Abstract
Purpose
To investigate the socioeconomic effect on pediatric ophthalmologists (POs) of the first year of the COVID-19 pandemic and to assess the association of practice type with financial impact.
Methods
An email follow-up survey of all AAPOS active members (POs) in April 2021, was used in conjunction with two prior surveys. The majority of US states were represented, and respondents were categorized as academic/university (AU), hospital employee (H), or one of three types of private practice: multispecialty ophthalmology practice (MSP), pediatric ophthalmology/strabismus group (PG), or solo practice (SP).
Results
The cumulative results during this one-year period revealed 1,533,203 examinations not performed, of which 498,291 were Medicaid. Over 65,000 surgeries were not performed. The average salary loss per PO was $57,188. The total loss of revenue for the pediatric ophthalmology sector was over $303,788,000. Practice groups making at least 75% of their prior year revenue were as follows: H, 81%; AU, 64%; MSP, 52%; PG, 50%; SP, 40%. Salary reduction in each group was as follows: H, 4.2%; AU, 15.4%; MSP, 17.2%; PG, 23.1%; SP, 40.9%. The average loss per practice was $290,151. More than 95% of private practice POs received funds from the Paycheck Protection Program.
Conclusions
At the one-year mark of the pandemic, patient care had been severely disrupted, with subsequent financial consequences. Private practice providers (and especially solo practices) were disproportionally negatively affected.
To assess the financial burden of COVID-19 on the pediatric ophthalmology community, an initial study1 was conducted 1 month into the lockdown in April 2020. This study of 416 pediatric ophthalmologists (POs) found surgical revenue plummeted by 82%, and clinic revenue dropped by 77%. A second study, approximately 17 weeks after the initial lockdown (July 2020), demonstrated persisting financial hardships but suggested improving trends (Robbins SL, et al. J AAPOS 2021;25:e44 [eAbstract 165], henceforth “interim study”). Both studies showed a significant reduction in surgical and clinical volumes associated with large financial losses, especially in private practice. The current study evaluates the socioeconomic standing of POs 1 year following the initial study of April 2020.
Methods
All AAPOS active members and candidates in training (CIT, ie, within 5 years of fellowship completion) were surveyed by email; 187 of 1047 surveyed members (17.9%) responded, and the 185 US member responses were used. The survey examined the one-year prior to April 18, 2021. Responses were tabulated for those who completed the necessary data for the questions provided. When response options consisted of ranges (ie, 20%-30%), the median of the range was used for analysis. The overall number of AAPOS members decreased during this one-year survey. This was thought to reflect membership nonrenewal; the original number of AAPOS members was used for all calculations.
Results were compared to current benchmarks from the American Academy of Ophthalmology AcadeMetrics for 2019.2 The two previously conducted surveys in April and July 2020 used AcadeMetrics 2018 data. The AAPOS benchmark data used in this study included the following: pediatric ophthalmology owners had a mean income of $440,683 while employed POs had a mean income of $272,324. Employed, as opposed to owner, status was used for this study, since ownership was not queried. The average, annual collections for a practice was $973,662. Annual operating expense was $519,225 (53.3%), with staffing costs of $298,789 (30.6%). The average practice had 6.5 staff per full-time equivalent (FTE). The average pediatric ophthalmology practice encountered a mean of 6,451 total patient encounters, with 1,670 new patients. The mean number of Medicaid patient visits was 2,098, accounting for 32.5% of patient encounters. A mean of 200 surgeries were performed per physician. The average collection per patient was $165.24, with average cost per patient being $97.07.
Results
A total of 185 surveys from US practitioners, representing practices in 40 states and Washington, DC, were returned: 4% from rural communities, 57% from suburban areas, and 39% from urban areas. Of these respondents, 8% were hospital employed (H), 27% were employed by university or academic centers (AU), 20% were solo private practice (SPs), 28% were employed in private, multispecialty practices (MSP), and 17% were pediatric/strabismus-only group practices (PG). Not all respondents answered every question.
Surgery Volume
At the time of the one-year follow-up, of 159 respondents, 10 (6.3%) were still not operating, 42 (26%) finished the year below 50% of pre-COVID annual surgical volume, and 7 (4.4%) performed more surgeries than before COVID; 133 (83.6%) finished below normal volume, with similar decreases across practice types.
