Abstract
Hippocampal formation (HF) volume loss is a well-established finding in schizophrenia, with select subfields, such as the cornu ammonis and dentate gyrus, being particularly vulnerable. These morphologic alterations are related to functional abnormalities and cognitive deficits, which are at the core of the insufficient recovery frequently seen in this illness. To counteract HF volume decline, exercise to improve aerobic fitness is considered as a promising intervention. However, the effects of aerobic fitness levels on HF subfields are not yet established in individuals with schizophrenia. Therefore, our study investigated potential associations between aerobic fitness and HF subfield structure, functional connectivity, and related cognitive impact in a multiparametric research design. In this cross-sectional study, 53 participants diagnosed with schizophrenia (33 men, 20 women; mean [SD] age, 37.4 [11.8] years) underwent brain structural and functional magnetic resonance imaging and assessments of aerobic fitness and verbal memory. Multivariate multiple linear regressions were performed to determine whether aerobic fitness was associated with HF subfield volumes and functional connections. In addition, we explored whether identified associations mediated verbal memory functioning. Significant positive associations between aerobic fitness levels and volumes were demonstrated for most HF subfields, with the strongest associations for the cornu ammonis, dentate gyrus, and subiculum. No significant associations were found for HF functional connectivity or mediation effects on verbal memory. Aerobic fitness may mitigate HF volume loss, especially in the subfields most affected in schizophrenia. This finding should be further investigated in longitudinal studies.
Clinical Trials Registration: The study on which the manuscript is based was registered in the International Clinical Trials Database, ClinicalTrials.gov (NCT number: NCT03466112) and in the German Clinical Trials Register (DRKS-ID: DRKS00009804).
Subject terms: Hippocampus, Schizophrenia
Introduction
The hippocampal formation (HF) is a complex structure that lies within the medial temporal lobe and comprises several subfields along its longitudinal axis [1]. These subfields show a high degree of specialization with regard to cytoarchitecture and include the hippocampus proper, the Cornu ammonis (CA; subfields CA 1–3), the dentate gyrus (DG) with its polymorph layer as CA4, the presubiculum, and the subiculum complex [2–4].
The HF plays a vital role in memory, navigation, and cognition and is considered to be essential for episodic memory because it provides a spatial and temporal framework for experiences [5]. The subfields within the HF contribute in distinct ways to memory formation. Rostral HF subfields such as the DG and CA2/3 are needed for the encoding of novel information, whereas caudal HF subfields such as the subiculum enable the retrieval of existing memories [6, 7]. As a crucial requirement for its cognitive and memory functions, the HF is involved in a tightly interconnected network that includes its subfields and extrahippocampal areas [1, 5]. The fimbria and fornix represent the efferent system of the HF and have projections to the rest of the brain [1].
In the clinical context, the HF is considered to be particularly susceptible to neurodegeneration in aging [8] and to be one of the key brain regions involved in the pathophysiology of psychiatric disorders, as was supported by the results of large-scale neuroimaging studies [2, 3]. HF atrophy is a well-established feature in schizophrenia [9], and pathological changes seem to occur in a subfield-specific manner [10]. Selected subfields, such as CA1, CA4, the DG, and the subiculum, have been suggested to be particularly vulnerable to volumetric reductions even at an early stage of schizophrenia [11, 12]. More widespread subregional and progressive global volume decline seems to occur with longer illness duration [13]. In addition to volume reductions, functional abnormalities of the HF have been demonstrated [13].
An association between HF morphologic and physiological abnormalities and cognitive deficits in individuals with schizophrenia has been consistently shown [14–18]. At the subfield level, negative correlations between CA1, CA2/3, CA4/DG, and subiculum volumes and cognitive functioning in individuals with schizophrenia have been demonstrated, whereby verbal memory seems to be particularly affected [19–21].
