Abstract
Much of young people’s fertility health knowledge has been limited to avoiding sexually transmitted infections and preventing pregnancy thus lacking what is necessary to support future overall health as well as reproductive goals. This study assesses university students’ knowledge related to fertility health factors to verify consistencies and discrepancies in fertility health knowledge, with a sub-assessment focusing on men’s knowledge. The Fertility Health Knowledge survey was delivered to 17,189 students at three American universities. Twenty percent or 546 of the 2,692 participants were male. The 30-question survey addresses knowledge of modifiable and non-modifiable risk factors on fertility health in men and women, and four questions regarding fertility intentions. Across all 30 questions, 63% of female responses were correct and 61% of male responses were correct. For 10 questions, less than 70% of males and females answered correctly, with men answering correctly more often than females for six of the questions. Males exhibited more knowledge regarding male fertility. Knowledge of fertility health was consistently limited, regardless of site or demographics. Men demonstrated improved overall fertility health knowledge and more knowledge regarding male factors. There are still considerable gaps in knowledge of modifiable risk factors that may impact fertility health and future overall health. Fertility health promotion through education should be comprehensive and widely available in secondary schools, colleges, and universities. As well, increased education regarding fertility health in primary care settings should become the norm—with male inclusion as a standard of their care.
Keywords: male fertility knowledge, male fertility health, health education, general health and wellness, health promotion, lifestyle modification
Fertility health knowledge is an essential component associated with fertility self-care among young people. Fertility self-care and knowledge of the issues associated with fertility and infertility are precursors to changing behaviors that may impair fertility and overall health. Avoiding sexually transmitted infections and preventing pregnancy are the typical limits of fertility knowledge in adolescents and young adults. For young men, the focus of “sex education” is typically the biology of reproduction, conception, and the use of condoms rather than actual “fertility education.” There is documentation that fertility health knowledge in young adults is lacking necessary content to support overall health and future reproductive goals (Boivin et al., 2018; Bunting et al., 2013; & Daumler et al., 2016).
Unhealthy lifestyle behaviors and associated risks related to body weight, nutrition, exercise, substance use, mental health, and sexual behaviors have been well studied in university students (Buhi et al., 2010; Capogrosso et al., 2018; Eisenberg et al., 2014). Demonstrating the breadth of this population, the percentage of students enrolling in college immediately following high school completion was 69.8% in 2016 (National Center for Education Statistics, 2020). College bound students, transitioning to independence from their parents, are faced with acceptance of personal responsibility for one’s health, including reproductive health. As such, assessing college students’ fertility health knowledge is an important step toward developing high-quality health information in the young adult population. Such knowledge identifies modifiable health behaviors that may form the foundation for health through their adult years.
The American College Health Association report (2019) identified modifiable health behaviors is a large study of 98 campuses and 67,972 students. The rate of overweight or obese was 37.3%, and only 4.3% consumed five or more servings of fruits and vegetables with the majority (62.7%) consuming 1 to 2 per day. Only 21.2% exercised 5 to 7 days/week. Use of substances as reported in the previous 30 days was: (1) tobacco cigarettes (6.4%), e-cigarettes (12.6%) and water pipe (2.1%), alcohol use (58.4%), and marijuana (22.1%). Although two thirds (66.9%) of students reported being sexually active, no other indicators of reproductive or fertility health were addressed.
Reproductive health is a sensitive marker for health behaviors and conditions that are associated with chronic disease that is, cancer, cardiovascular, and endocrine disease, later in life (Capogrosso et al., 2018; Eisenberg et al., 2014; Latif et al., 2017; & Senapati, 2018). Many of the same habits that promote cardiovascular health and reduce the risk of diabetes, such as healthy nutrition, exercise, and maintaining a healthy body weight, also support fertility (De Jonge & Barratt, 2019; Mahalingiah et al., 2017; Miner, 2012). Given the connection to possible future chronic disease, fertility health may sensitively reflect overall health in men and women. Although the lack of fertility health knowledge in general has been acknowledged in the past, the timing of optimal fertility health education is not well studied (Hashiloni-Dolev et al., 2011). There is some qualitative evidence that adolescence may not be ideal because of associated developmental challenges. Adolescents have difficulty relating to fertility and preconception health as this life event is perceived to be “important but far away” (Ekstrand Ragnar et al., 2018). Given this, it seems more studies are needed to determine best practices for fertility health education.
Postponement of Childbearing and Infertility Implications
Fertility declines as women age, and that delaying childbearing has been on the rise in recent decades (Nouri et al., 2014). Within the United States, the postponement of childbearing and the parallel rise in infertility rates is evident (Ledger, 2009; Levine et al., 2017; Nouri et al., 2014; and Sørensen et al., 2016). Of concern is that women tend to perceive fertility deadlines for their childbearing years as later than their actual biological deadlines, and that artificial reproductive technology can compensate for the declining fertility problems that arise with her age (Bretherick et al., 2012). Garcia et al. (2016) performed a systematic review of 41 studies that quantitatively measured fertility knowledge related to biological deadlines. Conclusions from this review indicated that “age-related fertility decline knowledge is insufficient, particularly in determining when female fertility markedly decreases.”
Daniluk and Koert (2013) also noted that the average age of childbearing in recent decades has been increasing in western societies and never before have parents had their first children as late as in recent decades. The reasons identified for postponement of motherhood were largely attributed to the clash between the optimal biological period for childbearing, and societal shifts in women obtaining education and building a career prior to building a family (Centers for Disease Control and Prevention, 2019). Men who delay fatherhood past 50 years old have recently been found to reduce the chances of successful births following pregnancies with assisted reproductive technology (Horta et al., 2019; Morris et al., 2021).
Fertility knowledge and attitudes have been assessed in numerous studies (Daniluk et al., 2012; Daumler et al., 2016; Deatsman et al., 2016; Hampton et al., 2013; Kudesia et al., 2017; Lundsberg et al., 2014; Peterson et al., 2012; Prior et al., 2019; & Sørensen et al., 2016). Generally, reproductive aged men and women are aware that fertility declines with age although they often are unaware of the age of the rapid rate of decline in fertility (Bretherick et al., 2012; Delbaere et al., 2020). Many early instruments designed to measure fertility knowledge and attitudes do not include information on male fertility and are fairly narrow in scope, that is, not including information about modifiable lifestyle issues and behaviors that are known to affect male fertility health. This gap in male-specific fertility health education has been acknowledged by a number of researchers who are calling for change in fertility health education to include male-specific factors (Bernardi et al., 2020; Harper et al., 2017; Pedro et al., 2018; Robins et al., 2016). In the related topic of preconception health knowledge, Cairncross et al. (2019) concluded that there is a need for a knowledge tool reflecting a holistic conceptualization of preconception health factors. Kruglova et al. (2021) importantly addressed this gap, noting that male infertility represents a public health issue, and subsequently introducing the development of a phone “app” to teach men about factors impacting male fertility. All this shines a light on the growing emphasis to include men in the fertility health discussions.
