Abstract
Background:
Sepsis, a serious condition with high mortality, usually causes sepsis associated encephalopathy (SAE) that involves neuronal cell death. However, the cell death programs involved and their underlying mechanisms are not clear. This study aimed to explore the regulatory mechanisms of different cell death programs in SAE.
Methods:
A neonatal rat model of SAE was established by cecal ligation and perforation. Survival rate and vital signs (mean arterial pressure and heart rate) were monitored, nerve reflexes were evaluated, and cortical pathological changes were observed by hematoxylin and eosin staining. The expression of pyroptosis, apoptosis, and necroptosis (PANoptosis)-related proteins, mitogen- activated protein kinase (MAPK), and its upstream regulator toll-like receptor 9 (TLR9) were detected. The expression of TLR9 in neurons was observed by immunofluorescence staining. The ultrastructure of neurons was observed by transmission electron microscope.
Results:
First, PANoptosis was found in cortical nerve cells of the SAE rats. Meanwhile, the subunits of MAPKs, p38 MAPK, Jun N- terminal kinase, and extracellular signal-regulated kinase (ERK) were activated. After pharmacologically inhibiting each of the subunits, only p38 MAPK was found to be associated with PANoptosis. Furthermore, blocking the p38 MAPK signaling pathway activated necroptosis but inhibited apoptosis and pyroptosis. When necroptosis was pharmacologically inhibited, apoptosis and pyroptosis were reactivated. Finally, we found that the expression of TLR9, a regulator of MAPKs, was significantly increased in this model. After down-regulation of TLR9, p38 MAPK, and ERK signaling pathways were inhibited, which led to the inhibition of PANoptosis. Further analysis found that down-regulation of TLR9 improved the survival rate and reduced the pathological changes in SAE rats.
Conclusions:
Our study showed that the programs comprising PANoptosis are activated simultaneously in SAE rats. TLR9 activated PANoptosis through the p38 MAPK signaling pathway. TLR9 may work as a potential target for SAE treatment.
Keywords: Sepsis associated encephalopathy, TLR9, Apoptosis, Pyroptosis, Necroptosis, p38 mitogen-activated protein kinase
Introduction
Sepsis is a disease with a high mortality rate in the pediatric intensive care unit. The latest sepsis guidelines highlight the impact of multiple organ dysfunction and/or failure on the host.[1] Sepsis associated encephalopathy (SAE), a serious complication of sepsis, is characterized by deterioration of mental state and cognitive function.[2,3] However, the pathological changes and underlying mechanisms of SAE are not fully understood.
Different types of cell death, including apoptosis, pyroptosis, and necroptosis, have been reported in sepsis.
However, the roles of these mechanisms are not clearly defined in SAE. Recently, the interaction of different cell death programs has been reported to have an important influence on the progression of disease.[4,5] One cell death program that is conducted by receptors interacting with inflammatory cytokines can simultaneously lead to pyroptosis, apoptosis, and necroptosis (PANoptosis).[6,7] PANoptosis has been widely reported in sepsis. Of these three types of cell death, cell death mediated by apoptosis often occurs in heart, kidney, and other organ failures during sepsis.[8,9] Cell death caused by pyroptosis usually occurs in lethal sepsis.[10] Cell death involving necroptosis has been observed in kidney damage brought about by mitochondrial dysfunction in sepsis.[11] Although the three cell death programs of PANoptosis have been studied separately in sepsis, they have not been studied simultaneously in SAE. Furthermore, the pathways enabling communication among the different forms of cell death are largely unknown.
The interaction of the multiple cell death programs affects the progression of sepsis. Studies have found that PANoptosis can be triggered after bacterial stimulation by Z-DNA-binding protein 1, interferon regulatory factor 1, or other regulatory factors.[12,13] Simultaneous deletion of the pyroptosis-related proteins caspase (CASP)-1/CASP- 11 and the necroptosis-related protein receptor-interacting serine/threonine protein kinase 3 (RIPK3) leads to inhibition of PANoptosis.[14] Apoptosis and necroptosis have also been shown to be cross-linked. Inhibiting necroptosis was found to normalize the apoptosis of nerve cells and protect brain injury caused by various causes.[15] Therefore, studying the interaction between different cell death programs triggered by sepsis is necessary to further understand their cross-talk mechanisms and pathological processes.
It is known that toll-like receptors (TLRs) play a key role in immunity by activating inflammatory factors and interferons after sepsis.[16] In the central nervous system, TLRs are involved in the cross-talk between immune cells and neurons.[17] Toll-like receptor 9 (TLR9), one subunit of TLRs, is mainly expressed in neuroinflammation. Overactivation of TLR9 promotes some diseases.[18] Inhibition of TLR9 activity was found to reduce growth impairment caused by inflammation.[19] Furthermore, TLR9 activation was shown to increase apoptosis after sepsis.[20] However, whether TLR9 participates in pyroptosis and necroptosis in the encephalopathy caused by sepsis is unknown. In addition, the possible signal pathways involved in TLR9 regulation of PANoptosis during SAE are also not clear. In this study, we set up a sepsis model using neonatal rats by cecal ligation and perforation (CLP) which caused SAE. After successfully establishing the model of PANoptosis in neurons, the expression of the p38 mitogen-activated protein kinase (MAPK), extracellular signal-regulated kinase (ERK), Jun N-terminal kinase (JNK), and TLR9 were observed. Furthermore, the regulation and mechanisms of PANoptosis were studied by detecting the relationship between TLR9 and signaling pathways.
Methods
Sepsis in rats
All the operations in this study are in line with the Research Animal Care Committee of Sichuan University. The male Sprague-Dawley rats (20–22 g, No. 51203500017296) were used in this study. At postnatal day 10, the rats were assigned to two groups including CLP surgery and sham operation. During the CLP procedure, the rats were continuously anesthetized with inhaled isoflurane and kept warm on a thermostatic plate (37°C). The sepsis model was established according to the guidelines.[21] A 1 cm incision was made in the abdomen, and then the cecum was isolated. After ligating the cecum with 4-0 silk, the cecum was punctured twice through-and-through with a 20- gauge needle. The cecum was pressed to release a droplet of feces.[22] The rats in the sham group only had their cecum isolated, without ligation or puncture. Then the contents of the enterocelia were returned and the abdominal wall was sutured layer by layer with 5-0 silk.
Treatments
The CLP rats were injected with 150 ng/g ODN2088 (agonist of TLR9, InvivoGen, San Diego, CA, USA), 50 ng/g SB203580 (inhibitor of p38 MApK, Cell Signaling Technology, Beverly, MA, USA), 75 ng/g PD98059 (inhibitor of ERK, Cell Signaling Technology), 150 ng/g SP600125 (inhibitor of JNK, Cell Signaling Technology), 100 ng/g Z-DEVD-FMK (inhibitor of apoptosis, Selleck, Houston, TX, USA), 12.5 ng/g INF39 (inhibitor of pyroptosis, Selleck), 37.5 ng/g Nec-1s (inhibitor of necroptosis, Cell Signaling Technology), and 1% dimethyl sulfoxide (DMSO) (vehicle, Sigma-Aldrich, St. Louis, MO, USA).[22–28]
Survival, vital signs, and neurobehavioral assessment
The survival number and death number of rats in each period were recorded. Vital signs (mean arterial pressure [MAP] and heart rate [HR]) were monitored. Neuro- behavioral assessment of the rats was conducted based on a previous study.[29] The neurobehavioral assessment included pinna reflex, corneal reflex, tail flexion reflex, righting reflex, and escape response. Each item was awarded two points for normal reflexes, one point for dull reflexes, and zero point for no reflexes. Overall, the higher the score, the less nerve damage, and vice versa.