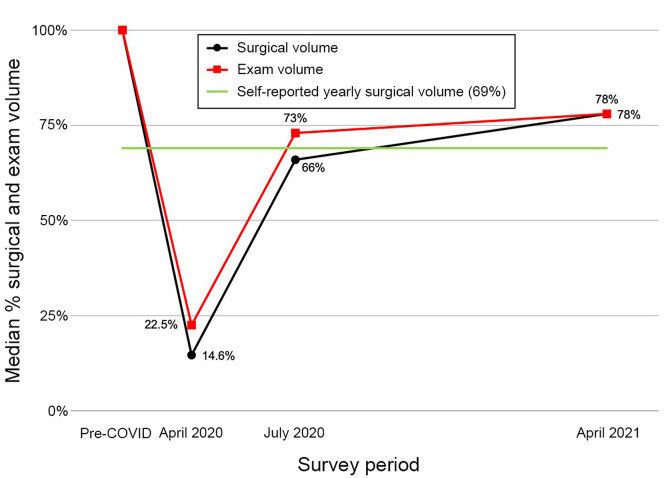
Based on previous surveys, 96% of respondents lost over 50% of their normal surgical revenue early in the pandemic1 through cancellation of elective cases. Surgical revenue in April 2020 was 14.6% of normal. The interim study showed that during July 2020 surgeries had increased to 66% of normal volume. Average surgery volume for this one-year COVID-19 period was 69% of normal (Figure 1 ), equating to approximately 65,000 surgeries not performed.
Fig 1.
Surgical and exam volume: one-year projected trend of surgical and examination volume, and actual one-year self-reported reduction of surgical volume, during COVID 19 pandemic.
For the most recent month prior to the survey (April 2021) POs reported their practices being 78% of normal surgical volume on average, with 68.6% (109/159) at a volume of ≥75% of their normal surgical volume.
Clinic Volume and Practice Revenue
Respondents were asked how their clinical examination volume (office examinations and telehealth) from the preceding 12 months compared to the 12 months before COVID-19. Examination volume improved from a low of 22.5% of normal (initial survey) to 73% (interim), to 78% (final), at which point 2 of 152 physicians (1.3%) were still not seeing patients, 11 (7.2%) had <50% of their normal annual clinical volume, 108 (67.6%) had 50%-99% of their usual volume, 23 (14%) saw the same volume, and 8 (5%) had increased volume. The mean reduction in patient volume for the year was 22.7%. Extrapolating to the entire AAPOS community, the estimated number of examinations not performed during the one-year COVID-19 period was approximately 1,533,203, including 498,291 examinations for children with Medicaid insurance. Clinical volume in the last month before the survey showed over 35% of practices at or above 100% of normal volume. At the final month of the one-year study, 21.5% of pre-COVID volume was still not being seen.
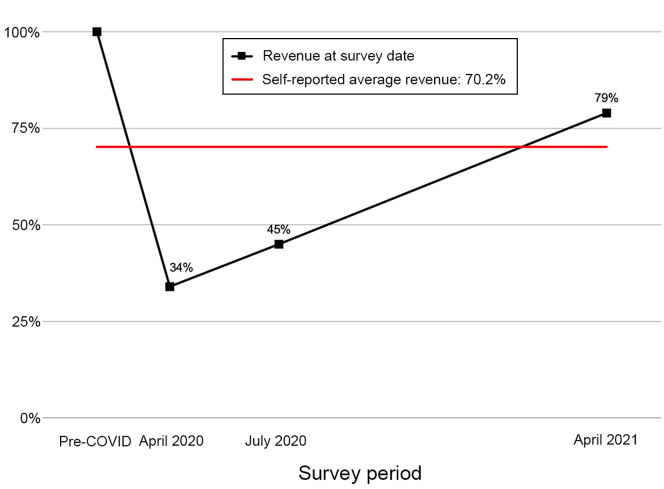
For the COVID-19 year, practice revenue decreased 29.8% compared with the prior year, equating to $248,876,175 of lost revenue for all POs. Of 159 respondents, 19 groups (11.9%) had a negligible change in revenue compared to the prior year, and 8 (5.0%) had increased revenue; 132 (83%) of all practices had a loss in revenue compared to the pre-COVID year.
Using the most recent month, gross collections and billing per month for clinical encounters (in-person and telehealth) were compared with the 12 months prior to the pandemic. Of 153 respondents, 55 (35.9%) had a negligible decrease in gross billing, 65 (42.4%) had a decrease of ≤25%. Three POs retired during the study period, and 1 closed practice. Of 149 practices, 120 (80.5%) had returned to at least 75% of their pre-COVID billing. POs lost $290,151 dollars per physician practice. This was improved from the 55% year-to-date loss of the interim study. See Figure 2 . For all AAPOS members and CITs, we can estimate a combined total loss of $303,788,097 dollars (Table 1 ).
