ABSTRACT
Background:
Suicidal ideation is higher in psychiatric patients, particularly in those with depressive disorders. It tends to be a precursor to suicide attempts.
Aim:
To estimate the frequency of suicide ideation and attempts and their sociodemographic and clinical correlations among the inpatients with depressive disorders at a tertiary care center in North India.
Methods:
A cross-sectional descriptive survey was carried out among 128 participants diagnosed with depressive disorders who were admitted from September 2019 to April 2021 at a tertiary care hospital, India, using a total enumerative sampling technique. The sociodemographic and clinical data (particularly on suicide) were supplemented with the Modified Scale of Suicide Ideation (to evaluate suicidality) and the Hamilton Depression Rating Scale (for the severity of depression).
Results:
The median suicide ideation score was 11 inter quartile range (IQR: 19), and the overall mean depression score of the sample was 22.74 standard deviation (SD = 6.24). About 87% reported moderate to severe suicidal ideas. Occupation (farmer) (P < 0.01), current medications (tricyclic antidepressant) (P < 0.05), and history of suicide (P < 0.05) were significantly associated with the severity of depression. However, only a history of suicide was significantly associated with the current suicidal ideation (P < 0.05). About 48% had a history of suicide attempts, and among those who were more severely depressed, intoxicated during a suicide attempt (P < 0.01), taken precautions against being interrupted (P < 0.05), and had an intention to die (P < 0.05) had a significant association with their suicide attempts.
Conclusion:
Among hospitalized patients with depressive disorders, suicidal ideation is common. The study reiterates the importance of screening for suicide, particularly in those with more severe depression in the inpatient setting.
Keywords: Depression, inpatients, risk factors, suicide attempt, suicide ideation
Introduction
Depression is one of the most frequently diagnosed psychiatric illnesses in primary care settings and the leading cause of disability worldwide. In India, it is reported that almost one-third of the patients seeking help from health care facilities could have depression-related symptoms, and the approximate prevalence rate of mood disorders was reported to range from as low as 0.5 to as high as 78 per 1,000 population.[1] A severe form of depression causes morbidity and inpatient hospitalization. The patients who require admission are more likely to have severe socio-occupational dysfunction, low self-esteem, suicidal, and neurocognitive problems than those who can be treated on an outpatient basis. Hospitalized depressive patients also have a poor prognosis, a high rate of completed suicide, and high ongoing morbidity.[2]
Suicide is a common occurrence among those suffering from depression, and it is one of the most distressing consequences of the illness—suicide results from a person’s feelings of worthlessness, inadequacy, and hopelessness.
Suicidal ideation is a general term to describe a wide range of thoughts, wishes, or preoccupations with suicidal death.[3] It is a common occurrence in the general population and is an important stage in the suicidal process before attempting suicide. Suicidal ideation is seen to be a dangerous precursor to suicidal behavior. Suicidal ideas or thoughts are also a significant risk factor for suicide attempts.
The prevalence of suicidal ideation has been reported since the 1970s. In recent years, the prevalence of suicidal ideation has been increasing. Depending on the setting of each particular study, the 12-month prevalence has varied from 2.3 to 83%. Previous studies also suggest various risk factors for suicidal ideation.[4] Low social support, substance-use disorder, previous suicide attempts, hopelessness and sleep disturbances, and elevated inflammation are associated with suicidal ideation. Understanding the factors that predict suicidal ideation in patients with depressive disorders is also important because they predict potential attempts.[5]
Suicidal risk in psychiatric inpatients is up to 50 times higher than in the general population with notably higher suicide risk in patients with personality and affective disorders.[6,7] Suicide is regularly the first or second most everyday sentinel event reported in the US hospitals after surgery to the wrong person or body part. About 1,500 suicides occur in the inpatient units in the United States annually (one-third of them on a 15-min watch), and 200 in the United Kingdom. The inpatient suicide rates vary between 70 and 270 per 1,00,000 psychiatric admissions.[8,9] A systematic review and meta-analysis noted that a history of deliberate self-harm, hopelessness, feelings of guilt or inadequacy, depressed mood, suicidal ideas, and a family history of suicide were significantly associated with inpatient suicides. The prevalence of inpatient suicides in the Indian psychiatric hospitals was 10 in 1,00,000 admissions, and the information about inpatient suicides is scarce from India.[10]
Unlike the tertiary care specialist setting where detecting patients at higher risk for suicide is routine (though far from satisfactory), the primary care and family physicians often miss this critical aspect in their practice despite patients with mental health issues, such as suicide ideation or depression, are more likely to be seen by the primary care physicians. Furthermore, many suicide victims had documented contact with a primary care physician in the weeks leading up to their suicide.[11]
Besides, suicide is still the most prevalent psychiatric emergency. Determining the risk of suicide in someone who has expressed suicidal ideation is critical in preventing death by suicide. According to reviews, a case-finding approach based on the risk factors and conducting a suicide risk assessment in the patients being treated for depression are suitable and may uncover patients with suicidal intent and are amenable to intervention.[12,13]
Though a few studies have reported on suicides in the inpatient setting,[10,14] the literature is scant in this regard. Thus, the current study aims to estimate the frequency of suicide ideation and its sociodemographic and clinical correlates among inpatients with depressive disorders at a tertiary care center in North India.