To counteract neurodegenerative effects and promote neuroregeneration, engagement in physical activity, and especially in exercise to improve aerobic fitness, is considered as a promising intervention [22]. Large-scale meta-analyses suggest that aerobic exercise may have the potential to prevent age-related decline in HF volume in the healthy population [23, 24], and positive correlations between aerobic fitness levels and HF volumes have been demonstrated repeatedly in structural magnetic resonance imaging (sMRI) studies in healthy individuals [22, 25].
Functional magnetic resonance imaging (fMRI) studies on the effects of exercise on the HF are few in number and have been conducted almost exclusively in healthy participants. The available evidence indicates that aerobic exercise and higher aerobic fitness levels may promote functional connectivity between the HF and several brain regions that are critical for cognitive functioning, whereby the strongest effects were found for the parahippocampal gyrus, middle frontal gyrus, and cingulate gyrus [26–28].
Across different imaging methods, studies in healthy populations that yielded positive associations between aerobic fitness and the HF also tended to demonstrate cognitive benefits [22, 29, 30], but results in individuals with schizophrenia remain scarce and equivocal [31]. A randomized controlled trial showed improvements in verbal memory after a 3-month aerobic exercise intervention [32] but no significant increase in HF or its subfield volumes in any of the study groups [33]. Almost all other schizophrenia‐related brain imaging studies on the effects of exercise focused on the overall HF volume and not its subfield volumes, despite the divergent functions of the subfields and their varying vulnerability in schizophrenia. Thus, it remains unclear whether potential associations are global or whether specific subfields may be subject to more localized effects. Furthermore, there is a lack of multiparametric MRI studies that examine not only HF morphology but also integrate resting-state fMRI (rs-fMRI) to provide further insights into the health of the HF circuitry. Studies aiming to elucidate the associations between exercise and fitness and the HF should also assess the related cognitive functions, a topic that has often been neglected [22].
To the best of our knowledge, our study in individuals with schizophrenia is the first to investigate the interrelations between aerobic fitness, HF subfield structure, HF functional connectivity, and verbal memory in a multiparametric research design. We hypothesize that there are regional specific, positive associations between aerobic fitness and HF subfield volumes. In addition, we hypothesize that aerobic fitness is positively related to functional connectivity within the HF subfields and between the HF and the parahippocampal gyrus, middle frontal gyrus, and cingulate gyrus and that potential associations between aerobic fitness and the HF mediate verbal memory functioning in schizophrenia.
Methods and materials
The present study analyzed cross-sectional baseline (i.e., preintervention) data of participants in the Enhancing Schizophrenia Prevention and Recovery through Innovative Treatments (ESPRIT) C3 study.
Before participation in the study, participants provided written informed consent. All study procedures complied with the Declaration of Helsinki and were approved by the ethics committee of the Faculty of Medicine at the LMU Munich.
The C3 study, a multicenter, randomized, controlled, rater-blind clinical trial, investigated the effects of exercise on multiple levels in individuals with schizophrenia. In a two-armed parallel-group design, the study assigned participants either to an aerobic endurance training program on bicycle ergometers or a balance and tone training program as the control intervention.
To accurately measure the HF on its subfield level, a scanning resolution of less than 1 mm³ is recommended. Because this requirement was met only by the MRI scans performed at the C3 study center in Munich, the present study analyzed the data from this site.
Study sample
At the Munich site, MRI was performed in 76 participants with schizophrenia and a valid baseline assessment of aerobic fitness data was available for 53 participants. For sMRI analysis, five participants had to be excluded because of a lack of a 3D magnetization prepared rapid gradient echo (MPRAGE) sequence, low image quality, or errors in the segmentation process. For rs-fMRI analyses, data from nine participants were excluded because of incomplete echo-planar imaging (EPI) sequences or insufficient data quality (see Supplemental Information, Quality control of MRI data and decisions on data exclusion). Therefore, data from 48 participants (29 men, 19 women; mean (SD) age, 37.4 (11.8) years) were included in the sMRI analysis, whereas data from 44 participants (27 men, 17 women; mean (SD) age, 37.7 [11.8] years) were included in the rs-fMRI analysis (for details, see Supplemental Information, Sample characteristics). All participants were diagnosed with schizophrenia in accordance with the DSM-IV criteria. Further inclusion and exclusion criteria, as well as other study details, can be found in Maurus et al. [34].
