Abstract
Background:
Blood tests are usually obtained by venipuncture which is an insertion of a needle into a vein. Since blood collection is frequently ordered, it contributes to the increased workload on healthcare professionals. Thus, utilization of previously inserted peripheral intravenous lines for blood collection is proposed to decrease the work burden.
Objective:
The aim of the study was to make assessment of the awareness and practice of emergency medicine and intensive care unit staff regarding blood sampling via pre-existing peripheral line.
Methods:
This is a cross-sectional study used a web-based and self-administered questionnaire. It distributed among emergency department and intensive care unit staff between November 2021 and February 2022.
Results:
A total of 95 healthcare providers participated in the study. Most respondents were nurses (n=49, 51.5%) with 58.5% assigned to the intensive care unit. The overall mean awareness score was 1.74 out of 4 points with standard deviation of 1.29. Poor awareness was found among (n=65, 68.4%) and the remaining (n=30, 31.6%) had good awareness. Positive significant association has been observed between the level of awareness and practice (p=0.015). no significant difference was found between the emergency department and intensive care unit staff in terms of awareness level and practice.
Conclusion:
Findings from the current study showed variation in participants’ views, hence, nurses and other health care providers are left to use their personal preferences in deciding patient care. This highlights the need for establishing institutional policies regarding blood sampling via a pre-existing peripheral intravenous line.
Keywords: Pre-existing peripheral intravenous cannula, venipuncture, blood sampling, policy, awareness
1. BACKGROUND
Blood tests are usually required to facilitate the diagnosis of patient’s disease, aid the assessment of disease progression, and to monitor the intervention effectiveness (1). These blood tests are usually obtained by venipuncture which is an insertion of a needle into a vein (1) which is an invasive and painful technique that may negatively impact patients’ experience (2). For instance, it can expose patients to infections, hematomas, bruises, peripheral nerve injury, and its influence may extend to affect the psychological status of the patient by provoking their anxiety (2, 3). Besides its effect on patients, health care providers are also prone to mental and physical risks in the form of stress and accidental needle stick injury, respectively (2, 3).
Venipuncture is one of the procedures performed daily in the emergency department and other hospital units. Although in most cases it is done by nurses, other trained healthcare staff are eligible to perform it. Since blood collection is frequently ordered, it contributes to the increased workload on healthcare professionals. Thus, utilization of previously inserted peripheral intravenous lines for blood collection is proposed to decrease the work burden and enhance the provided care (1, 3). Furthermore, it is perceived as a satisfactory method in the reduction of blood collection rate via venipuncture (1).
Several studies concluded that blood sampling through direct venipuncture and peripheral intravenous cannula are equivalent when hematology, coagulation, and chemistry laboratory tests are analyzed (1-5). To ensure the accuracy of these laboratory test various protocols have been suggested by numerous researchers. For instance, Corbo et al. have pursued the cessation of the infused intravenous solution for at least 2 minutes and a waste of 5 mL of blood before specimen aspiration to ascertain sample validity (6). On the other hand, Ortells-Abuye et al. demonstrated the application of a similar protocol except that the halted time of intravenous solution and discarded amount of blood are distinct (2).
Despite the interchangeability of the methods of blood collection, there is no unified policy that have been established until the current era. It is worth noting that Davies et al. have identified differences in the participants’ attitude and practice regarding the use of pre-existing peripheral intravenous line for blood sampling and attributed the variations in the clinical practice to the inconsistent adopted policies (7).
While it is not a common practice obtaining blood specimens from a pre-existing peripheral intravenous line, this study aims to assess the awareness and practice of emergency medicine and intensive care unit professionals regarding blood sampling from pre-existing peripheral line. The secondary goal encompasses the comparison of awareness levels among emergency medicine and intensive care unit staff along with highlighting potential benefits and limitations of practicing blood collection via pre-existing peripheral intravenous line in a tertiary center in Saudi Arabia.
2. OBJECTIVE
The aim of the study was to make assessment of the awareness and practice of emergency medicine and intensive care unit staff regarding blood sampling via pre-existing peripheral line.
3. MATERIAL AND METHODS
Study design and sample size
A descriptive cross-sectional study was conducted among emergency medicine (ED) and intensive care unit (ICU) departments’ staff to determine the awareness and practice of blood sampling through pre-existing intravenous peripheral line. A validated web-based self-administered survey distributed by the researchers comprised of twenty-three questions in the form of yes or no, multiple choice and multiple selection questions that have been divided into four sections. The first section covered the sociodemographic data followed by the work nature and work experience then the awareness and practice of pre-existing peripheral intravenous line as an alternative to venipuncture for blood sampling and ultimately venipuncture practice and its complication. The data was collected from November 2021 till March 2022.
We included all emergency medicine department as well as intensive care unit staff working in a single busy tertiary hospital including consultants, specialists, residents, and nurses where an annual visit reached 250,000 visits. we excluded nursing and medical interns and healthcare staff working outside emergency medicine and intensive care unit department. The minimum required sample size was calculated to be 80 participants, assuming a prevalence of 60% in the emergency department staff and 30% in the intensive care unit staff -since no literature data is available and Cronbach alpha value of 5% and power to be 80%. A written informed consent was obtained from each participant before the administration of the questionnaire. Anonymity and confidentiality of the responses of collected data were maintained.
