Abstract
Objectives
To explore the main factors affecting the knowledge, attitude and practice about influenza and influenza vaccine as well as the intention to receive influenza vaccination among the same group of medical students before (2019) and after (2021) the COVID-19 outbreak.
Design
A population-based prospective cohort study.
Setting
A longitudinal cohort study of a selected medical school in Chongqing, China, which ran from 2019 to 2021.
Participants
A total of 803 medical students participated in the study in 2019 and only 484 students responded in 2021. The response rate for our survey was only 60.27% due to graduation, emails being abandoned, etc.
Results
The influenza vaccination rate of students at this medical school was 6.7% in 2019, compared with 25.8% in 2021. The awareness rate of medical students about influenza and influenza vaccine was 82.8% in 2019 and 86% in 2021, and there was no significantly statistical difference between the 2 years (p=0.134); the number of medical students with supportive attitude towards influenza vaccine was 95.1% in 2019 and 97.1% in 2021, and there was no statistically significant difference between the 2 years (p=0.078); the number of students who actively learnt about knowledge related to influenza vaccine rose from 183 (22.8%) in 2019 to 195 (40.3%) in 2021.
Conclusions
The COVID-19 outbreak prompted an increase in influenza vaccination rates among medical students in Chongqing, with almost all students (96.0%) believing that the spread of COVID-19 promoted their knowledge about influenza and influenza vaccine, and the vast majority (74.8%) believing that the spread of COVID-19 promoted their willingness to receive influenza vaccine.
Keywords: epidemiology, public health, immunology, COVID-19
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Comparing knowledge attitude and practice toward influenza vaccine in the same group before and after the COVID-19 outbreak, and this condition cannot be replicated now.
This study will contribute to the promotion of influenza vaccination in the medical student population.
The data were collected online through social networking platforms. Thus, we might have failed to approach the students who were not able to access internet, resulting in a sampling bias.
Because our study was conducted at a medical school in Chongqing, it may limit the generalisability of the study.
Background
Influenza, a respiratory tract infectious disease, is extremely contagious. Influenza virus antigenicity is variable and spreads rapidly. This virus can cause seasonal epidemics each year.1 China’s Influenza Treatment Program (2020 version) clearly states that ‘annual influenza vaccination is the most effective means for influenza prevention, reducing the risk of influenza and serious complications in vaccinated individuals’.2 During the outbreak of the COVID-19 pandemic, the Chinese Ministry of Health considers influenza vaccination for 2020–2021 to be particularly important.3 Influenza vaccination has become especially important as the severe global epidemic of COVID-19 will continue this year and there may be a superimposed epidemic of COVID-19 along with influenza and other respiratory infectious diseases this winter and next spring.
As a place where students frequently gather, the relatively crowded learning and living environment of schools makes it easy for students to catch the influenza, and college students are highly mobile between campuses. Surveillance data from several provinces in recent years have shown that more than 90% of influenza each year occurs on campus. From 2004 to 2008, 90.48% of influenza outbreaks in Jiangsu Province occurred on campus. From 2006 to 2013, 97.26% of influenza outbreaks in Shanxi Province also occurred on campus.4–6 Among all the students on campus, medical students are believed to possess a higher risk of influenza illness than other students due to the specificity of their discipline. They are the future medical workers and important disseminators of health knowledge, so there is a need for vaccination for them.7
However, few has been reported regarding the current status of influenza vaccination in this group in China. From the few studies, it was found that the current vaccination rate of medical students in China was much lower than that of foreign countries. Influenza vaccination rates for medical students were 17.1% in northwest China, 25.3% in Brazil, 20.7% in Saudi Arabia, 53.8% in Australia, 76% in the UK and 43% in the USA.4 7–12 To explore whether medical students’ knowledge, attitude and practice about influenza and influenza vaccine have changed under the influence of today’s COVID-19 epidemic, we compared the results of a survey on their knowledge and attitude about influenza and influenza vaccine among the same group of medical students before the outbreak (2019) and after the outbreak (2021) to (1) investigate the main factors affecting medical students’ willingness to receive influenza vaccination; (2) provide a scientific basis for improving influenza vaccination rates among medical students and strengthening influenza prevention and control efforts in the current context.
