ABSTRACT
Background:
Stroke is primarily a clinical diagnosis. It can be hemorrhagic or ischemic in etiology. Computed tomography (CT) brain is usually the initial investigation in most patients with suspected stroke. Although it has excellent accuracy in diagnosing hemorrhage, ischemic changes may not be apparent in the first few hours. Some centers use focused magnetic resonance imaging (MRI) studies to help in selecting appropriate patients for reperfusion therapy. However, clinicians often use this investigation even when reperfusion therapy is not being considered. This study aims to find out whether doing an MRI in addition to a CT scan has any clinical utility in this situation.
Primary Objective:
To determine the proportion of patients who undergo a change in their management based on MRI findings.
Secondary Objectives:
1. To determine the time duration from the onset of symptoms to presentation at the hospital. 2. To determine the time duration from presentation to the hospital to get CT performed. 3. To determine the proportion of patients who had MRI in addition to CT. 4. To determine the time duration from CT performed to MRI performed.
Materials and Methods: Study Design:
Retrospective, descriptive observational study.
Inclusion Criteria:
Patients above age 18 admitted at a tertiary hospital with a clinical diagnosis of stroke between 1/8/2018 and 30/7/2019.
Exclusion Criteria:
Patients who had already undergone MRI before presentation to the hospital and patients undergoing thrombolysis. Patients meeting the inclusion and exclusion criteria were identified from the hospital information system and the ward admission register and by manual examination of the patients’ case notes. Relevant data were obtained from the case notes and collected on a google form and downloaded in Microsoft Excel 2019. SPSS version 22 was used for data analysis.
Results:
Out of the 106 patients, 54% (n = 57) were diagnosed as having ischemic stroke, whereas 46% (n = 49) were diagnosed with hemorrhagic stroke after initial assessment and CT scan. Only 2.8% (n = 3) of the patients presented within 4.5 hours of the onset of symptoms. 43.4% (n = 46) presented between 4.5 and 24 hours from the onset, whereas 53.8% (n = 57) presented more than 24 hours after the onset. Twenty-seven patients had their CT scan performed prior to their presentation at the center. For the remaining 79, the median time from presentation to CT scanning was 2 ± 1.5 hours. 24.5% (n = 26) of all patients had an MRI performed in addition to the CT scan. There was wide variation in the time from CT scanning to the MRI. Among the patients who had an MRI, additional information was obtained by the investigation in 58% (n = 15). However, this led to a change in management in only three (11.5%) of the patients. On review, it was found that the change was justified in only two patients. Furthermore, one patient who was diagnosed with tuberculoma had a long history of fever which was missed on initial evaluation. Considering these, MRI can be credited for a meaningful change in management in only 4% (n = 1) of the cases.
Conclusion:
The findings of this study do not support the routine use of MRI in patients who are not candidates for reperfusion therapy. Their use should be restricted to cases where some specific information is sought or where there is diagnostic uncertainty. Allocation of resources in developing integrated acute stroke pathways is likely to give a better value for money.
