Abstract
Optimal management of pedunculated ulnar polydactyly is not defined. This systematic review summarises objective and patient-reported outcomes following primary treatment. Two authors screened articles for inclusion according to a PROSPERO published protocol. The meta-analysis of adverse events was performed, and a narrative synthesis of satisfaction and patient-reported outcomes was reported. The risk of bias was assessed using Cochrane's ROBINS-I tool. Of 1650 articles identified, 15 were eligible, including 13 single-arm and 2 multi-arm studies. Complications were 6 times as likely with ligation procedures (22%), compared to surgical removal (1%) whether this was performed in the outpatient setting or operating theatre (OR 6.89 [95% CI 1.73, 27]). Parent-reported satisfaction was high for all treatments. Studies were at high risk of bias and low methodological quality. Outcome measurement and follow-up were heterogenous. Well-designed prospective observational and experimental studies are required to inform practice, incorporating clinician and parent-reported outcomes and economic analyses.
Level of evidence: I.
Keywords: Ulnar polydactyly, Adverse events, Patient-reported outcomes, Surgical outcomes, Excision ligation
Introduction
Ulnar (post-axial) polydactyly is a congenital upper limb anomaly characterised by the presence of an extra digit on the ulnar border of the hand at birth. Two distinct subtypes are recognised (Temtamy and MsKusick): type A, in which a fully developed extra digit articulates with either the fifth metacarpal or a duplicated metacarpal; or more commonly type B, a rudimentary non-functional digit that is attached by a soft tissue bridge.1 Approximately three quarters of cases of type B ulnar polydactyly are bilateral, and 85% have a family history.1,2
The treatment of type B ulnar polydactyly is the removal of the non-functioning accessory digit, which carries a mild degree of functional disability, to restore a normal appearance of the hand.3,4 The most effective treatment remains a topic of debate, and there is substantial variation in practice globally.4 Two treatments are most frequently reported: (1) suture/clip ligation2 or (2) surgical excision.5,6
Ligation involves tying off the base of the skin bridge with (typically) either a suture or metal clip, thereby inducing ischaemic necrosis and auto-amputation of the accessory digit. It is regarded as effective, well tolerated by patients and families and may avoid costs and complications associated with hospital admission and surgery under anaesthesia.2,7 The disadvantages include a delay to autoamputation, a residual skin bridge that may be problematic in later life, risk of treatment failure and infection.2,4
Surgical excision of the accessory digit may be performed in the outpatient clinic or operating theatre, under local or general anaesthesia depending on the age of the infant. Surgery may facilitate more proximal excision of accessory nerves, therefore, theoretically reducing the incidence of neuroma2,8 and may improve the aesthetic outcome.9,10 Potential disadvantages include parental distress whilst awaiting treatment, need for general anaesthesia in older infants, and increased costs associated with hospital admission and an operative procedure.11 One systematic review reports that complications are more prevalent following ligation compared with surgical excision; however, significant methodological flaws render their results unreliable.4
The aim of this systematic review is to compare the outcomes of suture ligation, office-based excision and operating room-based excision in type B ulnar polydactyly through a systematic appraisal of the literature.
Methods
The study was conducted in accordance with the Cochrane handbook for systematic reviews of interventions and was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The protocol was registered on Prospero (CRD42019156164).
Search strategy
The following databases were searched through the OVID search platform: (1) PubMed, (2) EMBASE, (3) PsycINFO, and (4) the Cochrane Library on October 30, 2019 to identify all articles reporting outcomes in primary interventions for type B ulnar polydactyly. See Supplementary Figure 1 for the search strategy in full.
Study selection
Studies that assessed outcomes following primary intervention for type B ulnar polydactyly were determined as eligible for inclusion. We included observational and experimental studies of any design. Case reports, review articles with no new primary data, and commentaries were excluded. Titles and abstracts were reviewed by two independent reviewers (LG and HS) against the inclusion and exclusion criteria, and discrepancies were resolved through discussion with a third independent reviewer (JW). The full texts of those considered to be potentially eligible for inclusion were reviewed by two independent reviewers against the inclusion/exclusion criteria. Any disagreements were resolved by discussion and review by a third independent reviewer.