Material and methods
Study design and settings
In this prospective cohort study, a survey study focusing on influenza and influenza vaccine awareness and willingness to vaccinate was first conducted among freshman-year to senior-year medical students in a medical school in Chongqing, China from September 2019 to October 2019, and the questionnaire applied was named Q1. A new survey on influenza and influenza vaccine knowledge, attitude and practice to vaccinate with some slight modifications due to the COVID-19 was sent by email to volunteers who had previously received the questionnaire (Q1) in November 2021, and the new questionnaire was named Q2. The questionnaire data were compiled and collected in January 2022. The final return rate of the questionnaire was only 60.27% due to graduation, email discontinuation, etc. All participants in 2019 were randomly selected and volunteered to participate in this experiment and were not involved in the conduct of the study.
Patient and public involvement
This research was done without patient involvement. Patients were not invited to comment on the study design and were not consulted to develop patient-relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Questionnaire
Both questionnaires (Q1 and Q2) were pilot tested on a sample of 30 participants, and their feedback was used to further modify the items. The finalised instrument was administered electronically. The questionnaires used the precautionary measures promoted by the National Health Commission of the People’s Republic of China on its official website as questions to determine the level of knowledge about influenza prevention. The survey consisted of two parts. The first part collected demographic information on profession and gender, while the second part asked about respondents’ knowledge about influenza and the influenza vaccine, as well as attitude towards influenza vaccine—a set of questions with a Cronbach’s α coefficient greater than 0.7.
Survey
We collated questions on influenza-related knowledge and influenza vaccine attitude from both Q1 and Q2 and analysed them after excluding redundant and repetitive questions. Influenza-related knowledge was scored 1 point for a correct answer and 0 point for a wrong answer. The full score was 18 points and a score ≥11 would be judged as knowing. Influenza vaccine knowledge rate (%)=number of correct answers/total number of respondents×100%. For influenza vaccine attitude, a score was assigned according to the attitude towards influenza vaccine (5=very positive, 4=positive, 3=fair, 2=negative, 1=very negative). The full score was 25, any scores ≥15 would be considered as having a positive attitude towards influenza vaccine. Vaccine vaccination rate (%)=number of influenzas vaccinated/total number of surveyed×100%. Influenza vaccination willingness rate (%)=number of people willing to receive influenza vaccination/total number of people surveyed×100%.
Data analysis
Epidata V.3.0 software was used for double data entry, and SPSS V.24.0 software was used for statistical analysis. The differences between rates were analysed by Χ2 test, and unconditional logistic stepwise regression analysis was used for influencing factors of influenza vaccination intention. The level of statistical significance was chosen to be 0.05 (α=0.05).
Results
Demographics
A total of 803 medical students participated in the study between September and October 2019. Only 484 medical students answered the questionnaire during the return visit in November 2021. We define freshmen, sophomores and juniors as lower division students, and seniors and fifth-year students as the senior group. In the comparison between 2021 and 2019, there are statistically significant differences in gross monthly income (GMI), age and grade level, and the specific information can be seen in table 1.
Table 1.
Demographic characteristics of the study participants in Chongqing
| Demographic information | 2019 n (%) |
2021 n (%) |
Total | P value |
| Gender | ||||
| Male | 294 (36.6) | 179 (37.0) | 473 | 0.894 |
| Female | 509 (63.4) | 305 (63.0) | 814 | |
| GMI | ||||
| <¥4000 | 507 (63.1) | 275 (56.8) | 782 | 0.025 |
| ≥¥4000 | 296 (36.9) | 209 (43.2) | 505 | |
| Age | ||||
| 18–20 years old | 350 (43.6) | 177 (36.6) | 527 | 0.013 |
| 21–23 years old | 453 (56.4) | 307 (63.4) | 760 | |
| Grade level | ||||
| Lower division | 167 (20.8) | 39 (8.1) | 206 | <0.001 |
| Senior group | 636 (79.2) | 445 (91.9) | 1081 |
GMI, gross monthly income.