Keywords: MRI, reperfusion therapy, stroke
Introduction
Stroke is a “clinical syndrome consisting of rapidly developing clinical signs of focal (or global in the case of coma) disturbance of cerebral functions lasting more than 24 hours or leading to death with no apparent cause other than a vascular origin”.[1] It is a major public health problem and one of the leading causes of mortality and morbidity globally as well as in India.[2,3] Stroke can be classified as either ischemic or hemorrhagic. Blockage of an artery supplying blood to an area of the brain either because of in situ thrombus formation or because of an embolus leads to an ischemic stroke, whereas rupture of a blood vessel and consequent spillage of blood causes a hemorrhagic stroke. Of all strokes, 87% are ischemic and the remaining are hemorrhagic.[4] Some Indian studies have suggested a relatively higher proportion of hemorrhagic strokes.[5]
A non-contrast computed tomography (CT) (NCCT) scan of the brain is often the first imaging modality in a patient with suspected stroke and can reliably identify a hemorrhagic stroke.[6] However, radiological signs of ischemia may not be evident in the first few hours.[7] Magnetic resonance imaging (MRI) is more sensitive in detecting ischemia and as sensitive as CT in demonstrating intracranial hemorrhage.[8,9] MRI is costly, time-consuming, less easily available and difficult to perform in a critically ill patient. Thus, CT scan is usually the first imaging modality in patients with suspected stroke. It is especially useful in patients presenting within 4.5 hours in rapidly excluding intracranial hemorrhage before thrombolysis can be offered. In patients who wake up with symptoms of stroke or in whom the precise time of onset of symptoms is not clear, MRI to identify diffusion-positive fluid-attenuated inversion-negative lesions can be useful in selecting patients who can benefit from thrombolysis.[10] Some centers offer mechanical thrombectomy to selected patients with acute ischemic stroke who present beyond the time window for thrombolysis but within 24 hours from the onset of symptoms. In patients who present within this duration and who have features of large vessel occlusion of the anterior circulation, either a CT angiogram with CT perfusion or an MR angiogram with diffusion-weighted MRI with or without MRI perfusion can be used for selecting patients for mechanical thrombectomy.[10] It is not clear whether MRI has any role in the management of patients with stroke outside the specific scenarios mentioned above. This study intends to find out if MRI has a role in the management of patients with stroke who are not candidates for reperfusion therapy. The findings are likely to help stroke physicians, neurologists, general physicians, emergency physicians and primary physicians involved in acute care in choosing the most appropriate and cost-effective investigations for patients presenting with stroke.
Materials and Methods
The study was carried out at a single tertiary care hospital in Eastern India after obtaining approval from the institutional ethics committee. It was a descriptive observational study based on retrospective analysis of medical records. The aim was to identify whether doing an MRI in addition to a CT scan of the brain makes a difference in the management of patients with acute stroke who are not candidates for reperfusion therapy. The primary objective was to determine the proportion of patients who underwent a change in their management on the basis of MRI findings. The secondary objectives included the determination of (a) the proportion of patients who presented to the hospital within 4.5 hours, between 4.5 and 24 hours, and after 24 hours from the onset of symptoms; (b) the average duration from the presentation at the hospital to the CT brain; (c) the proportion of patients who had MRI in addition to CT; and (d) the average duration from CT to MRI.
All patients above the age of 18 who were admitted with a clinical diagnosis of stroke between August 01, 2018 and July 31, 2019 were included in the study. Those patients who underwent thrombolysis or had an MRI performed prior to their presentation to the hospital were excluded from the study. To identify the eligible cases for the study, a list of all patients admitted under general medicine in the given period was obtained from the hospital information system. Among these, those patients who had an initial diagnosis of stroke or who had presented with suggestive symptoms, namely, speech disturbance, limb weakness, facial weakness, visual field defect, or sudden loss of consciousness were identified from the ward admission register maintained by the nursing staff. Their case notes were obtained from the medical records department and manually examined to identify the cases who actually had a clinical diagnosis of acute stroke on admission and were suitable for the study according to the inclusion and exclusion criteria mentioned above. Data regarding the patient’s age, sex, time of onset of symptoms, date and time at presentation to the hospital, time at which CT was performed, CT findings, treatment given, whether MRI was performed, time of MRI if performed, MRI findings and changes in treatment if any based on MRI findings were obtained from the case notes and entered into a pre-formed semi-structured online Google form and then downloaded in Microsoft Excel 2019. SPSS version 22 was used for data analysis. Continuous variables were expressed as mean and standard deviation or median and inter-quartile range. Categorical variables were expressed as frequency and proportion. Independent sample t-test analysis was used to compare the mean age between two groups. Chi-square test of significance was used to compare categorical variables. The significance level was set at P < 0.05.
Results
On initial screening from the hospital information system and the ward register, 267 patients were identified to have either an initial diagnosis of stroke or symptoms potentially suggestive of stroke. On examination of the doctor’s clinical notes in the admission file, patients who did not have a clinical diagnosis of stroke (n = 149) and those who had their MRIs done before admission to the hospital (n = 12) were excluded. The remaining 106 patients were included in the final analysis.