Histological examination
After the rats were sacrificed, brains were quickly removed and fixed with 4% (w/v) paraformaldehyde, then embedded and sectioned. The pathological changes of the cortex were observed after hematoxylin and eosin staining.[30] Five cortical regions from each rat were randomly selected.
Western blotting
After the rats were sacrificed, the cortex was separated on ice, homogenized, and centrifuged. The supernatant was extracted and loading buffer (Beyotime, Shanghai, China) was mixed. The samples were separated and then transferred to membranes (Millipore, Billerica, MA, USA). Primary antibodies, including rabbit anti-TLR9, rabbit anti-CASP-3, mouse anti-RIPK1, rabbit anti-RIPK3 (1:1000, Abcam, Cambridge, MA, USA), rabbit anti-Bcl-2, goat anti-NOD-, LRR-, and pyrin domain-containing protein 3 (NLRP3), rabbit anti-CASP-1, rabbit anti- phospho-mixed lineage kinase domain-like protein (MLKL) (Ser345), rabbit anti-MAPKAP kinase 2 (MK2), rabbit anti-phospho-MK2 (Thr334) (1:500, Abcam), rabbit anti-ERK, rabbit anti-phospho-ERK (Thr202/Tyr204), rabbit anti-JNK, and rabbit anti-phospho-JNK (Thr183/Tyr185; 1:1000, Cell Signaling Technology), and mouse anti-glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (1:5000, ZSGB-BIO, Beijing, China), were incubated overnight. Then, horseradish peroxidase-conjugated anti-goat/rabbit/mouse (1:5000, ZSGB-BIO) IgGs were incubated for 1 h. The blots were visualized using the electrochemiluminescence method (Millipore) and imaged with a ChemiDocTM MP imaging system (Bio-Rad, Hercules, CA, USA).[31]
Immunofluorescence staining
Primary antibodies including rabbit anti-cleaved CASP-3 (1:200), goat anti-NLRP3 (1:200, Abcam), rabbit anti- RIPK3 (1:200), rabbit anti-TLR9 (1:200), and mouse anti- NeuN (1:500, Abcam) were used to detect TLR9 expression with neurons. Sections were incubated with DyLight Cy3 anti-rabbit IgG or Alexa488 anti-mouse IgG (1:500, Jackson ImmunoResearch, West Grove, PA, USA), and the nuclei were stained with 4′,6-diamidino-2-phenyl- indole (1:500, Beyotime). Five cortical regions from each rat were randomly selected. The fluorescent signal intensity of the target proteins was detected by a confocal laser scanning microscope (Olympus, Tokyo, Japan).[31]
Transmission electron microscope (TEM)
Cardiac perfusion was performed in rats with normal saline and 2% glutaraldehyde. About 1 mm3 cortical tissue was collected and fixed in glutaraldehyde. The tissue was embedded in epoxy resin and sectioned. The sections (0.12 μm) were stained with 1% uranium acetate. The ultrastructure of the neurons was observed by HT7700 120 kV TEM (Hitachi, Tokyo, Japan).[31]
Statistical analysis
Data were presented as mean ± standard deviation. The survival rate was calculated by the Kaplan-Meier method. The neurobehavioral score was analyzed by Friedman's repeated-measures analysis of variance (ANOVA). Twotailed t-test and one-way ANOVA were performed on group comparisons. All the statistical analyses were performed using SPSS version 19.0 software (IBM, Armonk, NY, USA). P value < 0.05 was considered statistically significant.
Results
A neonatal rat model with SAE was successfully established
To verify whether CLP successfully induced SAE in rats, a series of assessments were conducted. We found the survival rate was decreased especially at 12 to 24 h in the CLP group. The survival rates at all time points in sham group were 100% (30/30), while the survival rates at 3, 6, 12, 24, and 48 h in CLP group were 93.3% (28/30), 80.0% (24/30), 53.3% (16/30), 20.0% (6/30), and 13.3% (4/30), respectively [Supplementary Figure 1A]. In CLP group, the MAP gradually decreased from 6 h to its lowest point at 24 h, while HR gradually increased from 6 h and peaked at 24 h [Supplementary Figure 1B and 1C]. In addition, the neurobehavioral scores of the CLP group decreased significantly [Supplementary Figure 1D]. Pathological changes in the CLP group showed disordered cell arrangement and abnormal morphology (arrows) [Supplementary Figure 1E]. These findings are in accordance with the findings by Kafa et al,[29] which suggest that the model of SAE was successfully established.
PANoptosis activation in CLP-induced SAE rats
To study the death programs for nerve cells of CLP- induced SAE rats, we detected various death-related proteins. First, we found that cleaved/total CASP-3 was increased whereas Bcl-2 was decreased in the CLP group, indicating that apoptosis was activated [Figure 1A]. Second, we found that the pyroptosis-related proteins NLRP3 and cleaved/total CASP-1 were increased, indicating activation of pyroptosis [Figure 1B]. Finally, we found that all of the necroptosis-related proteins RIPK1, RIPK3, and phospho(p)-MLKL were increased, indicating activation of necroptosis [Figure 1C]. Additionally, we also observed the ultrastructure of cortical neurons by TEM [Figure 1D]. The morphology of neurons in the sham group was normal, with abundant organelles, and no obvious pathological changes. In the CLP-24 h group, apoptosis, pyroptosis, and necroptosis were observed. Apoptosis was characterized by cell atrophy, nucleo- cytoplasmic ratio increase, nuclear membrane invagination, and chromatin agglutination. Pyroptosis was mainly characterized by swelling of the cell, mitochondria, and other organelles, and loss of ribosomes. Necroptosis was characterized by overall cell morphological shrinkage, swelling of organelles, and severe vacuolization of the cytoplasm. Finally, to study which cell death program was dominant in SAE, immunofluorescence staining was performed for apoptosis-associated protein-cleaved caspase-3, pyroptosis-associated protein-NLRP3, and necroptosis-associated protein-RIPK3, to observe their positive cells in proportion to the total cells. The sum of apoptosis-, pyroptosis-, and necroptosis-positive cells was assumed to be 100%. Results showed that the percentage of apoptosis, pyroptosis, and necroptosis cells accounted for 41.2%, 32.2%, and 26.6% in PANoptosis cells, respectively [Supplementary Figure 2]. These results indicated that PANoptosis was activated in CLP-induced SAE rats in which apoptosis and pyroptosis were dominant and necroptosis played a secondary role.
Figure 1.