Methods
Study design
A descriptive, cross-sectional design was adopted to determine the pattern and frequency of suicide ideation and attempts among inpatients with depressive disorders.
Setting
The present study was conducted at the inpatient General Hospital Psychiatric Unit of a tertiary care hospital in Northern India. It offers inpatient and outpatient psychiatric services. Presently, it is a 1,060-bedded general hospital with 20–25 beds allotted for psychiatry inpatients. The clinical services provided are inpatient (200–300 new admissions/year) and outpatient consultation (approximately 500–600 new consultations per annum). The treatment consists mainly of pharmacological management and psycho-educational strategies. As depressive disorders are common mental health disorders, on average, 10–12 patients with depressive disorders get admitted to the psychiatric inpatient unit per month, and typically, the inpatient hospitalization lasts for 2–4 weeks.
Participants
Assuming the prevalence of suicidal ideation among individuals with depressive disorders as 66%[15] (sample proportion 0.76), power (%) = 80, and with an absolute precision of 5 and 95% confidence level, the calculated sample size for the study was 130. All individuals with major depressive disorders (MDD) admitted to the psychiatry inpatient unit were screened between September 2019 and April 2021. Of the 145 patients assessed for eligibility, 132 patients met the inclusion criteria, out of which four patients did not consent (95% response rate). Hence, the data collected from 128 patients were considered for analysis.
The participants were included in the study if they met the following criteria: (a) International classification of disorders ICD-10 diagnostic criteria of depressive disorders of any subtype, (b) aged between 19 and 65 years, and (c) patients who were able to converse in Hindi (local language) or English. The participants were excluded if they had cognitive impairment (Abbreviated Mental Score <6), severe psychotic symptoms, acute comorbid medical or surgical conditions, mental retardation, and were admitted other than in the psychiatric ward.
Procedures and data collection
Ethical approval for the research was obtained from the Institute’s Ethics Committee (IEC) (study protocol number ECR/736/Inst/UK/2015/RR-18). Informed written consent was taken from the participants in English or Hindi (at the participant’s convenience) before starting the interview and thoroughly explaining the study’s nature. The participation was purely voluntary, and they could withdraw consent at any time. Privacy, anonymity, and confidentiality were ensured throughout the study.
Measures
After prior permission from the respective authors, the tools were translated in the local (Hindi) language and subsequently validated by psychiatry, psychiatric nursing, psychology, and bilingual (Hindi and English) language experts. A trial run of the translated tools (in Hindi) was conducted among 10 patients and necessary changes were incorporated. The information was gathered through structured interviews, which took about 10–15 minutes to complete. All the participants were subjected to the following assessment procedures:
i. Complete psychiatric examination was conducted through a semi-structured interview (including specific demographic data and suicide-related information such as the number of past suicide attempts, suicide communication, intention to die, precautions taken before the attempt, intoxication during the attempt, methods of suicide).
ii. General medical examination of the patients was performed to exclude severe physical disorders and organic brain disease.
iii. Abbreviated Mental Test was administered to rule out any cognitive impairment. The patients who had a score of 07 or less were excluded.
The following psychometric scales were administered for psychometric assessment:
a. Sociodemographic and Clinical Sheet
b. Modified Scale for Suicidal Ideation (MSSI) (Miller, 1991)
c. Hamilton Depression Rating Scale-17 (HDRS)[16]
Sociodemographic and Clinical Sheet
A range of background data was gathered to determine the representative nature of the sample. Information regarding age, gender, years of education, occupation, family income, religion, family type, and residence type was collected. The clinical parameters included age of onset of illness, history of suicide attempt(s), history of previous depressive episodes, the total duration of illness, family history of psychiatric illness, history of electroconvulsive therapy, and history of antipsychotic intake.
MSSI
The scale consists of 18 questions with scores ranging from 0 to 3. The first four items of the scale are identified as screening items (e.g., patients expressing a moderate or strong wish to die) to warrant administering the rest of the scale. To measure the severity of suicidal ideation, a total score based on the sum of all items calculated range from 0 to 54. The total scores of the MSSI classify as a 0–8 = None/Low Suicide Ideation, 9–20 = Mild/Moderate and 21+ = Severe Suicide Ideation. The concurrent validity of the MSSI has been established. The MSSI has a moderately high correlation with the Scale of Suicide Ideation (r =0.74) and a moderate correlation with the suicide item from the Beck Depression Inventory (r =0.60). The MSSI has high internal consistency, with Cronbach’s alpha coefficients ranging from. 87 to. 94 (Miller et al., 1986).[17] The tool was translated and the reliability was tested using the split-half method for the present study population. (Translated version [Hindi] of the Modified Scale of Suicide Ideation [r = 0.949].)