Fig 2.
Revenue as percentage of normal: one-year projected trend of practice revenue, and one-year actual self-reported reduction of total practice revenue, during COVID 19 pandemic.
Table 1.
Reduction in care and revenue for the entire COVID-19 study period (April 2020 through April 2021)
| Study parameter | Result |
|---|---|
| Exams not performed | |
| Cumulative | 1,533,203 |
| Medicaid | 498,291 |
| Surgeries not performed | 65,000 |
| Average salary loss per AAPOS | $57,1888 |
| Total lost income all pediatric ophthalmologists | $303,788,097 |
Of practices surveyed, 138 of 159 (86.8%) had <25% decrease in staff, with 90 (56.6%) having no decrease. On average, most practices lost at most 1-2 FTE.
Of 156 respondents, 53 (34%) had no decrease in compensation, 50 (32.1%) had a 1%-20% decrease, and 53 (34%) experienced a decrease of >20% or were no longer working. For the year, 17 of 156 respondents (10.9%) lost >40% of their income. Fourteen of these 17 respondents (82%) were in private practices, which were most affected by salary loss (Table 2 ). In the final month of the study period, salaries had recovered to at least 80% of normal according to 126 of 157 respondents (80.3%) with 73 (46.5%) reporting full recovery.
Table 2.
The effect of the COVID-19 pandemic (percentages) on practice group type
| Study metrica | Hospital | Academic/university | Multispecialty practice | Pediatric group | Solo practice |
|---|---|---|---|---|---|
| Recovered to >75% of normal billing at end of study period (% of practices) | 91.6 | 87.5 | 83.7 | 74.1 | 60 |
| >20% salary decrease during COVID-19 year compared with prior year (% of practices) | 8.3 | 22.2 | 35.5 | 46.2 | 46.7 |
| % salary reduction during COVID-19 year | 4.2 | 15.4 | 17.2 | 23.1 | 40.9 |
| Current salary reduction to <70% of pre-COVID-19 during final month of 1-year period (% of practices) | 0 | 14.3 | 22.2 | 22.2 | 26.7 |
| Surgery volume <75% of amount prior to COVID-19 during 1-year period (% of practices) | 18.2 | 20.5 | 31.1 | 21.4 | 56.7 |
| Surgery volume <75% of amount prior to COVID-19 during final month of study period (% of practices) | 0 | 13.6 | 20 | 21.4 | 36.7 |
| Clinical volume <75% during study period compared with prior to COVID-19 (% of practices) | 9.1 | 27.9 | 33.3 | 34.6 | 63.3 |
| Total revenue during study period <75% of pre-COVID-19 (% of practices) | 19 | 26 | 48 | 50 | 60 |
| Current percentage revenue loss during final month of study period | 21.7 | 25.5 | 35.3 | 33.4 | 33.2 |
COVID-19 study period from April 2020 to April 2021.
Of 157 respondents who knew their practice ownership status, 15 (9.6%) were part of a private equity group: 10 of 39 MSP (25.6 %), 3 of 27 PG (11.1%), 1 of 34 SP (2.9%), 1 of 44 AU (2.3%) and 0 of 13 H (0%). Of these, 12 of 15 knew the financial status of their group. Three of 12 had lost >50% of their income for the year. This compares with approximately 18% of all respondents who had lost >50% of their income, suggesting that private equity–owned practices did not fare better.
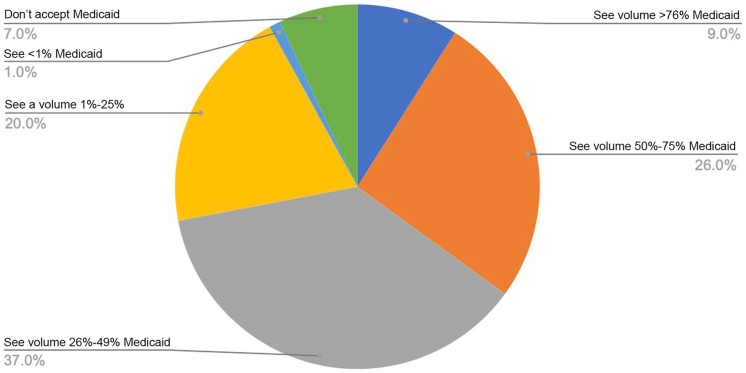
Medicaid
Prior benchmarks showed Medicaid insured patients comprising 38.7% of PO practices on average in 2018 and 32.5% in a 2019 AcadeMetrics study. In the interim study, 4% of participants reported planning on decreasing or eliminating Medicaid, and 19% were still unsure. The proportion of Medicaid patients seen in PO practices (including managed care and school community intervention partnership) is shown in Figure 3 .
