Abstract
Objective
To examine the skeletal, dental, and soft-tissue cephalometric effects of class II correction using Invisalign’s mandibular advancement feature in growing patients.
Materials and Methods
A retrospective cohort clinical study was performed on cases that were started between 2017 and 2019. A total of 32 patients (13 females, 19 males), with an average age of 13 years old (9.9-14.8 years) had undergone Invisalign treatment (Align Technology, Inc., San Jose, CA) wherein the mandibular advancement phase was completed were included. Photos, digital study models, and cephalograms were taken once during the patients’ initial visit and again upon completing the mandibular advancement phase of treatment. The number of aligners worn and the time of treatment in months was recorded for each subject. Cephalometric analysis was performed and overjet and overbite were measured. Statistical analysis was performed using SPSS statistical software (version 25; SPSS, Chicago, Ill) and the level of significance was set at P <0.05. Descriptive statistics were performed to generate means and differences for each cephalometric measurement as well as patient data including age, treatment time, and aligner number. Differences between measurements from patients before treatment (T1) and after treatment (T2) with the mandibular advancement feature were evaluated using a paired t -test.
Results
All 32 patients had multiple jumps staged for the precision wings, i.e., incremental advancement. The average length of treatment for the MA phase was 9.2 months (7.5-13.8 months) and the average number of aligners used during this time was 37 (30-55). Statistically significant differences between T1 and T2, in favor of class II correction, were observed in the ANB angle, WITS appraisal, facial convexity, and mandibular length. The nasolabial angle, overjet, and overbite also showed statistically significant changes between T1 and T2.
Conclusion
Invisalign aligners with the mandibular advancement feature took approximately 9 months for 1.5 mm of overjet correction. The lower incisor angulation was maintained during class II correction. The minimal skeletal changes are in favor of class II correction.
Keywords: Aligners, Class II, Mandibular advancement, Invisalign, Digital orthodontics
INTRODUCTION
Mandibular changes can be produced by using a variety of different functional appliances.[1,2] In systematic reviews on this subject,[1,3] correction of a Class II malocclusion was found to be achieved through a combination of an increase in mandibular length and dentoalveolar changes. Invisalign has recently designed a mandibular advancement feature (MA) on their clear aligners to aid in class II correction in growing patients. MA works on a similar principle to the twin-block appliance and is composed of inclined planes positioned buccally in the posterior area of the aligners to posture the mandible forward [Figure 1].
Figure 1:
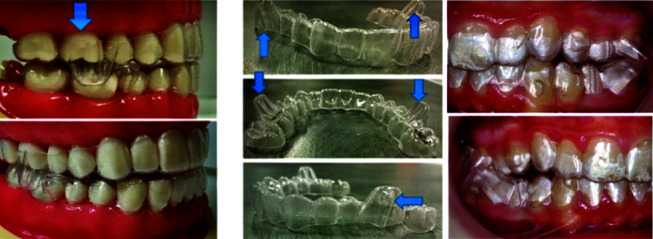
The Invisalign MA feature incorporated into the aligner.
Correct timing for the treatment of class II malocclusions is critical. The ideal time to begin treatment is around the pubertal growth spurt (i.e., CS3 and CS4 stages).[4] In any type of orthodontic treatment, patient compliance is an important consideration, particularly when using removable appliances.[1,4-7] In regards to compliance, there can be barriers and enablers for treatment.[8] Barriers to compliance can include a patient’s quality of life while using the appliance, self-motivation, and aesthetic concerns.[9-11] Oppositely, enablers can improve the degree of compliance through effective communication, increased monitoring, internal motivation, as well as improved quality of life.[12-14] The ability for patients to view their treatment plan on the ClinCheck software provides effective communication of the treatment plan. The discrete nature of the precision wings may also provide an advantage in patient comfort and aesthetics, compared to traditional appliances.[15]
However, to date, there have been very few studies to evaluate the treatment effects of the aforementioned MA feature.[16] Thus the aim of the present study was to examine the skeletal, dental and soft tissue cephalometric effects of class II correction using Invisalign’s MA feature in growing patients.
