ABSTRACT
Background:
Countries, including India, were quick to adopt telemedicine for delivering primary care in response to the widespread disruptions due to the coronavirus disease 2019 (COVID-19) pandemic. This expeditious adoption was critical and the challenges faced during this exigency could guide the design and delivery of future telemedicine applications toward strengthening primary healthcare services.
Methods:
To identify the challenges in delivering primary care via telemedicine technology in the Indian context, a scoping review was conducted. Drawing from the systems approach in healthcare delivery, the review findings are summarized at four levels, patient, provider, healthcare organizations, and policy.
Results:
The initial search yielded 247 articles and 13 met our inclusion criteria. This review highlighted that telemedicine facilitated the continuity of care during COVID-19 but not without challenges. Low levels of education and computer literacy along with the language barriers posed the predominant challenges at the patient level. Providers had concerns related to digital literacy, clinical process flows, legal liabilities, and unethical behavior of the patients. The policy-level challenges include data privacy and security, reimbursement models, unethical behavior by the patient, or provider, and regulating prescriptions of psychotropic drugs. A lack of an integrated telehealthcare model covering diagnostics, prescriptions, and medication supply mirrored the existing fragmentation of care delivery.
Conclusion:
Telemedicine has the potential to improve primary healthcare delivery even beyond COVID-19. Currently, telemedicine applications in India are only facilitating a remote consultation wherein an integrated person-centered care is lacking. There is a need to acknowledge and factor in the inter-connectedness of health system elements for ensuring an effective and efficient healthcare delivery via telemedicine.
Keywords: Challenges, COVID-19, India, primary care, systems approach, telemedicine
Introduction
The world health organization (WHO) declared a public health emergency on March 11, 2020, and in the absence of a definitive treatment for the severe acute respiratory syndrome coronavirus 2 (SARS COV-2) virus, countries adopted preventive measures including safe distancing and face-covering while enforcing restrictive measures including lockdowns and quarantine measures.[1] These restrictive measures resulted in severe disruption of health services delivery, and in particular, covid primary health services were significantly affected, especially in low-middle income countries (LMICs) and in this context, the WHO recommended virtual consultations using telemedicine.[2] As the pandemic surged, care of COVID-19 infected patients was of utmost priority. This unprecedented demand on the healthcare delivery systems resulted in widespread panic and avoidance of health services utilization. This was more pronounced among people with chronic conditions particularly patients with non-communicable diseases (NCDs), those dependent on interventions such as dialysis, chemotherapy, and regular blood transfusions suffered the most due to the movement restrictions and repurposing of routine health services delivery for COVID-19 management.[3] Many studies have highlighted the challenges in availing treatment for chronic conditions during the COVID-19 pandemic in India.[4–6] These range from transportation issues due to lockdown, non-availability of prescribed medications, non-availability of teleconsultation slots, deferral of surgeries, loss to follow-up, among others. Early in the pandemic, recognizing the potential impact of disruptions to routine health services delivery, a shift to a virtual care delivery model became necessary, and countries across the globe started issuing guidelines for teleconsultations. The board of governors of the Medical Council of India issued Telemedicine Practice Guidelines in late March 2020, which was then ratified as a gazette notification.[7] The exigent adoption of telehealth modalities for delivering healthcare was ad hoc. The adoption of telemedicine on a large scale is a significant shift in the healthcare delivery model.[8,9,10] A primary care physician needs to be cognizant of these shifts—architectonic and far-reaching as they are potentially because of the following. There is a lack of congruence between the dangers in the future due to multiple factors, which are the mining of personally identifiable patient-specific data, the immediacy of the need of primary and tertiary care physicians to provide immediate attention to critical patients even in India’s LMIC setting, making nascent telemedicine technologies the only viable option, but finally, the use of which is compounded by the lack of overarching legal, technological, reimbursement, and medical frameworks. These multiple, overarching, and interdependent factors make for a paradigm shift that will affect patients, doctors as well as the healthcare system.[9,11,12] This is why this paper adopts a systems approach as under.
The effectiveness and efficiency of a healthcare delivery system using technology (like telemedicine) would depend upon the interactions among the interdependent elements within a broader system, which include patients, providers, the healthcare delivery system, and the environment (policy). The healthcare systems ought to be patient-centered wherein the needs and preferences of the individual patients must be factored in the design and delivery of healthcare[11,12,13] For this, the question that needs to be answered is how the system will ensure that preferences and values are factored while delivering care through telemedicine.