Knowledge
The knowledge rate of medical students about influenza and influenza vaccine was 82.8% in 2019 and 86% in 2021, and there was no statistically significant difference between the two comparisons (p=0.134). The following six questions: (1) ‘wearing a mask can prevent the spread of the influenza to some extent’; (2) ‘incubation period of influenza’; (3) ‘influenza can be spread through close contact with patient’; (4) ‘influenza vaccination for immunity is less costly and more cost-effective than developing immunity from influenza infection’; (5) ‘the best time to get an influenza vaccination’; and (6) ‘How often should you get an influenza vaccination?’ are significantly more known to the students in 2021 than in 2019. Meanwhile, these three questions: (1) ‘patients with influenza can spread the infection before symptoms appear’; (2) ‘influenza vaccination does not give you the influenza although it carries live virus’; and (3) ‘What do you think the purpose of influenza vaccination is?’ are less known to the students in 2021 than in 2019 (table 2).
Table 2.
Comparison of influenza vaccine knowledge in 2019 and 2021
| Knowledge | Knowledge awareness level | ||
| 2019 awareness rate n (n/N×100%) |
2021 awareness rate n (n/N×100%) |
P value | |
| Wearing a mask helps to prevent the spread of the influenza | 699 (87.0) | 472 (97.5) | <0.001 |
| Influenza is mainly spread by respiratory (coughing, sneezing) droplets | 785 (97.8) | 475 (98.1) | 0.640 |
| Incubation period of influenza | 193 (24.0) | 156 (32.2) | 0.001 |
| Influenza carriers (without symptoms) can spread the infection | 706 (87.9) | 391 (80.8) | 0.001 |
| Patients are contagious | 525 (65.4) | 439 (90.7) | <0.001 |
| The influenza shot that contains live viruses cannot cause people to get influenza | 690 (85.9) | 272 (56.2) | <0.001 |
| Influenza vaccination for immunity is less costly and more cost-effective than developing immunity from influenza infection | 373 (46.5) | 420 (86.8) | <0.001 |
| The best time to get vaccinated | 412 (51.3) | 310 (64.0) | <0.001 |
| Frequency of vaccination | 297 (37.0) | 213 (44.0) | 0.013 |
| Perception of the aim of influenza vaccination | 733 (91.3) | 422 (87.2) | 0.020 |
| Side effects of influenza vaccination | |||
| Fever | 540 (67.2) | 364 (75.2) | 0.002 |
| Pain and swelling at the injection site | 672 (83.7) | 419 (86.6) | 0.160 |
| Headaches | 448 (55.8) | 318 (65.7) | <0.001 |
| Influenza vaccination priority groups | |||
| People over 60 years old | 577 (71.9) | 351 (72.5) | 0.797 |
| Patients with chronic illnesses and infirmity | 705 (87.8) | 400 (82.6) | 0.011 |
| Health facility staff, especially front-line staff | 715 (89.0) | 415 (85.7) | 0.082 |
| Pupils and kindergarten children | 714 (88.9) | 420 (86.8) | 0.253 |
| Pregnant women over the first trimester of pregnancy | 360 (44.8) | 192 (39.7) | 0.069 |
Attitudes
The percentage of medical students who were supportive of influenza vaccine was 95.1% in 2019 and 97.1% in 2021, with no statistically significant difference between the two comparisons (p=0.078). As compared with the students’ responses from 2019, a higher percentage of medical students in 2021 believe that the influenza vaccine is safe (91.5%>65.1%); the influenza vaccination is necessary (83.9%>67.0%); the seasonal influenza vaccine is effective in preventing seasonal influenza (86.8%>73.2%); vaccination is important. However, we also observed a higher percentage of students in 2021 worried about the side impacts of influenza vaccine relative to those in 2019 (56.0%>25.5%) (table 3).
Table 3.
