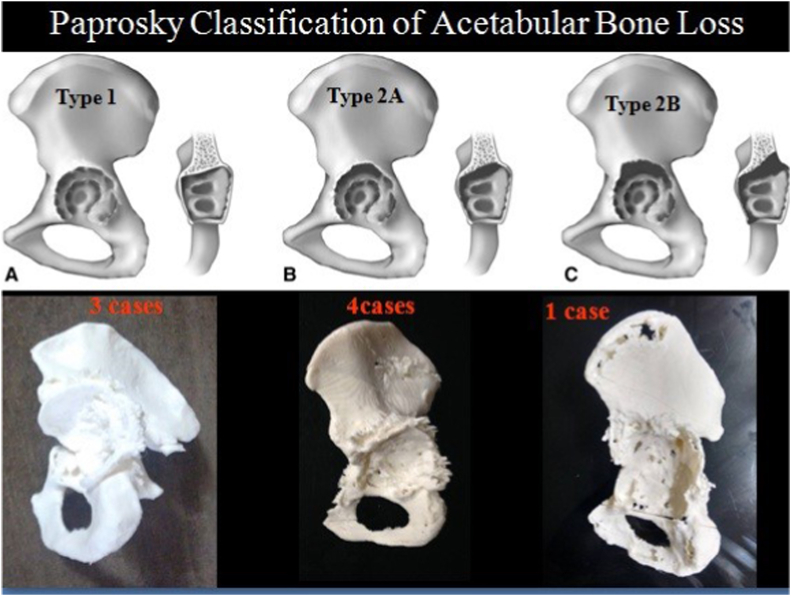
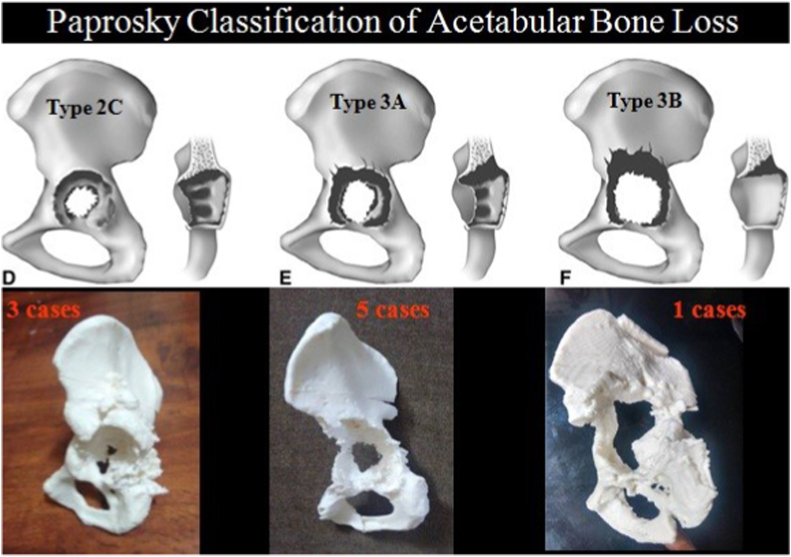
The acetabular cup size and placement was accurate in 25 (92.6%) cases. The templated size was not used in two cases which needed 2 mm larger acetabular cups. The screw trajectory planning was simplified with the model on-table for reference. there was 100% correlation with preoperative grading of acetabular defect as per the Paprosky classification system8 in all revision cases (Fig. 8a, Fig. 8ba and b).
Fig. 8a.
Paprosky Classification of Acetabular Defects and the corresponding anatomical 3D printed model for reference.
Fig. 8b.
Paprosky Classification of Acetabular Defects and the corresponding anatomical 3D printed model for reference.
17 (63%) cases of complex revision total hip arthroplasty were associated with acetabular bone loss, which was classified using the Paprosky classification system (Table .2).
Table 2.