Out of the 106 patients, 58% (n = 61) were male and 42% (n = 45) were female. Furthermore, 54% (n = 57) were diagnosed as having ischemic stroke, whereas 46% (n = 49) were diagnosed with hemorrhagic stroke after initial assessment and CT scan. The mean age was 64.03 years. The mean age of patients with ischemic stroke was 3.165 years more than those with hemorrhagic stroke. However, the difference was not statistically significant [Table 1].
Table 1.
Comparison of age in patient groups based on the type of stroke [n=106]
| n | Mean±SD | Mean difference (95% CI) | t (df) | P | |
|---|---|---|---|---|---|
| All patients | 106 | 64.03±13.224 | |||
| Ischemic | 57 | 65.49±12.717 | 3.165 (-1.931-8.261) | 1.231 (104) | 0.221 |
| Hemorrhagic | 49 | 62.33±13.724 |
Only 2.8% (n = 3) of the patients presented within 4.5 hours of the onset of symptoms. 43.4% (n = 46) presented between 4.5 and 24 hours from the onset, whereas 53.8% (n = 57) presented more than 24 hours after the onset. Twenty-seven patients had their CT scan done prior to their presentation at the center. For the remaining 79 patients, the median time from presentation to CT scanning was 2 ± 1.5 hours [Figure 1].
Figure 1.
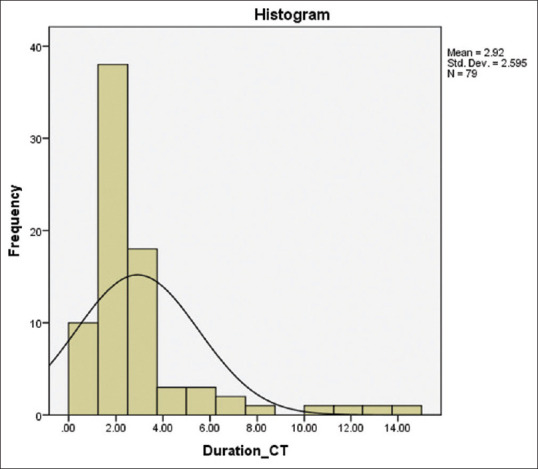
Duration (in hours) from presentation at hospital to CT scan being done [n = 79]: on its visual inspection of the histogram, it is obvious that the distribution is not normal but right-skewed (skewness = 2.896) and platykurtic (kurtosis = 8.928). The median duration from presentation at hospital to CT scanning is 2 ± 1.5 hours
24.5% (n = 26) of all patients had an MRI done in addition to the CT scan. These patients, on an average, were 1.821 years younger than those who did not have an MRI performed but this difference was not significant statistically [Table 2]. Out of the 26 patients, five had hemorrhagic stroke, whereas 21 had ischemic stroke. Patients with ischemic stroke were significantly more likely to undergo an MRI [Table 3]. The duration between CT scan and MRI is shown in Table 4.
Table 2.
Comparison of age in patient groups based on whether or not MRI was done [n=106]
| n | Mean±SD | Mean difference (95% CI) | t (df) | P | |
|---|---|---|---|---|---|
| All patients | 106 | 64.03±13.224 | |||
| MRI not done | 80 | 64.48±13.223 | 1.821 (-4.116-7.759) | 0.608 (104) | 0.544 |
| MRI done | 26 | 62.65±13.392 |
Table 3.
Comparison of groups of getting MRI performed in patients based on the type of stroke [n=106]
| n | MRI | Chi-square (df) | P | ||
|---|---|---|---|---|---|
|
| |||||
| Not done (%) | Done (%) | ||||
| Type of stroke | |||||
| Ischemic | 57 | 36 (63.2%) | 21 (36.8%) | 10.1 (1) | 0.001 |
| Hemorrhagic | 49 | 44 (89.8%) | 5 (10.2%) | ||
Table 4.
Frequency table showing the duration from CT scan to MRI [n=26]
| Duration | Frequency | Percentage |
|---|---|---|
| Not known (CT scan performed outside prior to admission) | 5 | 19.2 |
| 1-2 days | 2 | 7.7 |
| 3-5 days | 7 | 26.9 |
| More than 5 days | 12 | 46.2 |
Among the patients who had an MRI, additional information was obtained by the investigation in 58% (n = 15). Table 5 lists the additional findings obtained from MRI. These findings led to a change in the management in 11.5% (n = 3) of the patients. These changes are listed in Table 6.