PANoptosis was activated in SAE rats. The protein levels of (A) caspase-3, Bcl-2, (B) NLRP3, caspase-1, (C) RIPK1, RIPK3, and p-MLKL in sham and CLP groups are shown, with GAPDH used as the loading control. n = 5. Data are represented by histograms, and sham group is normalized. ∗P < 0.05. All experiments were repeated three times and error bars depict mean ± standard deviation. (D) At 24 h after CLP, cortical neurons in sham and CLP groups were observed by TEM, and the morphology is normal in sham group, while CLP group shows the characteristics of apoptosis, pyroptosis, and necroptosis (arrows). Scale bar = 1 or 2 μm. CASP: Caspase; CLP: Cecal ligation and perforation; MLKL: Mixed lineage kinase domain-like protein; NLRP3: NOD-, LRR-, and pyrin domain-containing protein 3; PANoptosis: Pyroptosis, apoptosis, and necroptosis; RIPK: Receptor-interacting protein kinase; SAE: Sepsis associated encephalopathy; TEM: Transmission electron microscope.
Interaction of different cell death programs in PANoptosis
CLP induced SAE in rats, which resulted in various cell death programs. To study the role of different cell death programs in SAE and their interaction, specific inhibitors, including apoptosis inhibitor-Z-DEVD-FMK, pyroptosis inhibitor-INF39, and necroptosis inhibitor-Nec-1s, were administrated to SAE rats, respectively. The results showed that Z-DEVD-FMK inhibited pyroptosis but activated necroptosis while inhibiting apoptosis. Meanwhile, INF39 inhibited pyroptosis, it also inhibited apoptosis, but activated necroptosis. However, while Nec-1s inhibited necroptosis, both apoptosis and pyroptosis were activated [Supplementary Figure 3]. These results suggest that although the three cell death programs in PANoptosis were simultaneously activated by SAE, the interaction among them, specifically, was more likely to be synergistic between apoptosis and pyroptosis, which balanced necroptosis.
p38 MAPK, ERK, and JNK signaling pathways were activated in SAE rats
According to the previous research of our team, it is believed that the MAPKs can regulate PANoptosis.[22,31] By western blotting, we found that phosphorylated expression of MK2, the specific substrate downstream of p38 MAPK, was increased, and the p-ERK/ERK and p-JNK/JNK were increased [Supplementary Figure 4].[32] These findings suggested that p38 MAPK, ERK, and JNK pathways were activated in CLP-induced SAE rats.
p38 MAPK, ERK, and JNK pathways play a regulatory role in PANoptosis
To verify the regulatory role of MAPKs on PANoptosis in SAE, we administered SB203580, PD98059, and SP600125 to the rats. All three inhibitors inhibited apoptosis in CLP-induced SAE rats [Figure 2A]. Only SB203580 inhibited pyroptosis in CLP-induced SAE rats, whereas PD98059 and SP600125 had no obvious effect on pyroptosis [Figure 2B]. We further found that only SB203580 activated necroptosis [Figure 2C]. These results suggest that only p38 MAPK can simultaneously regulate apoptosis, pyroptosis, and necroptosis in CLP-induced SAE rats.
Figure 2.
The MAPKs regulate PANoptosis in SAE rats. Rats administered SB203580, PD98059, and SP600125, respectively. At 24 h after CLP, the protein levels of (A) caspase-3, Bcl-2, (B) NLRP3, caspase-1, (C) RIPK1, RIPK3, and p-MLKL in different groups are shown, with GAPDH used as the loading control. n = 5. Data are represented by histograms, and the sham group is normalized. ∗P < 0.05. All experiments were repeated three times and error bars depict mean ± standard deviation. CASP: Caspase. CLP: Cecal ligation and perforation; MAPK: Mitogen- activated protein kinase; MLKL: Mixed lineage kinase domain-like protein; NLRP3: NOD-, LRR-, and pyrin domain-containing protein 3; PANoptosis: Pyroptosis, apoptosis, and necroptosis; RIPK: Receptor-interacting protein kinase; SAE: Sepsis associated encephalopathy.
Necroptosis inhibition reactivated apoptosis and pyroptosis in SAE rats
Since apoptosis and pyroptosis were inhibited while necroptosis was activated after inhibition of the p38 MAPK, we investigated the effects of necroptosis inhibition on apoptosis and pyroptosis. We administered the necroptosis inhibitor Nec-1s under the action of SB203580 and found that Nec-1s inhibited necroptosis, while also reactivating the inhibited apoptosis and pyroptosis caused by SB203580 treatment [Figure 3]. Our findings suggested that necroptosis has a negative regulatory effect on apoptosis and pyroptosis in CLP-induced SAE rats.
Figure 3.
Further inhibition of necroptosis reactivated apoptosis and pyroptosis. Rats were further administered with Nec-1s based on SB203580. At 24 h after CLP, (A) caspase-3, Bcl-2, (B) NLRP3, caspase-1, (C) RIPK1, RIPK3, and p-MLKL in different groups are shown, with GAPDH used as the loading control. n = 5. Data are represented by histograms, and the sham group is normalized. ∗P < 0.05. All experiments were repeated three times and error bars depict mean ± standard deviation. CASP: Caspase; CLP: Cecal ligation and perforation; MLKL: Mixed lineage kinase domain-like protein; NLRP3: NOD-, LRR-, and pyrin domain-containing protein 3; RIPK: Receptor-interacting protein kinase.
TLR9 increased in SAE rats
Since TLR9, a regulator of inflammation, was found to promote B cell death through MAPKs, we wondered whether TLR9 could regulate PANoptosis in SAE through MAPKs.[33] We found that TLR9 expression was significantly increased from 6 h, and peaked at 24 h, as detected by western blotting in this model [Figure 4A]. The fluorescence signal of TLR9 was significantly enhanced in the CLP group, as detected by immunofluorescence staining [Figure 4B]. We also found that TLR9 colocalized primarily with neurons. These results suggest that TLR9 is activated in SAE rats.
Figure 4.
TLR9 expression is increased in SAE rats. (A) The protein levels of TLR9 in sham and CLP groups are shown, with GAPDH used as the loading control, and sham group is normalized. n = 5. (B) TLR9 (red) co-stains with NeuN (green) at 24 h after CLP. The arrowheads point to the overlap of red, green, and blue (DAPI). The IntDen of TLR9 was analyzed by Image J. Scale bar = 20 μm in magnified images. n = 5. Data are represented by histograms. ∗P < 0.05. All experiments were repeated three times and error bars depict mean ± standard deviation. CLP: Cecal ligation and perforation; SAE: Sepsis associated encephalopathy; TLR9: Toll-like receptor 9.
TLR9 regulated p38 MAPK and ERK pathways in SAE rats
The TLR9 inhibitor ODN2088 was administered to SAE rats, to study the regulatory effect of TLR9 on MAPKs. We found that p-MK2, the specific substrate downstream of p38 MAPK, and p-ERK were inhibited, while p-JNK was not changed significantly [Supplementary Figure 5]. These results suggest that TLR9 can regulate the p38 MAPK and ERK but not JNK in CLP-induced SAE rats.