Fig 3.
Pediatric ophthalmology clinical Medicaid percentages during the study period of the COVID-19 pandemic, from July 2020 interim survey.
The most recent study (April 2021) found 11 of 157 (7%) not accepting Medicaid and 4 (2.5%) retiring. Of 142 Medicaid providers, 12 (8.4%), all within private practice, had some decrease in Medicaid acceptance; 124 (79.0%) did not plan to change Medicaid acceptance. Six Medicaid providers (4.2%) reported increasing their volume. For the 2.5% of the respondents who retired or closed practice, Medicaid acceptance is unknown.
Practice Viability
The initial study showed only 8% of respondents anticipating rapid recovery, with 33% feeling their practices’ viability was in jeopardy and 10%, mainly in private practice, considering bankruptcy. At the time of the interim study, 61% of PO practices planned on limiting patient care as the practice moved forward. At that time, 3% of practices were closing, of which 5.4% were considering or had declared bankruptcy. At that time, 42% of POs felt that their future plans could include bankruptcy. In April 2021, 38.7% responded that they were “back to normal,” and practices were “financially viable,” whereas 51.0% of participants responded they were “in a good position.” Unfortunately, 8.4% of respondents still felt unsure about their day-to-day status, and 1.9% had declared or were planning on declaring bankruptcy.
Financial Support
Additional financial compensation during COVID-19 was offered through the HHS program to providers who billed for Medicare and Medicaid prior to and during COVID-19. This program had three rounds: round 1 payment was based on Medicare revenue; round 2 was available for those practices in which HHS round 1 payments were <2% of gross revenue; round 3 was offered to those who saw only Medicaid and no Medicare. Round 1 minimally benefitted POs. More than 60% of respondents did not receive any payment, 26% received <$1,000, and 36% received <$5,000. Because of administrative rollout problems, the value of round 2 could not be adequately assessed at the time of this survey. At the time of this study only 4% of POs received HHS round 3. More than 30% of respondents did not know whether their practices applied for or received any of the 3 HHS loans, the majority (approximately 52%) of those being in MSP. Specifically, more than one-third did not answer the question, and of the 150 that did, 70 (46%) were unsure if they received payment, and 26 (17.3%) received nothing. As of the time of this study, regarding HHS payments, only 1 of 54 academics reported receiving HHS payment; the remaining 53 who received payments were from private practice groups: 3 (5.7%) received $0-$500; 1 (1.9%), $501-$1,000; 10 (18.9%), $1001-$10,000; 13 (24.5%), $10,001-$25,000; 10 (18.9%), $25,001-$50,000; and 16 (30.2%), >$50,000. Payments were fairly evenly spread across MSPs, PGs, and SPs.
The PPP loan was allocated based on the “normal gross collections for the reference quarter.” Using the 2019 benchmark values indicating that the average, annual practice collects $973,662, one-quarter would equate to $243,416 PPP payment per PO. The average practice lost 29.8% of their normal revenue, or $290,151, meaning practices that received PPP payments netted estimated losses over $46,000 per PO for the year.
In the 2020 interim study only 4.6% (6/130) of H or AU respondents stated they applied for the PPP. Among private practice POs, 85% received funds. At that juncture, 91% of POs expected to reduce staff by up to 25% after PPP loan conditions had been met. The one-year data, however, showed that less than half of those surveyed (69/159 [43.3%]) had staff reductions; only 13% (21/159) had >25% reduction of staff. As of April 2021, 95.6% (86/90) of applicants had received the PPP 1 loan, with 79 having applied for loan forgiveness, 56 having received it, and 20 waiting. Three applications were denied forgiveness (all MSPs). Of loan forgiveness applicants, 92% were in private practice (83/90). Two hospital employed POs applied for the loan, received it and were forgiven. Five AU POs applied and received the loan; 3 applied for forgiveness (2 forgiven, 1 pending).
A second round of funding became available with the PPP2 loan, still in progress at the close of this study. As of that time, 59 respondents applied and 51 received the loan, 49 (86.4%) of these in private practice.