Terminology and Measurement of Fertility Health Knowledge
In 2007, the Centers for Disease Control, seeing infertility as a public health problem, set a priority regarding infertility prevention, noting there was a need for a national comprehensive plan (Centers for Disease Control and Prevention (a), 2020). Although there are programs addressing surveillance, research, and management, there remain gaps in communication and education of the public on fertility health topics (Centers for Disease Control and Prevention (b), 2020). The terms of fertility, infertility, fertility awareness, fertility knowledge, and fertility health are often misunderstood, and somewhat overlapping, topics in the public arena.
The literature on measuring fertility knowledge includes a variety of approaches to the issues surrounding fertility health and includes varying definitions and uses of fertility health knowledge and fertility awareness. Pedro et al. (2018) conducted a systematic review of fertility awareness studies. These authors defined Fertility Awareness with specific dimensions, for example, infertility, age-related fertility decline, and infertility risk factors. Authors cited the studies that explored those specific dimensions. Daniluk and Koert (2013) compared childless men’s and women’s knowledge of fertility and Assisted Reproductive Technology (ART) using the Fertility Awareness Survey which had been developed for women and later adapted for men. In their study, fertility awareness included items that reflected physiological, lifestyle, age, and knowledge of risks and success of ART and in vitro fertilization.
In one of the few population-based surveys, Bunting et al. (2013) examined fertility knowledge and beliefs in a large international sample (N = 10,045; Men = 1,690, 16.9%) using the Cardiff Fertility Knowledge Scale. This instrument consists of a 13-item correct/incorrect scale addressing risk factors, misconceptions, and basic fertility facts, with four items addressing male fertility factors. Men averaged 46.2% correct responses, while women averaged 59.1%. Daumler et al. (2016) also conducted a population-based survey (Canadian men; N = 701) regarding knowledge of male fertility (32 items), concluding that there were specific gaps in their knowledge, particularly about lesser known associations with male infertility factors impacted by modifiable lifestyle habits. Men were able to identify 51% of risk factors and 45% of health issues.
Knowledge of significant modifiable risk factors for fertility health is lacking (Capogrosso et al., 2018; Latif et al., 2017). Previous studies, generally narrow in scope, indicate that both men and women of reproductive age have misconceptions and gaps in their knowledge of fertility health in general, but that they would be receptive to receiving information on this important topic (Monester et al., 2019). With regard to men’s fertility knowledge, Hammarberg and colleagues (2017) posited that the previous lack of inclusion of men in fertility health studies is a reflection of outdated and ill-conceived beliefs that men play lesser roles in fertility planning and intentions toward fatherhood. Clinical practice applications of infertility risk assessments and fertility health knowledge have been recommended to be part of all clinical encounters in reproductive age patients (Morse & Moos, 2018), yet tools for this health education are lacking, and men are less often the focus when developing such tools. Recent attention toward the inclusion of men and clinical tools has seen some improvement.
Hammarberg et al. (2017) made the point that the strength of their fertility awareness study was the inclusion of men in their research, in that men needed to be aware of factors influencing and potentiating optimum fertility because childbearing required the efforts of both partners to be successful. The authors advocated that the impression of men not being interested in fatherhood was outdated and that gauging fertility awareness research predominantly on women as a whole ignored men’s importance in the equation.
The literature reflects that while there is a considerable amount of research on “fertility awareness,” researchers have either not defined the meaning of fertility awareness or the studies reflect a variety of definitions of fertility awareness and fertility knowledge. Fertility Awareness–Based Methods for family planning is yet another use of the term. In some studies, fertility knowledge may simply mean knowledge of the fertile window (Righarts et al., 2017). For the purposes of this study, fertility health knowledge is defined as the knowledge of modifiable and non-modifiable fertility risk factors in men and women including lifestyle as well as the physiologic facts of reproduction.
Aims
The purpose of this study was to assess university students’ current knowledge of modifiable and non-modifiable factors related to fertility health using the validated Fertility Health Knowledge Survey (FHKS) (Barron et al., 2020). A sub-analysis of the data was performed with the added aim of examining fertility health knowledge in men at this point in time.
Methods
Study Design
This analysis to assess gender responses is a subset of a prospective cross-sectional exploratory survey design. The study was approved by the IRB at each respective United States’ university as Exempt: Southern Illinois University Edwardsville (SIUE), University of Delaware (UD), and Western University of Health Sciences (WUHS). The Fertility Health Knowledge Survey was administered online via Qualtrics®. To address the variability and heterogeneity of the sample, with the goal of increasing reliability, all undergraduate and/or graduate students at SIUE, UD, or WUHS were eligible to participate.
Participants
Although this is a convenience sample, university students were chosen for this study. The assumption is that they represent young adults who were the most likely to have previously acquired some formal and informal knowledge regarding fertility health. SIUE, UD, or WUHS educate undergraduate and graduate students in a variety of majors including health sciences; WUHS educates all graduate health-professions students. All students were invited by email to complete the online FHKS. Student identity was anonymous. Agreeing to complete the survey was taken as consent to participate. Respondents answering all questions were entered in a drawing for a US$100 gift card.
Instrument
The FHKS (Table 1) addresses knowledge and intentions toward male and female modifiable and non-modifiable risk factors on fertility health and may provide a framework for educating young men and women about this area of their health. As such, the 34-item survey (30 “question” items and four “intentions” items) was designed to be used either as an educational tool in the practice setting or for data collection in fertility health research. In clinical practice, the clinician might have the patient answer the survey ahead of the encounter and subsequently discuss the findings together as part of the health visit. With this scale, clinicians can assess confidence in the response chosen and tailor the education. Garcia et al. (2016) reported that tailored oral education in clinical practice, using a focused instrument, was successful in improving fertility knowledge outcomes during patient encounters.
Table 1.