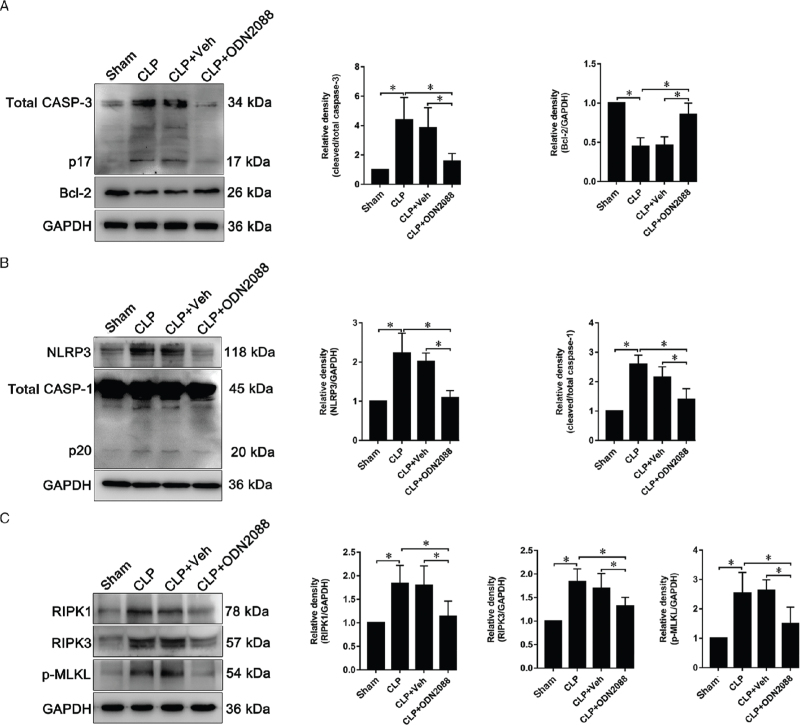
TLR9 activated PANoptosis in SAE rats
Since TLR9 can regulate the p38 MAPK and ERK, we wondered if TLR9 could regulate PANoptosis through these pathways. We found that cleaved/total CASP-3 was decreased, and Bcl-2 was increased after inhibition of TLR9 using ODN2088 [Figure 5A]. Furthermore, NLRP3 and cleaved/total CASP-1 were significantly inhibited [Figure 5B], which suggests that pyroptosis was suppressed. Additionally, necroptosis was also inhibited by ODN2088 because RIPK1, RIPK3, and p-MLKL were found to be decreased [Figure 5C]. These findings suggest that TLR9 could simultaneously regulate apoptosis, pyroptosis, and necroptosis in CLP-induced SAE rats.
Figure 5.
ODN2088 inhibited PANoptosis in SAE rats. At 24 h after CLP, (A) caspase-3, Bcl-2, (B) NLRP3, caspase-1, (C) RIPK1, RIPK3, p-MLKL in different groups are shown, with GAPDH used as the loading control. n = 5. Data are represented by histograms, and the sham group is normalized. ∗P < 0.05. All experiments were repeated three times and error bars depict mean ± standard deviation. CLP: Cecal ligation and perforation; MLKL: Mixed lineage kinase domain-like protein; NLRP3: NOD-, LRR-, and pyrin domain-containing protein 3; PANoptosis: Pyroptosis, apoptosis, and necroptosis; RIPK: Receptor-interacting protein kinase; SAE: Sepsis associated encephalopathy.
TLR9 inhibition improved survival rate and pathological changes in SAE rats
Since TLR9 activated PANoptosis in SAE rats, we wondered whether inhibition of TLR9 could protect SAE rats. We found that the administration of the TLR9 inhibitor, ODN2088, significantly increased the survival rate of SAE rats compared with the vehicle-treated rats. At 3, 6, 12, 24, and 48 h, the survival rate of sham group was 100% (30/30). In the CLP group, the survival rates were 96.7% (29/30), 76.7% (23/30), 53.3% (16/30), 23.3% (7/ 30), and 13.3% (4/30), respectively. In the CLP + Veh group, the survival rates were 93.3% (28/30), 70.0% (21/ 30), 50.0% (15/30), 20.0% (6/30), and 13.3% (4/30), respectively. Finally, in the CLP + ODN2088 group, the survival rates were 100% (30/30), 93.3% (28/30), 76.7% (23/30), 66.7% (20/30), and 60.0% (18/30), respectively [Figure 6A]. Furthermore, the pathological changes were rescued after inhibiting TLR9 in SAE rats [Figure 6B].
Figure 6.
Inhibition of TLR9 increased survival and improved cortical pathology in SAE rats. (A) Survival rate. n = 30. ∗P < 0.05. (B) At 24 h after CLP, cortical pathological changes were observed by H&E staining. Scale bar = 100 μm. n = 5. All experiments were repeated three times and error bars depict mean ± standard deviation. CLP: Cecal ligation and perforation; H&E: Hematoxylin and eosin; SAE: Sepsis associated encephalopathy; TLR9: Toll-like receptor 9.
Discussion
The roles of TLR9 in SAE and its related regulatory mechanisms are not clear. In this study, the role of TLR9 and its mechanisms in different cell death programs after SAE were studied. We found that SAE could induce PANoptosis. Among them, necroptosis regulated apoptosis and pyroptosis. In addition, the p38 MAPK pathway played an important role in regulating PANoptosis caused by TLR9. Further, inhibition of TLR9 had a neuro- protective effect on SAE in rats.
Sepsis often causes extensive cell death. Many damage- related factors released during cell death are directly involved in the development of sepsis. For many years, apoptosis has been the focus of cell death in sepsis. Recently, new cell death programs including pyroptosis and necroptosis have been found in sepsis, suggesting that cell death in sepsis is a complex process[11,34,35] Apoptosis is a common cell death program characterized by programmed DNA degradation, chromatin concentration, cell shrinkage, and fragmentation, and eventually the engulfment of cell fragments by macrophages[36,37] Apoptosis is a physiological self-destruction process, which helps the body to eliminate aging and abnormal cells and maintain normal function[4,38,39] The other two cell death programs, pyroptosis, and necroptosis, have been implicated in various auto-inflammatory conditions[40] Pyroptosis, driven by inflammasomes, is closely related to inflammation. By activating CASP-1, 4, 5, and 11, inflammation factors can cleave Gasdermin D at its N- terminus, creating a pore-forming domain, causing large pores to form in the cell membrane. These pores change the flow of extracellular fluid and affect the osmotic pressure gradient of the cells, and finally cause the cells to swell and rupture.[41–43] Necroptosis was found to be more sensitized after inhibition of apoptosis under the stimulation of inflammatory factors.[44] Necroptosis is also closely related to inflammation. Inflammatory factors, such as tumor necrosis factor, can signal RIPK1 to recruit RIPK3 and to form a necrosome, in which RIPK1 and RIPK3 interact with each other causing a series of cross-phosphorylation. Phosphorylated RIPK3 recruits and subsequently phosphorylates MLKL, which can penetrate the plasma membrane and organelles, resulting in membrane rupture and the spillage of cell contents.[45–47] The term PANoptosis was coined in recent years to emphasize the interaction and coordination of PANoptosis.[48] In this study, we found that PANoptosis exists in the cortical nerve cells of SAE rats, indicating that multiple cell death programs can be simultaneously triggered by SAE. It was further found that in the cortex of SAE rats, apoptosis and pyroptosis were dominant, while necroptosis was secondary. Apoptosis and pyroptosis cooperated to balance necroptosis.