Data extraction
Interventions have been grouped into the following three treatment methods: (1) Suture/clip ligation, (2) office based/minor treatment room excision and (3) operating room-based excision (under either local and general anaesthesia). A pre-piloted proforma was used to extract data from the studies that are included for analysis. The extracted information includes baseline characteristics, participant demographics and details of the intervention methods and study design. The outcomes for synthesis were as follows: (1) the prevalence of adverse events (clinician or parent-reported outcomes); (2) patient/parent satisfaction or ratings of appearance; (3) other clinician-assessed postoperative outcomes. Additional outcomes of interest include parent expressions of preference or motivation in treatment, local pathways, and influence of family history on decision-making.
Risk of bias in individual studies
The risk of bias was assessed using the risk of bias In Non-randomised Studies of Interventions (ROBINS-I) tool and presented using Robvis.12 Studies were assessed by two independent reviewers, and disagreements were resolved by discussion (HS/LG).
Synthesis of results
The pooled prevalence of complications was estimated using the metaprop package in Stata/MP v15. DerSimonian and Laird random effects were used given the clinical heterogeneity. The Freeman-Tukey arcsine transformation was used to stabilise the variance. However, 95% confidence intervals (CIs) around the study-specific and pooled prevalence were computed using the score-test statistic. Variations in the prevalence of complications were explored by meta-regression using metareg.13 P-values were permuted with 20,000 iterations. Statistical heterogeneity was assessed by I2. A z-test (and the corresponding p-values) assessed whether the observed prevalence was different from zero per cent. To assess possible small-study effects (or publication bias across studies), we produced a funnel plot using metafunnel.
Results
Study selection
After screening 1650 records, 15 studies2,5,16, 17, 18, 19, 20,6, 7, 8, 9, 10, 11,14,15 were included (PRISMA flowchart, as shown Figure 1).
Figure 1.
PRISMA flow diagram.
Study characteristics
The studies originated from different 5 countries (UK, USA, Israel, India and Austria; Table 1). All were cohort studies, three prospective2,1,20 and 12 retrospective.5,6,18,19,7, 8, 9, 10,14, 15, 16, 17 There were two multi-arm studies8,11 whilst the remainder was single-arm studies. Across all studies, interventions to remove the accessory digit were performed from 2 days of age20 up to a maximum of 4.2 years6 with an average age of 96 days. Revisional procedures were performed up to a maximum age of 13 years.9 Age of intervention varied with treatments, with ligation performed from 1 week2 to 40 weeks of age,7 clinic-based excision from 2 days20 to 4.2 years6 and OR-based excision from 3 days18 to 36 months.19 Where reported, the male/female ratio was 1.3:1 (Table 2).
Table 1.
Study design and characteristics.