Statistical analysis
All statistical analysis were performed using the Statistical Packages for Software Sciences (SPSS) version 26 (IBM Corp., Armonk, NY, USA). The overall level of awareness of blood sampling through pre-existing peripheral line has been assessed using a 4-item questionnaire. The total score was obtained by adding the 4 items. A score range from 0 to 4 has been generated which indicates that the higher the score, the higher the level of awareness about blood sampling through pre-existing peripheral line. The overall score was divided into two groups to determine the level of awareness. Participants were considered to have poor awareness if the score was ranging from 0 to 2 points. However, participants were considered to have good awareness if the score was ranging from 3 to 4 points. The general practice of the participants was obtained by using yes or no question which was used as an absolute indicator of the practice. Participants were classified to have a negative practice if they answered “no” to the question while they were classified to have a positive practice if they answered “yes” to the question.
4. Results
A total of 95 healthcare providers (HCPs) responded to the survey (ED: 54; ICU: 41). The socio-demographic characteristics are presented in Table 1. Of these, more male HCPs were from ICU department (46.3%), however, more females were from ED (55.6%). Most respondents were nurses with an approximate of 60% assigned to the ICU. Less than two-thirds (64%) of the nursing technicians were working in the ED whereas (70.8%) of nursing specialists were working in the ICU. Most respondents reported that they had 5 years or less of working experience. Regarding the working hours, (85.4%) of ICU and (68.5%) of ED staff were working up to 48 hours per week. In the ICU, the greatest workload was reported to be in the morning shift (70.7%), however, the evening shift has the greatest workload in the ED department (94.4%). In the assessment of awareness regarding the use of pre-existing peripheral intravenous line as an alternative to venipuncture to collect blood samples, approximately half of the respondents were aware about the existence of policies when using pre-existing peripheral intravenous lines to collect a blood sample. (44.2%) of the respondents had the knowledge regarding the amount of blood to be discarded before collecting blood sample. Concerning the duration of halting the infusion prior to blood extraction, only (31.6%) of the respondents were aware about it. In addition, (68.4%) of the respondents reported the need for further educational materials regarding the correct technique of blood sampling through pre-existing peripheral intravenous lines. In comparison between ED and ICU, the results showed that there were no significant differences found between the awareness statements except for the amount of discarded blood statement. The overall mean awareness score was 1.74 (SD 1.29) out of 4 points with poor awareness was found among (68.4%) and the remaining (31.6%) had good awareness (Table 2). In Figure 1, a positive significant association has been observed between the level of awareness and practice (p=0.015). The discarded volume of blood before collecting the sample by almost half of respondents was 5 mL (n=44, 46.3%) without significant difference between ED and ICU staff (p=0.248) as shown in Table 3. Moreover, halting the intravenous infusion for a duration of 2 minutes prior to blood sampling was stated by nearly one-third of respondents (n=30, 31.6%). Similarly, there was no statistically significant difference between ED and ICU staff (p=0.855).
Table 1. Socio-demographic characteristics of participants according to hospital department (n=95).
| Study variables | ED N (%)(n=54) | ICU N (%)(n=41) |
|---|---|---|
| Gender | ||
| Male | 24 (44.4%) | 19 (46.3%) |
| Female | 30 (55.6%) | 22 (53.7%) |
| Nationality | ||
| Saudi | 30 (55.6%) | 18 (43.9%) |
| Non-Saudi | 24 (44.4%) | 23 (56.1%) |
| Job title | ||
| Nurse | 25 (46.3%) | 24 (58.5%) |
| Resident | 15 (27.8%) | 07 (17.1%) |
| Specialist | 08 (14.8%) | 05 (12.2%) |
| Consultant | 06 (11.1%) | 05 (12.2%) |
| Professional level of the nurses(n=49) | ||
| Nursing technician | 16 (64.0%) | 06 (25.0%) |
| Nursing specialist | 09 (36.0%) | 17 (70.8%) |
| Senior specialist | 0 | 01 (04.2%) |
| Years of experience in KFUH | ||
| ≤5 years | 29 (53.7%) | 25 (61.0%) |
| 6 – 10 years | 18 (33.3%) | 11 (26.8%) |
| >10 years | 07 (13.0%) | 05 (12.2%) |
| Is blood collection one of your job duties? | ||
| No | 29 (53.7%) | 16 (39.0%) |
| Yes | 25 (46.3%) | 25 (61.0%) |
| Current average working hours per week? | ||
| 24 – 32 hours | 17 (31.5%) | 04 (09.8%) |
| 40 – 48 hours | 37 (68.5%) | 35 (85.4%) |
| ≥56 hours | 0 | 02 (04.9%) |
| Which shift has the greatest workload? | ||
| Morning | 02 (03.7%) | 29 (70.7%) |
| Evening | 51 (94.4%) | 06 (14.6%) |
| Night | 01 (01.9%) | 06 (14.6%) |
Table 2. Assessment of awareness regarding the use of pre-existing peripheral intravenous line as an alternative to venipuncture to collect blood samples. † Not included in the assessment of awareness score. * Indicates positive response. § P-value has been calculated using Fischer Exact test.