The MAPK family plays an important role in cell proliferation and death. There are three main subfamilies of the MAPK family including p38 MAPK, ERK, and JNK. p38 MAPK negatively regulates cell cycle procession and eventually leads to cell death.[49] ERK is involved in many biological reactions such as proliferation and cytoskeleton construction.[50] JNK plays an important role in regulating cell proliferation and differentiation.[51] Since the MAPK family can regulate cellular proliferation, differentiation, and death, we further studied their regulatory effects on PANoptosis in SAE. We found that all of these three signaling pathways were activated after SAE. Our findings are similar to the previous findings that p38 MAPK, ERK, and JNK were activated in sepsis.[22,52] MAPKs may positively or negatively regulate cell death programs. Their effect on PANoptosis is closely regulated by the degree and duration of stimulation.[52] Through transcription-dependent or -independent mechanisms, MAPKs integrate signals in a cell-specific manner and activate cellular apoptosis.[53,54] In other studies, pyroptosis was found to be regulated by MAPKs in SAE and intracerebral hemorrhage models.[22,55] Recently, necroptosis was found to be regulated by MAPKs in liver and spleen of sepsis models.[56,57] Interestingly, we found, using specific MAPK inhibitors, only the p38 MAPK signaling pathway could simultaneously regulate the three PANoptosis pathways. Moreover, blocking the p38 MAPK activated necroptosis but inhibited apoptosis and pyroptosis. These findings suggest that p38 MAPK plays different roles in the programs forming PANoptosis; namely, p38 MAPK negatively regulated necroptosis but positively regulated apoptosis and pyroptosis in the SAE model. These data are consistent with the findings in HT-29 cells, glioblastoma multiform cells, and the intracerebral hemorrhage mouse model[55,58,59] It is possible that MK2, the downstream effector kinase of p38 MAPK, directly phosphorylates RIPK1, which causes inhibition of its kinase activity, and thereby inhibits necroptosis.[58,60] Another reason may be the interaction between apoptosis and necroptosis. Necroptosis was triggered after apoptosis was blocked, which is thought to be a “backup” defense mechanism. Previous studies have shown that activation of apoptosis inhibits necroptosis, whereas activation of necroptosis inhibits apoptosis.[40,61]
Necroptosis is a recently discovered cell death program, and it acts as a double-edged sword to the organism. It can maintain homeostasis by prohibiting responses to stress. Necroptosis can trigger the inflammatory cascade by releasing inflammatory factors such as interleukin[39] To investigate the differences in the regulation of p38 MAPK on necroptosis as well as apoptosis and pyroptosis in the SAE model, we further inhibited necroptosis and found that apoptosis and pyroptosis were reactivated. These findings were similar to the report of Fritsch et al[44] who found that blocking necroptosis could activate the inflammasome and promote apoptosis-mediated tissue pathology. Furthermore, inhibiting RIPK1 through kinase-dependent and non-dependent functions could inhibit necroptosis and then trigger inflammation, suggesting necroptosis plays a key role in inflammation.[62] Recently, Gasdermin E, a specific regulatory protein for pyroptosis, was found to be specifically cleaved by CASP-3 and thus induce pyropto-sis.[63] This means that activated apoptosis could trigger pyroptosis through cleaved Gasdermin E. Since necroptosis could inhibit apoptosis, its function in inhibiting pyroptosis may be due to its role in inhibiting apoptosis.
MAPKs signaling pathways are related to inflammatory cascades and were found to be involved in the regulation of PANoptosis in the SAE model. We further studied the regulatory mechanisms of MAPKs. TLR9, an inflammation-related protein, participates in the occurrence and development of sepsis. It was reported that TLR9 mediated the functional damage of multiple organs caused by sepsis.[19,64] Since multiple organ dysfunction is often seen in patients with SAE in the clinic, we investigated whether TLR9 expression was regulated in the SAE model. We found that TLR9 was significantly increased in SAE rats, suggesting that TLR9 activation may be one of the pathogenic causes of SAE. Recently, TLR9 was found to trigger cell death by initiating an inflammatory response under the condition of bacterial infection.[65,66] In this study, we found that after down-regulating TLR9, PANoptosis was significantly inhibited suggesting that TLR9 regulated PANoptosis in SAE. Although several previous studies have found that TLR9 could regulate apoptosis and pyroptosis in different disease models, our findings suggest a novel purpose for TLR9 function in regulating necroptosis.[20,67] Furthermore, this study also found that down-regulation of TLR9 inhibited p38 MAPK and ERK but not JNK, suggesting TLR9 is the upstream regulator of MAPKs in the SAE model. Therefore, we think that TLR9 regulation of PANoptosis might be through its action on the p38 MAPK signaling pathway in SAE. Although TLR9 could separately regulate inflammation through p38 MAPK pathway and regulate apoptosis by ERK signaling pathway, our findings suggested that TLR9 regulated PANoptosis through both p38 MAPK and ERK pathways in SAE.[68,69] We also found that TLR9 could not regulate JNK, which might be due to the fact that JNK is the upstream regulator of TLR9. This was confirmed by the finding that the deletion of TLR9 had no effect on the JNK signaling pathway.[70,71] In this study, we found that necroptosis was blocked by inhibiting TLR9 leading to p38 MAPK inhibition. However, inhibition of p38 MAPK alone could activate necroptosis. This difference may be due to the existence of different pathways such as NF- κB in regulating necroptosis.[72]
After inhibiting TLR9, we found that the survival rate of SAE rats was improved, and cortical pathological changes were alleviated. These findings support previous literature. For example, one study found that the deletion of TLR9 significantly eliminated the neutrophil-mediated inflammatory reaction and provided a protective effect.[73] In another study, researchers found that the deletion of TLR9 improved the heart function of rats with sepsis, suggesting that TLR9 is involved in sepsis-induced heart damage.[74]
In conclusion, our study showed that the cell death programs comprising PANoptosis occurred simultaneously in SAE rats. The results indicated that TLR9 activated PANoptosis by the p38 MAPK signaling pathway. Further, inhibition of TLR9 provided a neuroprotective effect in SAE rats. Hence, TLR9 may function as a potential target for the treatment of SAE.
Funding
This work was supported by grants from the National Natural Science Foundation of China (Nos. 81630038, 81771634, 81842011, 81801629, 81971433, 81971428, and 82071353), the National Key Research and Development Program (Nos. 2017YFA0104200 and 2017YFA0104201), the grants from the Science and Technology Bureau of Sichuan Province (Nos. 2021YJ0017 and 2020YFS0041), the Fundamental Research Funds for the Central University (No. SCU2020D006), and the National Key Project of Neonatal Children (No. 1311200003303).
Conflicts of interest
None.
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
How to cite this article: Zhou R, Ying J, Qiu X, Yu L, Yue Y, Liu Q, Shi J, Li X, Qu Y, Mu D. A new cell death program regulated by toll-like receptor 9 through p38 mitogen-activated protein kinase signaling pathway in a neonatal rat model with sepsis associated encephalopathy. Chin Med J 2022;135:1474–1485. doi: 10.1097/CM9.0000000000002010
Ruixi Zhou and Junjie Ying contributed equally to this work.
Supplemental digital content is available for this article.