MATERIALS AND METHODS
A retrospective clinical cohort study was conducted at Bandol Rivage Clinic in France by a single experienced Diamond Plus Invisalign Provider (WS) on consecutively treated cases that were started between 2017 and 2019. Only those patients who had undergone Invisalign treatment (Align Technology, Inc., San Jose, CA) wherein the MA phase was completed were included. In total, 32 patients (13 females, 19 males) were evaluated with an average age of 13 years old (9.9-14.8 years), and who were additionally classified as CS3 or CS4 according to vertebrae analysis.
Patients were given Invisalign aligners with the MA feature (precision wings) and instructed to perform weekly aligner changes. Photos, scans, and cephalograms were taken once during the patients’ initial visit and again upon completing the MA phase of treatment. Digital study models were acquired using an iTero scanner (Align Technology, Inc., San Jose, CA). The number of aligners worn and the time of treatment in months was recorded for each subject.
Cephalometric analysis was completed using Dolphin Imaging Software (Patterson Dental, Chatsworth, CA). The measurements generated from cephalogram analysis included ANB (angle determined by points A, Nasion, and B point), Wits appraisal, convexity, mandibular length, MP-SN (angle determined by the Mandibular Plane and Sella to Nasion line), FMA (Frankfort-mandibular plane angle) (MP=FH), SNA (Angle formed by the intersection of sella-nasion and nasion- A lines), SNB (Angle formed by the intersection of sella-nasion and nasion- B lines), interincisal angle, and IMPA (Incisor mandibular plane angle). Additionally, soft tissue analysis was also performed to examine the nasolabial angle (Col-Sn-UL) and the chin angle (ID-Pg-MP). The overjet and overbite were also assessed in all patients.
Data were collected and statistical analysis was performed using Microsoft Excel 2016 (Microsoft, Redmond, WA) and SPSS statistical software (version 25; SPSS, Chicago, Ill). The level of significance was set at P < 0.05. Descriptive statistics were performed to generate means and differences (delta) for each cephalometric measurement as well as patient data including age, treatment time, and aligner number. Differences between measurements from patients before treatment (T1) and after treatment (T2) with the MA feature were evaluated using a paired t -test.
RESULTS
Thirty-two patients successfully completed the MA phase of Invisalign treatment [Table 1]. Ten patients had some alignment performed prior to the MA stage. All 30 patients had multiple jumps staged for the precision wings, i.e., incremental advancement. The average length of treatment for the MA phase was 9.2 months (7.5-13.8 months) and the average number of aligners used during this time was 37 (30-55).
Table 1:
Patient details.
| Average | Range | |
|---|---|---|
| Total | 32 | |
| Age (years) | 13 | (9.9-14.8) |
| Gender | ||
| Male | 14 | |
| Female | 18 | |
| Treatment time (months) | 9.2 | (7.5-13.8) |
| Number of aligners | 37 | (30-55) |
Statistically significant differences between T1 and T2, in favor of class II correction, were observed in the ANB angle, WITS appraisal, facial convexity, and mandibular length [Table 2]. The IMPA did not undergo changes [Table 2]. The Col-Sn-UL, overjet, and overbite also saw statistically significant changes between T1 and T2 [Table 3].
Table 2:
Cephalometric measurements in patients following treatment.
| Measure | Unit | T1 (Mean ± SD) | T2 (Mean ± SD) | Delta | Value |
|---|---|---|---|---|---|
| ANB | degrees | 5.01 ± 2.3 | 4.45 ± 2.5 | −0.55* | <0.001 |
| WITS appraisal | mm | 2.53 ± 1.9 | 1.79 ± 2.0 | −0.74* | 0.0015 |
| Convexity | degrees | 9.39 ± 6.2 | 8.07 ± 6.6 | −1.32* | <0.001 |
| Mandibular length | mm | 94.3 ± 4.8 | 95.8 ± 4.9 | 1.5* | <0.001 |
| MP-SN | degrees | 33.0 ± 5.5 | 32.6 ± 5.4 | −0.33 | 0.159 |
| FMA (MP-FH) | degrees | 23.3 ± 5.1 | 22.73 ± 4.9 | −0.57 | 0.055 |
| SNA | degrees | 80.44 ± 3.5 | 80.14 ± 3.7 | −0.31 | 0.071 |
| SNB | degrees | 75.44 ± 3.1 | 75.69 ± 3.3 | 0.25 | 0.122 |
| Interincisal angle (U1-L1) | degrees | 128.7 ± 9.0 | 130.3 ± 8.2 | 1.6 | 0.102 |
| IMPA | degrees | 97.66 ± 6.6 | 97.56 ± 6.2 | −0.11 | 0.454 |
*Statistically significant (P < 0.05)
Table 3:
Cephalometric measurements in patients following treatment.