| Statement | Overall N (%)(n=95) | ED N (%)(n=54) | ICU N (%)(n=41) | P-value§ |
|---|---|---|---|---|
| Are you aware about any policy to be followed when using pre-existing peripheral intravenous line to collect blood sample? | ||||
| No | 46 (48.4%) | 28 (51.9%) | 18 (43.9%) | 0.535 |
| Yes * | 49 (51.6%) | 26 (48.1%) | 23 (56.1%) | |
| Have you ever been educated or introduced to the institution protocol regarding the correct technique of blood sampling through pre-existing peripheral intravenous line? | ||||
| No | 53 (55.8%) | 30 (55.6%) | 23 (56.1%) | 1.000 |
| Yes * | 42 (44.2%) | 24 (44.4%) | 18 (43.9%) | |
| Do you know how much milliliter (mL) of blood must be discarded before collecting the blood sample from pre-existing peripheral intravenous line? | ||||
| No | 51 (53.7%) | 34 (63.0%) | 17 (41.5%) | 0.041 ** |
| Yes * | 44 (46.3%) | 20 (37.0%) | 24 (58.5%) | |
| Do you know for how long intravenous infusion must be stopped before collecting the blood sample from pre-existing peripheral intravenous line? | ||||
| No | 65 (68.4%) | 38 (70.4%) | 27 (65.9%) | 0.662 |
| Yes * | 30 (31.6%) | 16 (29.6%) | 14 (34.1%) | |
| Do you need further educational materials regarding the correct technique of blood sampling through pre-existing peripheral intravenous lines? † | ||||
| No | 30 (31.6%) | 14 (25.9%) | 16 (39.0%) | 0.189 |
| Yes | 65 (68.4%) | 40 (74.1%) | 25 (61.0%) | |
| Total awareness score (mean ± SD) | 1.74 ± 1.29 | – | – | – |
| Level of awareness | ||||
| Poor | 65 (68.4%) | – | – | – |
| Good | 30 (31.6%) | – | – | – |
Figure 1. Association between the level of awareness and practice.
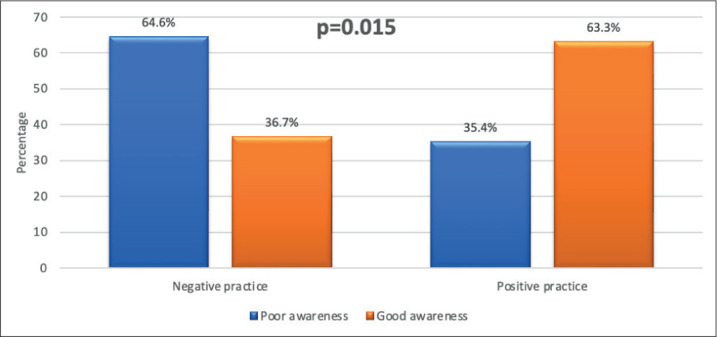
Table 3. Assessment of the participants’ background regarding blood sampling technique through pre-existing peripheral intravenous line. § P-value has been calculated using Fischer Exact test. ** Significant at p<0.05 level.
| Statement | Overall N (%)(n=95) | ED N (%)(n=54) | ICU N (%)(n=41) | P-value§ |
|---|---|---|---|---|
| How much milliliters (mL) of blood must be discarded before collecting the blood sample from pre-existing peripheral intravenous line? | ||||
| 2 mL | 24 (25.3%) | 14 (25.9%) | 10 (24.4%) | 0.248 |
| 3 mL | 06 (06.3%) | 05 (09.3%) | 01 (02.4%) | |
| 4 mL | 04 (04.2%) | 03 (05.6%) | 01 (02.4%) | |
| 5 mL | 44 (46.3%) | 20 (37.0%) | 24 (58.5%) | |
| >5 mL | 07 (07.4%) | 06 (11.1%) | 01 (02.4%) | |
| Unsure | 10 (10.5%) | 06 (11.1%) | 04 (09.8%) | |
| For how long intravenous infusion must be stopped before collecting the blood sample from pre-existing peripheral intravenous line? | ||||
| 15 seconds | 09 (09.5%) | 05 (09.3%) | 04 (09.8%) | 0.855 |
| 30 seconds | 13 (13.7%) | 08 (14.8%) | 05 (12.2%) | |
| 1 minutes | 22 (23.2%) | 14 (25.9%) | 08 (19.5%) | |
| 2 minutes | 30 (31.6%) | 16 (29.6%) | 14 (34.1%) | |
| >2 minutes | 11 (11.6%) | 07 (13.0%) | 04 (09.8%) | |
| Unsure | 10 (10.5%) | 04 (07.4%) | 06 (14.6%) | |
In Figure 2, several non-recommended blood parameters were reported by most ED staff when using a pre-existing peripheral intravenous line. The most frequently chosen parameters were creatinine (78.6%), followed by cardiac enzymes (77.8%), calcium, and glucose (73.9%).
Figure 2: Comparison of the knowledge between ED and ICU staff regarding blood parameters that are not advised to be measured when using a pre-existing peripheral intravenous line.

Forty-four (44.2%) had experienced blood sample collection through a pre-existing peripheral IV line as an alternative to direct venipuncture as shown in (Table 4). Among respondents, “time-saving method” was the most frequently noticed benefit of using pre-existing peripheral IV line (66.3%). On the other hand, the most common concern of respondents which affects the preference of using this method was “sample dilution” (58.9%). When comparing ED and ICU staff, there was no significant difference regarding the practice (all p>0.05).