Fertility Health Knowledge Questions and Abbreviations.
| Abbreviation for question | Full question |
|---|---|
| Couple Items | |
| Infertility rate, couples a | About 10% of couples are not fertile |
| Couple infertility at 1 year | A couple is considered infertile if they did not achieve a pregnancy after 1 year of regular sexual intercourse |
| History of STD, effect on fertility b | People who have had a sexually transmitted infection are likely to have reduced fertility. |
| Dietary fat type, healthy fertility | The type of fat in the diet is important to healthy fertility. |
| Female Items | |
| Ovulation, frequency MC (menstrual cycle) | A woman ovulates once in a menstrual cycle. |
| Rapid weight change, MC effect | If a woman gains or losses weight rapidly it can disrupt the menstrual cycle. |
| Percent body fat, ovulation | The average woman needs at least 18% body fat in order to ovulate. |
| Irregular cycles, frequency | Irregular cycles are those that occur less than 9 times a year. |
| “Normal” MC variation | It is “normal” for the menstrual cycle to vary in the length of cycle by a few days such as 27 days to 35 days to 29 days |
| Emotional stress, MC effect | Suffering emotional stress can alter the usual length of the menstrual cycle. |
| Worrying about, MC effect | Worrying about exams or losing a job can affect the length of the cycle. |
| Marijuana, effect on MC | Marijuana can disrupt women’s menstrual cycles. |
| Tobacco use, woman’s fertility | Tobacco use can lower fertility in a woman. |
| Second-hand smoke, woman’s fertility | Second-hand smoke exposure can lower fertility in a woman. |
| Exercise, woman’s fertility | Exercise in moderation is good for a woman’s fertility. |
| Light on at night, effect on woman’s fertility | Leaving the light on at night during sleeping can have an effect on fertility in some women |
| Working night shifts, effect on woman’s fertility | Working night shifts can reduce fertility in some women. |
| Woman’s age, fertility rate | Women over the age of 35 are less fertile than women under the age of 35. |
| Sperm survival in woman’s body | Sperm can live for 3–5 days in the woman’s body when the woman is in the fertile phase of the cycle. |
| Male Items | |
| Male age, fertility | Men over the age of 40 are less fertile than men under the age of 40. |
| Marijuana, effect on sperm | Marijuana decreases the quality of a man’s sperm. |
| Tobacco use, male fertility | Tobacco use can lower fertility in a man. |
| Trans-fat in the diet . . . sperm | Trans-fats consumed in the diet can later be found in human sperm. |
| >3 caffeinated colas/day and sperm c | Drinking more than 3 caffeinated colas a day can decrease the sperm count. |
| Steroid use, effect on male fertility | Using steroids to build muscles has a negative effect on a man’s fertility by decreasing sperm counts. |
| Intense exercise, male fertility | Intense exercise will decrease male fertility. |
| Obesity, male fertility | Obesity is associated with decreasing male fertility. |
| Erection, fertility status a | As long as a man can have an erection, he is fertile. |
| Cell phone, effect on sperm d | Carrying a cell phone in the pants pocket can lower sperm quality. |
| Laptop use, scrotal temperature | Continuously using a laptop on the lap for one or more hours can increase the temperature of the scrotum and have an effect on sperm quality. |
Note. Answers are true with these exceptions: a False. b The current rate of infertility is closer to 15%. c Unsure as some sexually transmitted infections do not lead to infertility. d Unsure because there is some evidence but not well-studied or conflicting results.
The 30 items include 14 female, 12 male, and four “couples” statements addressing “fertility facts,” lifestyle and fertility, and “age and fertility.” Response categories are on a five-point Likert-type scale (definitely yes, probably yes, unsure, probably not, definitely not). Survey items were informed by evidence- and practice-based indicators, expert opinion, and a review of related literature. To assess intentions, participants were asked to identify if they had children, their desire to have children, the planned or actual age for first child, and planned or actual age for last child. The FHKS instrument has shown to be internally consistent and reliable short screening tool in a previous study (Barron et al., 2020). Responses to the survey indicated the student’s extent of agreement using a 5-point Likert-type scale. Student responses were then categorized as “correct” or “incorrect,” irrespective of confidence, for the purpose of this sub analysis. Therefore, “definitely/probably” responses were not distinguished in regards to correctness. Question answers are reflected in Table 1. Development of the survey tool and psychometric evaluation is published elsewhere (Barron et al., 2020).
Demographic variables included in this study were as follows: gender, race (African American, Caucasian, Hispanic, Asian American, Native American, Other), and age (17–22, 23+ years). The university that the student attended was also identified.
Data Analysis
All statistical analyses were performed in SAS, version 9.4. Student response was categorized as correct (coded as “1”) or incorrect (coded as 0) for all 30 questions retained for analysis. A Wilcoxon two-sample test was used to compare the age between students that responded correctly to students that responded incorrectly due to the distribution of age being right-skewed and violating the normality assumption (p < .01). A Fisher’s Exact Test was used to compare percentage of correct responses between age group for each question. Age group was defined as younger if the student was less than 23 and older if the student was 23 or older. A Fisher’s Exact Test was also used to compare percentage of correct responses between genders for each question. Significance was set at the 0.05 level, but adjusted for multiple comparisons using a Bonferroni correction. Thus, significance was determined at the 0.0016 level after adjusting for the 30 questions. A Wilcoxon Two-sample test was also used to compare intentions (number of children, planned/actual age of first child, and planned/actual age of last child) between gender due to the distribution of intention variables being either left or right-skewed and violating the normality assumption (p < .01).