Further, the delivery of holistic and effective care is an integrated process and requires an understanding of the interdependencies among various healthcare system elements.[14] Thus, a systems approach is critical to understanding the challenges in delivering healthcare via information and communication technology (ICT). With this background, this study adopts a systems approach to synthesize the challenges faced in providing primary care during COVID-19 in the Indian context. A systems approach recognizes the multiplicity of elements and their interaction that affects the intended outcome.[14,15] The elements in a systems framework for healthcare delivery consist of patients, frontline healthcare providers, organization (infrastructure/resources), and environment (regulatory, market, and policy framework). These elements serve as our themes for narrative synthesis.
Methodology
A scoping review was conducted using the Arksey & O’Malley framework,[16] wherein the search strategy is guided by the study objectives. The literature review followed the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [Figure 1]. The literature search was conducted using the popular medical literature electronic database MEDLINE (through PUBMED) and SCOPUS, the largest database of peer-reviewed literature. The initial search with the identified search criteria yielded 247 articles (PUBMED = 145; SCOPUS = 102). The search included articles published up to April 2021. Thirteen articles met the inclusion criteria and were read to extract the data within the systems framework in healthcare delivery.
Figure 1.
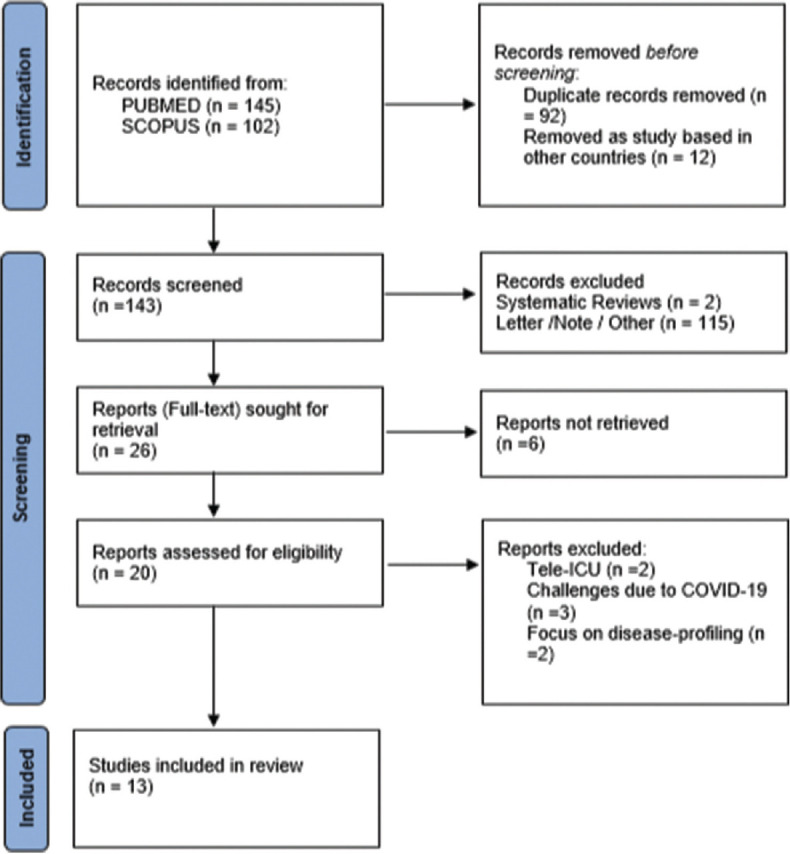
PRISMA Flow diagram depicting the selection of studies in our review
Search terms
Telehealth OR telemonitoring OR teleconsultation OR telemedicine OR telehealth OR telecare OR telepathology OR telepsychiatry OR tele-dermatology OR tele-rehabilitation) AND (“covid-19” OR “2019 novel coronavirus infection” OR “2019-nov” OR “SARS-CoV-2” OR “COVID19” OR “COVID-19 pandemic” OR “COVID19 pandemic” OR “covid 19” OR “covid 2019” OR “severe acute respiratory syndrome coronavirus 2” OR “severe acute respiratory syndrome coronavirus 2” OR “2019 ncov” OR “sars cov 2” OR “2019 ncov”) AND (“Challenges” OR “barriers” OR “concern” OR “implementation” OR “experience”) AND (“India” OR “Andhra Pradesh” OR “Arunachal Pradesh” OR “Assam” OR “Bihar” OR “Chhattisgarh” OR “Goa” OR “Gujarat” OR “Haryana” OR “Himachal Pradesh” OR “Jharkhand” OR “Karnataka” OR “Kerala” OR “Madhya Pradesh” OR “Maharashtra” OR “Manipur” OR “Meghalaya” OR “Mizoram” OR “Nagaland” OR “Odisha” OR “ Punjab” OR “Rajasthan” OR “Sikkim” OR “Tamil Nadu” OR “Telangana” OR “Tripura” OR “Uttar Pradesh” OR “Uttarakhand” OR “West Bengal” OR “Delhi”)
Inclusion criteria
Primary studies published in peer-reviewed journals on using, implementing, or evaluating telemedicine in its various modes during COVID-19 in the Indian context were included. The title and abstracts of the retrieved searches were screened for relevance to answer the study questions and to remove duplicates using the Reference Management Software, Mendeley.