Classification of Acetabular Bone Defects based on Paprosky classification.
| Paprosky Type | Number (%) |
|---|---|
| 1 | 3 (17.6%) |
| 2A | 4 (23.5%) |
| 2B | 1 (5.8%) |
| 2C | 3 (17.6%) |
| 3A | 5 (29.4%) |
| 3B | 1 (5.8%) |
| Total | 17 |
Survey responses obtained from five surgeons are summarized in Table .3. Average overall usefulness of 3D models was 4.86/5 among all surgeons. Average model realism was 4.9/5, average usefulness for planning was 4.74/5 and usefulness for teaching was 5/5 among all surgeons.
Table 3.
Survey response evaluating role of 3D models in complex primary and revision THR.
| Surgeons' Response |
I |
II |
III |
IV |
IV |
All surgeons |
|---|---|---|---|---|---|---|
| Out of 5a | Out of 5a | Out of 5a | Out of 5a | Out of 5a | Out of 5a | |
| MODEL REALISM | ||||||
| 1.Models are anatomically accurate | 5 | 5 | 5 | 5 | 5 | |
| 2.Models give better understanding and more information about abnormal pelvic anatomy than 3D images | 5 | 4 | 5 | 5 | 5 | |
| AVERAGE SCORE | 5 | 4.5 | 5 | 5 | 5 | 4.9 |
| PLANNING | ||||||
| 3.Pre op planning easy and better than templates | 5 | 5 | 5 | 5 | 5 | |
| 4.Models help in choosing the implant | 4 | 5 | 4 | 4 | 5 | |
| 5.Models was useful during surgery for reference | 5 | 5 | 5 | 5 | 4 | |
| 6.Over all useful for operative technique | 5 | 5 | 5 | 5 | 4 | |
| AVERAGE SCORE | 4.7 | 5 | 4.75 | 4.7 | 4.5 | 4.7 |
| TEACHING | ||||||
| 7.Useful for teaching complex THR | 5 | 5 | 5 | 5 | 5 | |
| 8.Useful for teaching surgical planning | 5 | 5 | 5 | 5 | 5 | |
| AVERAGE SCORE | 5 | 5 | 5 | 5 | 5 | 5 |
| USEFULLNESS IN COMPLEX PRIMARY AND REVISION THR | ||||||
| 9.Recommend to others to use | 5 | 5 | 5 | 4 | 5 | 4.9 |
| OVERALL USEFULLNESS | 4.9 | 4.9 | 4.9 | 4.8 | 4.8 | 4.86 |
Responses were graded on a 5-point Likert scale: 1-strongly disagree; 2, disagree; 3, neutral; 4, agree; 5, strongly agree.
7. Discussion
The results of the present study suggest that 3-D printing is accurate for preoperative implant size, augment requirement and acetabular bone defect assessment in complex primary and revision total hip arthroplasty.
Pre-operative planning is essential for successful THR surgery. This is of paramount importance in complex primary and revision cases which are associated with distorted anatomy and bone loss. Commonly used radiological modalities, apart from plain radiography, include CT scans with 3D Reconstruction. However, these reconstructions do not give the surgeon a tactile and spatial orientation.
CT Scan based 3D models are highly accurate in dimensions compared to native anatomy. Sariali et al.9 reported a high accuracy of planning using 3D CT scans. Gamble et al.10 reported a digital templating method that had an accuracy of 85% for the femoral stem and 80% for the acetabular component. However, these methods did not include THRs in severely deformed hips. The complex abnormal anatomy of the pelvis and the acetabulum makes preoperative assessment of such bony deficiencies in revision hip arthroplasty difficult.
Surgical planning is vital in cases of complex primary THA, revision THA and acetabular trauma. Hurson et al.11 reported their findings on the role of 3D printing in the management of acetabular fractures. It provided good surgical orientation and surgical plan/approach was changed in 2 cases based on the findings in the 3D printed models. With the use of 3D printing technology, pelvic deformities can be better evaluated by examining visual and tactile models of the patient's actual osseous anatomy. Life-size models allow accurate surgical simulation, enabling preoperative cup, augment, and buttress sizing, as well as cage templating and screw trajectory optimization. 3D models have also been described to be of significant use in acetabular surgery preoperatively when implants require contouring in three planes. Performing this in advance of surgery, combined with trialing the implant's positioning, reduces operative and anesthetic times.
