ABSTRACT
Background:
Coronavirus disease 2019 (COVID-19) was declared as a pandemic by the World Health Organization (WHO) on March 11, 2020. Researchers have evaluated many repurposed drugs for treating COVID-19 in terms of both efficacy and safety in the past several months. It has been seen that vaccination is an effective way to stop the pandemic from spreading further. Being frontline workers dealing with COVID-19 patients, the healthcare workers (HCWs) in public and private sectors were prioritized to get vaccinated first. Also, HCWs are a reliable source of information on vaccination to patients; therefore, their acceptance or otherwise of COVID-19 vaccines may influence the uptake of COVID-19 vaccine among the general population.
Methodology:
A cross-sectional study was conducted to assess the acceptance and adverse effects following the first dose of COVID-19 vaccine among HCWs of Shaheed Hasan Khan Mewati Government Medical College (SHKM GMC), a tertiary healthcare centre located in the district of Nuh Haryana.
Result:
In our study, more than half of the respondents (63.8%) experienced mild–moderate anxiety while the rest of the respondents experienced mild anxiety or moderately high levels of anxiety prior to the first dose, which is indicative of hesitancy towards the vaccine. Two-thirds of respondents in our study reported mild and common symptoms following vaccination while the remaining one-third did not report any symptom. More than half of the respondents (67.3%) claimed not taking the first dose even after two months after the initiation of vaccination drive at SHKM GMC, stating fear of some kind of reaction or side-effects, safety concerns regarding vaccine, reservations concerning the success of vaccination, and the efficiency of the vaccine.
Conclusion:
Our findings highlighted reasons for hesitancy among HCWs regarding COVID-19 vaccination along with the adverse effects encountered after the first dose. COVID-19 vaccine concerns among the HCW population should be addressed so that HCWs can be empowered to lead communication campaigns to improve COVID-19 vaccine uptake among the general population. Thus, it is important to hold such surveys.
Keywords: Acceptance, COVID-19 vaccination, health care workers, hesitation
Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), was declared as a pandemic by the World Health Organization (WHO) on March 11, 2020.[1] Since its discovery, the SARS-CoV-2 has crossed boundaries of almost more than 200 countries across the globe, affecting tens of millions of people and killing more than 1 million.[2,3] Researchers have evaluated many repurposed drugs for treating COVID-19 in terms of both efficiency and safety where few drugs have exhibited the potential to reduce mortality among the patients with COVID-19 in the past several months.[4,5,6,7] Governments globally have imposed several measures to mitigate the spread of COVID-19, such as travel bans, wearing of nose masks, lockdowns, social distance, and frequent washing of hands with soap and water, among others. However, the only way to stop the pandemic from spreading further is to create a scientifically safe and widely available COVID-19 vaccine.[8,9]
Countries all over the world are constantly working for the rapid development of COVID-19 vaccines.[10,11] Normally, vaccine development would take years and perhaps decades. Hence, the public acceptance for a new vaccine for the ongoing COVID-19 pandemic which is being developed with short period of testing remains uncertain. Thus, vaccine hesitancy may become an important challenge in the immunization against COVID-19.[12,13]
On January 16, 2021, Indian government initiated the COVID-19 vaccination drive where the National Expert Group on Vaccine Administration for COVID-19 recommended healthcare workers (HCWs) in public and private sectors to get vaccinated first as they are the frontline workers dealing with COVID-19 patients.[14] The two vaccines in India that received permission for usage were Covishield (developed by Serum Institute) is deficient adenoviral vector vaccine, and Covaxin (developed by Bharat Biotech) is an inactivated vaccine.[15,16]
A successful COVID-19 vaccine should pass potency, efficacy, and safety testing stages while being free of any adverse reaction. However, little is known about the real-world post-vaccination experience outside of clinical trial conditions. Knowledge about what to expect after vaccination will help to educate public, dispel misinformation, and reduce the vaccine hesitancy. HCWs are a reliable source of information on vaccination to patients; therefore, their acceptance of vaccines may influence the mindset of general population and can play a vital role in the success of immunization programs.[17,18,19,20,21] Family physicians and general practitioners are the first to come in contact of the general community and are the role models for them. It is imperative to assess their intentions and acceptance about COVID-19 vaccine so they can spread the message further at the grassroots level.