Table 4. Assessment of the practice regarding the use of pre-existing peripheral intravenous line as an alternative to venipuncture to collect blood samples § P-value has been calculated using Fischer Exact test.
| Statement | Overall N (%)(n=95) | ED N (%)(n=54) | ICU N (%)(n=41) | P-value§ |
|---|---|---|---|---|
| Do you experience blood sample collection through a pre-existing peripheral intravenous line as an alternative to direct venipuncture? ‡ | ||||
| No | 53 (55.8%) | 32 (59.3%) | 21 (51.2%) | 0.532 |
| Yes | 42 (44.2%) | 22 (40.7%) | 20 (48.8%) | |
| If you prefer using pre-existing peripheral intravenous line to collect blood samples, what is/are the possible benefit/s you have noticed? † | ||||
| Time saving method | 63 (66.3%) | 36 (66.7%) | 27 (65.9%) | 1.000 |
| Safe method | 34 (35.8%) | 15 (27.8%) | 19 (46.3%) | 0.084 |
| Anxiety reduction | 36 (37.9%) | 19 (35.2%) | 17 (41.5%) | 0.670 |
| No special training is required | 13 (13.7%) | 08 (14.8%) | 05 (12.2%) | 0.772 |
| No idea | 03 (03.2%) | 02 (03.7%) | 01 (02.4%) | 1.000 |
| None of these | 06 (06.3%) | 05 (09.3%) | 01 (02.4%) | 0.231 |
| If you don’t prefer using pre-existing peripheral intravenous line to collect blood samples, what are the concerns you try to avoid? † | ||||
| Sample dilution | 56 (58.9%) | 30 (55.6%) | 26 (63.4%) | 0.529 |
| Sample hemolysis | 45 (47.4%) | 24 (44.4%) | 21 (51.2%) | 0.540 |
| Sample contamination by colonization | 32 (33.7%) | 20 (37.0%) | 12 (29.3%) | 0.513 |
| Sample not adequate | 17 (17.9%) | 10 (18.5%) | 07 (17.1%) | 1.000 |
| Catheter occlusion by a thrombus | 26 (27.4%) | 14 (25.9%) | 12 (29.3%) | 0.817 |
| No idea | 02 (02.1%) | 01 (01.9%) | 01 (02.4%) | 1.000 |
| None of these | 03 (03.2%) | 03 (05.6%) | 0 | 0.256 |
In Table 5, (29.5%) of the respondents stated that they perform venipuncture for blood samples less than 10 times per day. The prevalence of respondents who experienced a needle stick injury while performing venipuncture was (32.6%). When measuring the association between the level of awareness and practice according to the socio-demographic characteristics of participants, it was found that nurses had better awareness (p<0.001) and positive practice (p=0.008) toward blood sampling technique through pre-existing peripheral IV line. Additionally, participants with duty of blood sampling had better awareness (p<0.001) and positive practice (p=0.002). Working for 40 – 48 hours per week showed significantly better awareness (p=0.002) but negative practice (p=0.104). Other variables such as gender, hospital department, professional level of nurses, years of experience, shift with the greatest workload and complication of venipuncture did not significantly influence both the level of awareness and practice (p>0.05) (Table 6).
Table 5. Assessment of Venipuncture practice and its complication according to hospital department. † Variable with multiple response answers.
| Statement | Overall N (%)(n=95) | ED N (%)(n=54) | ICU N (%)(n=41) |
|---|---|---|---|
| How frequently you perform venipuncture for blood sampling per day? | |||
| Less than 10 times per day | 28 (29.5%) | 04 (07.4%) | 24 (58.5%) |
| 10-20 times per day | 11 (11.6%) | 08 (14.8%) | 03 (07.3%) |
| More than 20 times per day | 16 (16.8%) | 16 (29.6%) | 0 |
| I don’t perform it | 40 (42.1%) | 26 (48.1%) | 14 (34.1%) |
| Have you ever experienced a needle stick injury while performing venipuncture? | |||
| No | 64 (67.4%) | 40 (74.1%) | 24 (58.5%) |
| Yes | 31 (32.6%) | 14 (25.9%) | 17 (41.5%) |
Table 6. Association between the level of awareness and practice regarding the socio-demographic characteristics of participants (n=95). P-value has been calculated using Fischer Exact test. ** Significant at p<0.05 level.
