Introduction
Angiokeratomas are rare vascular skin lesions caused by the dilatation of blood vessels and skin hyperkeratosis. There are following 5 types of angiokeratomas: (1) solitary angiokeratomas; (2) angiokeratomas of the scrotum and vulva; (3) angiokeratoma corporis diffusum; (4) angiokeratoma of Mibelli; and (5) angiokeratoma circumscriptum. Angiokeratomas are caused by the dilatation of preexisting papillary blood vessels, except for the angiokeratoma circumscriptum subtype, which is caused by the malformation of capillary or capillary and lymphatic vessels.1 We report a case of acquired eruptive angiokeratomas in a previously healthy child.
Case report
A 7-year-old healthy girl presented to the dermatology outpatient clinic with a 2-week history of asymptomatic skin lesions over her right hand and wrist, with rapid progression in the number and size of the lesions. She had no previous medical problems, no fever or other symptoms, no history of physical trauma, and no contact with animals.
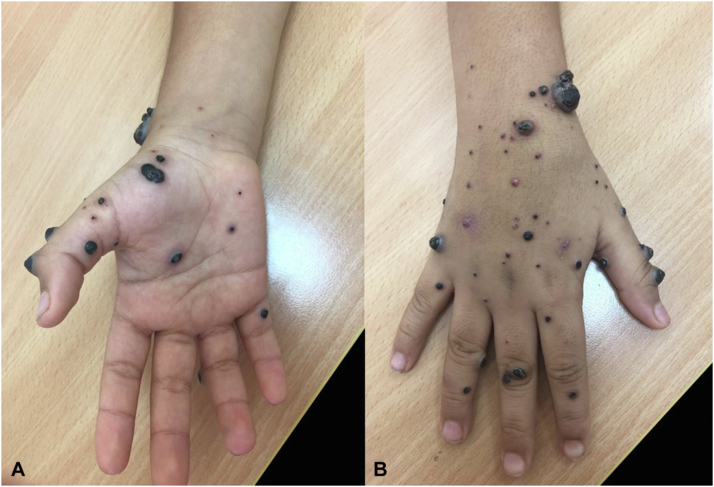
A dermatologic examination revealed multiple hyperkeratotic erythematous and dark blue nodules of varying sizes. The lesions were distributed over the palmar and dorsal aspects of the right hand, extending to the right wrist. The size of the lesions ranged from 2 × 2 mm to a maximum size of 1 × 1 cm in diameter (Fig 1).
Fig 1.
Multiple angiokeratomas over the palmar (A) and (B) dorsal aspects of the right hand.
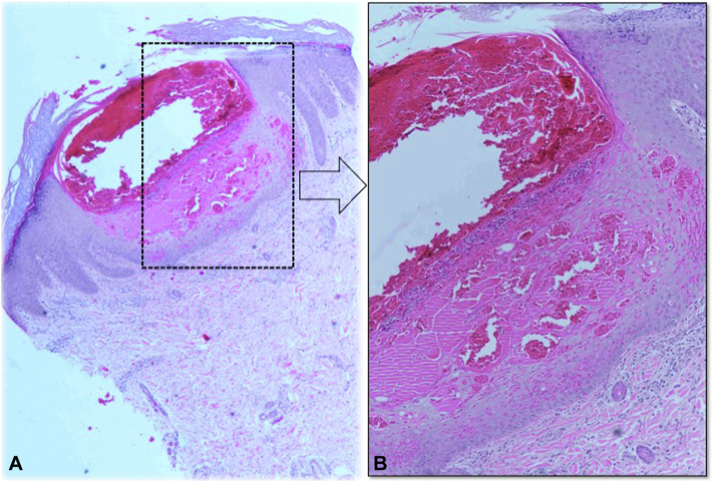
Our differential diagnoses at presentation included acquired angiokeratoma or other vascular tumors, acral pseudolymphomatous angiokeratoma of children, bacillary angiomatosis, Kaposi sarcoma, or giant molluscum contagiosum. A skin biopsy was performed on one of the well-formed lesions during the initial visit. This biopsy showed vascular ectasia of the papillary dermis extending into the epidermis with hyperkeratosis, acanthosis, and elongation of the rete ridges, with the epidermis encircling the dilated vascular spaces as shown in Fig 2. The periodic acid–Schiff and Grocott-Gomori’s methenamine silver stains were negative for microorganisms. These findings were consistent with angiokeratomas.