Operationalization of aerobic fitness
While participants were exercising on a bicycle ergometer, a lactate threshold test was performed that provided assessed the lactate concentration in mmol/L in relation to the wattage in watts. Depending on the individual fitness level, lactate concentrations between 1.8 and 2.5 mmol/L represent the aerobic threshold, i.e., the level at which the lactate curve starts to rise exponentially [34, 35]. We identified the aerobic threshold for each participant and divided the achieved wattage at the aerobic threshold by body weight to ensure comparability of individuals. We used this value as the measure of aerobic fitness because it reflected each individual’s performance capability during aerobic exercise.
MRI data acquisition and pre-processing
MRI data were acquired at the LMU Hospital Munich in a whole-body 3.0 Tesla MRI Scanner (Magnetom Skyra, Siemens Healthineers, Erlangen, Germany). The MRI scan consisted of one 3D T1-weighted MPRAGE sequence and two EPI sequences (see Supplemental Information, Scanning parameters) and was performed during rest. tRaw data files from the scanners were converted with dcm2niix software from DICOM to NIFTI files [36], which in turn were embedded into BIDS format [37].
Pre-processing of the structural T1-weighted images was performed with Freesurfer v7.2 (see Supplemental Information, Pre-processing of MRI data) and included motion correction and averaging [38], removal of non-brain tissue [39], automated Talairach transformation, segmentation of the subcortical white matter and gray matter volumes [40, 41], intensity normalization [42], tessellation of the boundary between gray and white matter, automated topology correction [43, 44], and surface deformation [45–47].
Pre-processing of the functional EPI images was performed with fMRIPrep [48] (see Supplemental Information, Pre-processing of MRI data). Independent Component Analysis-based Automatic Removal Of Motion Artifacts (ICA-AROMA) was employed to compute noise regressors [49]. The first 10 dummy scans of every pre-processed rs-fMRI file were removed. A Gaussian filter was used for smoothing (full-width at half-maximum = 6 mm), and the Nilearn v0.8.0 clean_img function was used for confound regression. In line with current findings on different denoising strategies, global signal, cerebrospinal fluid, white matter, and the extracted noise components from ICA-AROMA were regressed out from blood oxygenation level-dependent (BOLD) time series [50].
Quality control of sMRI and rs-fMRI raw images was performed with the automated software MRIQC [51]. The quality of the pre-processed sMRI images was evaluated with VisualQC v0.3.7.1 [52], and rs-fMRI data quality was monitored by evaluating various quality metrics after pre-processing, smoothing, and denoising (see Supplemental Information, Quality control of MRI data and decisions on data exclusion).
MRI data post-processing
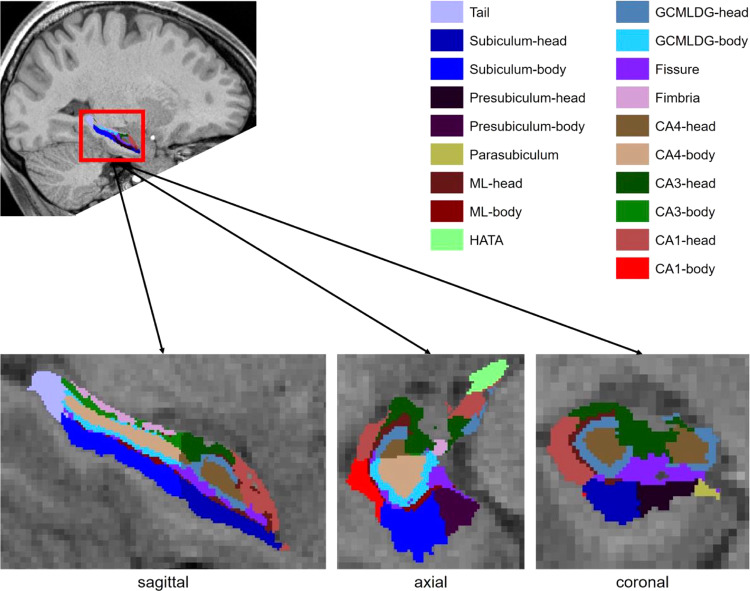
For sMRI data analysis, the volumes of 38 HF subfields (19 per hemisphere) were computed from the T1-weighted 3D sequence by using the current extension of the hippocampal module of Freesurfer v7.2 [53]. The resulting volumes were concatenated in one file and corrected by the intracranial volume utilizing proportions method [54]. Figure 1 illustrates the segmented HF subfields and their anatomical location (note that CA2 is included in CA3). For more details on the definition of HF subfields, see Table 1.