Data extraction
The included studies were reviewed in full-text (N = 13) and the data were obtained regarding the healthcare organization type (tertiary hospital/clinic), hospital ownership type (public/private/non-governmental organization (NGO)), location of the hospital, and purpose for initiating the telemedicine (TM) service (primary consultation/follow-up care). As part of the analysis, we focused on the challenges faced by the patients/healthcare providers while receiving/delivering care through TM modalities. The data extraction guided by the systems approach in healthcare delivery followed four themes: issues faced by patients; providers, challenges at the level of organization; and challenges at the policy level. The findings are summarized using the narrative synthesis approach with the identified themes.
Results
The initial search yielded 247 articles through the PUBMED and SCOPUS databases. After applying our screening criteria, we identified 13 articles for the full-text review. All 13 articles were read carefully to extract the relevant information. [Table 1] provides a summary of telemedicine interventions in India during COVID-19. More than 50% of the studied interventions are from the northern region. Close to 50% of the interventions were from public hospitals. All the included studies were performed in tertiary care centers except one which was done in a private clinic in Kerala. It is worth noting that all the interventions used the WhatsApp platform either for video consultation or for sharing prescriptions.
Table 1.
Summary of the articles (telemedicine interventions) included
| Variable | Frequency/Percentage |
|---|---|
| India Region | |
| South | 4 |
| North | 6 |
| Northeast | 1 |
| West | 1 |
| East | 1 |
| Hospital Type | |
| Public | 5 |
| Private | 3 |
| NGO | 2 |
| PPP | 1 |
| Purpose | |
| Primary Consultation and Follow-up Care | 40% |
| Follow-up Cases | 60% |
| Month/Year of Publication | |
| June - August 2020 | 4 |
| September - November 2020 | 4 |
| December - February 2021 | 5 |
| WhatsApp used for consultation/ sharing prescriptions | 100% |
| Followed India’s Telemedicine Guidelines | 100% |
Table 2 provides a summary of the identified challenges or concerns. It is evident from this review that telemedicine is more acceptable for follow-up case management. Specialties like Ophthalmology find it difficult to diagnose without in-person visits.[17,18] Providers involved in long term care expressed the need for an integrated care as loss to follow-up becomes common when effective referral mechanisms are missing.[19,20] Some studies mention that patients, specifically elderly age groups, prefer face-to-face consultations.[21] A common agreement across the studies is that telemedicine can be used effectively for forward triaging, is useful in reducing the risk of infections for multi-morbidity patients, reduces crowding at the health centers, and reduces the travel cost for the patient.
Table 2.