Table 5.
Frequency table showing the additional findings obtained from MRI [n=15]
| Additional findings | Frequency |
|---|---|
| Confirmation of ischemic stroke where NCCT was normal but clinical diagnosis of stroke was made | 5 |
| More detailed information on ischemic changes where ischemic stroke was diagnosed on NCCT | 4 |
| Features suggestive of viral encephalitis | 1 |
| Change in the size of hemorrhagic area after initial hemorrhagic stroke | 2 |
| Tuberculoma was seen in addition to ischemic infarction | 1 |
| Hemorrhagic transformation of ischemic stroke was seen | 2 |
Table 6.
Changes in management after MRI [n=3]
| Changes in management | Frequency |
|---|---|
| Anti-tuberculosis treatment started after diagnosis of intra-cranial tuberculoma. | 1 |
| The diagnosis was changed to encephalitis. Aspirin and atorvastatin were stopped. The patient was discharged immediately after the MRI report. | 1 |
| Aspirin was stopped because of small internal active bleed within the area of ischemic infarction. | 1 |
Discussion
Most strokes are ischemic. Less than 15% of all strokes are expected to be hemorrhagic.[4] However, 46% of the patients in this study had hemorrhagic stroke. Previous studies from different parts of India have noted the proportion of hemorrhagic strokes to be 17.7%, 11.6%, and 32%, respectively.[5,11,12] Larger studies are needed for a more reliable estimation of the proportion of ischemic and hemorrhagic strokes in India and to see if there are any regional variations. The sample size (n = 106) of this study was small. Moreover, as the study was carried out in a tertiary hospital which also receives a lot of referred patients, the findings may not reflect the true proportion of ischemic and hemorrhagic strokes in the community.
Only three patients (2.8%) presented within 4.5 hours of the onset of symptoms, that is, within the time window for thrombolysis. All the three had hemorrhagic strokes. Therefore, there was not a single patient who could be considered for thrombolysis. Forty-six patients (43.4%) presented between 4.5 and 24 hours from the onset. They were not evaluated for thrombectomy as the center does not currently offer this service to patients with acute ischemic stroke. More than half of the patients (n = 57, 53.8%) presented more than 24 hours after the onset of symptoms which is clearly beyond the time window for any form of reperfusion therapy. Previous studies have noted that an overwhelming majority of patients fail to present within the time window for thrombolysis because of inability of patients, relatives and physicians to recognize symptoms of stroke; the lack of imaging facilities at primary health care centers; the lack of transport facilities and financial constraints.[13,14] This highlights the need for increased awareness, better training of health care workers and streamlining of services so that a larger proportion of the patients can receive this evidence-based treatment.
Twenty-seven patients had their CT scan performed prior to their presentation at the center. For the remaining 79 patients, the median time from presentation to CT scanning was 2 ± 1.5 hours [Figure 1]. The National Institute for Health and Care Excellence (NICE) guidelines recommend that an NCCT scan of the brain should be performed as soon as possible and within 24 hours of symptom onset in everyone with suspected acute stroke who does not have an indication for immediate imaging, namely, indication for reperfusion therapy, anti-coagulant therapy, a history of bleeding tendency, a Glasgow Coma Score below 13, unexplained progressive or fluctuating symptoms, papilledema, fever or neck stiffness and severe headache. All the 79 patients had their brain CT performed well within this audit standard.