| Factor | Level of awareness | Level of practice | ||
|---|---|---|---|---|
| Poor N (%)(n=65) | Good N (%)(n=30) | Negative N (%)(n=53) | Positive N (%)(n=42) | |
| Gender | ||||
| Male | 30 (46.2%) | 13 (43.3%) | 27 (50.9%) | 16 (38.1%) |
| Female | 35 (53.8%) | 17 (56.7%) | 26 (49.1%) | 26 (61.9%) |
| P-value | 0.828 | 0.222 | ||
| Hospital department | ||||
| ED | 37 (56.9%) | 17 (56.7%) | 32 (60.4%) | 22 (52.4%) |
| ICU | 28 (43.1%) | 13 (43.3%) | 21 (39.6%) | 20 (47.6%) |
| P-value | 1.000 | 0.532 | ||
| Nationality | ||||
| Saudi | 41 (63.1%) | 07 (23.3%) | 32 (60.4%) | 16 (38.1%) |
| Non-Saudi | 24 (36.9%) | 23 (76.7%) | 21 (39.6%) | 26 (61.9%) |
| P-value | <0.001 ** | 0.040 ** | ||
| Job title | ||||
| Nurse | 24 (36.9%) | 25 (83.3%) | 20 (37.7%) | 29 (69.0%) |
| Resident | 21 (32.3%) | 01 (03.3%) | 14 (26.4%) | 08 (19.0%) |
| Specialist | 10 (15.4%) | 03 (10.0%) | 09 (17.0%) | 04 (09.5%) |
| Consultant | 10 (15.4%) | 01 (03.3%) | 10 (18.9%) | 01 (02.4%) |
| P-value | <0.001 ** | 0.008 ** | ||
| Professional level of nurse (n=49) | ||||
| Nursing technician | 08 (33.3%) | 14 (56.0%) | 09 (45.0%) | 13 (44.8%) |
| Nursing/Senior specialist | 16 (66.7%) | 11 (44.0%) | 11 (55.0%) | 16 (55.2%) |
| P-value | 0.154 | 1.000 | ||
| Years of experience | ||||
| ≤5 years | 39 (60.0%) | 15 (50.0%) | 29 (54.7%) | 25 (59.5%) |
| 6 – 10 years | 17 (26.2%) | 12 (40.0%) | 17 (32.1%) | 12 (28.6%) |
| >10 years | 09 (13.8%) | 03 (10.0%) | 07 (13.2%) | 05 (11.9%) |
| P-value | 0.418 | 0.956 | ||
| Is blood collection one of your job duties? | ||||
| No | 40 (61.5%) | 05 (16.7%) | 33 (62.3%) | 12 (28.6%) |
| Yes | 25 (38.5%) | 25 (83.3%) | 20 (37.7%) | 30 (71.4%) |
| P-value | <0.001 ** | 0.002 ** | ||
| Current average working hours per week? | ||||
| 24 – 32 hours | 20 (30.8%) | 01 (03.3%) | 15 (28.3%) | 06 (14.3%) |
| 40 – 48 hours | 43 (66.2%) | 29 (96.7%) | 36 (67.9%) | 36 (85.7%) |
| ≥56 hours | 02 (03.1%) | 0 | 02 (03.8%) | 0 |
| P-value | 0.002 ** | 0.104 | ||
| Which shift has the greatest workload? | ||||
| Morning | 22 (33.8%) | 09 (30.0%) | 15 (28.3%) | 16 (38.1%) |
| Evening | 39 (60.0%) | 09 (30.0%) | 36 (67.9%) | 21 (50.0%) |
| Night | 04 (06.2%) | 03 (10.0%) | 02 (03.8%) | 05 (11.9%) |
| P-value | 0.829 | 0.132 | ||
5. Discussion
Blood sampling is a common measure that enables the assessment of patients’ condition (2). Therefore, utilization of newly advancement aids such as ultrasound guidance have been established to minimize the delay occurring due to difficulty in obtaining IV access (9). However, the availability of less sophisticated and feasible approach in particular blood sampling through PIVC would assist more in the reduction of the time lag of blood collection process. Based on this study’s findings, participants with poor awareness scored 1.74 out of 4 with a standard deviation of 1.29, which encompasses (68.4%) of the total participants, whereas (31.6%) had good awareness. Besides, a proportion of respondents (48.4%) are not aware of such a policy (Table 2). In contrast to earlier findings, Davies et al. discovered that only (28.4%) of respondents were unsure of the hospital policy (7). In addition, this study examined the association between the level of awareness and practice. The results showed that positive practice was seen among those with a higher level of awareness. An unanticipated finding was that some participants, despite their lack of awareness, practiced PIVC (Figure 1).
Another aspect to note was that good awareness of the positive practice was significantly found among nurses (Table 6). This finding can be attributed to their day-by-day duty of blood sampling. Furthermore, there is no significant difference in awareness level between ER and ICU staff, except for a statistically significant difference regarding the amount of discarded blood statements (p=0.041) (Table 2). Consequently, the respondents stated that they need additional educational materials about the proper protocol (Table 2). This result was in concordance with previously published research in which (25.4%) of respondents pinpointed their need for additional education (10).
Given that the validity of a subsequent blood sample was affected by the discarded volume of blood obtained via PIVC, the responses received from the survey indicated that almost half of respondents (46.3%) would prefer to discard 5mL before blood sampling. Similarly, Davis et al. reported that (47.9%) of the surveyed Australian nurses would discard 5 mL before blood sampling (7).
Numerous researchers proposed pausing fluid infusion for 2 or 3 minutes instead of 1 minute to improve blood specimen accuracy and prevent dilution. (16-18). Therefore, a study by Jeong et al. suggested that the observed differences in potassium values between PIVC and venipuncture in Yazdankhahfard et al. study could be attributed to the infusion being stopped for only 1 minute before sampling. (1) In this study, 31.6 % of participants chose to pause the infusion for 2 minutes before sampling, while 23.2 % chose to pause it for 1 minute.
Contrary to expectations, potassium values in Ortells-Abuye et al. were equivalent between the two methods with moderate concordance (3). Adding to that, Dr Fawcett’s also comments and confirms that, when laboratory samples being collected after flushing with normal saline and 5% glucose, no dramatic change will happen in potassium level (19).