Telemedicine initiatives and challenges or concerns
| Zone | Public/Private Hospital | Department | Main Purpose | Challenges/Concerns |
|---|---|---|---|---|
| South | Non-Profit Charitable Hospital | Cardiology | Active surveillance of already registered patients (patients on anticoagulants) [22] | Transition to virtual mode is desirable after at least two in-person visits Lab test reports need to be uploaded. Thus, patients residing in remote areas may have to travel long distances to get tests done |
| Northeast | PPP | Psychiatry | Tele-counseling for new as well as follow-up cases[23] | Difficulty getting a formal signed consent Refiling the doses without actual examination is tricky Difficult to build trust for new cases |
| South | Private Clinic | Rheumatology | Teleconsultation for primary and follow-up cases[21] | 26% of the patients preferred face-to-face visits even though as per clinicians they were eligible for teleconsultations |
| North | Public Tertiary Care Center | Ophthalmology | Teleconsultation for primary and follow-up cases[17] | 40% of the new cases required in-person visits Virtual mode is more time-consuming |
| North | Private Tertiary Care Center | Cardiology | Active surveillance of patients on anticoagulants[24] | Patients were required to visit labs for repeated testing |
| North | Public Tertiary Level | Gastroenterology | Follow-up for inflammatory bowel disease[25] | Not all patients were familiar with video consultations |
| North | Public Tertiary Level | Oncology | End-of-life care to cancer patients in terminal stage[26] | Continuous monitoring not possible |
| South | NGO (Not-for-profit) | Ophthalmology | Teleconsultation for primary and follow-up visits[18] | About 20% of the patients required in-person visits TM can act as an effective forward triage |
| North | Public | Rheumatology | Continuity of care for chronic patients[20] | The recording and reporting of outcome measures was a challenge for patients with lower education status Misinterpretation of the symptoms by the patients Voice and video quality Language barrier Incivility by patients sharing of inappropriate content Accessibility to lab services Involving other disciplines for ensuring holistic care |
| North | Public | Oncology | Palliative care for cancer patients[19] | Safety of patient data is an issue while using platforms like WhatsApp for consultations Opioids’ prescription Loss to follow-up Lack of multi-disciplinary approach |
| South | Private | All Departments | Teleconsultations for primary and follow-up visits[27] | Elderly patients prefer face-to-face consultations Computer literacy is a concern Internet connectivity |
| West | Public/Private | Psychiatry/General Physicians | Perceptions/challenges faced by physicians while delivering care for dementia through telemedicine[28] | Virtual assessment is a challenge Interrupted connections make it difficult for patients to comprehend questions Establishing therapeutic rapport with the patient is a challenge in virtual mode Physicians are concerned as there is a lack of clarity of legal implications Ensuring coordinated care (referral to other departments) was a challenge |
| East | Private Tertiary Care Hospital |
Cancer | Challenges faced by patients[4] | Non-availability of slots for teleconsultation Network connectivity Lack of guidance on accessing modes of care |
Challenges or concerns summarized using the systems approach
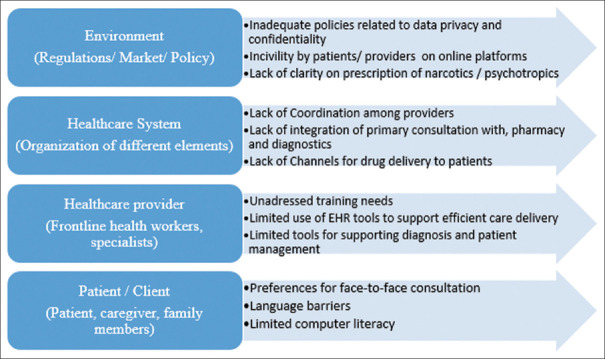
A recent review of the systems approach in healthcare design and delivery defined the systems approach as “a way of addressing health delivery challenges that recognize the multiplicity of elements interacting to impact an outcome of interest and implements processes or tools in a holistic way.”[15] Adopting the four-level model of the systems approach by Reid et al.,[14] the challenges in delivering primary healthcare via telemedicine are outlined in [Figure 2].
Figure 2.
Challenges in delivering primary care - synthesis using systems approach
At the level of the patient, preferences for face-to-face consultation, language barriers, and limited digital literacy, especially among the elderly population, are predominant challenges. For achieving an equitable healthcare system (using teleconsultation) issues related to computer literacy and language barriers must be addressed.
Providers had concerns related to the efficiency of clinical workflows when delivering remote care.
Some of the studies have highlighted that providers are not comfortable using technology for delivering care owing to risks of misdiagnosis, and the use of technology being more time-consuming relative to face-to-face consultations.[20] There is a need to address the training needs of the healthcare providers by incorporating healthcare informatics education early in their careers. The National Institute of Mental Health and Neurosciences (NIMHANS) under the Ministry of Health and Family Welfare is actively involved in promoting telepsychiatry services by training the healthcare providers in delivering remote care and issuance of telepsychiatry guidelines during the COVID-19 pandemic.[29,30] There is a need for such initiatives by other organizations as well.