The present study was conducted at Shaheed Hasan Khan Mewati Government Medical College (SHKM GMC), which is the only tertiary healthcare centre situated in Nuh district of Haryana state, India. Nuh district is one of the most backward districts in India, which stands at the bottom of the National Institute of Transforming India (NITI) Aayog’s 101 backward districts in India.[22] Approximately, 80% of the population are Meo Muslims, an agrarian, cattle-rearing community and a listed backward class.[23] District Nuh in comparison to other parts of the state of Haryana has completely different sociocultural environment with strict religious beliefs and culture that have contributed towards lowest children immunization records and lowest hospital birth rate in this area.[24,25] In such scenario, where the HCWs are either residents or belong to Nuh district may get influenced by the longstanding beliefs and culture. Hence, it becomes imperative to identify the barriers that may restrict the acceptance of COVID-19 vaccine in this population. This study was conducted to assess and identify the COVID-19 vaccine acceptability among HCWs and the adverse effects faced by them post-vaccination.
Subjects and Methods
Study design and setting
A cross-sectional study was conducted to assess the acceptance and adverse effects following the administration of COVID-19 vaccine (Covishield) among the HCWs of SHKM GMC, Nuh. HCWs in this setting comprised of medical doctors, nurses, laboratory technicians, ward-boys, as well as ancillary staff, that is, administrative and sanitation workers. The vaccination drive began at SHKM GMC Nuh from 18th January 2021. Approval from the Institution’s Ethical Committee was obtained with number EC/OA- 25/2021.
Study sample
-
i- Sample Size Calculation: This was done using the following formula
- 4pq/d2;
- Where p = assumed prevalence of the outcome measure (50%)
- q = 1-p
- d = absolute error (6%)
The sufficient sample size for our study was thus calculated to be 278, and with a nonresponse rate of 5% it came out to be 293. This was rounded off to 300.
ii. Sampling Methodology: Convenient sampling method was used in this study. All HCWs who gave the consent were given a questionnaire for them to fill up and return.
Data collection tool
A self-administered questionnaire was distributed among the HCWs from January 18 to March, 2021. Forms were distributed irrespective of whether the respondents had contacted COVID-19 disease earlier or not.
First part of the questionnaire involved demographic variables of the respondents, like name, age, gender, residential address, designation, and education.
Second part of the questionnaire had reasons for not taking the vaccination; for example, if the respondent was suffering from any comorbidity or there was any contraindication known to him or her, and various other reasons like safety efficiency, side effects in the mind of the respondent, vaccination success was doubtful, and if respondents felt anxious before the vaccination.
Third part of the questionnaire consisted of responses submitted by those who had received the first dose of vaccine. Any kind of adverse effects faced post-vaccination, such as local site pain/swelling, generalized weakness, fever, chills, body ache, headache, and itching, were recorded; in addition, time of onset of symptoms, duration of continuation of symptoms, and management of the symptoms were noted.
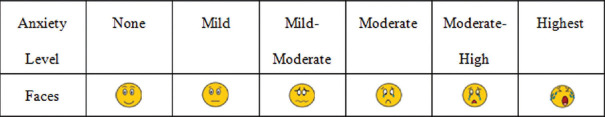
The level of anxiety faced by respondents, irrespective of their decision to take or not take the vaccine, was noted using the proposed visual anxiety scale. It is a brief scale that examiners use to assesses the facial expressions of respondents and use the facial depictions to measure the level of anxiety in respondents. The anxiety was measured at 5 levels: mild, mild–moderate, moderate, moderate–high, and high [Figure 1].[26]
Figure 1.