| Measure | Unit | T1 (Mean ± SD) | T2 (Mean ± SD) | Delta | P-value |
|---|---|---|---|---|---|
| Nasolabial angle (Col-Sn-UL) | mm | 116.92 ± 8.5 | 120.68 ± 7.8 | 3.76* | 0.0011 |
| Chin angle (Id-Pg-MP) |
mm | 76.23 ± 6.1 | 75.59 ± 6.1 | −0.64 | 0.118 |
| Overjet | mm | 4.9 ± 2.0 | 3.43 ± 1.4 | −1.47* | <0.001 |
| Overbite | mm | 4.36 ± 1.4 | 3.56 ± 1.2 | −0.81* | 0.0128 |
*Statistically significant (P < 0.05)
DISCUSSION
Over the 9-month mean treatment duration, patients experienced skeletal changes in favor of class II correction, i.e., ANB, WITS, and convexity decreased, while mandibular length increased. However, these changes were relatively minor and rare reflective of the quantum of change needed in the cohort of patients treated.
The study by Caruso et al.[16] compared the MA feature to conventional twin blocks and found a 2-fold greater overjet correction in the twin-block group (3.3 mm vs 1.4 mm, respectively). This value is very similar to the present study results which showed a 1.5 mm reduction in overjet. According to Thiruvenkatachari et al. in their Cochrane review, removable functional appliances reduced the overjet on average by 4.62 mm.[17] In the current study and the study by Caruso,[16] the mean reduction in overjet was only around 1.5 mm. This may be clinically noteworthy. The mean initial overjet in this study was approximately 5 mm, which can be considered mild. The final overjet, being on average 3.5 mm, was suboptimal where overcorrection is usually performed in conventional functional appliances. However, this should be seen in the light of the total skeletal change that occurred as there was no compensatory lower incisor proclination in our study. Rarely have studies analyzing functional appliance effects reported no change in lower incisor proclination post-therapy.[3] The aligner design has probably contributed to this and is an encouraging finding that should be investigated in further studies.
The mean mandibular length increased 1.5 mm over 9.2 months. This is similar to the results demonstrated by Vaid et al. for removable functional appliances.[3] This gives a coefficient of efficiency of 0.16 mm per month. This number is comparable to the mean efficiency of functional appliances, however, this is much less compared to the Herbst fixed functional appliance (0.28 mm per month) and Twin block removable functional appliance (0.23 mm per month).[1] Due to the lack of a control group, it is impossible to determine if the observed increase was due to normal growth changes or due to the treatment performed using the MA feature in Invisalign. The average growth rate of the mandibular body length during puberty for class II patients was reported to be around 1.96 mm/year.[18] If this value is used to compare our results, it can be interpreted that the mandibular body length was not increased as a result of the treatment effect.
The ANB angle was reduced by 0.55 degrees, which is less than that mentioned by Vaid et al. in their meta-analysis.[3] In their paper, the average ANB reduction was around 2 degrees for patients treated with functional appliances. Caruso et al.[16] found an ANB reduction of -3.4 degrees using the MA feature, which contradicts our results. However, they also found a greater twin-block effect of 5.6 degrees.
One of the more commonly used class II correctors for patients desiring aligner treatment is the Carriere appliance. This appliance showed a 2.1 mm change in overjet in a study by Kim-Berman et al.[19] which is slightly greater than that of the present study results. ANB in the Carriere study was reduced by 0.8 degrees, compared to 0.55 degrees in the present study. Though the MA feature required more time, around 9 months for the class II correction, in comparison to the Carriere appliance which required only 5.2 months for the correction to occur, the key advantage of the MA feature was that the class II correction was achieved while maintaining control of the inclination of the lower incisors, which did not significantly change in angulation, compared to the Carriere appliance which caused proclination of 4.9 degrees.