Hamilton Depression Rating Scale
Depression was assessed using the hamilton depression rating scale (HDRS). The tool comprises 17 items that determine the severity of the depressive symptoms. Scores between 0 and 7 are standard/no depression, 8 and 16 indicate mild depression, 17 and 23 are moderate depression, and more than 24 show severe depression. The inter-rater reliability of the hamilton depression rating scale has ranged from. 65 to. 98 (Pearson’s r). Nine of the 11 studies have reported inter-rater reliability to be above. 82. The intraclass correlation coefficients have ranged from. 46 to. 99. The Hindi version HDRS reliability for the current setting was also established using the split-half method and found to be r =0.91.
Data analysis
The data were collected, cleaned, entered, and then, analyzed. A professional statistician examined the data using the Stata software, version 13. The data are reported as mean (SD) and percentages for continuous and categorical variables. The association is explored by the Kruskal–Wallis test, Mann–Whitney U test, independent t-test, and analysis of variance. The results were considered significant when the P value was less than 5% (P < 0.05) (Armitage, 1998).[18]
Results
Table 1 shows the sociodemographics of the sample and their association with suicidal ideation (MSSI score) and depression (HDRS Score) at the baseline. Most of the participants were younger than 40 years of age (55.5%), males (65.6%), Hindus (87.5%), and married (55.5%). Approximately, equal representation of those less than primary educated (35.9%) and graduates (38.3%). Most participants were from a rural background (53%), living in a nuclear family (67%). About half of the participants were employed, homemakers, or students and earning < Rs. 10,000/month.
Table 1.
Sociodemographics of the sample and their association with suicidal ideation (MSSI Score) and severity of depression (HDRS Score) at baseline (n=128)
| Sociodemographic variables | n (%) | MSSI Score | HDRS Score | ||
|---|---|---|---|---|---|
|
|
|
||||
| Median (q1, q3) | U/H | Mean (SD) | t/F | ||
| Age | |||||
| <=40 years | 71 (55.5) | 9 (0,19) | -1.43 | 23.3 (6.2) | 1.18 |
| >40 years | 57 (44.5) | 12 (5, 19) | 22.0 (6.3) | ||
| Gender | |||||
| Male | 84 (65.6) | 11.5 (0, 21) | 1.00 | 22.3 (6.0) | -1.15 |
| Female | 44 (34.4) | 10.5 (1.5, 13) | 23.6 (6.6) | ||
| Religion | |||||
| Hindu | 112 (87.5) | 11 (0, 19.5) | -0.53 | 22.5 (6.3) | -0.99 |
| Muslim | 16 (12.5) | 11 (9, 14.5) | 24.2 (5.7) | ||
| Marital status | |||||
| Single | 47 (36.7) | 8 (0, 16) | 2.10 | 22.3 (6.9) | 1.43 |
| Married | 71 (55.5) | 12 (4, 20) | 22.6 (6.0) | ||
| Widow/Separated/Divorced | 10 (07.8) | 9.5 (4, 15) | 25.9 (3.7) | ||
| Education | |||||
| No formal/primary education | 46 (35.9) | 10.5 (8, 13) | 0.55 | 22.0 (5.9) | 0.66 |
| Secondary education | 33 (25.8) | 11 (0, 20) | 22.8 (5.9) | ||
| Graduation and others | 49 (38.3) | 10 (0, 19) | 23.4 (6.8) | ||
| Residence | |||||
| Rural | 68 (53.1) | 12 (1.5, 20.5) | 0.93 | 22.5 (5.6) | -0.41 |
| Urban | 60 (46.9) | 10 (0, 18.5) | 23.0 (6.9) | ||
| Type of family | |||||
| Nuclear | 86 (67.2) | 11 (0, 20) | 0.09 | 22.6 (6.7) | -0.30 |
| Joint | 42 (32.8) | 10.5 (4, 19) | 23.0 (5.1) | ||
| Occupation | |||||
| Unemployed | 25 (19.5) | 8 (0, 16) | 3.54 | 20.7±7.0 | 3.55** |
| Student/Housewife | 38 (29.7) | 11 (0, 16) | 23.1±7.1 | ||
| Farmer | 19 (14.8) | 14 (4, 23) | 25.8±3.9 | ||
| Business/Private Job | 33 (25.8) | 10 (0, 19) | 23.6±5.2 | ||
| Government Service | 13 (10.2) | 9 (0, 19) | 18.8±4.5 | ||
| Income | |||||
| <Rs. 5000/- | 32 (25.0) | 9.5 (2, 19.5) | 2.29 | 21.7 (6.3) | 0.56 |
| Rs. 5000-10000 | 33 (25.8) | 12 (4, 20) | 22.5 (6.2) | ||
| Rs. 10001-20000 | 27 (21.1) | 12 (0, 20) | 23.7 (6.1) | ||
| >20,000 | 36 (28.1) | 8 (0, 16) | 23.2 (6.4) | ||
MMSI: Modified Scale for Suicidal Ideation, HDRS: Hamilton Depression Rating Scale, *P<0.05
The overall median score on MSSI was 11 (Q1 = 0, Q3 = 19). In comparing the MSSI score among the various categories of sociodemographic variables, no significant relationship was observed. Similarly, the overall mean HDRS Score of the sample was 22.74 (SD = 6.24). On a similar comparison of the HDRS scores among the various categories of sociodemographic variables, occupation showed a significant relationship. On post hoc analysis, farmers were significantly more depressed than those in the government service.