Comparison of influenza vaccine attitudes in 2019 vs 2021
| Attitude | 2019 | 2021 | P value | ||
| n | % (n/N) | n | % (n/N) | ||
| Influenza vaccine is safe | |||||
| Agree | 523 | 65.1 | 443 | 91.5 | <0.001 |
| Disagree | 280 | 34.9 | 41 | 8.5 | |
| Influenza vaccination is necessary | |||||
| Agree | 538 | 67.0 | 406 | 83.9 | <0.001 |
| Disagree | 265 | 33.0 | 78 | 16.1 | |
| You are not worried about the side effects of the influenza vaccine | |||||
| Agree | 205 | 25.5 | 271 | 56.0 | <0.001 |
| Disagree | 598 | 74.5 | 213 | 44.0 | |
| The seasonal influenza vaccine is more effective in preventing seasonal influenza | |||||
| Agree | 588 | 73.2 | 420 | 86.8 | <0.001 |
| Disagree | 215 | 26.8 | 64 | 13.2 | |
| Annual influenza vaccination is important for you | |||||
| Agree | 346 | 43.1 | 287 | 59.3 | <0.001 |
| Disagree | 457 | 56.9 | 197 | 40.7 | |
| You are planning to get an influenza vaccination this autumn/winter | |||||
| Agree | 268 | 33.4 | 187 | 38.6 | 0.056 |
| Disagree | 535 | 66.6 | 297 | 61.4 | |
Practices
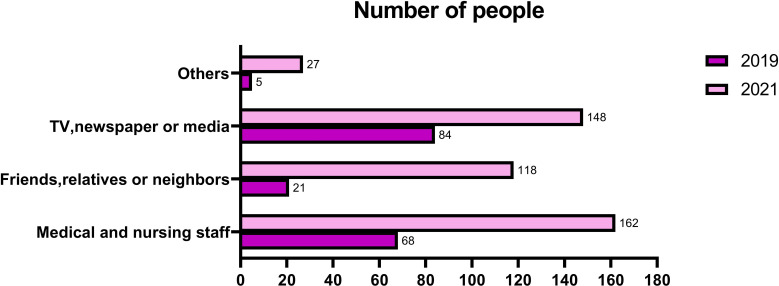
The main source of influenza vaccine information in 2019 was television, newspapers and the media (48.6%), while the main source in 2021 was healthcare professionals (35.6%) (figure 1).
Figure 1.
Sources of influenza vaccine information for 2019 vs 2021.
The number of people actively seeking information about influenza vaccine rose from 183 (22.8%) in 2019 to 195 (40.3%) in 2021. The number of people who received influenza vaccination in 2021 was much higher than in 2019 (25.8%>6.7%), and the most significant increase in adverse reactions to vaccination was seen in the phenomenon of temporary mild pain, redness and swelling at the injection site (39.2%>18.5%). Among the reasons for receiving influenza vaccination, both ‘to enhance resistance and prevent influenza’ (88.8%>75.9%) and ‘recommended by government and health authorities’ (72.0>44.4%) were selected by a higher percentage of students in 2021 relative to 2019 (table 4).
Table 4.
Comparison of influenza vaccination behaviour in 2019 vs 2021
| Behaviour | 2019 | 2021 | P value | ||
| n | % (n/N) | n | % (n/N) | ||
| Do you take the initiative to learn about the influenza vaccine? | |||||
| Yes | 183 | 22.8 | 195 | 40.3 | <0.001 |
| No | 620 | 77.2 | 289 | 59.7 | |
| Did you get an influenza vaccination last year? | |||||
| Yes | 54 | 6.7 | 125 | 25.8 | <0.001 |
| No | 749 | 93.3 | 359 | 74.2 | |
| Did you have any of the following adverse reactions in your last influenza vaccination? | |||||
| Severe allergic reactions | 7 | 13.0 | 23 | 18.4 | 0.362 |
| Dizziness | 9 | 16.7 | 26 | 20.8 | 0.483 |
| Low fever | 7 | 13.0 | 23 | 18.4 | 0.337 |
| Transient mild pain, redness and swelling at the injection site | 10 | 18.5 | 49 | 39.2 | 0.004 |
| No adverse reactions | 36 | 66.7 | 67 | 53.6 | 0.136 |
| What are your reasons for getting the influenza vaccine? | |||||
| Build up your resistance and prevent influenza | 41 | 75.9 | 111 | 88.8 | 0.033 |
| Recommendation from government and health authorities | 24 | 44.4 | 90 | 72.0 | <0.001 |
| Recommended by family and friends | 17 | 31.5 | 58 | 46.4 | 0.061 |
| Other | 3 | 5.6 | 1 | 0.8 | 0.061 |
| Have you had an influenza-like illness within 1 year of vaccination? | |||||
| Yes | 8 | 14.8 | 17 | 13.6 | <0.001 |
| No | 25 | 46.3 | 96 | 76.8 | |
| Don’t remember | 21 | 38.9 | 12 | 9.6 | |
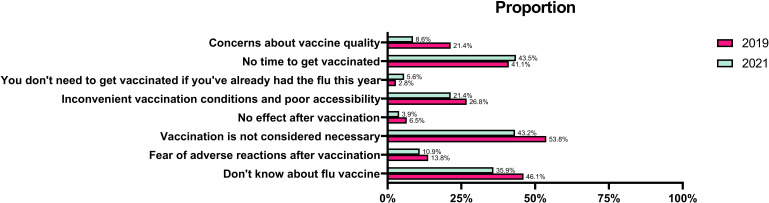
The three main reasons for not getting vaccinated in 2019 were ‘did not think it was necessary to get vaccinated’ (53.8%), ‘did not know about the influenza vaccine’ (46.1%) and ‘did not have time’ (41.1%). The three main reasons for not getting vaccinated in 2021 were: ‘didn’t have time to get vaccinated’ (43.5%), ‘didn’t think it was necessary to get vaccinated’ (43.2%) and ‘didn’t know about the influenza vaccine’ (35.9%) (figure 2).