The proposed Visual Facial Anxiety Scale (VFAS) used to measure anxiety in respondent
Statistical/data analysis
Descriptive statistics were used to assess the baseline characteristics of data. All quantitative variables were presented as mean and standard deviation and frequency and percentages. All the data were entered in Microsoft Excel and analyzed using the statistical analytical software SPSS (version 20.00).
Results
Majority of the respondents were doctors (62%), followed by nurses (16%), technicians (7%), ward boys (12%), sanitation workers (2%), and administrative staff (1%).
Among these, 66% were male and 34% female. Only 32.7% had received vaccination while 67.3% had not taken vaccination at SHKM GMC.
The reason respondents did not take the first dose of vaccine was either they had comorbidities or had few contraindications as listed in Table 1. Many had vaccination-related concerns and fears that prevented them from taking the vaccine [Graph 1].
Table 1.
Barriers for not taking vaccine in non-vaccinated respondents
| Barriers | % |
|---|---|
| Comorbidities | |
| Diabetes mellitus | 57 |
| Hypertension | 28 |
| Asthma | 11 |
| None | 4 |
| Contraindications | |
| Pregnancy | 11 |
| Lactating mothers | 20.27 |
| Immune-suppression | 2.9 |
| Hypersensitivity | 3.5 |
| None | 61 |
Graph 1.
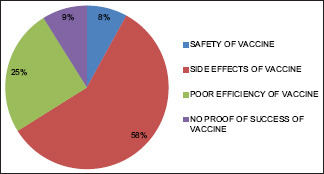
Vaccine-related concerns in non-vaccinated respondents
Anxiety in relation to vaccination was recorded using the proposed visual facial anxiety scale, irrespective of whether the respondent had taken the vaccine or not [Graph 2].
Graph 2.
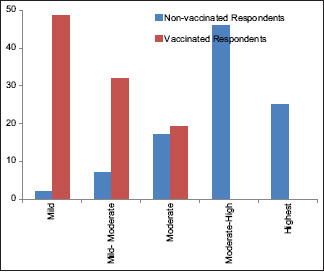
Anxiety levels in vaccinated and non-vaccinated respondents
As much as 98.2% had post-vaccination adverse effects, and the majority of them who experienced the side effects were women (67.7%); in contrast, only 32.3% of the men had such adverse effects. In addition, local pain or swelling at injection site followed by generalized weakness and so on were some of the adverse events commonly seen following immunization [Graph 3].
Graph 3.
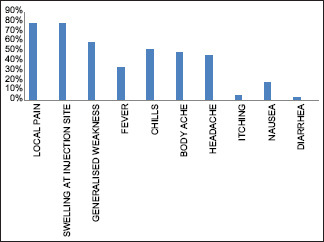
Adverse events faced by vaccinated respondents
Among those who took the vaccine, 32% experienced the symptoms within 30 minutes of getting the shot, 49% reported to have had symptoms after 24 hours, and 19% had symptoms within 48 hours or within a week.
The majority of respondents (63%) experienced adverse effects which lasted for a few hours, whereas in 28% it persisted for 1-2 days and 9% had adverse effects that lasted for 3-7 days after vaccination.
Regarding management, 67.8% respondents took no treatment, 32% took self-medication for symptoms. There were only 2.2% of respondents who had consulted the doctor on Outpatient Department (OPD) for treatment of post-vaccination adverse effects.
Discussion
This study examined the acceptability of COVID-19 vaccines among HCWs at SHKM GMC, which is the only tertiary healthcare center in district Nuh. It is often mistakenly believed that HCWs’ attitudes must be positive toward vaccines because they have scientific and medical training. Nevertheless, HCWs are not a homogenous group and most are not experts in the field of vaccination.[27]
In our study, more than half of the respondents (67.3%) had not received the vaccination, with 46% experiencing moderate to high level of anxiety and 25% experiencing the highest level of anxiety. This large percentage of non-vaccinated respondents with a high level of anxiety about vaccination is a clear indication of their hesitation towards receiving vaccination.[27]
Numerous studies by Yaqub et al., Karlsson et al., Wilson et al., and Zhu et al.[12,28,29,30] also demonstrated that hesitation about receiving vaccination exists among HCWs at prevalence and intensity levels that vary inversely with their level of training on this topic. The perception that vaccines developed in an emergency cannot be guaranteed to be safe appeared to play an important role in the acceptance of COVID-19 vaccines.