Discussion
One year into the pandemic, despite trending toward normalcy, many practices reported difficulties returning to baseline clinically and financially, with continuing backlogs of examinations and surgeries not performed, exacerbated by staffing issues.3 Private practices—particularly solo practice—were most affected in almost all regards studied (Table 2). While potential benefits of private equity practice ownership have been noted,4 such ownership did not appear to protect against loss of income. Surgery and examination volumes were about 80% of normal at the end of the year with a concurrent increase in expenses and supply-line shortages. Lockdown of outside activities along with decreased practice volumes would be expected to affect ancillary sources of income (eg, glasses dispensary, product sales, lectures/honorariums) as well. While current benchmarks show overhead in the 50%-60% range, most private practice POs experience overhead >60% (Joseph Pinto, personal communication). Ongoing practice productivity of 80% would leave little financial margin for many private practices, especially less diversified practices, and would require physicians to continue to decrease their salaries. The pandemic has exacerbated preexisting threats to the viability of SP.5 , 6
Pandemic-related practice pattern changes had a disproportionate impact on Medicaid and state-insured patients, who comprise a higher proportion of pediatric practices than most adult practices. The decision for a PO to return to patient care requires careful ethical (patient needs) and financial (practice viability) consideration. One potential mechanism utilized to decrease financial loss is to decrease the volume of Medicaid patients since, in most locales, Medicaid reimbursement rates are substantially lower than other payers or Medicare.7 Although the actual decrease in Medicaid patient acceptance turned out to be less than predicted from early surveys, most of the decrease was within private practices, who were most impacted financially by the pandemic. Trends suggest that the disproportionate strain on private practices will cause prolonged access to care issues for Medicaid patients. This is exacerbated by approximately 40% of children versus 17.8% of adults being on Medicaid.8 , 9 While resources for pediatric practices are available,10 help remains limited for pediatric ophthalmology.
While the one-year survey indicated revenue, surgical volume, and examination volumes were returning toward normal, the patient outcome implications of at least 1.5 million examinations and 65,000 surgeries not performed may not be fully understood for years. This will disproportionately impact Medicaid patients (approximately 500,000 examinations and 20,000 surgeries not performed), with ongoing stalled recovery further adding to the volume of deferred care.
Vision loss in children already results in billions of lost dollars due to long-term financial consequences throughout the life of the child,11 , 12 and the ophthalmic consequences of deferred care as a result of the pandemic will ultimately add to this burden.
This deferred or unperformed patient care and loss of income for PO (Table 1) exacerbates future delivery of care and adds additional strain to the health care system.
During COVID-19, the average loss in salary was 21.2%. This contrasts markedly with a recent compensation survey13 finding that income for general ophthalmologists was about the same in 2020 as in 2019. The difference between PO and general ophthalmologist salaries during COVID-19 may be in part be due to surgical volume. Many adult ophthalmology cases are done in surgery centers with local anesthesia, whereas much of pediatric ophthalmic surgery is hospital-based with general anesthesia and thus more vulnerable to hospitals’ limitations on surgery cases.
For PO, the burden of salary loss fell disproportionately on private practices (Table 2), especially SP (40.9% average salary loss), in spite of the fact that private practices benefitted most from PPP loans. University and hospital employed physicians are typically salaried and, while patient care was similarly affected, salary was much less affected in these groups, with ancillary staff similarly protected. Hospitals were “open for business” during the pandemic, although their models of care delivery were greatly affected. While salary is often “guaranteed” in hospital and academic practices, private practice revenue losses disproportionately affect physician salary in those practices. Unlike reduced salary findings for the whole year, the improved recovery for the final month may, in part, reflect PPP (Paycheck Protection Program), HHS (Human Health Services), or other external funding.
The 2020 interim study found that many practices furloughed or had staff hour reductions, but few laid off staff. The PPP loans obtained in many private pediatric practices required that practices retain employees. Thus, the PPP disbursement along with some of the HHS loans should have kept most practices close to their normal net revenue per year, helping to bolster salaries, preserve jobs and ensure practice viability.
Limitations of this study include the possibility of redundant data from physicians in the same practice (although most practices had only one pediatric ophthalmologist), recall bias, and the exclusion of POs who are not AAPOS members. Although the response rate was low (possibly due to short response window and survey fatigue), we believe responses to be representative of practice groups and US demographics. Our results indicate that hospitals and universities were better able to mitigate the financial impact for their POs and staff than private practices, although long-term problems may persist even for the larger employers.14 Because approximately 80% of all AAPOS members are in private practice (Christie Morse, personal communication), the plight of such practices cannot be easily dismissed. Most private practices required PPP loans, with Medicare-related loans (HHS) being much less helpful. As of April 2021, PO practices were recovering, but private practices, especially solo practices, were disproportionately affected and recovering more slowly. The PPP loan and HHS funds appear to be instrumental in preserving jobs and keeping practices viable.