In this study, advantages of using PIVC for blood sampling were surveyed. Around two-thirds (66.3%) of participants noticed that blood sampling through PIVC is a technique that plays a role in saving time. Managing the smoothness of patients’ flow contributes to the avoidance of delay of provided care as well as the facilitation of medically related decisions (22). Similar to other research, the key rationale that consolidated nursing staff preference to collect blood samples through PIVC was efficiency and workflow maintenance (10).
Other advantage was reported by approximately (38%) of respondents which is the reduction of anxiety and discomfort for patients. This result is compared with a finding of previous research in which patients’ physical and psychological comfort influenced nursing staff preference (10). Utilization of PIVC for blood sampling would enhance patients’ satisfaction as the successive attempts of blood collection by the standard venipuncture is significantly associated with higher pain perception scores (23). In addition, it permits venous access site preservation, particularly for those with poor and limited access (24). Not to mention its suitability for certain age groups, such as paediatric patients (25).
Boden et al. found that the most common occupational injuries in the hospital setting were back pain and needle stick injury on days away and no days away, respectively (26). 32.6% of this study participants have been exposed to needle stick injury which emphasizes previous research findings. Blood collection carries the risk of needle stick injury by healthcare providers, exposing them to blood-borne organisms (27). Almost (36%) of respondents of this study have noticed the safety that is offered by the use of PIVC for blood sampling. Hence, serial blood testing by a needleless method would be a valuable precautionary measure that would diminish possible hazards of blood exposure (6). Since PIVC is usually used for saline and medication infusion, nurses and other healthcare providers are concerned about sample dilution (7). This study revealed that more than half of the respondents don’t prefer using PIVC to collect blood due to the risk of sample dilution (58.9%). Baker et al. established that discarding at least an amount more than the interior volume of the PIVC with the attached extension tube is sufficient to prevent sample dilution (14).
Fear of sample hemolysis is one of the most common causes that limit the use of PIVC to collect blood samples. Nearly 50% of participants would not support the practice of PIVC to collect blood due to the possibility of sample hemolysis. Lowe et al. found that hemolysis rates were significantly higher in samples drawn through intravenous catheter (28). In contrast, a recent study by Jacob et al. concluded that sample hemolysis was not related to the collection method (29). Additionally, newly invented PIVOTM (Velano Vascular, Inc., San Francisco, CA) technology was associated with non-hemolyzed samples. Moreover, the PIVO device reduces the need for blood waste prior to collection and decrease the waiting time to 30 seconds (15). Due to the worrisome of sample contamination, 33.7% of respondents would not prefer drawing blood from PIVC. Contamination and colonization of the catheter hub could be caused by repeated hub handling (7). Therefore, implementing infection control measures such as wearing gloves, performing adequate hand hygiene, and using 70% alcohol wipes could reduce the rates of specimen contamination (30). The concerns match those observed in a previous study (10). Furthermore, catheter occlusion by a thrombus was stated by (27.4%) of respondents as a concern that restrains the blood collection via PIVC. To prevent thrombus-related catheter occlusion, Xu et al. recommended using a normal saline flush after blood sampling to maintain the catheter patency (31). While Guiffant et al. suggested push-pause methods before and after blood collection using normal saline (32).
Despite the growing use of PIVC for blood sampling, the ambiguity of guidelines on such practice remains a major cause for inconsistency across different institutions and even territories within the same country (33-35). Jacob et al. demonstrated that policies differ in the purpose of cannula insertion, preferred setting, and infusion flushing instructions, indicating that they are not unanimous on the pre-analytic technique of blood collection. Moreover, the size of veins, the use of vacutainer or syringe, and the dwell time are all controversial considerations among different policies (35).
Overall, patient care standards are frequently mandated by regulatory agencies. These standards are approached by creating global or institutional policies (28). Lacking standardized policies and specific protocol regarding blood sampling from PIVC resulted in incongruous practice. Unfortunately, the studied hospital did not adopt a particular policy which resulted in a variation in the participants’ responses to the protocol. This stems from the lack of conclusive evidence of blood sampling through PIVC which is a fertile territory for further research (7, 35).
6. Conclusion
The present research was designed to investigate the level of awareness and practice of blood sampling through PIVC as an alternative to venipuncture among ED and ICU staff, who are able to employ this method more frequently in relation to other healthcare providers. One of the most remarkable results to emerge from this study is the positive linear association between the level of awareness and practice of blood sampling through PIVC. Regrettably, the study participants showed poor awareness with conflicting opinions and points of view regarding the use of such a method. These findings contribute to a growing body of literature on the need for integrated health policies that are built on solid and reliable evidence to minimize discrepancies across institutions.
Application
The findings of this study would positively influence several aspects such as satisfaction of patients, occupational risk exposure by healthcare providers, and workflow in acute care settings. By highlighting deficiencies in the literature regarding blood sampling via PIVC, stakeholders would be enabled to establish appropriate guidelines.
Strengths and limitations
To the best of our knowledge, this is the first study to assess the awareness and practice of PIVC as an alternative to venipuncture among ED and ICU staff in Saudi Arabia. Indeed, despite being viewed as a strength, the lack of literature on this topic has restricted the ability to make direct comparisons with other research findings. Few publications have looked at the real-world use of PIVC for blood sampling among healthcare providers. However, despite the small number of participants, the received responses provided an opportunity to view the knowledge and clinical practice among hospital acute care staff. Furthermore, the current findings emphasize the necessity for the hospital departments and other institutions on a national and worldwide scale to be expanded in future research.