Results
Overall Fertility Health Knowledge
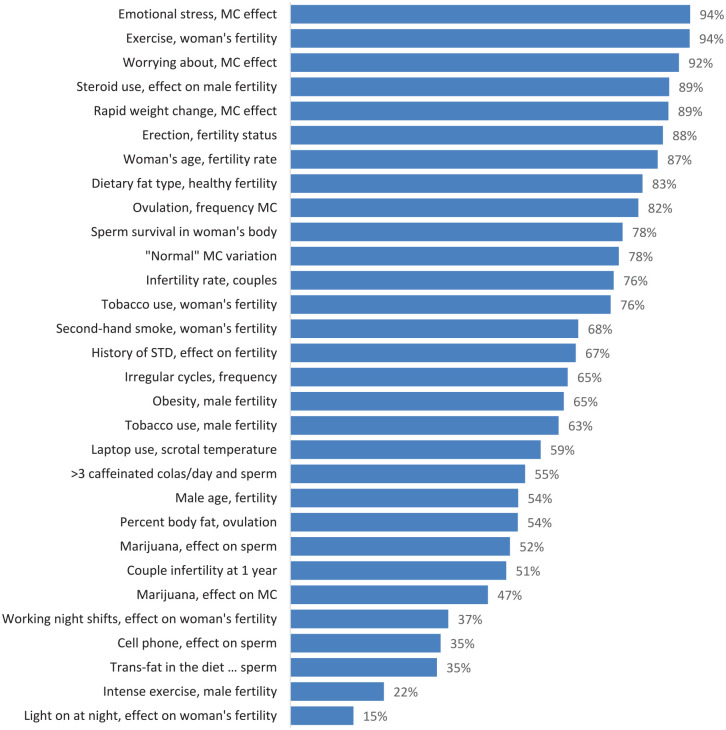
The FHKS was delivered to 17,189 students. There were 2,692 student responses (15.7% response rate). Males (546) comprised 20.2% of responses (Table 2). Age ranged from 17 to 54 years with an average age of 22.5 (standard deviation [SD] of 4.5). The majority of respondents identified as Caucasian (2043, 75.8%) followed by 223 (8%) identifying as African American, 159 (5.9%) as Asian American, 130 (4.8%) as Hispanic, 11 (0.04%) as Native American and 126 (4.7%) as “Other.” More demographic information by school can be found in Table 2. Thirteen of the 30 questions were answered correctly by 70% or more of respondents with the greatest percentage of correct responses being 94.4%. The distribution of overall correct responses can be seen in Figure 1.
Table 2.
Demographic Characteristics by School.
| Gender | Race/Ethnicity | Age | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| School | Male | Female | African Am |
Asian Am |
Caucasian | Hispanic | Native Am |
Other | 17–22 Years |
23 + years |
| SIUE N=1724 |
389 22.5% |
1,335 77.4% |
182 10.5% |
47 2.7% |
1,339 77.6% |
68 3.9% |
6 0.03% |
82 4.7% |
1,417 82.1% |
307 17.8% |
| UD N=595 |
72 12% |
523 88% |
31 0.05% |
29 0.05% |
495 83% |
22 3.6% |
1 0.1% |
17 2.8% |
473 79% |
122 20% |
| WUHS N=373 |
85 22.7% |
288 77.2% |
10 2.6% |
83 22.2% |
209 56% |
40 10.7% |
4 1% |
27 7.2% |
25 6.7% |
348 93.2% |
| Total | 546 20.2% |
2,146 79.7% |
223 8.2% |
159 5.9% |
2,043 75.8% |
130 4.8% |
11 0.04% |
126 4.7% |
1,629 60.5% |
777 29% |
Figure 1.
Percentage of Correct Responses by Fertility Health Question.
Gender Differences in Fertility Health Knowledge
Fertility health knowledge was compared between men and women respondents. Across all 30 questions, 66% of female responses were correct and 63% of male responses were correct. Table 3 shows the questions with significant gender differences and those without. Seventeen of the 30 questions exhibited significant differences in the percentage correct between genders. Respondents were considered “knowledgeable” if 70% or more answered correctly. An “unsure” response was incorrect unless the correct answer was “unsure.” For the seven questions where more than 70% of respondents answered correctly, more women were correct than men. The difference in percent correct responses between men and women ranged from 4% to 15% with an average percent difference of 9%. The largest discrepancy was seen in the question, “A women ovulates once in a menstrual cycle.” For 10 questions, less than 70% of men and women answered correctly, with men answering correctly more often than women for six of the questions. The discrepancy when men answered correctly more often was 9% on average compared to 14% discrepancy when women answered correctly more often.
Table 3.
Percentage Correct Responses With Gender Differences.
| Fertility health question | |||
|---|---|---|---|
| ≥70% Women and men answered correctly | Female | Male | Signif. |
| (F) Emotional stress, MC effect | 95.8% | 89.0% | *** |
| (F) Exercise, woman’s fertility. | 95.1% | 91.2% | ** |
| (F) Worrying about, MC cycle | 93.2% | 85.9% | *** |
| (F) Rapid weight change, MC effect | 91.9% | 79.1% | *** |
| (F) Woman’s age, fertility rate | 88.4% | 80.4% | *** |
| (F) Ovulation, frequency MC | 85.1% | 70.5% | *** |
| (F) Sperm survival in woman’s body | 80.1% | 72.0% | *** |
| (M) Steroid use, effect on male fertility | 89.8% | 88.1% | |
| (M) Erection, fertility status | 88.0% | 87.9% | |
| (C) Dietary fat type, healthy fertility | 83.8% | 80.4% | |
| (F) “Normal” MC variation | 78.7% | 73.3% | |
| (F) Tobacco use, woman’s fertility | 75.6% | 75.6% | |
| ≥70% Women Answered Correctly and <70% Men Answered Correctly | |||
| (C) Infertility rate, couples | 78.4% | 68.1% | *** |
| <70% Women Answered Correctly and ≥70% Men Answered Correctly | |||
| (F) Second-hand smoke, woman’s fertility | 67.1% | 71.6% | |
| <70% Women and Men Answered Correctly | |||
| (C) History of STD, effect on fertility | 69.6% | 58.8% | *** |
| (F) Irregular cycles, frequency | 68.0% | 56.0% | *** |
| (F) Percent body fat, ovulation | 57.4% | 39.2% | *** |
| (M) Laptop use, scrotal temperature | 56.6% | 69.1% | *** |
| (M) >3 caffeinated colas/day and sperm | 53.5% | 63.2% | *** |
| (M) Male age, fertility | 52.1% | 60.3% | ** |
| (F) Working night shifts, effect on woman’s fertility | 35.2% | 45.4% | *** |
| (M) Trans-fats in the diet . . . sperm | 32.9% | 41.2% | ** |
| (F) Light on at night, effect on woman’s fertility | 13.6% | 20.0% | ** |
| (M) Obesity, male fertility | 65.2% | 62.1% | |
| (M) Tobacco use, male fertility | 62.6% | 66.1% | |
| (C) Couple infertility at 1 year | 52.1% | 46.3% | |
| (M) Marijuana, effect on sperm | 52.0% | 51.5% | |
| (F) Marijuana, effect on MC | 45.7% | 50.4% | |
| (M) Cell phone, effect on sperm | 36.3% | 32.2% | |
| (M) Intense exercise, male fertility | 23.0% | 18.7% | |
Note. Dark blue denotes women’s knowledge greater than men’s. Light blue denotes men’s knowledge is greater than women’s knowledge. (F) = Female Item; (M) = Male Item; (C) = Couples Item.