References
- 1.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016; 315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sonneville R, de Montmollin E, Poujade J, Garrouste-Orgeas M, Souweine B, Darmon M, et al. Potentially modifiable factors contributing to sepsis-associated encephalopathy. Intensive Care Med 2017; 43:1075–1084. doi: 10.1007/s00134-017-4807-z. [DOI] [PubMed] [Google Scholar]
- 3.Stubbs DJ, Yamamoto AK, Menon DK. Imaging in sepsis-associated encephalopathy-insights and opportunities. Nat Rev Neurol 2013; 9:551–561. doi: 10.1038/nrneurol.2013.177. [DOI] [PubMed] [Google Scholar]
- 4.Galluzzi L, Vitale I, Aaronson SA, Abrams JM, Adam D, Agostinis P, et al. Molecular mechanisms of cell death: recommendations of the nomenclature committee on cell death 2018. Cell Death Differ 2018; 25:486–541. doi: 10.1038/s41418-017-0012-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang J, Zhou H. Mitochondrial quality control mechanisms as molecular targets in cardiac ischemia-reperfusion injury. Acta Pharm Sin B 2020; 10:1866–1879. doi: 10.1016/j.apsb.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Place DE, Lee S, Kanneganti TD. PANoptosis in microbial infection. Curr Opin Microbiol 2021; 59:42–49. doi: 10.1016/j.mib.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zheng M, Kanneganti TD. The regulation of the ZBP1-NLRP3 inflammasome and its implications in pyroptosis, apoptosis, and necroptosis (PANoptosis). Immunol Rev 2020; 297:26–38. doi: 10.1111/imr.12909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang GW, Bao JW, Shao XH, Zhou WY, Wu B, Ni ZH, et al. Inhibiting pannexin-1 alleviates sepsis-induced acute kidney injury via decreasing NLRP3 inflammasome activation and cell apoptosis. Life Sci 2020; 254:117791.doi: 10.1016/j.lfs.2020.117791. [DOI] [PubMed] [Google Scholar]
- 9.Zhang WX, He BM, Wu Y, Qiao JF, Peng ZY. Melatonin protects against sepsis-induced cardiac dysfunction by regulating apoptosis and autophagy via activation of SIRT1 in mice. Life Sci 2019; 217:8–15. doi: 10.1016/j.lfs.2018.11.055. [DOI] [PubMed] [Google Scholar]
- 10.Deng MH, Tang YT, Li WB, Wang XY, Zhang R, Zhang XY, et al. The endotoxin delivery protein HMGB1 mediates caspase-11- dependent lethality in sepsis. Immunity 2018; 49:740–753. e7. doi: 10.1016/j.immuni.2018.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sureshbabu A, Patino E, Ma KC, Laursen K, Finkelsztein EJ, Akchurin O, et al. RIPK3 promotes sepsis-induced acute kidney injury via mitochondrial dysfunction. JCI Insight 2018; 3:e98411.doi: 10.1172/jci.insight.98411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Banoth B, Tuladhar S, Karki R, Sharma BR, Briard B, Kesavardhana S, et al. ZBP1 promotes fungi-induced inflammasome activation and pyroptosis, apoptosis, and necroptosis (PANoptosis). J Biol Chem 2020; 25:18276–18283. doi: 10.1074/jbc.RA120.015924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karki R, Sharma BR, Lee E, Banoth B, Malireddi RKS, Samir P, et al. Interferon regulatory factor 1 regulates PANoptosis to prevent colorectal cancer. JCI Insight 2020; 18:e136720.doi: 10.1172/jci. insight.136720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen H, Li YS, Wu JF, Li GP, Tao X, Lai KM, et al. RIPK3 collaborates with GSDMD to drive tissue injury in lethal polymicrobial sepsis. Cell Death Differ 2020; 27:2568–2585. doi: 10.1038/s41418-020-0524-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heckmann BL, Tummers B, Green DR. Crashing the computer: apoptosis vs. necroptosis in neuroinflammation. Cell Death Differ 2019; 26:41–52. doi: 10.1038/s41418-018-0195-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Majer O, Liu B, Barton GM. Nucleic acid-sensing TLRs: trafficking and regulation. Curr Opin Immunol 2017; 44:26–33. doi: 10.1016/j. coi.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li L, Acioglu C, Heary RF, Elkabes S. Role of astroglial toll-like receptors (TLRs) in central nervous system infections, injury and neurodegenerative diseases. Brain Behav Immun 2021; 91:740–755. doi: 10.1016/j.bbi.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shepard CR. TLR9 in MAFLD and NASH: at the intersection of inflammation and metabolism. Front Endocrinol (Lausanne) 2021; 29:613639.doi: 10.3389/fendo.2020.613639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodríguez-Nuevo A, Díaz-Ramos A, Noguera E, Díaz-Sáez F, Duran X, Muñoz JP, et al. Mitochondrial DNA and TLR9 drive muscle inflammation upon Opa1 deficiency. EMBO J 2018; 37:e96553.doi: 10.15252/embj.201796553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu FY, Fan D, Yang Z, Tang N, Guo Z, Ma SQ, et al. TLR9 is essential for HMGB1-mediated post-myocardial infarction tissue repair through affecting apoptosis, cardiac healing, and angiogenesis. Cell Death Dis 2019; 10:480.doi: 10.1038/s41419-019-1718-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rittirsch D, Huber-Lang MS, Flierl MA, Ward PA. Immunodesign of experimental sepsis by cecal ligation and puncture. Nat Protoc 2009; 4:31–36. doi: 10.1038/nprot.2008.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou RX, Yang XY, Li XH, Qu Y, Huang Q, Sun XM, et al. Recombinant CC16 inhibits NLRP3/caspase-1-induced pyroptosis through p38 MAPK and ERK signaling pathways in the brain of a neonatal rat model with sepsis. J Neuroinflammation 2019; 16:239.doi: 10.1186/s12974-019-1651-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li L, Ni L, Eugenin EA, Heary RF, Elkabes S. Toll-like receptor 9 antagonism modulates astrocyte function and preserves proximal axons following spinal cord injury. Brain Behav Immun 2019; 80:328–343. doi: 10.1016/j.bbi.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 24.Thi PAN, Chen MH, Li N, Zhuo XJ, Xie L. PD98059 protects brain against cells death resulting from ROS/ERK activation in a cardiac arrest rat model. Oxid Med Cell Longev 2016; 2016:3723762.doi: 10.1155/2016/3723762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guan QH, Pei DS, Zhang QG, Hao ZB, Xu TL, Zhang GY. The neuroprotective action of SP600125, a new inhibitor of JNK, on transient brain ischemia/reperfusion-induced neuronal death in rat hippocampal CA1 via nuclear and non-nuclear pathways. Brain Res 2005; 1035:51–59. doi: 10.1016/j.brainres.2004.11.050. [DOI] [PubMed] [Google Scholar]