More than half of the respondents (67.3%) claimed not taking the vaccine even after 2 months of initiation of vaccination drive at SHKM GMC, Nuh, India, citing fear of some kind of reaction or side effects, safety concerns about vaccine, reservations concerning the success of vaccination, or that they did not have enough trust in the efficacy of the vaccine. Many studies conducted in France, French-speaking parts of Belgium and Canada, and the USA were in accordance with our study, and it was reported by these studies that the most common concern for vaccination among HCWs was vaccine safety, including its potential side effects. Meanwhile, there were also concerns about the efficacy and effectiveness of COVID-19 vaccine due to its rapid development.[17,21,31]
More than two-thirds of the respondents in our study reported to have had mild common symptoms post-vaccination, like pain or swelling at injection site followed by generalized weakness, chills, body ache, and headache. The post-vaccination side effects lasted for few hours in majority of respondents (63%) while in 9% it lasted for 3-7 days. The results of our study were consistent with finding of a study by Jayadevan et al.,[32] who concluded that most of the healthcare professionals who took the vaccine reported mild and short-lived post-vaccination symptoms. Tiredness, myalgia, and fever were most commonly reported. These symptoms were consistent with an immune response commonly associated with vaccines.
In our study, 66.8% respondents took no treatment while 33.2% had self-medication for symptoms. Similar results were found by Hatmal et al.[33] in Jordon, who reported that most of the participants took painkillers and stayed at home to relieve post-vaccination side effects, without the need for hospitalization, or even to consult a doctor, while only a few took only a rest at home without any medication.
Due to the fast-tracked process of vaccine development, hesitancy pertaining to COVID-19 vaccine has been a known fact. Other than misinformation and budding anxiety, many other local factors of an area, such as environmental and cultural barriers, may add up to the already existing vaccine distrust. In Nuh district, the majority population belongs to an ethnic Muslim community; other factors promoting their hesitation about receiving vaccination include the following: low level of education, lower annual income, work burden due to large family sizes, denial by elders, and traditional beliefs creating an anti-vaccination mindset (that there is no mention of vaccination in their religion) combined with a fear of impotency post-vaccination.[23,25] Since most of the HCWs at SHKM are residents of Nuh district the aforesaid factors, including especially religious beliefs, could’ve influenced them and made them suspicious about the potential adverse side effects post-vaccination and, hence, hesitant towards receiving the vaccination.
Though a large population of the country is getting vaccinated, there are residents in the Nuh district who still have received the first vaccine dose. One way to resolve this situation is to seek the help of religious leaders to disseminate messages through loudspeakers from local mosques in order to persuade people to take vaccine and increase the rate of vaccination among the people.
Thus, this study holds a great clinical significance to impart clear, accurate, and transparent information to build vaccine confidence in the community and to instil positive behaviour toward COVID-19 vaccination.