0.0010 < p < .0016. **0.0001 < p < .0009. ***p < .0001.
Gendered (male and female related) fertility health items were examined for correct responses by men and women to determine whether men were more or less familiar with male fertility health issues and whether females were more or less familiar with female fertility health issues. Nine female fertility items were answered correctly by both men and women more than 70% of the time, and nine of the male fertility items were answered correctly by both men and women less than 70% of the time. The couples’ fertility item correct responses were distributed between those groups.
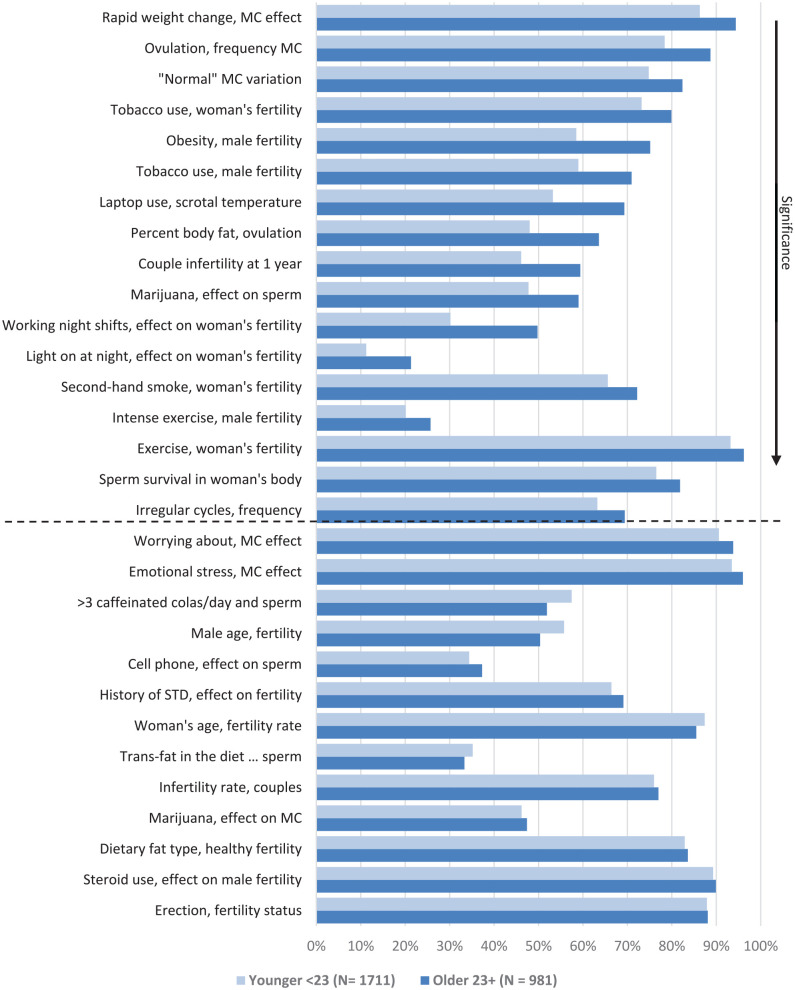
Age Differences in Fertility Health Knowledge
Fertility health knowledge was also compared between younger and older respondents (Figure 2). There were significant differences in the percentage of correct responses between younger and older respondents for 17 of the 30 fertility health questions (p < .0016). When there was a significant difference, older students responded correctly more often than the younger. The largest percent difference seen between age groups was 20% for the question, “working night shifts can reduce fertility in some women.” Fifty percent of older students responded correctly to this question compared to only 30% of younger students.
Figure 2.
Percentage of Correct Responses by Fertility Health Question and Age Group.
Note. Questions above the dashed line exhibit a statistically significant difference between age groups (p < .0016).
Intentions
In the combined sample of 2,692 students, 2,468 (91.6%) affirmed the desire for future children, 206 (0.076%) did not want children and 18 (0.006%) students gave no response. In comparing men and women on the questions regarding intentions for children: the number of children, the planned or actual age for the first child, and the planned or actual age for the last child produced the following results: there was no significant gender difference in the number of children desired (Z = −1.74, p = .082). There is a significant difference in the planned ages to have first and last children. Men were slightly older than women, but this difference was not clinically different (i.e., 27.4 vs. 27.9) and (32.8 vs. 33.5). The desired age of first child for females was (Z = 3.9, p < .0001) 27.4 (3.2) versus 27.9 (3.3) for males. The desired age of last child for females (Z = 3.7, p = .0002) 32.8 (3.7) versus 33.5 (4.4) for males.
Discussion
The overarching aim of this research was to assess the level of knowledge of modifiable and non-modifiable fertility health factors in young adults and adults, using university students as a likely knowledgeable representation of that population. The response rate of 15.1% is low but is consistent with previous studies on this topic, ranging from 15.1% to 31%. The proportion of male respondents at 20% is also consistent at a range from 15.2% to 22.5% male participation in previous studies (Bretherick et al., 2012; Bunting et al., 2013; Monester et al., 2019; Sørensen et al., 2016). Through that lens, the new finding of this study was that men and women performed comparably in the percentages of questions answered correctly on the Fertility Health Knowledge Survey. This was significantly different than prior fertility health knowledge studies where men often were less knowledgeable than women overall and had deficits in gender specific fertility knowledge (Daumler et al., 2016; Peterson et al., 2012). Collectively, questions were answered correctly more than 70% of the time nearly equally by both men and women (men 14 items and women 13 items). When looking at the range between 50% and 70% correctly answered, men and women were consistent at 11 items apiece. The lower range of less than 50% answered correctly was also nearly evenly split with men at five and women at six items.
In that both men and women answered the same 12 questions correctly greater than 70% of the time, gender specificity in correctly answered questions was not evident. Yet, within those 12 questions men did score lower on all questions, with the difference between 9% and 14% scoring correctly. This demonstrated that in this study men did close the fertility health knowledge gap over previous studies, with even further growth in knowledge still a potential. A clear example of this was that both men and women knew that women ovulated once per menstrual cycle greater than 70% of the time, but women were correct 85.1% of the time and men were correct at 70.5% frequency. Thus, in this item’s knowledge area, men have more growth potential.