- 26.Stepanichev MY, Kudryashova IV, Yakovlev AA, Onufriev MV, Khaspekov LG, Lyzhin AA, et al. Central administration of a caspase inhibitor impairs shuttle-box performance in rats. Neuroscience 2005; 136:579–591. doi: 10.1016/j.neuroscience.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 27.Pu ZC, Han CZ, Zhang WW, Xu MD, Wu ZJ, Liu YH, et al. Systematic understanding of the mechanism and effects of Arctigenin attenuates inflammation in dextran sulfate sodium-induced acute colitis through suppression of NLRP3 inflammasome by SIRT1. Am J Transl Res 2019; 11:3992–4009. [PMC free article] [PubMed] [Google Scholar]
- 28.Takahashi N, Duprez L, Grootjans S, Cauwels A, Nerinckx W, DuHadaway JB, et al. Necrostatin-1 analogues: critical issues on the specificity, activity and in vivo use in experimental disease models. Cell Death Dis 2012; 3:e437.doi: 10.1038/cddis.2012.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kafa IM, Uysal M, Bakirci S, Kurt MA. Sepsis induces apoptotic cell death in different regions of the brain in a rat model of sepsis. Acta Neurobiol Exp (Wars) 2010; 70:246–260. [DOI] [PubMed] [Google Scholar]
- 30.Zhou RX, Li YY, Qu Y, Huang Q, Sun XM, Mu DZ, et al. Regulation of hippocampal neuronal apoptosis and autophagy in mice with sepsis-associated encephalopathy by immunity-related GTPase M1. CNS Neurosci Ther 2020; 26:177–188. doi: 10.1111/cns.13229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou RX, Qu Y, Huang Q, Sun XM, Mu DZ, Li XH. Recombinant CC16 regulates inflammation, oxidative stress, apoptosis and autophagy via the inhibition of the p38MAPK signaling pathway in the brain of neonatal rats with sepsis. Brain Res 2019; 1725:146473.doi: 10.1016/j.brainres.2019.146473. [DOI] [PubMed] [Google Scholar]
- 32.Menon MB, Gropengießer J, Fischer J, Novikova L, Deuretzbacher A, Lafera J, et al. p38 MAPK/MK2-dependent phosphorylation controls cytotoxic RIPK1 signalling in inflammation and infection. Nat Cell Biol 2017; 19:1248–1259. doi: 10.1038/ncb3614. [DOI] [PubMed] [Google Scholar]
- 33.Hancz A, Koncz G, Szili D, Sármay G. TLR9-mediated signals rescue B-cells from Fas-induced apoptosis via inactivation of caspases. Immunol Lett 2012; 143:77–84. doi: 10.1016/j.imlet.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Li N, Wang W, Zhou H, Wu QQ, Duan MX, Liu C, et al. Ferritinophagy-mediated ferroptosis is involved in sepsis-induced cardiac injury. Free Radic Biol Med 2020; 160:303–318. doi: 10.1016/j.freeradbiomed.2020.08.009. [DOI] [PubMed] [Google Scholar]
- 35.Liu L, Sun BW. Neutrophil pyroptosis: new perspectives on sepsis. Cell Mol Life Sci 2019; 76:2031–2042. doi: 10.1007/s00018-019-03060-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou H, Toan S, Zhu PJ, Wang J, Ren J, Zhang YM. DNA-PKcs promotes cardiac ischemia reperfusion injury through mitigating BI- 1-governed mitochondrial homeostasis. Basic Res Cardiol 2020; 115:11.doi: 10.1007/s00395-019-0773-7. [DOI] [PubMed] [Google Scholar]
- 37.Zhou H, Zhu PJ, Wang J, Zhu H, Ren J, Chen YD. Pathogenesis of cardiac ischemia reperfusion injury is associated with CK2α- disturbed mitochondrial homeostasis via suppression of FUNDC1- related mitophagy. Cell Death Differ 2018; 25:1080–1093. doi: 10.1038/s41418-018-0086-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kinloch RA, Treherne JM, Furness LM, Hajimohamadreza I. The pharmacology of apoptosis. Trends Pharmacol Sci 1999; 20:35–42. doi: 10.1016/s0165-6147(98)01277-2. [DOI] [PubMed] [Google Scholar]
- 39.Tower J. Programmed cell death in aging. Ageing Res Rev 2015; 23:90–100. doi: 10.1016/j.arr.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Frank D, Vince JE. Pyroptosis versus necroptosis: similarities, differences, and crosstalk. Cell Death Differ 2019; 26:99–114. doi: 10.1038/s41418-018-0212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kovacs SB, Miao EA. Gasdermins: effectors of pyroptosis. Trends Cell Biol 2017; 27:673–684. doi: 10.1016/j.tcb.2017.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shi JJ, Gao WQ, Shao F. Pyroptosis: gasdermin-mediated programmed necrotic cell death. Trends Biochem Sci 2017; 42:245–254. doi: 10.1016/j.tibs.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 43.Walle LV, Lamkanfi M. Pyroptosis. Curr Biol 2016; 26:R568–R572. doi: 10.1016/j.cub.2016.02.019. [DOI] [PubMed] [Google Scholar]
- 44.Fritsch M, Günther SD, Schwarzer R, Albert MC, Schorn F, Werthenbach JP, et al. Caspase-8 is the molecular switch for apoptosis, necroptosis and pyroptosis. Nature 2019; 575:683–687. doi: 10.1038/s41586-019-1770-6. [DOI] [PubMed] [Google Scholar]
- 45.Yuan JY, Amin P, Ofengeim D. Necroptosis and RIPK1-mediated neuroinflammation in CNS diseases. Nat Rev Neurosci 2019; 20:19–33. doi: 10.1038/s41583-018-0093-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhou H, Li DD, Zhu PJ, Ma Q, Toan S, Wang J, et al. Inhibitory effect of melatonin on necroptosis via repressing the Ripk3-PGAM5-CypD-mPTP pathway attenuates cardiac microvascular ischemiareperfusion injury. J Pineal Res 2018; 65:e12503.doi: 10.1111/jpi.12503. [DOI] [PubMed] [Google Scholar]
- 47.Zhu PJ, Hu SY, Jin QH, Li DD, Tian F, Toan S, et al. Ripk3 promotes ER stress-induced necroptosis in cardiac IR injury: a mechanism involving calcium overload/XO/ROS/mPTP pathway. Redox Biol 2018; 16:157–168. doi: 10.1016/j.redox.2018.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zheng Q, Wang YC, Liu QX, Dong XJ, Xie ZX, Liu XH, et al. FK866 attenuates sepsis-induced acute lung injury through c-jun-N-terminal kinase (JNK)-dependent autophagy. Life Sci 2020; 250:117551.doi: 10.1016/j.lfs.2020.117551. [DOI] [PubMed] [Google Scholar]
- 49.Hoppstädter J, Ammit AJ. Role of dual-specificity phosphatase 1 in glucocorticoid-driven anti-inflammatory responses. Front Immunol 2019; 10:1446.doi: 10.3389/fimmu.2019.01446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Burotto M, Chiou VL, Lee JM, Kohn EC. The MAPK pathway across different malignancies: a new perspective. Cancer 2014; 120:3446–3456. doi: 10.1002/cncr.28864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu QH, Wu WD, Fu BS, Shi L, Wang X, Kuca K. JNK signaling in cancer cell survival. Med Res Rev 2019; 39:2082–2104. doi: 10.1002/med.21574. [DOI] [PubMed] [Google Scholar]