Currently, TM applications are only facilitating a remote consultation with e-prescription wherein the continuity of care ranging from prevention strategies, diagnostics, delivery of prescribed medicines, and referral to other departments (if required) are missing[29,31]. There is a need to organize the health system elements such that integrated care can be ensured. The efficiency in the current practices of TM could be enhanced by ensuring that the providers are familiarized in using these technology systems, enhancing the user interface, and embedding electronic health records (EHR) that would permit tracking and measuring of outcomes including assessing for the variability of care and deviations from the standard treatment workflows. Studies from developed economies have highlighted the significance of an integrated telemedicine approach in reducing costs and improving efficiency.[32–34] An integrated system ensures timely access to patients’ records, saves time in data entry, and reduces chances of medical errors.[34]
With the adoption of new technology arises new legal and accountability issues such as data privacy, patient consent, standardization of varied applications, maintaining ethical standards both by patients and providers. All the studied interventions have used WhatsApp either for video consultation or sending prescriptions. This has implications for privacy and data security around sensitive demographic and individual patient data in the context of recent debates and increasing recognition of privacy infringements by these social media platforms.
Discussion
This scoping review focuses on telemedicine initiatives in the Indian healthcare system implemented during COVID-19. The review found that hospitals, both public and private, were quick to adopt telemedicine technology in response to the COVID-19 pandemic and delivered care via audio and video mode using the easily available platforms facilitating video calls, such as WhatsApp, Facebook, and Skype. Though providers were using social media platforms due to the emergent situation, they had concerns about patient privacy and data security while using these platforms. Thus, there is an evident need of adopting safe and secure platforms for delivering care to mitigate patients’ as well as providers’ perceived risks, thus, ensuring better acceptability and sustainability of the telemedicine platforms. Several public and private initiatives emerged in the telehealth space as the digital health ecosystem became favorable with the release of Telemedicine Practice Guidelines during the COVID-19 pandemic. Telemedicine for care delivery is not a new development but has gained momentum during the pandemic owing to lockdowns, travel restrictions, and fear of disease transmission. The longstanding concern regarding the widespread adoption of health information technologies in healthcare is linked to poor-user acceptance and stems from a lack of process reengineering to garner the efficiencies that these technologies offer. Often despite automation, several manual steps continue to co-exist, thereby, placing an additional burden on the users, which perhaps explains the slow and sluggish adoption of telemedicine for delivering care. While the COVID-19 pandemic has accelerated its uptake, the sustainability of the initiatives remains questionable. Thus, it is critical to understand the challenges faced by different stakeholders at various health system levels and adapt the systems accordingly. In recent months, governments across developing countries are expanding telemedicine service use in routine care. This review is timely and summarizes the learnings from the experience of using telemedicine for delivering primary care in a resource-constraint setting.
The Indian Government, in its efforts toward achieving universal health coverage (UHC), plans to ensure comprehensive primary healthcare through health and wellness centers (HWCs) under its flagship program, Ayushman Bharat. For addressing healthcare delivery challenges and workforce shortages, specifically in rural and remote areas, HWCs are expected to harness the potential of technology.[35] The eSanjeevani provider-to-provider program is expected to connect 150,000 HWCs via telemedicine services to specialist services. With effective implementation of telemedicine services at HWCs, the Indian Government envisages decongesting secondary-care facilities, reducing the cost of care, improving referral advice, and ensuring specialist services.[35] Before COVID-19, the focus was on provider-to-provider telemedicine application, however, the unprecedented situation created by the pandemic mandated a shift toward patient-to-provider teleconsultation, eSanjeevani out-patient department (OPD).
The issues faced by the patients in India, particularly those suffering from chronic conditions due to the COVID-19 pandemic, are well outlined in the existing literature.[6] The continuity of care was disrupted, many patients had to skip their medicines due to the non-availability of drugs, travel restrictions, and financial hardships. Teleconsultations provided a means to reach healthcare providers and ensure continuity of care. Thus, the launch of the eSanjeevani OPD during the COVID-19 pandemic by the Indian Government was critical and timely. Owing to the increased shift toward virtual consultations there is a need to continuously adapt and learn from our existing experiences. The study findings could guide the expansion of the eSanjeevani program and other telemedicine initiatives in India.
Utilizing the systems approach, this review has identified challenges at four levels in the healthcare system including the patients, healthcare providers, healthcare organization, and policy. At the policy level, data privacy and confidentiality remain pertinent issues. At present, the existing platforms are focussed on providing timely patient care. As a result of this, there is silence about the issues concerning patient data and privacy/confidentiality. One of the studies in our review highlighted the issue of incivility by patients.[20] There is a need for clear accountability frameworks for patients as well as providers for maintaining ethical standards during online consultations. At the health system level, the provision of integrated care remains a challenge. The current platforms only provide consultation with e-prescriptions sent to the patients. There was no follow-up mechanism to ensure if the patient received the drug or not. Some studies also report the abuse of e-prescriptions for drug overuse, especially psychotropic drugs.[36] At the provider level, the most frequently reported issues in delivering care via TM include difficulty in diagnosing, difficulty in utilizing the system, more time-consuming, and difficulty in building a rapport with the patient.