Recommendations
This research has thrown up many questions in need for further investigations regarding the accuracy of blood results obtained via PIVC, and the existence of differences in dilution rate, hemolysis rate, contamination rate, and occlusion rate when PIVC is used as an alternative to venipuncture.
Authors contribution:
The author was involved in all steps of the preparation this article, including final proofreading.
Conflict of interest:
None declared.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Jeong Y, Park H, Jung MJ, Kim MS, Byun S, Choi Y. Comparisons of laboratory results between two blood samplings: Venipuncture versus peripheral venous catheter - a systematic review with meta- analysis. J Clin Nurs. 2019;28(19-20):3416–3429. doi: 10.1111/jocn.14918. [DOI] [PubMed] [Google Scholar]
- 2.Hambleton VL, Gómez IA, Andreu FA. Venipuncture versus peripheral catheter: Do infusions alter laboratory results? J Emerg Nurs. 2014;40(1):20–26. doi: 10.1016/j.jen.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 3.Ortells-Abuye N, Busquets-Puigdevall T, Díaz-Bergara M, Paguina-Marcos M, Saánchez-Peárez I. A cross-sectional study to compare two blood collection methods: direct venous puncture and peripheral venous catheter. BMJ Open. 2014;4(2) doi: 10.1136/bmjopen-2013-004250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seemann S, Reinhardt A. Blood sample collection from a peripheral catheter system compared with phlebotomy. J Intraven Nurs. 2000 Sep-Oct;23(5):290–297. [PubMed] [Google Scholar]
- 5.Lesser FD, Lanham DA, Davis D. Blood sampled from existing peripheral IV cannulae yields results equivalent to venepuncture: A systematic review. JRSM Open. 2020;11(5):205427041989481. doi: 10.1177/2054270419894817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corbo J, Fu L, Silver M, Atallah H, Bijur P. Comparison of laboratory values obtained by phlebotomy versus Saline Lock Devices. Acad Emerg Med. 2007;14(1):23–27. doi: 10.1197/j.aem.2006.06.053. [DOI] [PubMed] [Google Scholar]
- 7.Davies H, Coventry LL, Jacob A, Stoneman L, Jacob E. Blood sampling through peripheral intravenous cannulas: A look at current practice in Australia. Collegian. 2020;27(2):219–225. [Google Scholar]
- 8.Chow S, Wang H, Shao J. Sample Size Calculations in Clinical Research. 2nd ed. New York: CRC Press; 2007. Section 3.1, Test for Equality. p. 3-4. [Google Scholar]
- 9.Davis E, Feinsmith S, Amick A, Sell J, McDonald V, Trinquero P, et al. Difficult intravenous access in the emergency department: Performance and impact of ultrasound-guided IV insertion performed by nurses. Am. J. Emerg. Med. 2021;46:539–544. doi: 10.1016/j.ajem.2020.11.013. [DOI] [PubMed] [Google Scholar]
- 10.Jacob E, Jacob A, Davies H, Stoneman L, Coventry L. Peripheral intravenous cannulas for blood drawing: Nurses’ views through content analysis. Collegian. 2021;28(4):408–414. [Google Scholar]
- 11.Alexandrou E, Ray-Barruel G, Carr PJ, Frost S, Inwood S, Higgins N, et al. International prevalence of the use of peripheral intravenous catheters. J Hosp Med. 2015;10(8):530–533. doi: 10.1002/jhm.2389. [DOI] [PubMed] [Google Scholar]
- 12.Giavarina D, Lippi G. Blood venous sample collection: Recommendations overview and a checklist to improve quality. Clin Chem. 2017;50(10-11):568–573. doi: 10.1016/j.clinbiochem.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 13.Taghizadeganzadeh M, Yazdankhahfard M, Farzaneh M, Mirzaei K. Blood samples of peripheral venous catheter or the usual way: Do infusion fluid alters the biochemical test results? GlobJ Health Sci. 2015;8(7):93. doi: 10.5539/gjhs.v8n7p93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baker RB, Summer SS, Lawrence M, Shova A, McGraw CA, Khoury J. Determining optimal waste volume from an intravenous catheter. J Infus Nurs. 2013;36(2):92–96. doi: 10.1097/NAN.0b013e318282a4c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adams S, Toroni B, Lele M. Effect of the PIVO device on the procedure of phlebotomy from Peripheral IV catheters. Nurs Res Pract. 2018;2018:1–6. doi: 10.1155/2018/7380527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herr RD, Bossart PJ, Blaylock RC, Kroger K, Ash O. Intravenous catheter aspiration for obtaining basic analytes during intravenous infusion. Ann Emerg Med. 1990;19(7):789–792. doi: 10.1016/s0196-0644(05)81705-6. [DOI] [PubMed] [Google Scholar]
- 17.Read DC, Viera H, Arkin C. Effect of drawing blood specimens proximal to an in-place but discontinued intravenous solution: Can blood be drawn above the site of a shut-off IV? AmJ Clin Pathol. 1988;90(6):702–706. doi: 10.1093/ajcp/90.6.702. [DOI] [PubMed] [Google Scholar]