AAPOS Socioeconomic Committee
Eric A. Packwood, MD, Chair; Traci Fritz, COE, Vice Chair; Robert Wendell Arnold, MD; Michael J. Bartiss, OD, MD; John E. Bishop, MD; Angela N. Buffenn, MD, MPH; Brian N. Campolattaro, MD; Christopher Gappy, MD; Jonathan Go; Richard P. Golden, MD; Charlotte Gore, MD; Joseph F. Griffith, MD; Rachael H. Jenkins, CO; Kartik S. Kumar, MD; Carolyn Lederman, MD; Eric Lichtenstein, MD (Board Liasion); Danielle M. Ledoux, MD; Stephen W. Merriam, MD; Lance M. Siegel, MD; Lisa J.T. Vredevoogd, MD.
Contributor Information
AAPOS Socioeconomic Committee:
Eric A. Packwood, Traci Fritz, Robert Wendell Arnold, Michael J. Bartiss, John E. Bishop, Angela N. Buffenn, Brian N. Campolattaro, Christopher Gappy, Jonathan Go, Richard P. Golden, Charlotte Gore, Joseph F. Griffith, Rachael H. Jenkins, Kartik S. Kumar, Carolyn Lederman, Eric Lichtenstein, Danielle M. Ledoux, Stephen W. Merriam, Lance M. Siegel, and Lisa J.T. Vredevoogd
References
- 1.Robbins S.L., Packwood E.A., Siegel L.M. The impact of COVID-19 shutdown on US pediatric ophthalmologist. J AAPOS. 2020;24:189–194. doi: 10.1016/j.jaapos.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Academy of Ophthalmology, AcadeMetrics, academetrics.aao.org. Accessed September 8, 2022.
- 3.Wohl C.Z., Pinto J.B. How can I recruit and retain staff? This challenge has only grown since the start of the pandemic. Ophthalmology Management. December 1, 2021 [Google Scholar]
- 4.Baker-Schena L. Private equity and ophthalmology. EyeNet Magazine, November. 2019:39–44. [Google Scholar]
- 5.Jagannathan M. For the first time, physicians are less likely to operate their own practices. Market Watch. May 8, 2021 [Google Scholar]
- 6.American Academy of Ophthalmology. Thriving in a solo or small practice group. https://www.aao.org/practice-management/article/thriving-in-solo-small-practice-group May 10, 2017. Accessed August 10, 2021.
- 7.Zuckerman S., Skopec L., Aarons J. Medicaid physician fees remained substantially below fees paid by Medicare in 2019. Health Aff (Millwood) 2021;40:343–348. doi: 10.1377/hlthaff.2020.00611. [DOI] [PubMed] [Google Scholar]
- 8.Suk-fong T.S., Hudak M.L., Cooley D.M., Shenkin B.N., Racine A.D. Increased Medicaid payment and participation by office-based primary care pediatricians. Pediatrics. 2018;141 doi: 10.1542/peds.2017-2570. [DOI] [PubMed] [Google Scholar]
- 9.Congressional Research Service. U.S. Health Care Coverage and Spending, IN FOCUS, Updated April 1, 2022.
- 10.American Academy of Pediatrics Resources for primary care, medical subspecialty, and surgical specialty physicians, including small business, practice management, and telehealth tips. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/help-for-pediatricians accessed May 7, 2020.
- 11.Wittenborn J.S., Zhang X., Feagan C.W., et al. Vision Cost-Effectiveness Study Group. The economic burden of vision loss and eye disorders among the United States population younger than 40 years. Ophthalmology. 2013;120:1728–1735. doi: 10.1016/j.ophtha.2013.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frick K.D., Gower E.W., Kempen J.H., et al. Wolff J.L. Economic impact of visual impairment and blindness in the United States. Arch Ophthalmol. 2007;125:544–550. doi: 10.1001/archopht.125.4.544. [DOI] [PubMed] [Google Scholar]
- 13.Martin K.L. Medscape Ophthalmologist Compensation Report. May 14, 2021 [Google Scholar]
- 14.Khuller D., Bond A.M., Schpero W.L. COVID-19 and the financial health of US hospitals. JAMA. 2020;323:2127–2128. doi: 10.1001/jama.2020.6269. [DOI] [PubMed] [Google Scholar]