Fig. 1. Hippocampal formation subfields.
The hippocampal formation subfields segmented with Freesurfer v7.2 shown in different views. The table is based on Iglesias et al. [53] ML molecular layer, HATA hippocampal amygdala transition area, GCMLDG granule cell and molecular layer of the dentate gyrus, CA cornu ammonis.
Table. 1.
Subfields of the hippocampal formation.
| Name | Description |
|---|---|
| Tail | In the posterior part of the hippocampal formation |
| Subiculum | Divided into head and body; inferior part of the hippocampal formation |
| Presubiculum | Divided into head and body; inferior medial part of the hippocampal formation between the subiculum and parasubiculum (Brodmann 27) |
| Parasubiculum | Medial part of the hippocampal formation between the presubiculum and entorhinal cortex (Brodmann 49) |
| ML | Molecular layer: divided into head, body, and intermediate region, which contains parts of the subiculum or cornu ammonis (CA) fields |
| HATA | Hippocampus-amygdala transition area: superior medial part of the hippocampal formation |
| GCMLDG | Granule cell and molecular layer of the dentate gyrus: divided into head and body; between the molecular layer and CA4 |
| Fissure | Anterior medial part of the hippocampal formation; white matter structure |
| Fimbria | Posterior superior part of the hippocampal formation; white matter structure |
| CA4 | Cornu ammonis 4: inferior to the CA3 within the dentate gyrus |
| CA3 | Cornu ammonis 3: superior to the dentate gyrus; includes CA2 |
| CA1 | Cornu ammonis 1: anterior lateral part of the hippocampal formation |
Note. Description of the subfields of the hippocampal formation segmented with Freesurfer v7.2. For details on the segmentations, see Iglesias et al. [53].
For rs-fMRI data analysis, the NiftiLabelsMasker function from Nilearn v0.8.0 was used to extract the BOLD time series of seeds from the HF, parahippocampal gyrus, middle frontal gyrus, and cingulate gyrus as defined by the Brainnetome Atlas [55]. Functional connectivity between these participant-specific time series was computed with the ConnectivityMeasure function from Nilearn v0.8.0. Partial correlations were used to quantify functional connectivity, and the resulting correlation coefficients were converted to z-values with Fisher’s r-to-z transformation. For every participant, 166 functional connectivity measures were calculated that comprised functional connections between HF seeds, seeds from the HF and the parahippocampal gyrus, seeds from the HF and the middle frontal gyrus, and seeds from the HF and the cingulate gyrus. Table 2 provides a list of the examined seeds from the HF, parahippocampal gyrus, middle frontal gyrus, and cingulate gyrus based on the Brainnetome Atlas [55].
Table. 2.