There was large variation in the duration from CT scan to MRI with the majority of patients getting the MRI more than 5 days after the CT scan. MRI yielded additional information in 15 (57.7%) out of the 26 patients who had this investigation [Table 5]. However, this led to a change in the management in only three (11.5%) patients. In the first patient, an additional diagnosis of brain tuberculoma was made and the patient was given anti-tubercular treatment. On reviewing the history, it was found that a long history of fever was missed in the primary evaluation which would otherwise have prompted a more detailed workup of fever including an MRI. In the second patient, the diagnosis was changed to encephalitis; aspirin and atorvastatin were stopped and the patient was discharged. In the third patient, aspirin was stopped as a small bleed was noted within the area of ischemic infarction. Spontaneous hemorrhagic transformation is a very frequent complication of ischemic stroke, incidence varies from 13% to 43% in CT studies and incidence of symptomatic hemorrhagic transformation varies from 0.6% to 20%.[15,16] Generally, anti-platelet treatment can be safely continued after hemorrhagic transformation of an ischemic stroke and is not associated with adverse neurological outcomes.[17] Hence, it is debatable whether stopping aspirin was actually warranted in this case. Moreover, a repeat NCCT would also have picked up the small bleed that was seen on the MRI. Considering the above, it may be argued that in only one case (4%), MRI as a part of stroke workup can be credited for a meaningful change in the patient’s management. A previous study on 97 patients had noted a change in the treatment plan based on MRI in 26% (n = 25) of the patients. However, these were hyper-acute cases with the average time from onset of symptoms to clinical evaluation of 125 minutes and focused MRI studies were performed to facilitate the decision regarding reperfusion treatment. On the other hand, most patients in this study had presented late and the MRI was often performed a few days later.
MRI is costly, takes time and requires availability of the equipment as well as trained manpower. Many hospitals have very long waiting lists for out-patient MRIs.[18] Thus, their judicious use is imperative. MRIs may be useful in some special circumstances, for example, posterior fossa or posterior circulation strokes, wake-up strokes, or where the time of onset is unclear and suspected large vessel occlusion of the anterior circulation in patients who present within 24 hours but after the time window for thrombolysis to assess suitability for mechanical thrombectomy. Some centers may include a focused MRI in their acute stroke protocol to facilitate the decision regarding thrombolysis. However, the findings of this study do not support the routine use of MRI in patients who are not candidates for reperfusion therapy. Allocation of resources in developing integrated acute stroke pathways is likely to give a better value for money.
The role of the primary physician is crucial in the acute as well as long-term care of stroke patients.[19] Some primary physicians may choose to work in the emergency department or to provide in-patient care within hospitals on a part time or full time basis. They often provide the majority of emergency care in rural areas that do no not have designated emergency doctors.[20] In India, urgent care practice is an emerging concept that envisages a greater role for primary physicians in the management of illnesses and injuries requiring immediate care.[21] Moreover, in some countries, primary physicians are directly involved in the commissioning of health care for their patients and populations.[22] Thus, the findings of this study are likely to be useful for a large number of primary physicians in deciding about the best care for their patients.
Conclusion
To the best of the authors’ knowledge, this is the first study evaluating the utility of MRI in patients with stroke who are not candidates for reperfusion therapy. Although this investigation offers additional information in a majority of cases, it seldom leads to a change in the management. Thus, it should be reserved for special circumstances as discussed above. None of the patients with ischemic stroke presented within 4.5 hours, which is the time window for thrombolysis. Thus, there is a need for increased awareness and streamlining of services to ensure that a greater number of patients can receive this evidence-based treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hatano S. Experience from a multicentre stroke register: A preliminary report. Bull World Health Organ. 1976;54:541–53. [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Stoke Facts. [accessed on 2021 Oct 14]. Available from: https://www.cdc.gov/stroke/facts.htm .