- 52.Yue JC, López JM. Understanding MAPK signaling pathways in apoptosis. Int J Mol Sci 2020; 21:2346.doi: 10.3390/ijms21072346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sui XB, Kong N, Ye L, Han WD, Zhou JC, Zhang Q, et al. p38 and JNK MAPK pathways control the balance of apoptosis and autophagy in response to chemotherapeutic agents. Cancer Lett 2014; 344:174–179. doi: 10.1016/j.canlet.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 54.Wang J, Zhang WT, Ma B, Zhang HC, Fan ZY, Li MK, et al. A novel biscoumarin derivative dephosphorylates ERK and alleviates apoptosis induced by mitochondrial oxidative damage in ischemic stroke mice. Life Sci 2021; 264:118499.doi: 10.1016/j.lfs.2020.118499. [DOI] [PubMed] [Google Scholar]
- 55.Chen SP, Zuo YC, Huang L, Sherchan P, Zhang J, Yu ZT, et al. The MC 4 receptor agonist RO27-3225 inhibits NLRP1-dependent neuronal pyroptosis via the ASK1/JNK/p38 MAPK pathway in a mouse model of intracerebral haemorrhage. Br J Pharmacol 2019; 176:1341–1356. doi: 10.1111/bph.14639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chi QR, Wang DX, Hu XY, Li SP, Li S. Hydrogen sulfide gas exposure induces necroptosis and promotes inflammation through the MAPK/NF- (B pathway in broiler spleen. Oxid Med Cell Longev 2019; 2019:8061823.doi: 10.1155/2019/8061823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhao ZR, Zhang QJ, Xu CJ, Wang SC, Li JH, Liu ZY, et al. Methionine selenium antagonizes LPS-induced necroptosis in the chicken liver via the miR-155/TRAF3/MAPK axis. J Cell Physiol 2021; 236:4024–4035. doi: 10.1002/jcp.30145. [DOI] [PubMed] [Google Scholar]
- 58.Wu YH, Chou TF, Young L, Hsieh FY, Pan HY, Mo ST, et al. Tumor suppressor death-associated protein kinase 1 inhibits necroptosis by p38 MAPK activation. Cell Death Dis 2020; 11:305.doi: 10.1038/s41419-020-2534-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xu Y, Sun Q, Yuan FE, Dong HM, Zhang HK, Geng RX, et al. RND2 attenuates apoptosis and autophagy in glioblastoma cells by targeting the p38 MAPK signalling pathway. J Exp Clin Cancer Res 2020; 31:174.doi: 10.1186/s13046-020-01671-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jaco I, Annibaldi A, Lalaoui N, Wilson R, Tenev T, Laurien L, et al. MK2 phosphorylates RIPK1 to prevent TNF-induced cell death. Mol Cell 2017; 66:698–710. e5. doi: 10.1016/j.molcel.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schwabe RF, Luedde T. Apoptosis and necroptosis in the liver: a matter of life and death. Nat Rev Gastroenterol Hepatol 2018; 15:738–752. doi: 10.1038/s41575-018-0065-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schwarzer R, Laurien L, Pasparakis M. New insights into the regulation of apoptosis, necroptosis, and pyroptosis by receptor interacting protein kinase 1 and caspase-8. Curr Opin Cell Biol 2020; 63:186–193. doi: 10.1016/j.ceb.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 63.Wang YP, Gao WQ, Shi XY, Ding JJ, Liu W, He HB, et al. Chemotherapy drugs induce pyroptosis through caspase-3 cleavage of a gasdermin. Nature 2017; 547:99–103. doi: 10.1038/na- ture22393. [DOI] [PubMed] [Google Scholar]
- 64.Sekheri M, Kebir DE, Edner N, Filep JG. 15-Epi-LXA4 and 17-epi- RvD1 restore TLR9-mediated impaired neutrophil phagocytosis and accelerate resolution of lung inflammation. Proc Natl Acad Sci U S A 2020; 117:7971–7980. doi: 10.1073/pnas.1920193117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lai CY, Yu GY, Luo YP, Xiang R, Chuang TH. Immunostimulatory activities of CpG-oligodeoxynucleotides in teleosts: toll-like receptors 9 and 21. Front Immunol 2019; 10:179.doi: 10.3389/fimmu.2019.00179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu WC, Yang XJ, Wang N, Fan SJ, Zhu YF, Zheng XC, et al. Multiple immunosuppressive effects of CpG-c41 on intracellular TLR-mediated inflammation. Mediators Inflamm 2017; 2017:6541729.doi: 10.1155/2017/6541729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhao CC, Xie QM, Xu J, Yan XB, Fan XY, Wu HM. TLR9 mediates the activation of NLRP3 inflammasome and oxidative stress in murine allergic airway inflammation. Mol Immunol 2020; 125:24–31. doi: 10.1016/j.molimm.2020.06.016. [DOI] [PubMed] [Google Scholar]
- 68.Gu XL, Wu GN, Yao YW, Zeng JL, Shi DH, Lv TF, et al. Intratracheal administration of mitochondrial DNA directly provokes lung inflammation through the TLR9-p38 MAPK pathway. Free Radic Biol Med 2015; 83:149–158. doi: 10.1016/j.freerad- biomed.2015.02.034. [DOI] [PubMed] [Google Scholar]
- 69.Gao M, Ha TZ, Zhang X, Wang XH, Liu L, Kalbfleisch J, et al. The toll-like receptor 9 ligand, CpG oligodeoxynucleotide, attenuates cardiac dysfunction in polymicrobial sepsis, involving activation of both phosphoinositide 3 kinase/Akt and extracellular-signal-related kinase signaling. J Infect Dis 2013; 207:1471–1479. doi: 10.1093/infdis/jit036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hu K, Fu M, Wang J, Luo SK, Barreto M, Singh R, et al. HSV-2 infection of human genital epithelial cells upregulates TLR9 expression through the SP1/JNK signaling pathway. Front Immunol 2020; 11:356.doi: 10.3389/fimmu.2020.00356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wu HM, Shen QY, Fang L, Zhang SH, Shen PT, Liu YJ, et al. JNK- TLR9 signal pathway mediates allergic airway inflammation through suppressing melatonin biosynthesis. J Pineal Res 2016; 60:415–423. doi: 10.1111/jpi.12323. [DOI] [PubMed] [Google Scholar]
- 72.Kaiser WJ, Sridharan H, Huang CZ, Mandal P, Upton JW, Gough PJ, et al. Toll-like receptor 3-mediated necrosis via TRIF, RIP3, and MLKL. J Biol Chem 2013; 288:31268–31279. doi: 10.1074/jbc. M113.462341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yang ZG, Wang LW, Yu HM, Wang RN, Gou YW, Zhang MM, et al. Membrane TLR9 positive neutrophil mediated MPLA protects against fatal bacterial sepsis. Theranostics 2019; 9:6269–6283. doi: 10.7150/thno.37139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fattahi F, Russell MW, Malan EA, Parlett M, Abe E, Zetoune FS, et al. Harmful roles of TLR3 and TLR9 in cardiac dysfunction developing during polymicrobial Sepsis. Biomed Res Int 2018; 30:4302726.doi: 10.1155/2018/4302726. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.