Figure 2.
Main reasons for not getting an influenza vaccination in 2019 vs 2021.
During the COVID-19 epidemic in 2021, most students believed that the epidemic promoted awareness of influenza and influenza vaccine (96%) and willingness to receive influenza vaccination (74.8%) (table 5).
Table 5.
Analysis of COVID-19-related behaviours in 2021 (frequency statistics)
| COVID-19-related acts | Number of people | Percentage |
| The COVID-19 outbreak promotes your learning about respiratory infectious diseases | ||
| Yes | 400 | 82.6 |
| No | 84 | 17.4 |
| The COVID-19 outbreak raised your awareness of influenza and influenza vaccine | ||
| Yes | 384 | 96.0 |
| No | 16 | 4.0 |
| The COVID-19 outbreak boosts your intention to get influenza vaccinated | ||
| Yes | 362 | 74.8 |
| No | 122 | 25.2 |
Analysis of single factors affecting medical students’ vaccination intentions in 2021
The vaccination rate of medical students who actively learnt about influenza vaccine was significantly higher than that of medical students who did not actively learn about it (47.2%>11.4%), and the vaccination rate of medical students who actively learnt about respiratory viral infectious diseases during COVID-19 was also higher than that of medical students who did not actively learn about it (29.5%>8.3%) (table 6).
Table 6.
Analysis of factors influencing medical students' willingness to receive vaccinations in 2021
| Variables | Number of people vaccinated (%) | Number of unvaccinated persons (%) | OR value (95% CI) | P value |
| Gender | ||||
| Male | 49 (27.4) | 130 (72.6) | 1.136 (0.747 to 1.726) | 0.551 |
| Female | 76 (24.9) | 229 (75.1) | Reference | |
| Age | ||||
| 18–20 | 48 (27.1) | 129 (72.9) | 1.111 (0.7300 to 1.692) | 0.622 |
| 21–23 | 77 (25.1) | 230 (74.9) | Reference | |
| Grade level | ||||
| Lower school | 14 (35.9) | 25 (64.1) | 1.685 (0.846 to 3.355) | 0.137 |
| Upper school | 111 (24.9) | 334 (75.1) | Reference | |
| GMI | ||||
| <¥4000 | 65 (23.6) | 210 (76.4) | 0.769 (0.511 to 1.157) | 0.207 |
| ≥¥4000 | 60 (28.7) | 149 (71.3) | Reference | |
| Attitudes towards the influenza vaccine | ||||
| Negative | 1 (7.1) | 13 (92.9) | Reference | 0.140 |
| Active | 124 (26.4) | 346 (73.6) | 4.659 (0.603 to 35.984) | |
| Level of knowledge | ||||
| Understanding | 112 (26.9) | 304 (84.7) | 1.559 (0.820 to 2.962) | 0.443 |
| Don’t understand | 13 (19.1) | 55 (80.9) | Reference | |
| Proactive about information about influenza vaccines | ||||
| Yes | 92 (47.2) | 103 (52.8) | 6.929 (4.380 to 10.963) | <0.001 |
| No | 33 (11.4) | 256 (88.6) | Reference | |
| Learning about respiratory infectious diseases during the COVID-19 outbreak | ||||
| Yes | 118 (29.5) | 282 (70.5) | 4.603 (2.062 to 10.275) | <0.001 |
| No | 7 (8.3) | 77 (91.7) | Reference | |
GMI, gross monthly income.