Survey items specific to “male” and “female” fertility health issues are those that impact male body fertility and those that affect female body fertility. While previous studies demonstrated differing knowledge between men and women on male and female fertility items, (Bernardi et al., 2020; Hammarberg et al., 2017), this study found both men and women similarly exhibited correct knowledge, and narrowed knowledge gaps, on male and female fertility items. Since the Fertility Health Knowledge tool reflects both male- and female-specific fertility questions, along with couples’ questions (Table 1), the common perception that men would know more about male fertility issues and women would know more about female issues was challenged. Nine female items were answered correctly by men and women greater than 70% of the time (Table 3). With a similar demonstrable knowledge deficit on display, nine male items were answered correctly by men and women less than 70% of the time. Knowledge strengths and weaknesses were evident in men and women equally across male and female fertility health issues. However, as with the overall correctly answered questions, there is a significant difference in the percent answering male and female items correctly (>70%) in that women’s percentages were higher than men’s on seven questions which were female items. There were only two items in which men and women differed in their rate of answering these male/female item questions correctly (>70%). Knowledge gaps in this population have been consistent across findings in previous studies in which participants demonstrated limited and/or inaccurate fertility knowledge of predominantly female factors with women comparatively more knowledgeable than men (Daumler et al., 2016; Lundsberg et al., 2014; Peterson et al., 2012).
Knowledge of female fertility health and the effects of age on reproduction are far more studied than knowledge of male fertility health. Participation by men is often less than participation by women in fertility health studies. In a large international study (N = 10,045) including 79 countries, the proportion of men in the sample was 16.8% (Bunting et al., 2013). When including men, studies on the topic vary in the number of “male fertility” items, which are frequently less than “female fertility” items, with gender specificity present. (Bernardi et al., 2020; Bunting et al., 2013; Daniluk et al., 2012; Maeda et al., 2016; Peterson et al., 2012; Prior et al., 2019). The effect of lifestyle factors on fertility (particularly in males) is an area in this body of work that is evolving. Daumler et al. (2016), in studying men’s knowledge of male fertility, reported mean scores on three categories of modifiable, fixed, and health factors (32 total items) associated with male infertility. Men’s knowledge scores in these categories were low, 53.1%, 46.9%, and 45.0%, respectively. This study, a few years later, demonstrates significant increases in men’s understanding of male fertility knowledge in two modifiable and fixed items (88.1% and 87.9%), but lagging knowledge in eight items reflecting modifiable, fixed and health issues (ranging from 18.7% to 69.1%). Thus, improving the picture for knowledge in men.
Strengths and Limitations
Giving strength to this study, participants came from three universities in different US regions which increases generalizability of the findings. Undergraduate and graduate level students of a wide range of ages were included, also increasing the generalizability of this study to the larger population of college students and their fertility knowledge. Although men were well represented in raw numbers (n = 546), they comprised only 20.2% of the overall sample. This may lead to results not reflecting actual understanding of fertility health in this population.
An additional limitation of this study is that African American (8.2%) and Hispanic American participants (4.8%) are underrepresented when compared to the US Census proportions for each race (13.4% and 18.3%; U.S. Census Bureau Quick Facts, n.d.). Asian-Americans were proportionate across the universities but only due to the high percentage from WUHS, which has a high percentage of Asian-American students (Table 2).
Another limitation is the few questions in the survey tool on the environmental impact of emerging technologies and other environmental factors on fertility health. At the writing, the science on this topic is rapidly evolving.
Conclusions
The Fertility Health Knowledge Survey is a valid and reliable, short, screening tool aimed at both men and women that can be used as a research instrument and to assess knowledge of fertility self-care and identify misconceptions on this topic during a clinical encounter. While the findings of this study demonstrate that men are gaining in the area of fertility health knowledge and closing the knowledge gap between men and women. the findings suggest that young adults would benefit from more information about fertility health, especially about lifestyle issues that are known to affect fertility health and possibly reduce risk of infertility and, significantly, chronic disease later in life. The clinical encounter is an ideal setting for this client education, and the use of the FHKS tool during such encounters would afford the opportunity to identify knowledge gaps and specific educational need in both men and women alike. Gathering clinical information in a way that health care providers can readily provide corrective measures would be helpful in reducing risk to future fertility health in both men and women.
As part of a coordinated health education effort in this area, fertility health promotion through education about human fertility health, as recommended by the Centers for Disease Control, should be comprehensive and widely available on university and college campuses, and potentially in younger formative years as well. As noted, many of the same lifestyle habits promoted to reduce chronic disease risk also promote healthy fertility in both men and women (e.g., healthy weight, decreased substance use, and others).