The results of the current study suggest that, at this point in time, the MA feature needs to be evaluated in larger samples with a larger degree of discrepancy to make definitive conclusions on appliance efficacy and efficiency in regard to the skeletal and dental changes. The lower incisor control is an encouraging feature. In [Figures 2 and 3], cephalometric changes seen in the cohort treated with the Invisalign MA appliance.
Figure 2:
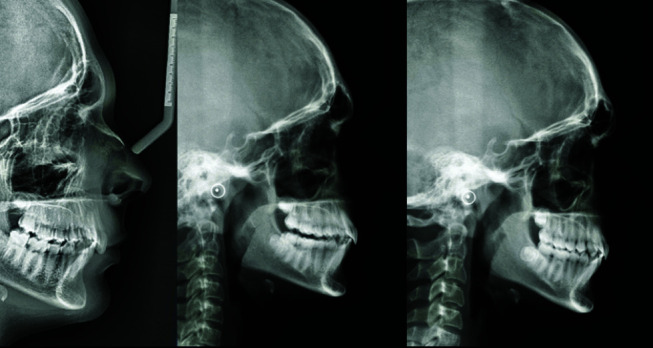
The Cephalometric changes observed in the cohort treated with Invisalign MA appliance.
Figure 3:
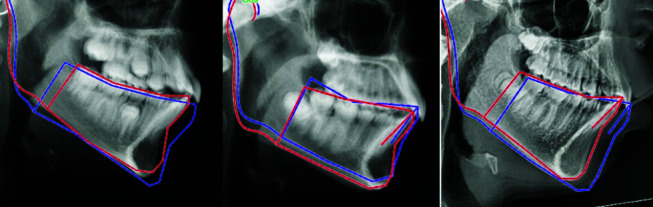
Cephalometric appraisal of mandibular changes.
LIMITATIONS
Cephalometric studies should be interpreted with caution due to the inherent limitations of a 2D projection. The retrospective nature of the study may result in selection bias. There was no control group to compare the results, so treatment changes could not be distinguished from normal growth changes. The initial overjet was mild with a mean of 5 mm.
CONCLUSION
Invisalign aligners with the MA feature took approximately 9 months for 1.5 mm of overjet correction.
The lower incisor angulation was maintained during class II correction.
There were only minor skeletal changes in favor of class II correction.
Footnotes
How to cite this article: Sabouni W, Hansa I, Al Ali SM, Adel SM, Vaid N. Invisalign treatment with mandibular advancement: A retrospective cohort cephalometric appraisal. J Clin Imaging Sci 2022;12:42.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- 1.Cozza P, Baccetti T, Franchi L, De Toffol L, McNamara JA. Mandibular changes produced by functional appliances in class II malocclusion: A systematic review. Am J Orthod Dentofac Orthop. 2006;129:599.e1–e12. doi: 10.1016/j.ajodo.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 2.Seehra J, Fleming PS, Mandall N, DiBiase AT. A comparison of two different techniques for early correction of class III malocclusion. Angle Orthod. 2012;82:96–101. doi: 10.2319/032011-197.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vaid N, Doshi V, Vandekar M. Class II treatment with functional appliances: A meta-analysis of short term treatment effects. Semin Orthod. 2014:20. doi: 10.1053/j.sodo.2014.09.008. [DOI] [Google Scholar]
- 4.Baccetti T, Franchi L, Kim LH. Effect of timing on the outcomes of 1-phase nonextraction therapy of class II malocclusion. Am J Orthod Dentofacial Orthop. 2009;136(04):501–9. doi: 10.1016/j.ajodo.2007.08.029. [DOI] [PubMed] [Google Scholar]
- 5.King EW. Treatment timing and planning in class II, division 1 malocclusions. Am J Orthod. 1964;50:4–14. doi: 10.1016/S0002-9416(64)80014-2. [DOI] [Google Scholar]
- 6.Li P, Feng J, Shen G, Zhao N. Severe class II division 1 malocclusion in an adolescent patient, treated with a novel sagittal-guidance Twin-block appliance. Am J Orthod Dentofac Orthop. 2016;150:153–66. doi: 10.1016/j.ajodo.2015.07.046. [DOI] [PubMed] [Google Scholar]