- 18.Watson KR, O’kell RT, Joyce JT. Data regarding blood drawing sites in patients receiving intravenous fluids. AmJ Clin Pathol. 1983;79(1):119–121. doi: 10.1093/ajcp/79.1.119. [DOI] [PubMed] [Google Scholar]
- 19.Fawcett W. Contamination of arterial blood samples by flushing solution. Anaesthesia. 2013;69(1):89–89. doi: 10.1111/anae.12553. [DOI] [PubMed] [Google Scholar]
- 20.McKenna P, Heslin S, Viccellio P, Mallon W, Hernandez C, Morley E. Emergency department and hospital crowding: causes, consequences, and cures. Exp. Emerg. Med. 2019;6(3):189–195. doi: 10.15441/ceem.18.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stead L, Jain A, Decker W. Emergency department over-crowding: a global perspective. IntJ Emerg Med. 2009;2:133–134. doi: 10.1007/s12245-009-0131-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bernstein S, Aronsky D, Duseja R, Epstein S, Handel, et al. The Effect of Emergency Department Crowding on Clinically Oriented Outcomes. J. Acad. Emerg. Med. 2009;16(1):1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 23.Fields JM, Piela N, Ku B. Association between Multiple IV attempts and Perceived Pain levels in the Emergency Department. J Vasc Access. 2014;15(6):514–518. doi: 10.5301/jva.5000282. [DOI] [PubMed] [Google Scholar]
- 24.Zlotowski S, Kupas D, Wood GC. Comparison of laboratory values obtained by means of routine venipuncture versus peripheral intravenous catheter after a normal saline solution bolus. Ann Emerg Med. 2001;38(5):497–504. doi: 10.1067/mem.2001.118015. [DOI] [PubMed] [Google Scholar]
- 25.Berger-Achituv S, Budde-Schwartzman B, Ellis M, Shenkman Z, Erez I. Blood Sampling Through Peripheral Venous Catheters Is Reliable for Selected Basic Analytes in Children. Pediatrics. 2010;126(1):179–186. doi: 10.1542/peds.2009-2920. [DOI] [PubMed] [Google Scholar]
- 26.Boden L, Sembajwe G, Tveito T, Hashimoto D, Hopcia K, Kenwood C, et al. Occupational Injuries Among Nurses and Aides in a Hospital Setting. Am. J. Ind. Med. 2012;55(2):117–126. doi: 10.1002/ajim.21018. [DOI] [PubMed] [Google Scholar]
- 27.Beltrami E, Williams I, Shapiro C, Chamberland M. Risk and Management of Blood-Borne Infections in Health Care Workers. Clin. Microbiol. Rev. 2000;13(3):385–407. doi: 10.1128/cmr.13.3.385-407.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lowe G, Stike R, Pollack M, Bosley J, O’Brien P, Hake A, et al. Nursing Blood Specimen Collection Techniques and Hemolysis Rates in an Emergency Department: Analysis of Venipuncture Versus Intravenous Catheter Collection Techniques. J Emerg Nurs. 2008;34(1):26–32. doi: 10.1016/j.jen.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 29.Jacob E, Jacob A, Davies H, Jenkins M, Husain M, Coventry L. The impact of blood sampling technique, including the use of peripheral intravenous cannula, on haemolysis rates: A cohort study. J Clin Nurs. 2021;00:1–11. doi: 10.1111/jocn.15744. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Guidelines for the Prevention of Intravascular Catheter-Related Infections. Atlanta (GA): Centers for Disease Control and Prevention; 2011. p. 80. p. [Google Scholar]
- 31.Xu L, Hu Y, Huang X, Fu J, Zhang J. Heparinized saline versus normal saline for maintaining peripheral venous catheter patency in China: An open-label, randomized controlled study. J Int Med Res. 2017;45(2):471–480. doi: 10.1177/0300060516685203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guiffant G, Durussel J, Merckx J, Flaud P, Vigier J, Mousset P. Flushing of Intravascular Access Devices (IVADs)–Efficacy of Pulsed and Continuous Infusions. J Vasc Access. 2012;13(1):75–78. doi: 10.5301/JVA.2011.8487. [DOI] [PubMed] [Google Scholar]
- 33.Carr P, Rippey J, Budgeon C, Cooke M, Higgins N, Rickard C. Insertion of Peripheral Intravenous Cannulae in the Emergency Department: Factors Associated with First-time Insertion Success. J Vasc Access. 2015;17(2):182–190. doi: 10.5301/jva.5000487. [DOI] [PubMed] [Google Scholar]
- 34.Coventry L, Jacob A, Davies H, Stoneman L, Keogh S, Jacob E. Drawing blood from peripheral intravenous cannula compared with venepuncture: A systematic review and meta-analysis. J Adv. Nurs. 2019;75(11):2313–39. doi: 10.1111/jan.14078. [DOI] [PubMed] [Google Scholar]
- 35.Jacob A, Coventry L, Davies H, Jacob E. Are current clinical guidelines on the use of Peripheral Intravenous Cannula for blood draws supported by evidence? An organizational case study. Nurs. Open. 2020;7(6):1746–1754. doi: 10.1002/nop2.559. [DOI] [PMC free article] [PubMed] [Google Scholar]