Discussion
This study showed that the influenza vaccination rate of medical students in the studied medical school was only 6.7% in the 2019 influenza season, which is lower than the vaccination levels of medical students in other cities such as Urumqi, China (9.2% in 2010).9 In 2021, the vaccination rate of medical students against influenza rose to 25.8%, which was not as high as the vaccination level of medical students in developed countries such as the USA and the UK, but it is also a significant improvement as compared with 2019. This finding indicates that the COVID-19 outbreak has significantly boosted the influenza vaccination rate of the medical students that we studied. Similar results were obtained in a teaching and research hospital in Milan, during the COVID-19 pandemic, and influenza vaccination rates for physicians and administrative staff rise significantly.13 This may be due to the fact that there are numerous studies showing a significant reduction in the possibility of contracting COVID-19 after receiving the influenza vaccine, therefore, the willingness to receive the influenza vaccine has increased.14 15
However, the level of influenza vaccination among medical students in Chongqing is still low and needs to be further improved, and it is recommended that medical students be included in the key recommended vaccination targets for influenza vaccination.
Looking at the demographic characteristics of the students, the GMI in 2021 is higher than that in 2019, which our speculation may be due to inflation. Over time, the age and grade level in 2021 are higher than in 2019, which is also in line with the objective rule and our speculation.
In terms of knowledge, there was no significant difference between the comparison of 2021 and 2019 (p=0.134). However, on average, only a quarter of the students knew the incubation period time of influenza, and one similar study found that university education has a positive impact on influenza knowledge,16 indicating that students at this university do not pay much attention to influenza-related courses. The questions ‘wearing a mask can prevent the spread of influenza to some extent,’ ‘influenza can be spread through close contact with patients’ and ‘compared with developing immunity from influenza infection, getting immunity from influenza vaccination has better cost-effectiveness’ are answered significantly more correctly in 2021 than in 2019. This is because of the emergence of COVID-19, which is more widely known due to state and government campaigns and changes in daily lifestyle (eg, the need to wear a mask when using public transportation). The question ‘side impacts of influenza vaccination: fever, headache’ was also better answered in 2021, probably due to the reactions that occurred during the vaccination with COVID-19 or the possible side impacts told by doctors or teachers before the vaccination.17 18 As for the question ‘chronically ill and frail people are the priority recommended population for influenza vaccination’, the answer was reversely better in 2019 than in 2021 (87.8%>82.6%), which we speculate that this may be due to the fact that the COVID-19 vaccine is prohibited for patients with acute exacerbation of chronic disease or severe uncontrolled chronic disease in the Chinese New Crown Vaccination Technical Guidelines (V.1), so some participants misunderstood that influenza vaccine is also contraindicated for patients with chronic disease, thus leading to a poor response to this question.19–22
Regarding the comparison of attitudes towards influenza vaccine, although there was no significant difference between 2021 and 2019 (p=0.078), students in 2021 were more likely to believe that influenza vaccine is safe and important, that vaccination against influenza is necessary and that they are not concerned about the side impacts of influenza vaccine. There are good reasons to attribute this to the COVID-19 epidemic.
The most important reason for influenza vaccination among medical students in both 2021 and 2019 was ‘to increase resistance and prevent influenza’, which is consistent with other studies,23–25 indicating that concerns for one’s health are the driving factor for influenza vaccination in this group. The reason ‘recommended by the government and health authorities’ increased from 44.4% in 2019 to 72% in 2021, this is likely because of the government’s strong call for people to get COVID-19 vaccine in the past year, which led to the group’s increased interest in influenza vaccination.
Among students who reported not receiving the influenza vaccine, the reasons for not receiving the vaccine in 2021 and 2019 are not very different, with a significant percentage of students not considering it necessary, suggesting that the influenza vaccine is not being taken seriously by this group. Among those who have not received the influenza vaccine, the percentage of students who have ‘never heard of the influenza vaccine’ reached 46.1% in 2019 and 35.9% in 2021. It is recommended that health education on influenza and influenza vaccine should be strengthened, such as holding a competition on influenza and influenza vaccine knowledge and providing specific training on influenza vaccination in degree programmes. Vaccine safety was the least influential factor impeding vaccination, indicating solid expertise among study participants. The results of the present study suggest that providing more information about increasing influenza vaccine awareness and basic knowledge of influenza vaccines among study participants may help improve vaccine coverage.