Fig 2.
Histopathology (hematoxylin-eosin) showing vascular ectasia of the papillary dermis, extending into the epidermis with hyperkeratosis, acanthosis, and elongation of the rete ridges with epidermis encircling the dilated vascular spaces.
Blood investigations included a complete blood cell count, liver function test, renal function test, coagulation profile, and HIV screening, all of which were normal. Initially, the condition progressed in lesion number and the size of the lesions, with bleeding secondary to the avulsion of one lesion with regrowth at the same site. She felt tenderness at the base of the thumb, involving the first metacarpophalangeal joint, which was relieved by the intake of oral analgesics.
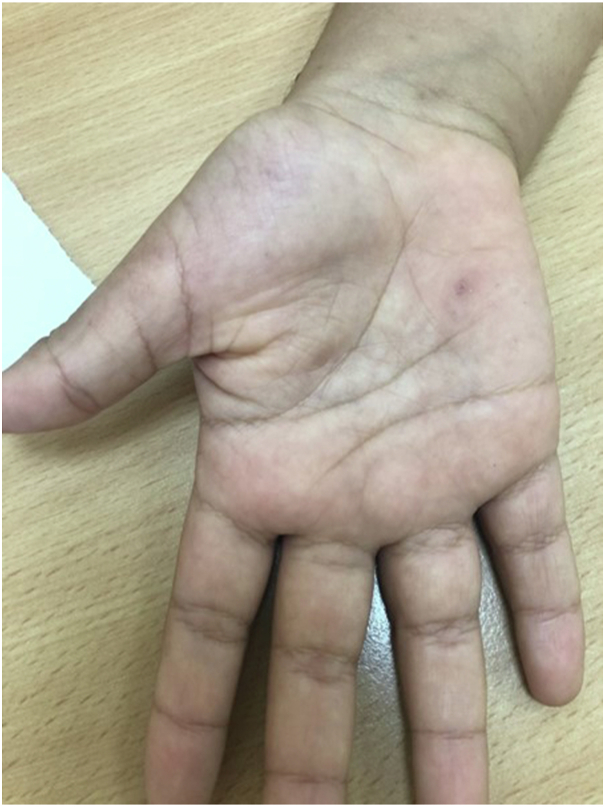
At subsequent follow-up visits, she still had the same previous lesions without progression. Cryotherapy was offered, but her parent preferred observation with no intervention, given the stability of the disease. Almost 95% of the lesions resolved spontaneously within 3 months of presentation. One small papule remained, which was treated with one session of cryotherapy. The lesions resolved completely with no recurrence after a 1-year follow-up, as shown in Fig 3.
Fig 3.
Complete clearance of lesions over the right hand after 1 year.
Discussion
Angiokeratoma is a vascular tumor that usually occurs as a solitary lesion.2 The pathogenesis of angiokeratoma remains unclear. Various factors have been considered to be the cause of angiokeratoma, such as congenital factors, nevoid or vascular malformation, tissue asphyxia, acute or chronic trauma, high venous pressure, chilblains, or pregnancy.3,4 For the patient, in this case, multiple localized angiokeratomas erupted rapidly over a short period with an unknown trigger. Acral pseudolymphomatous angiokeratoma of children may appear similarly to eruptive angiokeratomas, but the 2 entities are distinguished by histopathology. Acral pseudolymphomatous angiokeratoma presents histologically with dense inflammatory infiltrates that must be differentiated from true lymphoma by the immunohistochemical study.5 Here, acral pseudolymphomatous angiokeratoma of children was excluded by the typical changes of angiokeratoma, as seen in the histopathology.
Nearly all the known types of angiokeratomas are permanent and tend not to regress spontaneously.2 Usually, they need surgical intervention, such as electrocautery, cryotherapy, surgical excision, or laser treatment.1 The presented case is rare because the patient developed eruptive lesions without provoking factors and regressed spontaneously. The majority of reported cases with the same condition were adults who had preceding potential triggers, such as trauma, surgery, radiation, or drug-induced lesions, and nearly all of the previously reported cases required an intervention (Table I).2,6, 7, 8, 9
Table I.