| Author (date) | Location | Study design | Participants | Study size | Digits | Age at intervention | M:F ratio | Previous intervention | Procedure |
|---|---|---|---|---|---|---|---|---|---|
| Ligation | |||||||||
| Watson & Henrikus (1997) | USA | Prospective case series | Type B (T&M) | 21 | 37 | (1–2 weeks) | 12:9 | None | Suture ligation in neonatal nursery |
| Mills (2014) | USA | Retrospective case series | Type B (T&M) base of digit < 6mm | 132 | 231 | 8 weeks (2–40 weeks) | 77:55 | None | OPD clip application with LA |
| Clinic-based excision | |||||||||
| Katz (2011) | Israel | Prospective case series | Type B (T&M) | 11 | 15 | (2–3 days) | 6:5 | None | LA excision, neonatal minor ops room |
| Carpenter (2015) | USA | Retrospective case series | Type B (T&M) | 26 | 38 | 3.3months (9 days - 4.2 years) | NR | 5 patients had previous suture ligation, now being treated for residual bump | LA excision, office-based |
| Al Hassani (2019) | UK | Retrospective case series | Stelling I | 28 | 43 | 69 Days (27–134) | 14:16 | None | LA excision in paediatric minor treatment unit |
| Operating theatre-based excision | |||||||||
| Stewart (2001) | UK | Retrospective case series | ‘Minor forms’ of U.P. | 40 | NR | 3 days (1–14 days) | NR | None | LA surgical excision |
| Leber (2003) | USA | Retrospective case series | Pedunculated supernumerary digits | 6 | 11 | (3 weeks – 21 months) | 3:3 | none | Surgical excision |
| Mullick (2010) | USA | Retrospective case series | Type B (T&M) | 10 | 13 | (1 week – 13 years) | 5:5 | All presented with incomplete amputations, painful neuroma or both – prev. ligation | GA surgical excision |
| Khan (2012) | India | Retrospective case series | Stelling IIa UP | 10 | 20 | 18.2 months (6–36 months) | 5:5 | None | GA surgical excision |
| Ahmad (2014) | UK | Retrospective case series | Type B (T&M) | 86 | 135 | (<10 weeks) | NR | None | LA surgical excision |
| Singer (2014) | Austria | Retrospective case series | Stelling I/II/III | 32 | 41 | 8.6 months (0–10months) | NR | NR | GA surgical excision |
| Macdonald (2017) | UK | Retrospective case series | Type B (T&M) | 20 | NR | (< 6 weeks) | NR | None | LA surgical excision |
| Shirley (2019) | UK | Retrospective case series | Stelling I | 40 | 58 | (3 – 18 weeks) | NR | None | LA surgical excision |
| Comparative studies | |||||||||
| Rayan (2000) | USA | Retrospective cohort study | All types UP (82% Stelling I/II) | 122 | 123 | NR | 85:63 | None | Suture ligation Surgical excision No treatment |
| Samra (2016) | USA | Prospective cohort study | Type B (T&M) | 14 | 25 | NR | NR | None | Suture ligation LA excision in clinic, GA excision in OR |
Table 2.
Adverse events and patient-reported outcomes.
| Author | Admission (Y/N/NR) | FU period | Overall complication | Treatment failure | Neuroma | Nubbin Unaesthetic scar |
Revision procedure | Parent reported outcomes |
|---|---|---|---|---|---|---|---|---|
| Ligation | ||||||||