About half the participants had a severe level of suicidal ideation as well as depression. Furthermore, about 86.7% had moderate to severe suicidal ideation [Figure 1].
Figure 1.
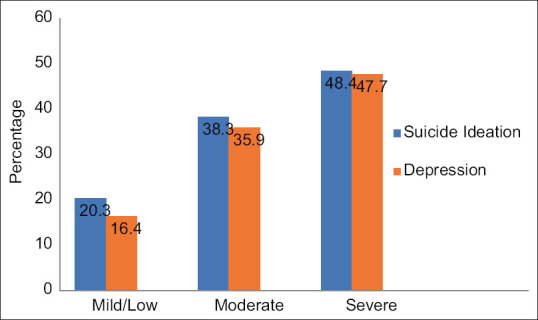
Level of suicide ideation and depression
Table 2 shows the clinical parameters of the sample and their association with suicidal ideation (MSSI score) and depression (HDRS Score) at the baseline. The majority of the study participants had their onset of illness before 30 years of age (58.6%), and about an equal number of participants had a duration of illness for 1 month, 1–3 months, and more than 3 months. About 48% of the participants had attempted suicide before. The majority of the participants had previous episodes of depression (63%), but about 39% had more than four past depressive episodes. Medications were the primary treatment modality in the past for the majority (83%). The majority of the participants (53%) were treated with selective serotonin reuptake inhibitors (SSRI) at the time of the study, and about 90% of them never had or were currently receiving electroconvulsive therapy. There were no comorbid disorders in the majority (77%), while the common comorbidities were sleep-related disorders, headache, somatization disorders, borderline personality disorder, and bipolar affective disorders. Most patients said they had no family history of mental illness (94%).
Table 2.
Distribution of clinical variables of the sample and their association with suicidal ideation (MSSI Score) and severity of depression (HDRS Score) at baseline (n=128)
| Clinical variables | n (%) | MSSI Score | HDRS Score | ||
|---|---|---|---|---|---|
|
|
|
||||
| Median (q1, q3) | U/H | Mean (SD) | t/F | ||
| Age of onset | |||||
| ≤30 years | 75 (58.6) | 9 (0, 17) | -1.71 | 23.1 (6.3) | 0.67 |
| >30 years | 53 (41.4) | 12 (4, 20) | 22.3 (6.2) | ||
| Duration of the present episode | |||||
| <4 weeks | 45 (35.2) | 12 (0, 19) | 0.03 | 21.8 (5.6) | 0.72 |
| 4-12 weeks | 42 (32.8) | 10 (0, 21) | 23.2 (6.8) | ||
| >12 weeks | 41 (32.0) | 10 (0, 19) | 23.2 (6.3) | ||
| History of suicide | |||||
| No | 66 (51.6) | 8.5 (0, 17) | -2.06* | 21.5 (5.7) | -2.31* |
| Yes | 62 (48.4) | 12 (4, 21) | 24.0 (6.6) | ||
| History of depression | |||||
| No | 48 (37.5) | 5.5 (0, 19) | -1.35 | 22.9 (5.9) | 0.24 |
| Yes | 80 (62.5) | 12 (2, 19.5) | 22.6 (6.5) | ||
| Number of past depressive episodes/year | |||||
| <4 | 49 (61.3) | 12 (4, 21) | 0.34 | 22.8 (6.1) | 0.31 |
| ≥4 | 31 (38.7) | 11 (0, 19) | 22.4 (7.1) | ||
| Mode of past treatment | |||||
| Medications only | 66 (82.5) | 12 (6, 19) | 0.98 | 22.6 (6.0) | -0.23 |
| Medications and alternative therapy | 14 (17.5) | 9 (0, 21) | 23.0 (8.6) | ||
| Present medications | |||||
| SSRIs | 68 (53.1) | 11.5 (0, 18.5) | 0.82 | 21.5 (6.1) | 3.86* |
| TCAs alone | 35 (27.3) | 11 (0, 21) | 25 (6.4) | ||
| Antianxiety drugs/Others | 25 (19.6) | 9 (1, 13) | 23.0 (5.7) | ||
| Presence of comorbidity | |||||
| No | 99 (77.3) | 11 (3, 20) | 1.38 | 22.5 (6.0) | -0.96 |
| Yes | 29 (22.7) | 7 (0, 14) | 23.7 (6.9) | ||
| No. of previous psychiatric hospitalizations | |||||
| Nil | 76 (59.4) | 11 (0, 19) | 1.92 | 22.7 (5.9) | 0.42 |
| ≤2 times | 42 (32.8) | 12 (5, 21) | 22.4 (6.7) | ||
| >2 times | 10 (07.8) | 8.5 (0, 12) | 24.4 (6.7) | ||
| History of ECT | |||||
| No | 115 (89.8) | 11 (0, 19) | 0.26 | 22.9 (6.3) | 1.02 |
| Yes | 13 (10.2) | 8 (0, 21) | 21.1 (5.7) | ||
| Family history of psychiatric disorders | |||||
| No | 120 (93.8) | 11 (0.5, 19) | 1.06 | 22.8 (6.2) | |
| Yes | 8 (06.3) | 2.5 (0, 16.5) | 21.8 (6.9) | 0.46 | |
MMSI: Modified Scale for Suicidal Ideation, HDRS: Hamilton Depression Rating Scale, SSRIs: Selective serotonin reuptake inhibitors, TCAs: Tricyclic antidepressants, *P<0.05