This study found that students with more knowledge about influenza vaccine were more inclined to receive influenza vaccine, which is consistent with previous studies.26 Students who took the initiative to learn about respiratory viral infectious diseases during COVID-19 transmission were also more likely to get the influenza vaccine, suggesting that the promotion and dissemination of knowledge about COVID-19 also helped people to understand more about influenza and influenza vaccine. This shows that in the current environment, we should attach knowledge about influenza to the promotion of COVID-19-related knowledge and prevention methods, so that people can receive COVID-19 vaccination and also pay attention to influenza vaccination, thereby increasing the influenza vaccination rate.
Limitations
This study has certain limitations. First, the data were collected via self-reported questionnaires, which can be a potential cause of reporting bias. Second, since our data were collected from medical students only, there is a possibility that they might have answered the questions positively on the basis of their medical knowledge as they had already perceived what would be expected from them. Third, the data were collected online through social networking platforms. Thus, we might have failed to approach the students who were not able to access internet, resulting in a sampling bias. Last, because our study was conducted at a medical school in Chongqing, China, it may limit the generalisability of the findings from this study. We will subsequently expand the sample source in hope of obtaining better results.
Conclusion
The COVID-19 outbreak prompted an increase in influenza vaccination rates among medical students in Chongqing (6.7% in 2019 to 25.8% in 2021), with almost all students (96.0%) believing that the spread of COVID-19 promoted their knowledge of influenza and influenza vaccine, and the vast majority (74.8%) believing that the spread of COVID-19 promoted their willingness to receive influenza vaccine. We could disseminate information about influenza vaccine along with information about COVID-19 vaccine to help increase influenza vaccination rates.
Supplementary Material
Acknowledgments
The authors thank all participants of this study for sharing their time and experiences.
Footnotes
YW and GW contributed equally.
Contributors: YW and XT drafted the manuscript. GW and XT designed the questionnaire. YW and FZ collected the data. GW, LG, QL, YJ and FZ participated in data analysis and data extraction. YW and XW finalised the manuscript. All authors read and approved the final manuscript. XT is the guarantor of our article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This 2-year prospective cohort study was approved by the Ethics Committee of Chongqing Medical University. Participation in this study was voluntary, and informed consent was gained. Our data collection procedures complied with the institutional and national ethical guidelines and followed the Declaration of Helsinki. The anonymity and confidentiality of data were maintained. Written informed consent was obtained from the investigators for this experiment.
References
- 1.Chinese Center for Disease Control and Prevention . Technical guidelines for seasonal influenza vaccination in China (2020-2021). Chin J Viral Dis 2020;10:403–16. [Google Scholar]
- 2.Guidelines for diagnosis and treatment of influenza (2020 version). Chin J Viral Dis 2021:1–5. [Google Scholar]
- 3.Krishnaratne S, Pfadenhauer LM, Coenen M, et al. Measures implemented in the school setting to contain the COVID-19 pandemic: a scoping review. Cochrane Database Syst Rev 2020;12:CD013812. 10.1002/14651858.CD013812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tuohetamu S, Pang M, Nuer X, et al. The knowledge, attitudes and practices on influenza among medical college students in Northwest China. Hum Vaccin Immunother 2017;13:1688–92. 10.1080/21645515.2017.1293769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li L, Pan H, Bao CJ. Epidemic features and influencing factors of recent influenza outbreaks in Jiangsu Province. Modern Preventive Med 2009;36:3221–4. [Google Scholar]
- 6.Ma P, Wang JJ, Zhang Y. Epidemiological characteristics and influence factors of influenza outbreak in Shaanxi Province, 2006–2013. Chinese J Public Health 2015;31:17–21. [Google Scholar]
- 7.Gray G, Cooper J. An evaluation of influenza vaccine uptake in UK medical students. Occup Med 2021;71:105–8. 10.1093/occmed/kqab014 [DOI] [PubMed] [Google Scholar]