Won et al.12 published their findings in the use of Rapid Prototype (RP) modeling in the pre-planning for complex THA in 21 patients. They found high accuracy of templating, sizing of implants used and reduced surgical time.
Sanchez-Perez et al.13 reported their use of 3D printing in the management of complex acetabular fractures with THA and concluded that 3D printing helped significantly in the management of delayed cases of post-acetabular fracture arthritis. Marongiu et al.14 studied rapid printing of 3D models in cases of peri-prosthetic acetabular fractures. They reported the difficulty of assessment with plain CT scans due to metal artifacts. This was overcome by 3D printed models with which surgeons can characterize defects quickly, to ensure adequate planning before surgery.
Tserovski15 et al. reported similar findings in revision total hip arthroplasty with their case report. Bagaria16 et al. did a study of post-surgery assessment of various fractures where 3D models were used. In their series the surgeons found that the model accurately represented the anatomy, helped in preoperative planning. In their series of 50 cases, only 6 cases were revision total hip arthroplasty.
Available studies on this topic are mostly case reports or small case series. We believe our study has a relatively larger sample size in comparison to existing literature on the role of 3D printed models in revision total hip arthroplasty. It also included a survey of the operating surgeons who documented high level of satisfaction with use of the models for preoperative planning, implant selection, teaching and overall ease of conducting the surgery in complex primary and revision situations.
Our study is not without limitations. We acknowledge the small numbers and drawbacks of a retrospective study. Also, clinical data regarding operative time, blood loss and follow up were not included. However, the study could demonstrate utility and accuracy of 3-D printing in the assessment of acetabular socket size and preoperative acetabular bone defect in patients undergoing complex primary and revision total hip arthroplasty. The assessment of bone defects by 3D-printing is a reliable and reproducible technique.
8. Conclusion
3D models help in greater understanding of bone deficiencies in complex primary and revision THR. 3D Models are accurate, allowing pre-operative surgical simulation and planning, and allow surgeons in deciding implant sizes and component positioning. The safe trajectory of acetabular screws can be determined accurately, thereby avoiding neuro-vascular injury. It may assist the surgeon to accurately assess bone defects and aid in defect management. 3D models help in predicting requirement of allograft, augments and cup-cage constructs or anti-protrusion cages which are not commonly available. Models are highly realistic and can be used reliably for simulation and teaching purposes.
Funding/sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Institutional ethical committee approval
This research was approved by the Institute Ethics Committee (SS/2015/IEC 193).
CRediT authorship contribution statement
Venkateshwar Reddy Maryada: Conceptualization, Methodology, Writing – original draft. Praharsha Mulpur: Writing – original draft, Writing – review & editing, Formal analysis. Krishna Kiran Eachempati: Methodology, Investigation, Data curation, Writing – review & editing. Adarsh Annapareddy: Formal analysis, Investigation. Vemaganti Badri Narayana Prasad: Supervision, Investigation. A.V. Gurava Reddy: Methodology, Resources, Writing – review & editing, Supervision.
Declaration of competing interest
None.
Acknowledgements
None.
Contributor Information
Venkateshwar Reddy Maryada, Email: reddymv@yahoo.com.
Praharsha Mulpur, Email: praharshamulpur9@gmail.com.
Krishna Kiran Eachempati, Email: kke1975@gmail.com.
Adarsh Annapareddy, Email: dradarshannapareddy@gmail.com.
Vemaganti Badri Narayana Prasad, Email: vemaganti.prasad@gmail.com.
A.V. Gurava Reddy, Email: guravareddy@gmail.com.