In comparing the MSSI scores among the various categories of clinical variables, a significant relationship was observed with a history of suicide. Those with a positive history scored significantly more on MSSI. A trend was also noted in the age of onset. Those with an age of onset later than 30 years scored more on suicidal ideation. On a similar comparison of the HDRS scores among the various categories of clinical variables, previous suicide attempts and present medications showed a significant association. Those with a positive history of suicide scored more on HDRS. On post hoc analysis, the participants treated with tricyclic antidepressants were significantly more depressed than those treated with the SSRIs.
Out of the 128 participants, 62 (48%) had a history of suicide attempts. The latter were enquired further about these attempts. Table 3 shows the characteristics of these suicide attempts and their association with the MSSI and HDRS scores. About 21% of the hospitalized depressive patients reported attempting suicide more than three times, and 56% indicated death wishes. Most suicide attempts were made without precautions taken against being interrupted during the attempt (69%). Approximately 42% of the participants were intoxicated (primarily with alcohol) before a suicide attempt, and 79% of them reported an intention to die. Approximately 52% of participants reported that they consumed poison to commit suicide, while 48% used other methods such as wrist cutting, hanging, jumping from a height, or jumping into a river [Table 3].
Table 3.
Characteristics of suicide attempts and their association with suicidal ideation (MSSI Score) and severity of depression (HDRS Score) at baseline (n=62)
| Characteristics of suicide attempts | n (%) | MSSI Score | HDRS Score | ||
|---|---|---|---|---|---|
|
|
|
||||
| Median (q1, q3) | U/H | Mean (SD) | t/F | ||
| Suicide communication | |||||
| Death wish only | 35 (56.4) | 12 (6, 21) | 0.64 | 23.4 (6.7) | 1.37 |
| Suicide ideas/plans | 20 (32.3) | 11 (0, 20) | 25.9 (5.5) | ||
| Suicide threat/warning | 7 (11.3) | 13 (0, 22) | 21.9 (8.3) | ||
| Precaution is taken against being interrupted during an attempt | |||||
| No | 43 (69.3) | 12 (4, 21) | -0.81 | 23.0 (6.3) | -1.99* |
| Yes | 19 (30.7) | 16 (0, 24) | 26.5 (6.7) | ||
| Intoxicated during an attempt | |||||
| No | 36 (58.1) | 11.5 (2, 20.5) | -0.96 | 22.2 (6.5) | -2.77** |
| Yes | 26 (41.9) | 12 (4, 22) | 26.6 (5.8) | ||
| Intention to die | |||||
| No/not sure | 13 (21.0) | 6 (0, 13) | -1.68 | 20.9 (6.0) | -1.96* |
| Yes | 49 (79.0) | 13 (8, 21) | 24.9 (6.5) | ||
| Suicide method | |||||
| Poisoning | 32 (51.6) | 12 (3, 21.5) | 0.04 | 23.0 (5.7) | -1.24 |
| Others | 30 (48.4) | 13.5 (4, 21) | 25.1 (7.3) | ||
MMSI: Modified Scale for Suicidal Ideation, HDRS: Hamilton Depression Rating Scale, *P<0.05, **<0.01
Though no significant relationship was observed between the MSSI scores with the various characteristics of suicide attempts, a trend was observed where the participants with the intent to die scored more on the MSSI. A similar relationship with severity of depression suggests that those who took precautions against being interrupted were intoxicated and intended to die during an attempt were significantly more depressed.
Discussion
Depression, among other mental health problems, has a substantial impact on public health, and if left untreated, has a high risk of relapse. Studies have indicated that the risk of suicide death among depressed hospitalized patients is significantly increased. The current study explored the frequency of suicide ideation and their sociodemographic and clinical correlates among inpatients with depressive disorders.
The setting of a study, inpatient-based, is one of the most critical factors determining the rate of suicidal behavior because hospitalized patients reflect the more severe forms of depressive disorders with high rates of suicidal ideation and attempts.[19] In the current study, the rate of suicidal ideation in patients with depressive disorders was 87%, and 48% attempted suicide. This high rate conforms to the rates reported in the other studies conducted within the inpatient and outpatients settings.