Conclusion
This cross-sectional study examined HCWs’ attitudes towards COVID-19 vaccination and related factors that would prove to be useful for public health policymakers and concerned government officials to implement effective strategies to achieve mass acceptance towards vaccination. The HCWs are the first to come into contact with the general community and are themselves like role models for them. Their recommendations are highly valued by the people at the community level. The identified barriers in this study can be utilized in tailoring the efforts and strategies to improve vaccination coverage among the general population of Nuh, the most backward district of India where the level of vaccination is still quite low.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Dhama K, Sharun K, Tiwari R, Dadar M, Malik YS, Singh KP, et al. COVID-19, an emerging coronavirus infection: Advances and prospects in designing and developing vaccines, immunotherapeutics, and therapeutics. Hum Vaccin Immunother. 2020;16:1232–8. doi: 10.1080/21645515.2020.1735227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–60. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharun K, Tiwari R, Natesan S, Yatoo MI, Malik YS, Dhama K. International travel during the COVID-19 pandemic: Implications and risks associated with ‘Travel Bubbles’. J Travel Med. 2020;27:taaa184. doi: 10.1093/jtm/taaa184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haritha CV, Sharun K, Jose B. Ebselen, a new candidate therapeutic against SARS-CoV-2. Int J Surg. 2020;84:53–6. doi: 10.1016/j.ijsu.2020.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frediansyah A, Tiwari R, Sharun K, Dhama K, Harapan H. Antivirals for COVID-19: A critical review. Clin Epidemiol Glob Health. 2021;9:90–8. doi: 10.1016/j.cegh.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharun K, Dhama K, Patel SK, Pathak M, Tiwari R, Singh BR, et al. Ivermectin, a new candidate therapeutic against SARS-CoV-2/COVID-19. Ann Clin Microbiol Antimicrob. 2020;19:23. doi: 10.1186/s12941-020-00368-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharun K, Tiwari R, Dhama J, Dhama K. Dexamethasone to combat cytokine storm in COVID-19: Clinical trials and preliminary evidence. Int J Surg. 2020;82:179–81. doi: 10.1016/j.ijsu.2020.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manning ML, Gerolamo AM, Marino MA, Hanson-Zalot ME, Pogorzelska-Maziarz M. COVID-19 vaccination readiness among nurse faculty and student nurses. Nurs Outlook. 2021;69:565–73. doi: 10.1016/j.outlook.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharun K, Tiwari R, Iqbal Yatoo M, Patel SK, Natesan S, Dhama J, et al. Antibody-based immunotherapeutics and use of convalescent plasma to counter COVID-19: Advances and prospects. Expert Opin Biol Ther. 2020;20:1033–46. doi: 10.1080/14712598.2020.1796963. [DOI] [PubMed] [Google Scholar]
- 10.Patel SK, Pathak M, Tiwari R, Yatoo MI, Malik YS, Sah R, et al. A vaccine is not too far for COVID-19. J Infect Dev Ctries. 2020;14:450–3. doi: 10.3855/jidc.12744. [DOI] [PubMed] [Google Scholar]
- 11.Yatoo MI, Hamid Z, Parray OR, Wani AH, Ul Haq A, Saxena A, et al. COVID-19-Recent advancements in identifying novel vaccine candidates and current status of upcoming SARS-CoV-2 vaccines. Hum Vaccin Immunother. 2020;16:2891–904. doi: 10.1080/21645515.2020.1788310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: A critical review. Soc Sci Med. 2014;112:1–11. doi: 10.1016/j.socscimed.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 13.Dubé E, MacDonald NE. In The Vaccine Book. Academic Press; Cambridge, MA, USA: 2016. Vaccine acceptance: Barriers, perceived risks, benefits, and irrational beliefs; pp. 507–28. [Google Scholar]
- 14.Ministry of Health and Family Welfare. National Expert Group on Vaccine Administration for Covid-19 Deliberates on Strategy to Ensure Covid-19 Vaccines Availability and its Delivery Mechanism. 2020. PIB Delhi. [Google Scholar]
- 15.Chakraborty C, Agoramoorthy G. India's cost-effective COVID-19 vaccine development initiatives. Vaccine. 2020;38:7883–4. doi: 10.1016/j.vaccine.2020.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sapkal GN, Yadav PD, Ella R. Inactivated COVID-19 vaccine BBV152/COVAXIN effectively neutralizes recently emerged B 1.1.7 variant of SARSCoV-2. J Travel Med. 2021;28:taab051. doi: 10.1093/jtm/taab051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shaw J, Stewart T, Anderson KB, Hanley S, Thomas SP, Salmon DA. Assessment of US health care personnel (HCP) attitudes towards COVID-19 vaccination in a large University health care system. Clin Infect Dis. 2021;73:1776–83. doi: 10.1093/cid/ciab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur J Epidemiol. 2020:35775–9. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verger P, Scronias D, Dauby N. Attitudes of healthcare workers towards COVID-19 vaccination: A survey in France and French-speaking parts of Belgium and Canada. Eurosurveillance. 2020;26:2000–21. doi: 10.2807/1560-7917.ES.2021.26.3.2002047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nzaji MK, Ngombe LK, Mwamba GN, Ndala DBB, Miema JM, Lungoyo CL, et al. Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo. Pragmat Obs Res. 2020;11:103–9. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shekhar R, Sheikh AB, Upadhyay S, Singh M, Kottewar S, Mir H, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. 2021;9:119. doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar A. Nuh at Bottom of Niti Aayog's 101 Most Backward Districts. [accessed on 2018 Mar 29]. Available from: https://wwwthehinducom .