There is a definitive need for telemedicine services for ensuring continuity of care, however, factors affecting the acceptability, and thus, sustainability of telemedicine initiatives, require attention. The patients’ preferences for face-to-face/virtual consultation are among the major factors that could affect the quality of the physician-patient interaction, and thus, the treatment outcome. The quality of treatment or treatment outcome would also depend upon the providers’ confidence in delivering care through the TM modality. As identified in this review, many providers doubt the effectiveness of virtual diagnosis, perhaps, such concerns could be managed by ensuring sophisticated remote diagnostic tools. Moreover, training medical professionals in health informatics early on in their career path would ensure the providers’ confidence in virtual consultations. The concerns related to data security, incivility by patients, prescription of psychotropic drugs, chances of drug abuse by patients via e-prescriptions among others could be addressed by strong regulatory frameworks. Many providers also raised concerns related to lost-to-follow-up in the current TM systems as the doctors’ task ended with e-prescription. There was no follow-up mechanism to ensure if the patient received the medications or adhered to the treatment. Some studies highlighted that teleconsultations ensured consultation with the provider but the patients faced issues in getting the prescribed medicines. Perhaps an integrated system wherein the delivery of medicines is ensured with the end of consultation are required. Similarly, for remote surveillance of chronic conditions, there is a need for repeat lab tests. Teleconsultation ensured that patients were guided to undergo tests but the process afterward was not defined and patients faced challenges. Many patients were not familiar with using the online system for consultations and there is a need to identify ways to address the issues of this sub-population. Thus, a systems lens is required for ensuring effective delivery of primary care wherein the interconnected elements in the healthcare delivery system, that is, the patients, providers, healthcare system, market, and regulatory environment support each other to work toward the common goal of improved health status.
Conclusion
In the wake of the COVID-19 pandemic, healthcare providers started providing telemedicine-supported consultations for primary care and/or follow-up care in India. The current telemedicine applications are facilitating consultations with/without e-prescriptions but fall short in ensuring integrated care, a majority of the telemedicine consultations do not generate a longitudinal electronic health record. The interdependencies of different health system elements must be factored in the design of telemedicine applications for ensuring effective and efficient healthcare delivery. As India does not have a primary care led gate-keeping function to ensure the health systems’ efficiencies through risk-based triage, care cascading, and referral services, a national scale implementation of telemedicine supported primary care through the evolving Ayushman Bharat Digital Mission ecosystem provides an opportunity for policy interventions to ensure equitable and accessible health to all citizens.
Financial support and sponsorship
The study was funded by WHO SEARO under the Telehealth Enhancing Access, ensuring Continuum of care and supporting Health systems during COVID-19 pandemic in the South-East Asia Region: REACH study.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Authors would like to thank eSanjeevani development team from C-DAC Mohali, Glocal Healthcare Systems Private Ltd., Assisted Telemedicine for Rural Healthcare team for having stimulating and insightful discussions with our team.
References
- 1.World Health Organization WHO. Weekly epidemiological update-2 February 2021. WHO Rep. Published online. 2021. [Last accessed on 2021 Jun 14]. Available from:https://www.who.int/publications/m/item/weekly-epidemiological-update---2-february-2021 .
- 2.WHO. Pulse survey on continuity of essential health services during the COVID-19 pandemic. Pulse Surv Contin Essent Heal Serv Dur COVID-19 pandemic. Published online. 2020. [Last accessed on 2021 Jun 14]. Available from:https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1 .
- 3.Wold Health Organization. Results of a Rapid Assessment. 2020. [Last accessed on 2021 Jun 10]. Available from:https://www.who.int/publications/i/item/ncds-covid-rapid-assessment .