Seeds of interest from the Brainnetome Atlas.
| Names of seeds from Brainnetome Atlas | Anatomical description |
|---|---|
| Hippocampus | |
| Hipp21 | Rostral hippocampus |
| Hipp22 | Caudal hippocampus |
| Parahippocampal gyrus | |
| PhG61 | Rostral area of Brodmann 35/36 |
| PhG62 | Caudal area of Brodmann 35/36 |
| PhG63 | Lateral posterior parahippocampal gyrus |
| PhG64 | Brodmann area 28/34 (entorhinal cortex) |
| PhG65 | Temporal agranular insular cortex |
| PhG66 | Medial posterior parahippocampal gyrus |
| Cingulate gyrus | |
| CG71 | Dorsal area of Brodmann 23 |
| CG72 | Rostroventral area of Brodmann 24 |
| CG73 | Pregenual area of Brodmann 32 |
| CG74 | Ventral area of Brodmann 23 |
| CG75 | Caudodorsal area of Brodmann 24 |
| CG76 | Caudal area of Brodmann 24 |
| CG77 | Subgenual area of Brodmann 32 |
| Middle frontal gyrus | |
| MFG71 | Dorsal area of Brodmann 9/46 |
| MFG 72 | Inferior frontal junction |
| MFG 73 | Brodmann area 46 |
| MFG 74 | Ventral area of Brodmann 9/46 |
| MFG 75 | Ventrolateral area of Brodmann 8 |
| MFG 76 | Ventrolateral of Brodmann 6 |
| MFG 77 | Lateral area of Brodmann 10 |
Note. The names of the examined seeds and their corresponding anatomical descriptions are taken from the Brainnetome Atlas [55].
Cognitive data
Several cognitive tests were administered as part of the baseline data collection of the ESPRIT C3 study. To investigate potential associations between HF subfield volumes and HF-dependent cognitive domains, we chose to analyze data from the Verbal Learning and Memory Test (VLMT) [56] because a meta-analysis showed that HF volume is associated with verbal learning in schizophrenia [18] and a previous study found exercise-induced improvements in the VLMT in individuals with this disease [57].
In the VLMT, immediately after a list of 15 words had been read out loud, participants were asked to recall as many words as possible from the list. This process was repeated five times in succession, whereby data from the first trial were analyzed (VLMT-first). Thereafter, an interference list of 15 different words was read out loud, and participants were asked to recall the words from this list (VLMT-inter). After the interference trial, participants were asked to immediately recall as many words as possible from the initial target list without it being presented again (VLMT-sixth). After a 20-minute delay, participants were asked to recall as many words as possible from the target list again (VLMT-seventh). The numbers of correctly recalled words in VLMT-first and VLMT-inter were z-standardized and summarized to a short-term verbal memory score (VLMT-STM), and the numbers of correctly recalled words in VLMT-sixth and VLMT-seventh were averaged to a long-term verbal memory score (VLMT-LTM), similar to the approach used in a previous study [57].
Statistical analyses
Rstudio v1.4.1717 based on R v4.1.2 was used for statistical data analyses [58, 59]. We detected outliers in the distributions of volumes, functional connectivity values, and VLMT scores (see Supplemental Information, Outlier detection). Age, sex, body mass index, disorder duration, education years, and chlorpromazine equivalents were defined as covariates, and chlorpromazine equivalents were computed by using the defined daily dose method [60]. Aerobic fitness values, volumes, VLMT scores, and all continuous covariables were z-standardized. After testing the corresponding pre-assumptions (see Supplemental Information, Tests of pre-assumptions of the multivariate multiple linear regression), two multivariate multiple linear regressions (MMLR) with aerobic fitness and the covariates as predictors and the volumes of 38 HF subfields and the 166 hippocampal functional connections as dependent variables were calculated with the MVLM package in R v4.1.2 [61]. If a significant main effect of aerobic fitness was found, mediation analyses with aerobic fitness as the independent variable, the hippocampal variables as mediators, and the VLMT-STM and -LTM scores as dependent variables were computed with the mediation package in R v4.1.2 [62]. Visualizations were performed with ggplot2 package in R v4.1.2 [63].