References
- 1.Eggli S., Pisan M., Müller M.E. The value of preoperative planning for total hip arthroplasty. J Bone Joint Surg Br. 1998 May;80(3):382–390. doi: 10.1302/0301-620x.80b3.7764. [DOI] [PubMed] [Google Scholar]
- 2.Wroblewski B.M. Current trends in revision of total hip arthroplasty. Int Orthop. 1984;8(2):89–93. doi: 10.1007/BF00265830. [DOI] [PubMed] [Google Scholar]
- 3.Ulrich S.D., Seyler T.M., Bennett D., et al. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008 Oct;32(5):597–604. doi: 10.1007/s00264-007-0364-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 5.Badarudeen S., Shu A.C., Ong K.L., Baykal D., Lau E., Malkani A.L. Complications after revision total hip arthroplasty in the medicare population. J Arthroplasty. 2017 Jun;32(6):1954–1958. doi: 10.1016/j.arth.2017.01.037. [DOI] [PubMed] [Google Scholar]
- 6.Sengodan V.C., Sinmayanantham E., Kumar J.S. Anthropometric analysis of the hip joint in South Indian population using computed tomography. Indian J Orthop. 2017;51(2):155–161. doi: 10.4103/0019-5413.201709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reddy M.V., Eachempati K., Gurava Reddy A.V., Mugalur A. Error analysis: how precise is fused deposition modeling in fabrication of bone models in comparison to the parent bones? Indian J Orthop. 2018;52(2):196–201. doi: 10.4103/ortho.IJOrtho_312_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paprosky W.G., Perona P.G., Lawrence J.M. vol. 9. 1994. (Acetabular Defect Classification and Surgical Reconstruction in Revision Arthroplasty A 6-Year Follow-Up Evaluation). 1. [DOI] [PubMed] [Google Scholar]
- 9.Sariali E., Mouttet A., Pasquier G., Durante E., Catone Y. Accuracy of reconstruction of the hip using computerised three-dimensional pre-operative planning and a cementless modular neck. J Bone Joint Surg Br. 2009 Mar;91(3):333–340. doi: 10.1302/0301-620X.91B3.21390. [DOI] [PubMed] [Google Scholar]
- 10.Gamble P., de Beer J., Petruccelli D., Winemaker M. The accuracy of digital templating in uncemented total hip arthroplasty. J Arthroplasty. 2010 Jun;25(4):529–532. doi: 10.1016/j.arth.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 11.Hurson C., Tansey A., O'Donnchadha B., Nicholson P., Rice J., McElwain J. Rapid prototyping in the assessment, classification and preoperative planning of acetabular fractures. Injury. 2007 Oct;38(10):1158–1162. doi: 10.1016/j.injury.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 12.Won S.-H., Lee Y.-K., Ha Y.-C., Suh Y.-S., Koo K.-H. Improving pre-operative planning for complex total hip replacement with a Rapid Prototype model enabling surgical simulation. Bone Joint Lett J. 2013 Nov;95-B(11):1458–1463. doi: 10.1302/0301-620X.95B11.31878. [DOI] [PubMed] [Google Scholar]
- 13.Sánchez-Pérez C., Rodríguez-Lozano G., Rojo-Manaute J., Vaquero-Martín J., Chana-Rodríguez F. 3D surgical printing for preoperative planning of trabecular augments in acetabular fracture sequel. Injury. 2018 Sep;49(Suppl 2):S36–S43. doi: 10.1016/j.injury.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 14.Marongiu G., Prost R., Capone A. Use of 3D modelling and 3D printing for the diagnostic process, decision making and preoperative planning of periprosthetic acetabular fractures. BMJ Case Rep. 2020 Jan;13(1) doi: 10.1136/bcr-2019-233117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tserovski S., Georgieva S., Simeonov R., Bigdeli A., Röttinger H., Kinov P. Advantages and disadvantages of 3D printing for pre-operative planning of revision hip surgery. J Surg Case Rep. 2019;2019:rjz214. doi: 10.1093/jscr/rjz214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bagaria V., Chaudhary K. A paradigm shift in surgical planning and simulation using 3Dgraphy: experience of first 50 surgeries done using 3D-printed biomodels. Injury. 2017 doi: 10.1016/j.injury.2017.08.058. [DOI] [PubMed] [Google Scholar]