| Watson & Henrikus (1997) | N | 1–2 weeks, then 15/21 patients at 20 months | 57.1% | 4.7% | NR | 52.4% | 4.7% | No parent reported outcomes |
| Rayan (2000) LIGATION N = 105 |
NR | 1–2 weeks (some at 12–37 months) | 23.5% | NR | 6.7% | 16.1% | 2.8% | No parent reported outcomes |
| Mills (2014) | NR | 10–14 days | 10.7% | NR | 7% | 3.7% | 7% | No parent reported outcomes |
| Samra (2016) LIGATION N = 2 |
NR | 1 month and 3 months | 0% | NR | NR | NR | NR | 0 – 10 satisfaction score 10 Higher perceived pain 5/10 |
| Clinic-based excision | ||||||||
| Katz (2011) | NR | Post-op Day 1, 1 week, 1 year | 0% | 0% | NR | 0% | 0% | ‘All expressed satisfaction with cosmetic result’ |
| Carpenter (2015) | N | NR | 7.7% | NR | NR | NR | NR | No parent reported outcomes |
| Samra (2016) LA Excision N = 10 |
NR | 1 month and 3 months | 0% | NR | NR | NR | NR | 9.8/10 satisfaction score |
| Al Hassani (2019) | N | Telephone questionnaire | NR | NR | NR | NR | NR | 100% rated scar as excellent. 24 would recommend, 4 would not |
| Operating theatre-based excision | ||||||||
| Rayan (2000) EXCISION N = 27 |
NR | 1–2 weeks (some at 12–37 months) | 3.7% | NR | 3.7% | 0% | 0% | No parent reported outcomes |
| Stewart (2001) | NR | None | NR | NR | NR | NR | NR | High levels of satisfaction 39/40 felt that scar barely noticeable |
| Leber (2003) | NR | Up to 6 years | 0% | NR | NR | NR | 0 | All were pleased with cosmetic result |
| Mullick (2010) | NR | 1–3 months post-op | 0 | 0 | 0 | 0 | 0 | Cosmetic outcome - All regarded ‘Acceptable’ to parents + surgeon |
| Khan (2012) | NR | 2 years | 10% (infection) | 0 | 0 | 0 | 0 | No parent reported outcomes |
| Ahmad (2014) | NR | None | 2.2% | 0% | 0% | 1.1% | 0% | ’Parents of patients were very pleased by the overall service’ |
| Singer (2014) | NR | Questionnaire FU years later | 10% | 0 | (5%) of nubbins | 10% | NR | VAS 1–100 for function – score 89/100 |
| SAMRA (2016) GA Excision N = 2 |
NR | 1 month and 3 months1 month and 3 months | 0% | NR | NR | NR | NR | 10/10 satisfaction score Both did describe emotional distress (6/10) with having to wait |
| Macdonald (2017) | N | Telephone FU, 20 received formal survey | NR | NR | NR | NR | NR | 19/20 very high overall satisfaction. 18/20 for scar |
| Shirley (2019) | N | Telephone questionnaire | 5% | NR | NR | 5% | NR | No parent reported outcomes |
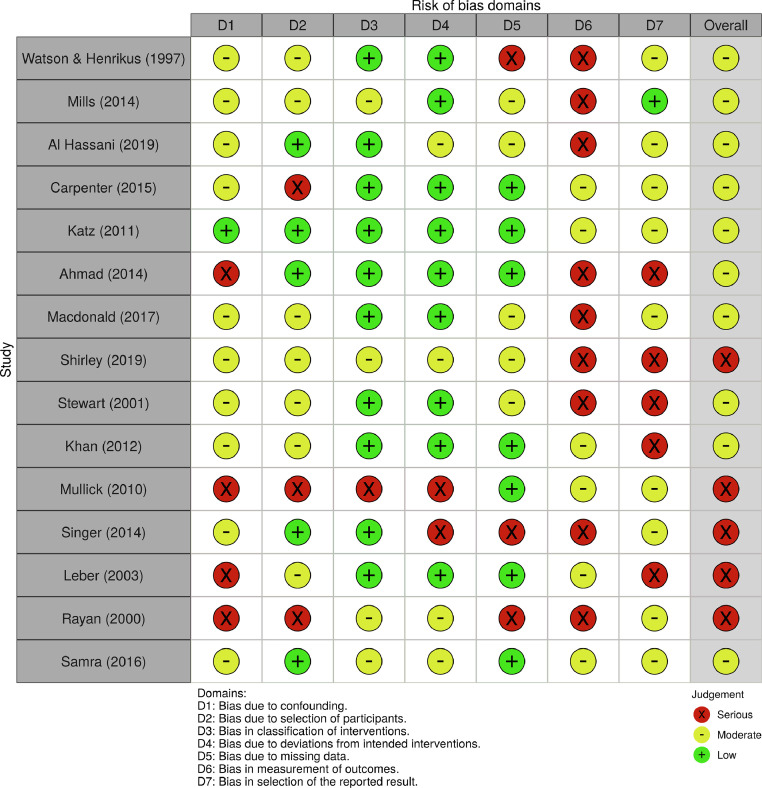
Risk of bias assessment
The risk of bias was high across included studies. Common limitations include non-consecutive inclusion of patients, incomplete or selective follow-up (with 6 studies not providing follow-up at all) and a lack of systematic analysis of outcomes. A total of 13 out of 15 included studies are case series, in which bias is inherent in participant selection, absence of comparators and retrospective reviews of notes. A more detailed breakdown of risk as determined by the ROBINS-I tool is provided in Figure 2.
Figure 2.
The summary risk of bias plot for included studies. Red = high risk; yellow = unclear risk; green = low risk.