- 8.Abalkhail MS, Alzahrany MS, Alghamdi KA, et al. Uptake of influenza vaccination, awareness and its associated barriers among medical students of a university hospital in central Saudi Arabia. J Infect Public Health 2017;10:644–8. 10.1016/j.jiph.2017.05.001 [DOI] [PubMed] [Google Scholar]
- 9.Tuohetamu S, Pang M, Nuer X, et al. The knowledge, attitudes and practices on influenza among medical college students in Northwest China. Hum Vaccin Immunother 2017;13:1688–92. 10.1080/21645515.2017.1293769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deckers Leme M, Elias Gilio A. Health worker recommended vaccination rates among medical students in Brazil. Vaccine X 2021;9:100118. 10.1016/j.jvacx.2021.100118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walker L, Newall A, Heywood AE. Knowledge, attitudes and practices of Australian medical students towards influenza vaccination. Vaccine 2016;34:6193–9. 10.1016/j.vaccine.2016.10.074 [DOI] [PubMed] [Google Scholar]
- 12.Rogers CJ, Bahr KO, Benjamin SM. Attitudes and barriers associated with seasonal influenza vaccination uptake among public health students; a cross-sectional study. BMC Public Health 2018;18:1131. 10.1186/s12889-018-6041-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perrone PM, Biganzoli G, Lecce M, et al. Influenza vaccination campaign during the COVID-19 pandemic: the experience of a research and teaching hospital in Milan. Int J Environ Res Public Health 2021;18:5874. 10.3390/ijerph18115874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jabr Alwazzeh M, Mohammed Telmesani L, Saud AlEnazi A, et al. Seasonal influenza vaccination coverage and its association with COVID-19 in Saudi Arabia. Inform Med Unlocked 2021;27:100809. 10.1016/j.imu.2021.100809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang M-J, Rooks BJ, Le T-TT, et al. Influenza vaccination and hospitalizations among COVID-19 infected adults. J Am Board Fam Med 2021;34:S179–82. 10.3122/jabfm.2021.S1.200528 [DOI] [PubMed] [Google Scholar]
- 16.Szilagyi PG, Schaffer S, Rand CM, et al. School-located influenza vaccination: do vaccine clinics at school raise vaccination rates? J Sch Health 2019;89:1004–12. 10.1111/josh.12840 [DOI] [PubMed] [Google Scholar]
- 17.Leng A, Maitland E, Wang S, et al. Individual preferences for COVID-19 vaccination in China. Vaccine 2021;39:247–54. 10.1016/j.vaccine.2020.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang Y, Zeng G, Pan H, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18-59 years: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect Dis 2021;21:181–92. 10.1016/S1473-3099(20)30843-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma A, Patnaik I, Kumar A, et al. COVID-19 vaccines in patients with chronic liver disease. J Clin Exp Hepatol 2021;11:720–6. 10.1016/j.jceh.2021.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morawska M. Reasons and consequences of COVID-19 vaccine failure in patients with chronic lymphocytic leukemia. Eur J Haematol 2022;108:91–8. 10.1111/ejh.13722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alghamdi AA, Aldosari MS, Alsaeed RA. Acceptance and barriers of COVID-19 vaccination among people with chronic diseases in Saudi Arabia. J Infect Dev Ctries 2021;15:1646–52. 10.3855/jidc.15063 [DOI] [PubMed] [Google Scholar]
- 22.Bureau of Disease Control Prevention, National Health Commission of the People′s Republic of China (Version 1) . Technical guidelines for novel coronavirus vaccination (first edition). Chinese J Viral Dis 2021;11:161–2. [Google Scholar]
- 23.Bednarczyk RA, Chu SL, Sickler H, et al. Low uptake of influenza vaccine among university students: evaluating predictors beyond cost and safety concerns. Vaccine 2015;33:1659–63. 10.1016/j.vaccine.2015.02.033 [DOI] [PubMed] [Google Scholar]
- 24.Seale H, Leask J, MacIntyre CR. Attitudes amongst Australian hospital healthcare workers towards seasonal influenza and vaccination. Influenza Other Respir Viruses 2010;4:41–6. 10.1111/j.1750-2659.2009.00112.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gallone MS, Gallone MF, Cappelli MG, et al. Medical students' attitude toward influenza vaccination: results of a survey in the University of Bari (Italy). Hum Vaccin Immunother 2017;13:1937–41. 10.1080/21645515.2017.1320462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fehér Ágnes, Fekete M, Varga JT, et al. [Medical students' knowledge on vaccinology]. Orv Hetil 2019;160:1193–9. 10.1556/650.2019.31426 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request.