- 3.Kamalakannan S, Gudlavalleti ASV, Murthy Gudlavalleti VS, Goenka S, Kuper H. Incidence and prevalence of stroke in India: A systematic review. Indian J Med Res. 2017;146:175–85. doi: 10.4103/ijmr.IJMR_516_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: A report from the American heart association. Circulation. 2020;141:e139–596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 5.Das SK, Banerjee TK, Biswas A, Roy T, Raut DK, Mukherjee CS, et al. A prospective community-based study of stroke in Kolkata, India. Stroke. 2007;38:906–10. doi: 10.1161/01.STR.0000258111.00319.58. [DOI] [PubMed] [Google Scholar]
- 6.Macllari F, Paciaroni M, Agnelli G, Caso V. Neuroimaging in intracerebral haemorrhage. Stroke. 2014;45:903–8. doi: 10.1161/STROKEAHA.113.003701. [DOI] [PubMed] [Google Scholar]
- 7.Shen J, Li X, Li Y, Wu B. Comparative accuracy of CT perfusion in diagnosing acute ischemic stroke: A systematic review of 27 trials. PLoS One. 2017;12:e0176622. doi: 10.1371/journal.pone.0176622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lansberg MG, Albers GW, Beaulieu C, Marks MP. Comparison of diffusion-weighted MRI and CT in acute stroke. Neurology. 2000;54:1557–61. doi: 10.1212/wnl.54.8.1557. [DOI] [PubMed] [Google Scholar]
- 9.Kidwell CS, Wintermark M. Imaging of intracranial haemorrhage. Lancet Neurol. 2008;7:256–67. doi: 10.1016/S1474-4422(08)70041-3. [DOI] [PubMed] [Google Scholar]
- 10.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2019;50:e344–418. doi: 10.1161/STR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 11.Dalal PM, Malik S, Bhattacharjee M, Trivedi ND, Vairale J, Bhat P, et al. Population-based stroke survey in Mumbai, India: Incidence and 28-day case fatality. Neuroepidemiology. 2008;31:254–61. doi: 10.1159/000165364. [DOI] [PubMed] [Google Scholar]
- 12.Sridharan SE, Unnikrishnan JP, Sukumaran S, Sylaja PN, Nayak SD, Sarma PS, et al. Incidence, types, risk factors, and outcome of stroke in a developing country: The Trivandrum stroke registry. Stroke. 2009;40:1212–8. doi: 10.1161/STROKEAHA.108.531293. [DOI] [PubMed] [Google Scholar]
- 13.Pandian JD, Sethi V, Dhillon R, Kaur R, Padala S, Chakravorty R, et al. Is intravenous thrombolysis feasible in a developing country? Cerebrovasc Dis Basel Switz. 2005;20:134–6. doi: 10.1159/000086804. [DOI] [PubMed] [Google Scholar]
- 14.Panwar A, Veeramalla M, Valupadas C, Ramesh K, Owais M, Muriki R. Barriers to stroke thrombolysis. J Clin Diagnostic Res. 2017;11:OC01–5. [Google Scholar]
- 15.Jaillard A, Cornu C, Durieux A, Moulin T, Boutitie F, Lees KR, et al. Hemorrhagic transformation in acute ischemic stroke. The MAST-E study. MAST-E group. Stroke. 1999;30:1326–32. doi: 10.1161/01.str.30.7.1326. [DOI] [PubMed] [Google Scholar]
- 16.Bang OY, Saver JL, Kim SJ, Kim G-M, Chung C-S, Ovbiagele B, et al. Collateral flow averts hemorrhagic transformation after endovascular therapy for acute ischemic stroke. Stroke. 2011;42:2235–9. doi: 10.1161/STROKEAHA.110.604603. [DOI] [PubMed] [Google Scholar]
- 17.Kim J-T, Heo S-H, Park M-S, Chang J, Choi K-H, Cho K-H. Use of antithrombotics after hemorrhagic transformation in acute ischemic stroke. PLoS One. 2014;9:e89798. doi: 10.1371/journal.pone.0089798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.3 years, that's how long you have to wait for an MRI at Delhi's GB Pant Hospital. India Today, 23 Nov 2016. [accessed on 2021 Oct 24]. Available from: https://www.indiatoday.in/india/delhi/story/gb-pant-hospital-mri-scan-353413-2016-11-23 .
- 19.Dhamija RK, Donnan G. Time is brain-- Acute stroke management. Aust Fam Physician. 2007;36:892–5. [PubMed] [Google Scholar]
- 20.American Academy of Family Physician: Career Options in Family Medicine. [Last accessed on 2022 Feb 04]. Available from: https://www.aafp.org/students-residents/medical-students/explore-career-in-family-medicine/career-practice-options.html .
- 21.Roy P, Kumar R, Aggarwal P. Emergency experts. J Family Med Prim Care. 2020;9:1801–4. doi: 10.4103/jfmpc.jfmpc_286_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.NHS England: Clinical Commissioning Groups. [Last accessed on 2022 Feb 04]. Available from: https://www.england.nhs.uk/commissioning/who-commissions-nhs-services/ccgs/