Adverse events
The pooled prevalence of complications was 6.0% (95% CI 1, 13; Figure 3). Complications were more common following ligation procedures (22.0% [95% CI 5, 44]; I2 87%) compared to surgical excision in the outpatient setting (1.0% [95% CI 0, 8]) or operating theatre (1.0% [95% CI 0, 4] I2 0%), although there was significant heterogeneity overall (I2 74%).
Figure 3.
Forest plot showing the prevalence (%) of complications and 95% CIs. Estimates by pooled according to the method used to remove the accessory digit.
Meta-regression showed that ligation was associated with 6 times the odds of complications (OR 6.89 [95% CI 1.73, 27] p = 0.013; permuted p = 0.012) when compared with surgical excision in either a theatre or the outpatient setting. Performing the procedure in an operating theatre did not reduce the risk of complications as compared to the outpatient clinic (OR 3.75 [95% CI 0.66, 21] p = 0.114).
A funnel plot of the risk of complications against study precision showed that datapoints were strongly asymmetrical (Figure 4; Egger's regression co-efficient 0.80 [95% CI −0.69, 2.29], p = 0.246; Figure 4), which suggests the presence of small-study effects (publication bias).
Figure 4.
Funnel plot suggesting the presence of small-study effects (publication bias).
Patient (parent)-reported measures
There was insufficient data for a meta-analysis of patient-reported outcomes. Such data were available in one multi-arm study11 and four single-arm studies, and none were recognised validated measures. Samra et al. report no difference in overall satisfaction between ligation and excision groups; however, they note that infants’ perceived pain scores were higher in the suture ligation group, whilst emotional distress was higher for parents choosing excision under GA, which they attributed to the delay to intervention.11 Parental ratings of scar/cosmesis were assessed in 4 single-arm studies, and the scores were consistently high.5,6,14,18
Discussion
This systematic review and metanalysis demonstrate a paucity of high-quality studies. The available evidence suggests that suture ligation carries a clinically and statistically significant higher risk of complications than surgical excision. Studies to date suggest a higher risk of aesthetically unacceptable remnant nubbins with suture/clip ligation, compared to excision2,8; however, the reliability of this observation is questionable due to a general lack of standardised outcome measurement and follow-up across the included studies. For example, between 2.8 and 7.0% of parents requested revisional procedures for remnant nubbins, suggesting they may not be as important to parents and patients as surgeons believe.2,7,8 A digital neuroma is infrequently assessed, though one study suggests a higher incidence after suture ligation (6.7%), compared with excision (3.7%)8; however, there is insufficient data on rates of revisional surgery.
Clinic-based and operating theatre-based excision should be recognised as distinct modalities owing to procedural differences and, in some cases, implications for anaesthesia and admission. This review finds comparable rates of adverse outcomes which suggests that some of the purported disadvantages of surgical excision that relate to treatment delay, distress due to perceived stigma and concern relating to general anaesthesia may be circumvented through clinic-based excision.11,17 The approach is best tolerated in younger infants, and well-established pathways for referral are key to timely delivery.14 Theatre-based local anaesthetic excision shares these advantages but comes with greater cost and resource consumption for services.
Our review shows a paucity of the patient and parent voice in current research, with only 5 studies evaluating this using archaic instruments. A postoperative questionnaire delivered by Samra et al.11 showed that parental satisfaction was high in all three treatment arms, despite differences in specific measures such as pain scores and satisfaction with cosmetic appearance. Some studies suggest that the timing of treatment is of paramount importance to parents. Shirley et al. commented that parents often express dissatisfaction with the stigma of accessory digits,17 and Stewart et al. ascribed the high satisfaction (39/40) rates in their study (LA excision at a median age of 3 days) to early treatment.18 Parent views on anaesthetic choice are also significant and not explored in the published literature.