- 4.Mitra M, Basu M. A study on challenges to health care delivery faced by cancer patients in India During the COVID-19 pandemic. J Prim Care Community Health. 2020;11:2150132720942705. doi: 10.1177/2150132720942705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Subathra GN, Rajendrababu SR, Senthilkumar VA, Mani I, Udayakumar B. Impact of COVID-19 on follow-up and medication adherence in patients with glaucoma in a tertiary eye care centre in south India. Indian J Ophthalmol. 2021;69:1264–70. doi: 10.4103/ijo.IJO_164_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gummidi B, John O, Jha V. Continuum of care for non-communicable diseases during COVID-19 pandemic in rural India:A mixed methods study. J Fam Med Prim care. 2020;9:6012–7. doi: 10.4103/jfmpc.jfmpc_1805_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ministry of Health and Family Welfare, Government of India, Telemedicine Practice Guidelines, 2020. [Last accessed on 2021 Feb 10]. Available from:https://www.mohfw.gov.in/pdf/Telemedicine.pdf .
- 8.Sood SP, Bhatia JS. Development of telemedicine technology in India:“Sanjeevani” -An integated telemedicine application. J Postgrad Med. 2005;51:308–11. [PubMed] [Google Scholar]
- 9.Dash S, Aarthy R, Mohan V. Telemedicine during COVID-19 in India—A new policy and its challenges. J Public Health Policy. 2021;42:501–9. doi: 10.1057/s41271-021-00287-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ministry of Health and Family Welfare, Guidelines for Telemedicine Services in Ayushman Bharat - Health and Wellness Centres (HWCs) 2020. [Last accessed on 2021 Feb 16]. Available from:https://ab-hwc.nhp.gov.in/download/document/ecc507d177d47211fab41162b1f21271.pdf .
- 11.Chandwani RK, Dwivedi YK. Telemedicine in India:Current state, challenges and opportunities. Transform Gov People, Process Policy. doi:10.1108/TG-07-2015-0029. [Google Scholar]
- 12.Dash M, Shadangi PY, Kar S, Prusty R. A conceptual model for telemedicine adoption:An examination of technology acceptance model. Int J Recent Technol Eng. 2019;8:1286–8. [Google Scholar]
- 13.Greene SM, Tuzzio L, Cherkin D. A framework for making patient-centered care front and center. Perm J. 2012;16:49–53. doi: 10.7812/tpp/12-025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reid PP, Compton WD, Grossman JH, Fanjiang G, editors. National Academy of Engineering (US) and Institute of Medicine (US) Committee on Engineering and the Health Care System. Building a Better Delivery System:A New Engineering/Health Care Partnership. Washington (DC): National Academies Press (US); 2005. doi:10.17226/11378. [PubMed] [Google Scholar]
- 15.Komashie A, Ward J, Bashford T, Dickerson T, Kaya GK, Liu Y, et al. Systems approach to health service design, delivery and improvement:A systematic review and meta-analysis. BMJ Open. 2021;11:37667. doi: 10.1136/bmjopen-2020-037667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arksey H, O'Malley L. Scoping studies:Towards a methodological framework. Int J Soc ResMethodol Theory Pract. 2005;8:19–32. [Google Scholar]
- 17.Pandey N, Srivastava RM, Kumar G, Katiyar V, Agrawal S. Teleconsultation at a tertiary care government medical university during COVID-19 Lockdown in India-A pilot study. Indian J Ophthalmol. 2020;68:1381–4. doi: 10.4103/ijo.IJO_1658_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deshmukh AV, Badakere A, Sheth J, Bhate M, Kulkarni S, Kekunnaya R. Pivoting to teleconsultation for paediatric ophthalmology and strabismus:Our experience during COVID-19 times. Indian J Ophthalmol. 2020;68:1387–91. doi: 10.4103/ijo.IJO_1675_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Biswas S, Adhikari DS, Gupta N, Garg R, Bharti SJ, Kumar V, et al. Smartphone-based telemedicine service at palliative care unit during nationwide lockdown:Our initial experience at a tertiary care cancer hospital. Indian J Palliat Care. 2020;26:S31–5. doi: 10.4103/IJPC.IJPC_161_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Naveen R, Sundaram TG, Agarwal V, Gupta L. Teleconsultation experience with the idiopathic inflammatory myopathies:A prospective observational cohort study during the COVID-19 pandemic. Rheumatol Int. 2021;41:67–76. doi: 10.1007/s00296-020-04737-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shenoy P, Ahmed S, Paul A, Skaria TG, Joby J, Alias B. Switching to teleconsultation for rheumatology in the wake of the COVID-19 pandemic:Feasibility and patient response in India. Clin Rheumatol. 