- 7.Singh GD, Clark WJ. Localization of mandibular changes in patients with class II division 1 malocclusions treated with Twin-block appliances: Finite element scaling analysis. Am J Orthod Dentofac Orthop. 2001;119:419–25. doi: 10.1067/mod.2001.113265. [DOI] [PubMed] [Google Scholar]
- 8.El-Huni A, Colonio Salazar FB, Sharma PK, Fleming PS. Understanding factors influencing compliance with removable functional appliances: A qualitative study. Am J Orthod Dentofac Orthop. 2019;155:173–81. doi: 10.1016/j.ajodo.2018.06.011. [DOI] [PubMed] [Google Scholar]
- 9.Vaid NR. Digital technologies in orthodontics- An update. Semin Orthod. 2018;24:373–5. doi: 10.1053/j.sodo.2018.10.001. [DOI] [Google Scholar]
- 10.Vaid NR, Doshi VM, Vandekar MJ. What’s “Trend”ing in orthodontic literature? APOS Trends Orthod. 2016;6:1–4. doi: 10.4103/2321-1407.173719. [DOI] [Google Scholar]
- 11.Vaid NR. The emperor's new clothes! APOS Trends Orthod. 2019;9:11–3. doi: 10.25259/APOS-9-1-1. [DOI] [Google Scholar]
- 12.Alseraidi M, Hansa I, Dhaval F, Ferguson DJ, Vaid NR. The effect of vestibular, lingual, and aligner appliances on the quality of life of adult patients during the initial stages of orthodontic treatment. Prog Orthod. 2021;22:3. doi: 10.1186/s40510-020-00346-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hansa I, Semaan SJ, Vaid NR, Ferguson DJ. Remote monitoring and “Tele-orthodontics”: Concept, scope and applications. Semin Orthod. 2018;24:470–81. doi: 10.1053/j.sodo.2018.10.011. [DOI] [Google Scholar]
- 14.Hansa I, Katyal V, Ferguson DJ, Vaid N. Outcomes of clear aligner treatment with and without dental monitoring: A retrospective cohort study. Am J Orthod Dentofac Orthop. 2021;159:1–7. doi: 10.1016/j.ajodo.2020.02.010. [DOI] [PubMed] [Google Scholar]
- 15.Zybutz T, Drummond R, Lekic M, Brownlee M. Investigation and comparison of patient experiences with removable functional appliances: Invisalign teen with mandibular advancement versus twin block. Angle Orthod. 2021;91:490–5. doi: 10.2319/050520-393.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caruso S, Nota A, Caruso S, et al. Mandibular advancement with clear aligners in the treatment of skeletal Class II. A retrospective controlled study. Eur J Paediatr Dent. 2021;22:26–30. doi: 10.23804/ejpd.2021.22.01.05. [DOI] [PubMed] [Google Scholar]
- 17.Thiruvenkatachari B, Harrison JE, Worthington HV, O’Brien KD. Orthodontic treatment for prominent upper front teeth (class II malocclusion) in children. Cochrane Database Syst Rev. 2013;2013 doi: 10.1002/14651858.CD003452.pub3. CD003452. [DOI] [PubMed] [Google Scholar]
- 18.Gomes AS, Lima EM. Mandibular growth during adolescence. Angle Orthod. 2006;76:786–90. doi: 10.1043/0003-3219(2006)076[0786:MGDA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Kim-Berman H, McNamara JA, Lints JP, McMullen C, Franchi L. Treatment effects of the Carriere Motion 3D appliance for the correction of class II malocclusion in adolescents. Angle Orthod. 2019;89:839–46. doi: 10.2319/121418-872.1. [DOI] [PMC free article] [PubMed] [Google Scholar]