- 23.Yadawar S. India's most ‘backward’ district lags in COVID vaccinations too India Spend, English Online 6 April, 2021 [Google Scholar]
- 24.Directorate of Census Operations Haryana. Census of India 2011 Haryana: Series-07: Part XII-B: District Census Handbook Mewat: Village and Town Wise Primary Census Abstract (PCA) Chandigarh: Ministry of Home Affairs, Government of India; 2011. [accessed on 2015 Jun 25]. Available from: http://censusindia.gov.in/2011census/dchb/0619_PART_B_DCHB_MEWAT.pdf . [Google Scholar]
- 25.Jain RB, Kumar A, Sharma E, Goel PK. Barriers to childhood vaccination as perceived by accredited social health activists and multipurpose health workers in Mewat, Haryana (India): A qualitative research. J Family Med Prim Care. 2020;9:4134–8. doi: 10.4103/2249-4863.293044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cao X, Yumul R, Elvir Lazo OL, Friedman J, Durra O, Zhang X, et al. A novel visual facial anxiety scale for assessing preoperative anxiety. PLoS One. 2017;12:e0171233. doi: 10.1371/journal.pone.0171233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raude J, Fressard L, Gautier A, Pulcini C, Peretti-Watel P, Verger P. Opening the ’ Vaccine Hesitancy’ black box: How trust in institutions affects French GPs’ vaccination practices. Expert Rev Vaccin. 2016;15:937–48. doi: 10.1080/14760584.2016.1184092. [DOI] [PubMed] [Google Scholar]
- 28.Karlsson LC, Lewandowsky S, Antfolk J, Salo P, Lindfelt M, Oksanen T, et al. The association between vaccination confidence, vaccination behavior, and willingness to recommend vaccines among Finnish healthcare workers. PLoS One. 2019;14:e0224330. doi: 10.1371/journal.pone.0224330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilson R, Zaytseva A, Bocquier A, Nokri A, Fressard L, Chamboredon P, et al. Vaccine hesitancy and self- vaccination behaviors among nurses in southeastern France. Vaccine. 2020;38:1144–51. doi: 10.1016/j.vaccine.2019.11.018. [DOI] [PubMed] [Google Scholar]
- 30.Zhu F-C, Guan X-H, Li Y-H, Huang J-Y, Jiang T, Hou L-H, et al. Immunogenicity and safety of a recombinant adenovirus type- 5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: A randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2020;396:479–88. doi: 10.1016/S0140-6736(20)31605-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lucia VC, Kelekar A, Afonso NM. COVID-19 vaccine hesitancy among medical students. J Public Health (Oxf) 2021;43:445–9. doi: 10.1093/pubmed/fdaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jayadevan R, Shenoy R, TS A. Survey of symptoms following COVID-19 vaccination in India. medRxiv. doi: 10.1101/2021.02.08.21251366. [Google Scholar]
- 33.Hatmal MM, Al-Hatamleh MAI, Olaimat AN, Hatmal M, Alhaj-Qasem D, Olaimat TM, et al. Side effects and perceptions following COVID-19 vaccination in Jordan: A randomized, cross-sectional study implementing machine learning for predicting severity of side effects. Vaccines. 2021;9:556–9. doi: 10.3390/vaccines9060556. [DOI] [PMC free article] [PubMed] [Google Scholar]