The struggle of infertility has emotional, relational, and financial implications. Including fertility health as an essential and consistent component of overall health education, at various ages and entry points, would likely positively impact fertility outcomes, and tangentially, positively impact overall health outcomes as a positive consequence. While there has been an increased effort to include men in these educational opportunities, more can and should be done. The results of this study suggest that a move toward a focus on fertility health education for men and women, including modifiable health behaviors, is an important consideration. It is time to take steps to include fertility health education in the public health and clinical practice arenas for both women and men.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Mary L. Barron  https://orcid.org/0000-0002-8323-398X
https://orcid.org/0000-0002-8323-398X
References
- American College Health Association. (2019). American College Health Association-National College Health Assessment II. Reference group executive summary (2019). American College Health Association. https://www.acha.org/documents/ncha/NCHA-II_SPRING_2019_US_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf [Google Scholar]
- Barron M. L., Lithgow D., Wade G., Mueller–Luckey G. H. (2020) Measuring fertility health knowledge in university students: Development and testing of a survey tool. Journal of Nursing Measurement, 28(1), 43–59. 10.1891/JNM-D-18-00060 [DOI] [PubMed] [Google Scholar]
- Bernardi L. A., Luck M., Kyweluk M. A., Feinberg E. C. (2020). Knowledge gaps in the understanding of fertility among non-medical graduate students. Fertility & Sterility Reports, 1(3), 177–185. 10.1016/j.xfre.2020.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boivin J., Koert E., Harris T., O’Shea L., Perryman A., Parker K., Harrison C. (2018). An experimental evaluation of the benefits and costs of providing fertility information to adolescents and emerging adults. Human Reproduction, 33(7), 1247–1253. 10.1093/humrep/dey107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bretherick K., Fairbrother N., Avila L., Harbord S. H., Robinson W. P. (2012). Fertility and aging: Do reproductive-aged Canadian women know what they need to know? Fertility & Sterility, 93, 2162–2168. 10.1016/j.fertnstert.2009.01.064 [DOI] [PubMed] [Google Scholar]
- Buhi E., Marhefka S., Hoban M. (2010). The state of the union: Sexual health disparities in a national sample of US college students. Journal of American College Health, 58(4), 337–346. 10.1080/07448480903501780 [DOI] [PubMed] [Google Scholar]
- Bunting L., Tsibulsky I., Boivin J. (2013). Fertility knowledge and beliefs about fertility treatment: Findings from the International Fertility Decision-making Study. Human Reproduction, 28(2), 385–397. 10.1093/humrep/des402 [DOI] [PubMed] [Google Scholar]
- Cairncross Z. F., Ravindran S., Yoganathan S., Dennis C. L., Enders J., Graves L., Mill C., Telner D., Brown H. K. (2019). Measurement of preconception health knowledge: A systematic review. American Journal of Health Promotion: AJHP, 33(6), 941–954. 10.1177/0890117119835518 [DOI] [PubMed] [Google Scholar]
- Capogrosso P., Ventimiglia E., Boeri L., Cazzaniga W., Chierigo F., Montorsi F., Salonia A. (2018). Male infertility as a proxy of the overall male health status. Minerva Urologica e Nefrologica = The Italian Journal of Urology and Nephrology, 70(3), 286–299. 10.23736/S0393-2249.18.03063-1 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2019). National Survey of Family Growth. https://www.cdc.gov/nchs/nsfg/key_statistics/i-keystat.htm#impaired
- Centers for Disease Control and Prevention (a). (2020). A public health focus on infertility prevention, detection, and management. https://www.cdc.gov/reproductivehealth/infertility/whitepaper-pg1.htm#three
- Centers for Disease Control and Prevention (b). (2020). CDC programs and activities. https://www.cdc.gov/reproductivehealth/infertility/resources.html
- Daniluk J. C., Koert E. (2013). The other side of the fertility coin: A comparison of childless men’s and women’s knowledge of fertility and assisted reproductive technology. Fertility & Sterility, 99(3), 839–846. 10.1016/j.fertnstert.2012.10.033 [DOI] [PubMed] [Google Scholar]
- Daniluk J. C., Koert E., Cheung A. (2012). Childless women’s knowledge of fertility and assisted human reproduction: Identifying the gaps. Fertility and Sterility, 97(2), 420–426. 10.1016/j.fertnstert.2011.11.046 [DOI] [PubMed] [Google Scholar]
- Daumler D., Chan P., Lo K. C., Takefman J., Zelkowitz P. (2016). Men’s knowledge of their own fertility: A population-based survey examining the awareness of factors that are associated with male infertility. Human Reproduction, 31(12), 2781–2790. 10.1093/humrep/dew265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deatsman S., Vasilopoulos T., Rhoton-Vlasak A. (2016). Age and fertility: A study on patient awareness. JBRA Assisted Reproduction, 20(3), 99–106. 10.5935/1518-0557.20160024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jonge C., Barratt C. (2019). The present crisis in male reproductive health: An urgent need for a political, social, and research roadmap. Andrology, 7(6), 762–768. 10.1111/andr.12673 [DOI] [PubMed] [Google Scholar]
- Delbaere I., Verbiest S., Tydén T. (2020). Knowledge about the impact of age on fertility: A brief review. Upsala Journal of Medical Sciences, 125(2), 167–174. 10.1080/03009734.2019.1707913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg M. L., Li S., Behr B., Cullen M. R., Galusha D., Lamb D. J., Lipshultz L. I. (2014). Semen quality, infertility and mortality in the USA. Human Reproduction, 29(7), 1567–1574. 10.1093/humrep/deu106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekstrand Ragnar M., Grandahl M., Stern J., Mattebo M. (2018). Important but far away: Adolescents’ beliefs, awareness and experiences of fertility and preconception health. The European Journal of Contraception & Reproductive Health Care: The Official Journal of the European Society of Contraception, 23(4), 265–273. 10.1080/13625187.2018.1481942 [DOI] [PubMed] [Google Scholar]
- Garcia D., Vassena R., Prat A., Vernaeve V. (2016). Increasing fertility knowledge and awareness by tailored education: A randomized controlled trial. Reproductive BioMedicine Online, 32, 113–120. 10.1016/j.rbmo.2015.10.008 [DOI] [PubMed] [Google Scholar]
- Hammarberg K., Collins V., Holden C., Young K., McLachlan R. (2017). Men’s knowledge, attitudes and behaviours relating to fertility. Human Reproduction Update, 23(4), 458–480. 10.1093/humupd/dmx005 [DOI] [PubMed] [Google Scholar]
- Hampton K. D., Mazza D., Newton J. M. (2013). Fertility-awareness knowledge, attitudes, and practices of women seeking fertility assistance. Journal of Advanced Nursing, 69(5), 1076–1084. 10.1111/j.1365-2648.2012.06095.x [DOI] [PubMed] [Google Scholar]