Compared to the findings of the National Mental Health Survey, India, conducted among the general population, the lifetime prevalence of suicidal ideation among MDD patients was high (Amudhan S, et al., 2020).[20] The current findings are similar to those of a medical record-based study in the UK in which patients attending secondary care with moderated to severe depression reported 71% suicidal thoughts and 38% attempted suicide.[21]
Over half of the participants were less than 40 years of age in the present study. It is commonly established that persons in this category are prone to depression due to various life stressors, such as marital strife, unemployment, and health concerns. The findings are comparable to Yoo et al.[22] who found that 23.1% of people aged 40–49 years have MDD.Click or tap here to enter text. In terms of the association between age and suicidal ideation, multiple follow-up studies have discovered that the risk of suicidal ideation was higher in older respondents than in younger respondents. Furthermore, increasing age was linked to a more considerable risk of suicide ideation. In our study, the proportion of patients with suicidal ideation was more significant in those over 40 years of age than in their younger counterparts, though this was not statistically significant.
The present study did not reveal any significant association between gender, religion, marital status, and education with suicidal ideation and depression. These findings are consistent with the other Indian studies.[5,23] However, the majority has found a gender gap in the prevalence of suicide ideation.
On the other hand, occupation showed a significant relationship with the scores of depression. A similar finding was noted in another Indian study.[24] Farmers were much more depressed than the government employees. According to research from around the world, those who work in agricultural occupations are more prone than anyone else to have depressive disorders.[25,26]
One of the study’s main findings is that severe depressive individuals had a higher likelihood of suicide ideation and attempts. Those with a positive history of suicide scored more on the HDRS. The participants treated with tricyclic antidepressants were significantly more depressed than those treated with SSRIs. These findings were consistent with those of the other studies, implying that suicidal thoughts are proportional to the severity of depression. Considering the temporal association of suicidal attempts with depressive symptoms, minimizing the duration of the depressed state would be an effective way to prevent suicidal acts.[21,27]
The current study showed no effect of clinical variables such as the age of onset, duration of present episode, past episode, or treatment modality, comorbidity, hospitalization, or history of electro convulsive therapy (ECT) on the severity of suicidal ideation or depression. However, there was significantly more severe suicidal ideation and depression in those with past attempts. These findings were concurrent with the findings of the other studies.[4,28] Besides, there was clear evidence from the other studies that the number of previous hospitalizations and length of the current episode had positively predicted depression.[29] Some studies had similar results regarding past suicide attempts, indicating that suicide attempts are the most powerful predictor of future suicidal acts.[28,29,30,31]
It is worth noting that in this study those who intended to die scored higher on the MSSI. Those who took precautions against being interrupted were intoxicated and had the intention to die during an attempt were much more depressed. Another study from an Indian state found that the attempters with a definite desire to die had proportionately higher psychiatric illnesses than those who were ambivalent.[32,33] Depression and alcoholism were comorbid in 85% of the 100 cases of completed suicides as reported by another study, which confirms an interaction between alcohol use, depression, and suicide attempt.[34]
This study provided insight on screening severe depressive patients for suicidal ideation in a general hospital psychiatric setting. Inpatient suicides contribute a small but significant proportion of the overall suicides.[35] Environmental modifications and educating the health care professionals appear to be the most promising strategies to reduce suicide-related mortality among inpatients.
Reducing suicide risks for inpatients requires a careful risk assessment, in addition to a safe environment with good teamwork and patient-staff communication. Inpatient suicides most often occurred off the ward with peaks in the short periods around admission and discharge.[36] Hence, the early evaluation at admission and increasing attention for suicide risk at follow-up after discharge are crucial for suicide prevention, including primary care.
Limitations
A few limitations of this study are its small sample size. As a result, the generalizability of the findings is limited. Because the participants with depressive disorders were receiving treatment, the impact of medications may have altered the severity ratings, though the data collection was completed within a week of admission. Some degree of recall bias cannot be ruled out regarding the previous suicide attempts, as the information was retrospective in nature. Even though limitations exist in the present study, it explored information using both structured and semi-structured tools to collect comprehensive information on the various aspects of suicide attempts.
Conclusion
The study on inpatients with MDD shows that the more severe the depression, the more the severity of suicidal ideation and attempts. Approximately 87% had suicidal ideation, and 48% attempted suicide. The severity of depression was higher in the farmers than in the government employees, and the history of suicide was related to more severe suicidal ideas and depression. Among those who were more severely depressed and more likely to make their suicide attempts were intoxicated, had taken precautions against being interrupted, and had an intention to die. The study reiterates the importance of screening for suicide, particularly in those with more severe depression in the inpatient setting.
Highlights
• Suicidal ideation is higher in depressive patients—a precursor to suicide attempts.
• The majority of the inpatients with depression reported moderate to severe suicidal ideas.