Validated outcome measures may improve our assessment of both objective surgical outcomes, such as scar quality and patient/parent-reported outcomes, such as overall satisfaction with treatment and appearance.21 To ensure optimal impact and relevance to patients, future comparative studies should select patient- or parent-centred primary endpoints. Patient and public involvement is an integral to this aim, specifically, in devising pertinent research questions and selecting impactful study outcomes.22 Future study design should consider that, given the strong genetic component in type B ulnar polydactyly, parental perspective may in many cases be shaped by personal experience of treatment and complications.10,15
Future studies should also consider the cost and benefits of proposed treatments. Excision under general anaesthesia is associated with increased costs. One study estimates that excision incurs a 40-fold increase in costs when compared to office-based clip application.7 Office-based excision may also offer comparative savings to services. Al-Hassani et al. reported a decrease in procedure time from 59 min in the OR to 18 min.14 This finding is not consistent across studies, however, with one study reporting operating time for local anaesthetic treatment to be 19 min.17
The optimum management of type B ulnar polydactyly is unclear based on the available evidence. Furthermore, prior studies have not been designed with patient or public involvement. There is a pressing need for a prospective observational or experimental study assessing the benefits and drawbacks of different treatment options and their cost-efficacy in the modern health service, with all relevant stakeholders involved.
Ethical approval declaration
Ethical approval was not sought for this review.
CRediT authorship contribution statement
Harsh Samarendra: Conceptualization, Formal analysis, Data curation, Investigation, Software, Writing – review & editing. Ryckie G. Wade: Conceptualization, Formal analysis, Data curation, Investigation, Software, Writing – review & editing. Louise Glanvill: Conceptualization, Formal analysis, Data curation, Investigation, Software, Writing – review & editing. Justin Wormald: Conceptualization, Formal analysis, Writing – review & editing. Abhilash Jain: Conceptualization, Formal analysis, Writing – review & editing.
Declaration of Competing Interest
The author(s) declare no potential competing of interest with respect to the research, authorship and/or publication of this article.
Funding
This work was supported by a grant (Grant code: HFR03580) from the British Society for Surgery of the Hand.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jpra.2022.05.002.
Appendix. Supplementary materials
References
- 1.Temtamy S.A., McKusick V.A. The genetics of hand malformations. Birth Defects Orig Artic Ser. 1978;14(3):i–xviii. 1-619. [PubMed] [Google Scholar]
- 2.Watson B.T., Hennrikus W.L. Postaxial type-B polydactyly. Prevalence and treatment. J Bone Joint Surg Am. 1997;79(1):65–68. doi: 10.2106/00004623-199701000-00007. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med4&NEWS=N&AN=9010187 [DOI] [PubMed] [Google Scholar]
- 3.Abzug J.M., Kozin S.H. Treatment of postaxial polydactyly type B. J Hand Surg Am. 2013;38(6):1223–1225. doi: 10.1016/j.jhsa.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Chopan M., Sayadi L., Chim H., Buchanan P.J. To tie or not to tie: a systematic review of postaxial polydactyly and outcomes of suture ligation versus surgical excision. Hand. 2018 doi: 10.1177/1558944718810885. (N Y). Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singer G., Thein S., Kraus T., Petnehazy T., Eberl R., Schmidt B. Ulnar polydactyly - an analysis of appearance and postoperative outcome. J Pediatr Surg. 2014;49(3):474–476. doi: 10.1016/j.jpedsurg.2013.06.029. [DOI] [PubMed] [Google Scholar]