Summary of reported cases of multiple eruptive angiokeratomas
|
Ref. |
Age (y) | Sex | Clinical presentation | Location | Triggering factor | Speed of onset | Treatment | Resolution |
|---|---|---|---|---|---|---|---|---|
| 6 | 56 | M | Multiple cutaneous and cerebral hemangiomas with angiokeratomas | Legs, thighs, abdomen, and chest | Unknown | Eruptive | Infrared coagulator, pulsed dye laser, curettage and cautery, intralesional interferon α-2a. | Not much benefit with reoccurrence |
| 7 | 51 | F | Multiple angiokeratomas | Left hand | Unknown | Eruptive | Electrocautery and laser therapy | Complete resolution |
| 2 | 84 | F | Eruptive overspread angiokeratomas | Hands, legs, oral mucosa | Drug, enoxaparin | Eruptive, 10 days after enoxaparin | Cessation of enoxaparin, prednisone 50 mg for 3 d | Complete resolution |
| 8 | 56 | M | Localized angiokeratoma | Left malar region | Unknown | Eruptive | Offered electrocoagulation | - |
| 9 | 21 | F | Multiple angiokeratomas | Flanks | Unknown | Eruptive | Oral and topical β-blockers | Angiokeratomas maintained at a smaller size |
This case report is an interesting occurrence of rapidly eruptive multiple angiokeratomas, localized over the right hand in a previously healthy child. To the best of our knowledge, there are no previous reports of localized acquired multiple angiokeratomas in a healthy child with spontaneous resolution. The other interesting finding in this patient was that the lesions resolved completely over 3 months without intervention. There is great importance to the early recognition and diagnosis of unusual skin lesions, to rule out a more serious differential diagnosis, such as Kaposi sarcoma, malignant melanoma, and bacillary angiomatosis, which all require early diagnosis and intervention to avoid serious consequences which could be avoided through early identification.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Bolognia J.L., Schaffer J.V., Cerroni . Dermatology. 4th ed. Elsevier; 2017. Vascular neoplasms and neoplastic-like proliferations; pp. 2020–2049. [Google Scholar]
- 2.Schliep S., Kiesewetter F., Simon M., Grupp C., Heinzerling L. Drug-induceddilemma: angiokeratomas and decreased renal function. Am J Med. 2014;127(7):598–600. doi: 10.1016/j.amjmed.2014.03.034. [DOI] [PubMed] [Google Scholar]
- 3.Jindal S.R., Chalvade P., Jerajani H.R. Late onset palmar angiokeratomacircumscriptum: an unusual presentation. Indian Dermatol Online J. 2014;5(3):320–322. doi: 10.4103/2229-5178.137790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bansal A., Gupta T. Angiokeratoma circumscriptum on the breast: a case with unusual features. Indian Dermatol Online J. 2020;11(4):655–657. doi: 10.4103/idoj.IDOJ_472_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lessa P.P., Jorge J.C.F., Ferreira F.R., de Alvarenga Lira M.L., Mandelbaum S.H. Acral pseudolymphomatous angiokeratoma: case report and literature review. An Bras Dermatol. 2013;88(6 suppl 1):39–43. doi: 10.1590/abd1806-4841.20132413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ostlere L., Hart Y., Misch K.J. Cutaneous and cerebral haemangiomas associated with eruptive angiokeratomas. Br J Dermatol. 1996;135(1):98–101. [PubMed] [Google Scholar]
- 7.Campbell T., Dimitropoulos V.A., Brown C., Jr. Successful treatment of eruptive unilateral angiokeratomas. Arch Dermatol. 2008;144(12):1663–1664. doi: 10.1001/archdermatol.2008.509. [DOI] [PubMed] [Google Scholar]
- 8.El-Azhari J., Hjira N. Acquired facial angiokeratoma. Article in French. Pan Afr Med J. 2018;30:140. doi: 10.11604/pamj.2018.30.140.14943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gandhi R., Ganatra B., Kelly A., Natkunarajah J. Treatment of eruptive angiokeratomas of the flanks with topical and oral beta-blockers. Clin Exp Dermatol. 2021;46(6):1126–1128. doi: 10.1111/ced.14660. [DOI] [PubMed] [Google Scholar]