• Reducing suicide risk for inpatients requires a careful risk assessment in addition to a safe environment with good teamwork and patient-staff communication.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Anniappan Arvind B, Gururaj G, Loganathan S, Amudhan S, Varghese M, Benegal V, et al. Prevalence and socioeconomic impact of depressive disorders in India:Multisite population-based cross-sectional study. BMJ Open. 2019;9:e27250. doi: 10.1136/bmjopen-2018-027250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Averill IRE, Beaglehole B, Douglas KM, Jordan J, Crowe MT, Inder M, et al. Activation therapy for the treatment of inpatients with depression-Protocol for a randomized control trial compared to treatment as usual. BMC Psychiatry. 2019;19:52. doi: 10.1186/s12888-019-2038-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harmer B, Lee S, Duong T vi H, Saadabadi A. Suicidal ideation. Acute Medicine:A Symptom-Based Approach Treasure Island (FL):StatPearls Publishing. 2021:415–20. [Google Scholar]
- 4.Basha EA, Mengistu BT, Engidaw NA, Wubetu AD, Haile AB. Suicidal ideation and its associated factors among patients with major depressive disorder at Amanuel mental specialized hospital, Addis Ababa, Ethiopia. Neuropsychiatr Dis Treat. 2021;17:1571–7. doi: 10.2147/NDT.S311514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lalthankimi R, Nagarajan P, Menon V, Olickal JJ. Predictors of suicidal ideation and attempt among patients with major depressive disorder at a tertiary care hospital, Puducherry. J Neurosci Rural Pract. 2021;12:122–12. doi: 10.1055/s-0040-1721558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ajdacic-Gross V, Killias M, Hepp U, Gadola E, Ma M, Bopp C, et al. Am J Public Health. [Last accessed on 201 Oct 05];2006 96 doi: 10.2105/AJPH.2005.075812. Available from:https://www.sciencedirect.com/science/article/pii/S0165032716307868 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mortensen PB, Agerbo E, Erikson T, Qin P, Westergaard-Nielsen N. Psychiatric illness and risk factors for suicide in Denmark. Lancet. 2000;355:9–12. doi: 10.1016/s0140-6736(99)06376-x. [DOI] [PubMed] [Google Scholar]
- 8.Sakinofsky I. Preventing suicide among inpatients. Can J Psychiatry. 2014;59:131–40. doi: 10.1177/070674371405900304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tishler CL, Reiss NS. Inpatient suicide:Preventing a common sentinel event. Gen Hosp Psychiatry. 2009;31:103–9. doi: 10.1016/j.genhosppsych.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Dahale A, Sherine L, Chaturvedi SK. In-patient suicide in psychiatry –An Indian experience. Epidemiol Psychiatr Sci. 2017;26:565–9. doi: 10.1017/S2045796017000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi Y-J, Lee W-Y. The prevalence of suicidal ideation and depression among primary care patients and current management in South Korea. Int J Ment Health Syst. 2017;11:18. doi: 10.1186/s13033-017-0123-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sinclair L, Leach R. Exploring thoughts of suicide. BMJ. 2017;356:j1128. doi: 10.1136/bmj.j1128. [DOI] [PubMed] [Google Scholar]
- 13.Ryan EP, Oquendo MA. Suicide risk assessment and prevention:Challenges and opportunities. [Last accessed on 2021 Oct 05];FOCUS The Journal of Lifelong Learning in Psychiatry. 2020 18:88–99. doi: 10.1176/appi.focus.20200011. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7587888/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khanra S, Mahintamani T, Bose S, Khess CRJ, Umesh S, Ram D. Inpatient suicide in a psychiatric hospital:A nested case-control study. Indian J Psychol Med. 2016;38:571–6. doi: 10.4103/0253-7176.194914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohamed AE, Abdel Fattah NR, El Masry NM. Demographic and personality assessment in relation to suicidal ideation in depressive disorders. Egypt J Psychiatr. 2014;35:151–60. [Google Scholar]
- 16.Carrozzino D, Patierno C, Fava GA, Guidi J. The Hamilton rating scales for depression:A critical review of clinimetric properties of different versions. Psychother Psychosom. 2020;89:133–50. doi: 10.1159/000506879. [DOI] [PubMed] [Google Scholar]
- 17.Miller IW, Norman WH, Bishop SB, Dow MG. The Modified Scale for Suicidal Ideation:reliability and validity. J Consult Clin Psychol. 1986;54:724–5. doi: 10.1037//0022-006x.54.5.724. doi:10.1037//0022-006x.54.5.724. [DOI] [PubMed] [Google Scholar]
- 18.Armitage P. Attitudes in clinical trials. Statist.Med.1998.17. pp. 2675–2683. Available from:https://onlinelibrary.wiley.com/doi/10.1002/(SICI)1097-0258(19981215)17:23%3C2675::AID-SIM34%3E3.0.CO;2-1 . [DOI] [PubMed]