- Harper J., Boivin J., O’Neill H. C., Brian K., Dhingra J., Dugdale G., Edwards G., Emmerson L., Grace B., Hadley A., Hamzic L., Heathcote J., Hepburn J., Hoggart L., Kisby F., Mann S., Norcross S., Regan L., Seenan S., Stephenson J., Walker H., Balen A. (2017). The need to improve fertility awareness. Reproductive Biomedicine & Society Online, 4, 18–20. 10.1016/j.rbms.2017.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashiloni-Dolev Y., Kaplan A., Shkedi-Rafid S. (2011). The fertility myth: Israeli students’ knowledge regarding age-related fertility decline and late pregnancies in an era of assisted reproduction technology. Human Reproduction, 26, 3045–3053. 10.1093/humrep/der304 [DOI] [PubMed] [Google Scholar]
- Horta F., Vollenhoven B., Healey M., Busija L., Catt S., Temple-Smith P. (2019). Male ageing is negatively associated with the chance of live birth in IVF/ICSI cycles for idiopathic infertility. Human Reproduction (Oxford, England), 34(12), 2523–2532. 10.1093/humrep/dez223 [DOI] [PubMed] [Google Scholar]
- Kruglova K., Gelgoot E. N., Chan P., Lo K., Rosberger Z., Bélanger E., Kazdan J., Robins S., Zelkowitz P. (2021). Risky business: Increasing fertility knowledge of men in the general public using the mobile health application Infotility XY. American Journal of Men’s Health, 15(5), 1–11. 10.1177/15579883211049027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudesia R., Chernyak E., McAvey B. (2017). Low fertility awareness in United States reproductive-aged women and medical trainees: Creation and validation of the Fertility & Infertility Treatment Knowledge Score (FIT-KS). Fertility & Sterility, 108(4), 711–717. 10.1016/j.fertnstert.2017.07.1158 [DOI] [PubMed] [Google Scholar]
- Latif T., Kold Jensen T., Mehlsen J., Holmboe S. A., Brinth L., Pors K., Skouby S. O., Jørgensen N., Lindahl-Jacobsen R. (2017). Semen quality as a predictor of subsequent morbidity: A Danish cohort study of 4,712 men with long-term follow-up. American Journal of Epidemiology, 186(8), 910–917. 10.1093/aje/kwx067 [DOI] [PubMed] [Google Scholar]
- Ledger W. L. (2009). Demographics of infertility. Reproductive Biomedical Online, 18(Suppl. 3), 11–14. 10.1016/s1472-6483(10)60442-7 [DOI] [PubMed] [Google Scholar]
- Levine H., Jørgensen N., Martino-Andrade A., Mendiola J., Weksler-Derri D., Mindlis I., Pinotti R., Swan S. H. (2017). Temporal trends in sperm count: A systematic review and meta-regression analysis. Human Reproduction Update, 23(6), 646–659. 10.1093/humupd/dmx022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundsberg L. S., Pal L., Gariepy A. M., Xu X., Chu M. C., Illuzzi J. L. (2014). Knowledge, attitudes, and practices regarding conception and fertility: A population-based survey among reproductive-age United States women. Fertility & Sterility, 101(3), 767–774. 10.1016/j.fertnstert.2013.12.006 [DOI] [PubMed] [Google Scholar]
- Maeda E., Nakamura F., Kobayashi Y., Boivin J., Sugimori H., Murata K., Saito H. (2016). Effects of fertility education on knowledge, desires and anxiety among the reproductive-aged population: Findings from a randomized controlled trial. Human Reproduction (Oxford, England), 31(9), 2051–2060. 10.1093/humrep/dew133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahalingiah S., Sun F., Cheng J. J., Chow E. T., Lunetta K. L., Murabito J. M. (2017). Cardiovascular risk factors among women with self-reported infertility. Fertility Research and Practice, 3, 1–7. 10.1186/s40738-017-0034-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miner M. (2012). Men’s health in primary care: An emerging paradigm of sexual function and cardiometabolic risk. The Urologic Clinics of North America, 39(1), 1–23. 10.1016/j.ucl.2011.09.003 [DOI] [PubMed] [Google Scholar]
- Monester J., Fisher J., Kirkman M., Rowe H., Holton S. (2019). “If I had known the fertility health facts sooner. . .” Knowledge gaps as a barrier to effective fertility management: Findings from the understanding fertility management in contemporary Australia survey. The European Journal of Contraception & Reproductive Health Care: The Official Journal of the European Society of Contraception, 24(4), 274–279. 10.1080/13625187.2019.1625326 [DOI] [PubMed] [Google Scholar]
- Morris G., Mavrelos D., Odia R., Viñals Gonzalez X., Cawood S., Yasmin E., Saab W., Serhal P., Seshadri S. (2021). Paternal age over 50 years decreases assisted reproductive technology (ART) success: A single UK center retrospective analysis. Acta Obstetricia et Gynecologica Scandinavica, 100(10), 1858–1867. 10.1111/aogs.14221 [DOI] [PubMed] [Google Scholar]
- Morse J. E., Moos M. K. (2018). Reproductive life planning: Raising the questions. Maternal Child Health Journal, 22, 439–444. 10.1007/s10995-018-2516-z [DOI] [PubMed] [Google Scholar]
- National Center for Education Statistics. (2020). The condition of college education–Immediate college enrollment rate. https://nces.ed.gov/programs/coe/indicator_cpa.asp
- Nouri K., Huber D., Walch K., Promberger R., Buerkle B., Ott J., Tempfer C. G. (2014). Fertility awareness among medical and non-medical students: A case-control study. Reproductive Biology and Endocrinology, 12, 95–102. 10.1186/1477-7827-12-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedro J., Brandão T., Schmidt L., Costa M. E., Martins M. V. (2018). What do people know about fertility? A systematic review on fertility awareness and its associated factors. Upsala Journal of Medical Sciences, 123(2), 71–81. 10.1080/03009734.2018.1480186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson B. D., Pirritano M., Tucker L., Lampic C. (2012). Fertility awareness and parenting attitudes among American male and female undergraduate university students. Human Reproduction, 27(5), 1375–1382. 10.1093/humrep/des011 [DOI] [PubMed] [Google Scholar]
- Prior E., Lew R., Hammarberg K., Johnson L. (2019). Fertility facts, figures and future plans: An online survey of university students. Human Fertility (Cambridge, England), 22(4), 283–290. 10.1080/14647273.2018.1482569 [DOI] [PubMed] [Google Scholar]
- Righarts A., Dickson N. P., Parkin L., Gillett W. R. (2017). Ovulation monitoring and fertility knowledge: Their relationship to fertility experience in a cross-sectional study. The Australian & New Zealand Journal of Obstetrics & Gynaecology, 57(4), 412–419. 10.1111/ajo.12606 [DOI] [PubMed] [Google Scholar]
- Robins S., Barr H. J., Idelson R., Lambert S., Zelkowitz P. (2016). Online health information regarding male infertility: An evaluation of readability, suitability, and quality. Interactive Journal of Medical Research, 5(4), e25. 10.2196/ijmr.6440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørensen N. O., Marcussen S., Backhausen M. G., Juhl M., Schmidt L., Tydén T., Hegaard H. K. (2016). Fertility awareness and attitudes towards parenthood among Danish university college students. Reproductive Health, 13(1), 146. 10.1186/s12978-016-0258-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senapati S. (2018). Infertility: A marker of future health risk in women? Fertility & Sterility, 110(5), 783–789. 10.1016/j.fertnstert.2018.08.058 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau Quick Facts (n.d.). Census Bureau Quick Facts. https://www.census.gov/quickfacts/fact/table/US/IPE120218