Results
Relation between aerobic fitness and the volumes of the HF subfields
Table 3 summarizes the results from the MMLR analysis predicting the volumes of the HF subfields on the basis of aerobic fitness and the covariates. The overall MMLR model was not significant (R2pseudo = 0.196, T(7) = 1.393, p = 0.059), but aerobic fitness significantly predicted the volumes of the HF subfields (T(1) = 3.639, R2pseudo = 0.073, p = 0.003). The covariates were not significant.
Table. 3.
Results from the multivariate multiple linear regression predicting volumes of the hippocampal formation subfields.
| Predictor | T(df) | R²pseudo | p |
|---|---|---|---|
| Omnibus effect1 | 1.393(7) | 0.196 | 0.059 |
| Aerobic fitness | 3.639(1) | 0.073 | 0.003* |
| Age | 1.203(1) | 0.024 | 0.267 |
| Sex | 1.136(1) | 0.023 | 0.305 |
| Body mass index | 1.538(1) | 0.031 | 0.139 |
| Education years | 0.496(1) | 0.010 | 0.875 |
| Disorder duration | 0.680(1) | 0.012 | 0.692 |
| Chlorpromazine equivalents | 1.483(1) | 0.030 | 0.155 |
1The omnibus effect represents the effect of the whole multivariate multiple linear regression model with n = 48.
Significant p values (<0.05) are written in bold and marked with an asterisk.
R²pseudo, effect size similar to the coefficient of determination; T(df), test statistics with numerator degrees of freedom.
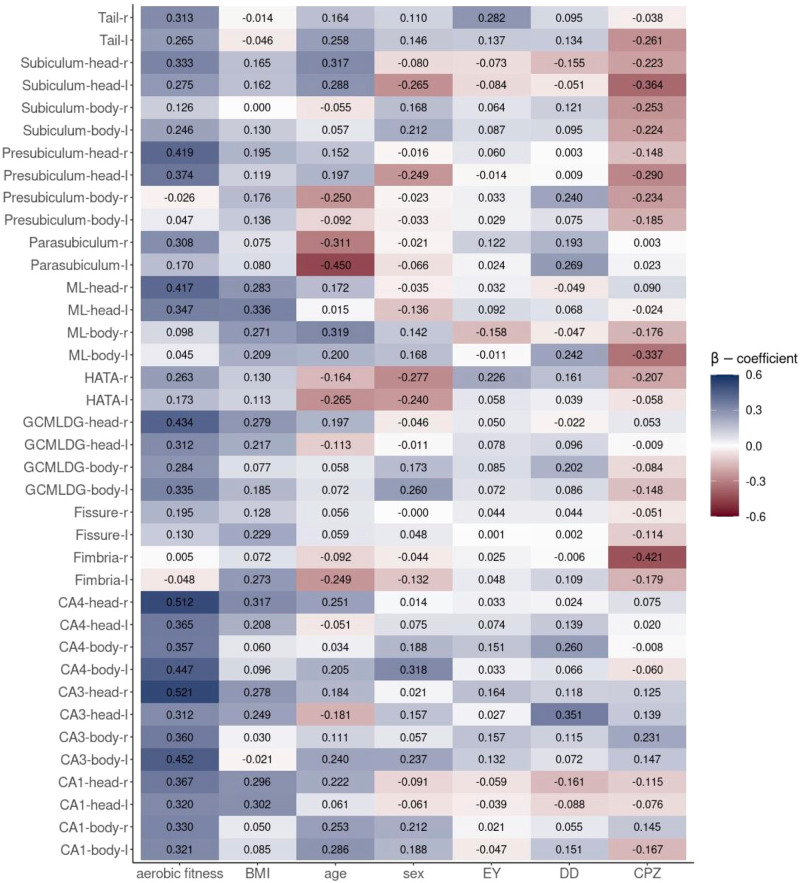
Figure 2 illustrates the regression coefficients β and indicates the size and direction of the effect of the predictors on volumes of each of the HF subfields. Aerobic fitness showed constant positive effects on all HF subfields apart from the bilateral fimbria and the bilateral bodies of the presubiculum and ML.