- 19.Isometsä E. Suicidal behavior in mood disorders--who, when, and why? Can J Psychiatry. 2014;59:120–30. doi: 10.1177/070674371405900303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amudhan S, Gururaj G, Varghese M, Benegal V, Rao GN, Sheehan DV, et al. A population-based analysis of suicidality and its correlates:Findings from the National mental health survey of India, 2015-16. Lancet Psychiatry. 2020;7:41–51. doi: 10.1016/S2215-0366(19)30404-3. [DOI] [PubMed] [Google Scholar]
- 21.Werbeloff N, Markou M, Hayes JF, Pitman AL, Osborn DPJ. Individual and area-level risk factors for suicidal ideation and attempt in people with severe depression. J Affect Disord. 2016;205:387–92. doi: 10.1016/j.jad.2016.08.015. [DOI] [PubMed] [Google Scholar]
- 22.Yoo HJ, Hong JP, Cho MJ, Fava M, Mischoulon D, Heo JY, et al. Lifetime suicidal ideation and attempt in adults with full major depressive disorder versus sustained depressed mood. J Affect Disord. 2016;203:275–80. doi: 10.1016/j.jad.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Sokero TP, Melartin TK, Rytsälä HJ, Leskelä US, Lestelä-Mielonen PS, Isometsä ET. Suicidal ideation and attempts among psychiatric patients with major depressive disorder. J Clin Psychiatry. 2003;64:1094–100. doi: 10.4088/jcp.v64n0916. [DOI] [PubMed] [Google Scholar]
- 24.Singh V, Srivastava A, Varma A, Chaudhry R, Desai NG, Gupta DK, et al. Sociodemographic and clinical profile of patients with attempted suicide attending emergency services at the mental health institute in Northern India. J Mental Health Hum Behav. 2014;19:69. [Google Scholar]
- 25.Tanveer AM, Jyothi J, Vishwanatha Prevalence of depression among the farmers and its determinants:A cross-sectional study. Natl J Community Med. 2019;10:466–9. [Google Scholar]
- 26.Yazd SD, Wheeler SA, Zuo A. Key risk factors affecting farmers'mental health:A systematic review. Int J Environ Res Public Health. 2019;16:4849. doi: 10.3390/ijerph16234849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hassan WAN, Noaman MM, Khalifa H, Abdelrahman AA, Omar SM. A clinical study of suicide in patients admitted in psychiatry unit in Assiut University. Middle East Curr Psychiatry. 2020;27:26. [Google Scholar]
- 28.Brioschi S, Franchini L, Fregna L, Borroni S, Franzoni C, Fossati A, et al. Clinical and personality profile of depressed suicide attempters:A preliminary study at the open-door policy mood disorder unit of San Raffaele hospital. Psychiatry Res. 2020;287:112575. doi: 10.1016/j.psychres.2019.112575. [DOI] [PubMed] [Google Scholar]
- 29.Kraus C, Kadriu B, Lanzenberger R, Zarate CA, Jr, Kasper S. Prognosis and improved outcomes in major depression:A review. Transl Psychiatry. 2019;9:127. doi: 10.1038/s41398-019-0460-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Melhem NM, Porta G, Oquendo MA, Zelazny J, Keilp JG, Iyengar S, et al. Severity and variability of depression symptoms predicting suicide attempt in high-risk individuals. JAMA Psychiatry. 2019;76:603–13. doi: 10.1001/jamapsychiatry.2018.4513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weissman CR, Hadas I, Yu D, Jones B, Kong D, Mulsant BH, et al. Predictors of change in suicidal ideation across treatment phases of major depressive disorder:Analysis of the STAR*D data. Neuropsychopharmacology. 2021;46:1293–9. doi: 10.1038/s41386-020-00953-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kar N. Profile of risk factors associated with suicide attempts:A study from Orissa, India. Indian J Psychiatry. 2010;52:48–56. doi: 10.4103/0019-5545.58895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kumar CTS, Mohan R, Ranjith G, Chandrasekaran R. Characteristics of high intent suicide attempters admitted to a general hospital. J Affect Disord. 2006;91:77–81. doi: 10.1016/j.jad.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 34.Poorolajal J, Haghtalab T, Farhadi M, Darvishi N. Substance-use disorder and risk of suicidal ideation, suicide attempt and suicide death:A meta-analysis. J Public Health (Oxf) 2016;38:e282–91. doi: 10.1093/pubmed/fdv148. [DOI] [PubMed] [Google Scholar]
- 35.Navin K, Kuppili PP, Menon V, Kattimani S. Suicide prevention strategies for general hospital and psychiatric inpatients:A narrative review. Indian J Psychol Med. 2019;41:403. doi: 10.4103/IJPSYM.IJPSYM_169_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee J, Burdick KE, Ko C, Liu T, Lin YC, Lee M. Prevalence and factors associated with suicide ideation and psychiatric morbidity among inpatients of a general hospital:A consecutive three-year study. Kaohsiung J Med Sci. 2021;37:427–33. doi: 10.1002/kjm2.12336. [DOI] [PubMed] [Google Scholar]