2020;39:2757–62. doi: 10.1007/s10067-020-05200-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shambu SK, B SPS, Gona OJ, Desai N, B M, Madhan R, et al. Implementation and evaluation of virtual anticoagulation clinic care to provide incessant care during COVID-19 times in an Indian tertiary care teaching hospital. Front Cardiovasc Med. 2021;8:648265. doi: 10.3389/fcvm.2021.648265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh Bhandari S, Joseph SJ, Udayasankaran JG, Konthoujam B, Shoib S, Dutta S. Telepsychiatry:A feasible means to bridge the demand-supply gaps in mental health services during and after the COVID-19 pandemic:Preliminary experiences from Sikkim State of India. Indian J Psychol Med. 2020;42:500–2. doi: 10.1177/0253717620951282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singh G, Kapoor S, Bansal V, Grewal M, Singh B, Goyal A, et al. Active surveillance with telemedicine in patients on anticoagulants during the national lockdown (COVID-19 phase) and comparison with pre-COVID-19 phase. Egypt Hear J. 2020;72:70. doi: 10.1186/s43044-020-00105-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghoshal UC, Sahu S, Biswas SN, Singh P, Chaudhary M, Ghoshal U, et al. Care of inflammatory bowel disease patients during coronavirus disease-19 pandemic using digital healthcare technology. JGH Open. 2021;5:535–41. doi: 10.1002/jgh3.12498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Biswas S, Adhikari S Das, Bhatnagar S. Integration of telemedicine for home-based end-of-life care in advanced cancer patients during nationwide lockdown:A case series. Indian J Palliat Care. 2020;26(Suppl 1):S176–8. doi: 10.4103/IJPC.IJPC_174_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.D'Souza B, Suresh Rao S, Hisham S, Shetty A, Sekaran VC, Pallagatte MC, et al. Healthcare delivery through telemedicine during the COVID-19 Pandemic:Case study from a tertiary care center in South India. Hosp Top. 2021;99:151–60. doi: 10.1080/00185868.2021.1875277. [DOI] [PubMed] [Google Scholar]
- 28.Banerjee D, Vajawat B, Varshney P, Rao TS. Perceptions, experiences, and challenges of physicians involved in dementia care during the COVID-19 Lockdown in India:A qualitative study. Front Psychiatry. 2021;11:615758. doi: 10.3389/fpsyt.2020.615758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ali F, Kamila V, Gowda MR, Srinivasa P, Gowda GS, Math SB. Setting up and providing telepsychiatry services in India. Indian J Psychol Med. 2020;42(Suppl 5):4S–10. doi: 10.1177/0253717620959783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ibrahim FA, Pahuja E, Dinakaran D, Manjunatha N, Kumar CN, Math SB. The future of telepsychiatry in India. Indian J Psychol Med. 2020;42(Suppl 5):112S–7. doi: 10.1177/0253717620959255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Agarwal D, Roy N, Panwar V, Basil A, Agarwal PM. Bringing health care closer to people–A review of various telemedicine models under the national health mission in India. Indian J Community Med. 2020;45:274–7. doi: 10.4103/ijcm.IJCM_334_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wan TTH, Lin BYJ, Ma A. Integration mechanisms and hospital efficiency in integrated health care delivery systems. J Med Syst. 2002;26:127–43. doi: 10.1023/a:1014805909707. [DOI] [PubMed] [Google Scholar]
- 33.Kvedar J, Coye MJ, Everett W. Connected health:A review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff. 2014;33:194–9. doi: 10.1377/hlthaff.2013.0992. [DOI] [PubMed] [Google Scholar]
- 34.Ghani MKA, Mostafa SA, Mustapha A, Aman H, Mohamed MA, Jaber MM. Investigating telemedicine approaches:A 10-country comparison. Int J Eng Technol. 2018;7:451–60. [Google Scholar]
- 35.NHSRC. Comprehensive Primary Health Care through Health &Wellness Centers. Operational Guidelines. 2018. [Last accessed on 4 2021 Mar 04]. Available from:https://www.nhm.gov.in/New_Updates_2018/NHM_Components/Health_System_Stregthening/Comprehensive_primary_health_care/letter/Operational_Guidelines_For_CPHC.pdf .
- 36.Sousa A De, Shrivastava A, Shah B. Telepsychiatry and telepsychotherapy:Critical issues faced by Indian patients and psychiatrists. Indian J Psychol Med. 2020;42(Suppl 5):74S–80. doi: 10.1177/0253717620960407. [DOI] [PMC free article] [PubMed] [Google Scholar]