- 6.Carpenter C.L., Cuellar T.A., Friel M.T. Office-based post-axial polydactyly excision in neonates, infants, and children. Plast Reconstr Surg. 2016;137(2):564–568. doi: 10.1097/01.prs.0000475787.67693.e7. [DOI] [PubMed] [Google Scholar]
- 7.Mills J.K., Ezaki M. Ulnar polydactyly: long-term outcomes and cost-effectiveness of surgical clip application in the newborn. Clin Pediatr. 2014;53(5):470–473. doi: 10.1177/0009922813514479. (Phila) [DOI] [PubMed] [Google Scholar]
- 8.Rayan G., Frey B. Ulnar polydactyly. Plast Reconstr Surg. 2001;107(6):1447–1449. doi: 10.1097/00006534-200105000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Mullick S., Borschel G.H. A selective approach to treatment of ulnar polydactyly: preventing painful neuroma and incomplete excision. Pediatr Dermatol. 2010;27(1):39–42. doi: 10.1111/j.1525-1470.2009.01071.x. [DOI] [PubMed] [Google Scholar]
- 10.Leber G.E., Gosain A.K. Surgical excision of pedunculated supernumerary digits prevents traumatic amputation neuromas. Pediatr Dermatol. 2003;20(2):108–112. doi: 10.1046/j.1525-1470.2003.20202.x. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med4&NEWS=N&AN=12657004 [DOI] [PubMed] [Google Scholar]
- 11.Samra S., Bourne D., Beckett J., Matthew M. Decision-making and management of ulnar polydactyly of the newborn: outcomes and satisfaction. J Hand Surg Asian-Pacific. 2016;21(3):313–320. doi: 10.1142/S2424835516500272. Vol. [DOI] [PubMed] [Google Scholar]
- 12.McGuinness L.A., Higgins J.P.T. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2020 doi: 10.1002/jrsm.1411. n/a(n/a) [DOI] [PubMed] [Google Scholar]
- 13.Harbord R.M., Higgins J.P.T. Meta-regression in Stata. Stata J. 2008;8(4):493–519. doi: 10.1177/1536867x0800800403. [DOI] [Google Scholar]
- 14.Al Hassani F., Nikkhah D., Pickford M.A. Correspondence and communications the management of ulnar polydactyly with a telemedicine-based referral system and a one-stop clinic. J Plast Reconstr Aesthetic Surg. 2019:1–2. doi: 10.1016/j.bjps.2019.11.024. Published online. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad Z., Park A. The milk anesthesia management of neonatal accessory digits: the 6 year coventry and warwickshire experience. JMS J Med Soc. 2014;28(3):149–153. doi: 10.4103/0972-4958.148496. [DOI] [Google Scholar]
- 16.Macdonald C.R., Kaur S., Jester A., Oestreich K., Lester R., Al-Ani S.A. Office-based postaxial polydactyly excision in neonates, infants, and children. Plast Reconstr Surg. 2017;139(1) doi: 10.1097/PRS.0000000000002873. 317e-318e. [DOI] [PubMed] [Google Scholar]
- 17.Shirley R., Pickford M. Local-anaesthetic day-case treatment of Stelling type 1 ulnar duplication in babies up to 4 months of age. J Hand Surg Eur. 2009;34(6):812–813. doi: 10.1177/1753193409337556. Vol. [DOI] [PubMed] [Google Scholar]
- 18.Stewart K.J., Holmes J.D., Kolhe P.S. Neonatal excision of minor congenital anomalies under local anaesthetic. Br J Plast Surg. 2002;55(2):170. doi: 10.1054/bjps.2001.3758. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med4&NEWS=N&AN=11987961 [DOI] [PubMed] [Google Scholar]
- 19.Khan P., Hayat H. Surgical approach for treatment of pedunculated ulnar polydactyly: our experience. Eur J Plast Surg. 2012;35(11):809–811. doi: 10.1007/s00238-012-0717-z. [DOI] [Google Scholar]
- 20.Katz K., Linder N. Postaxial type B polydactyly treated by excision in the neonatal nursery. J Pediatr Orthop. 2011;31(4):448–449. doi: 10.1097/BPO.0b013e31821addb6. [DOI] [PubMed] [Google Scholar]
- 21.Bickham R.S., Waljee J.F., Chung K.C., Adkinson J.M. Postoperative patient- and parent-reported outcomes for children with congenital hand differences: a systematic review. Plast Reconstr Surg. 2017;139(6):1422–1429. doi: 10.1097/PRS.0000000000003358. [DOI] [PubMed] [Google Scholar]
- 22.Crocker J.C., Pratt-Boyden K., Hislop J., et al. Patient and public involvement (PPI) in UK surgical trials: a survey and focus groups with stakeholders to identify practices, views, and experiences. Trials. 2019;20(1):119. doi: 10.1186/s13063-019-3183-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.