Fig. 2. β-coefficients of aerobic fitness and the covariates predicting volumes of the hippocampal formation subfields.
The x-axis shows the predictors of the multivariate multiple linear regression, and the y-axis, the 38 hippocampal formation subfields from both hemispheres. The heatmap is filled with the β-coefficients. Blue indicates a positive effect, red a negative effect. The darker the color, the stronger is the effect in the corresponding direction. BMI body mass index, CA cornu ammonis, CPZ chlorpromazine equivalents, DD disorder duration, EY education years, GCMLDG granule cell and molecular layer of the dentate gyrus HATA hippocampal amygdala transition area, l left hemisphere, ML molecular layer, r right hemisphere.
Relation between aerobic fitness and static functional connectivity of the HF
Table 4 summarizes the results from the MMLR analysis predicting functional connectivity of seeds from the HF (Table 2) on the basis of aerobic fitness and the covariates. Neither the overall MMLR model (R2pseudo = 0.16, T(7) = 1.01, p = 0.442) nor the predictors were significant. The figures that visualize the regression β-coefficients indicating the size and direction of the effect of the predictors on the functional connectivity of seeds from the HF can be found in the Supplemental Information (Fig. S7.1 and S7.2).
Table. 4.
Results from the multivariate multiple linear regression predicting functional connectivity of seeds from the hippocampal formation.
| Predictor | T(df) | R²pseudo | p |
|---|---|---|---|
| Omnibus effecta | 1.01(7) | 0.16 | 0.442 |
| Aerobic fitness | 1.04(1) | 0.02 | 0.399 |
| Age | 0.92(1) | 0.02 | 0.597 |
| Sex | 0.86(1) | 0.02 | 0.691 |
| Body mass index | 1.13(1) | 0.03 | 0.274 |
| Education years | 1.14(1) | 0.03 | 0.262 |
| Disorder duration | 1.05(1) | 0.02 | 0.391 |
| CPZ | 0.87(1) | 0.02 | 0.682 |
aThe omnibus effect represents the effect of the whole MMLR model with n = 44.
R²pseudo = effect size similar to the coefficient of determination; T(df), test statistics with numerator degrees of freedom.
Mediation effects of volumes of the HF subfields
The HF subfields that showed a positive association with aerobic fitness were used as mediators between aerobic fitness and the VLMT-STM and -LTM scores, resulting in 64 separate mediation analyses. No significant mediation effects were observed after controlling for the false discovery rate. Regarding the VLMT-STM score, significant positive mediation effects (evaluated with uncorrected p values) were observed for the body of the left GCMLDG and the body of the left CA4 (Table 5). Regarding the VLMT-LTM score, a significant positive mediation effect (evaluated with uncorrected p values) was found for the body of the left GCMLDG, but a negative effect was found for the head of the left subiculum (Table 6).
Table. 5.
Mediation between aerobic fitness, hippocampal formation subfield volumes, and Verbal Learning and Memory Test short-term memory scores.
| Mediator | ACME | CIlow | CIhigh | p | pfdr |
|---|---|---|---|---|---|
| Tail-r | 0.061 | −0.043 | 0.202 | 0.254 | 0.855 |
| Tail-l | 0.102 | −0.006 | 0.255 | 0.060 | 0.480 |
| Subiculum-head-r | 0.004 | −0.144 | 0.150 | 0.942 | 0.958 |
| Subiculum-head-l | −0.053 | −0.202 | 0.057 | 0.358 | 0.855 |
| Subiculum-body-r | 0.059 | −0.021 | 0.193 | 0.186 | 0.792 |
| Subiculum-body-l | 0.046 | −0.038 | 0.177 | 0.312 | 0.855 |
| Presubiculum-head-r | −0.010 | −0.173 | 0.158 | 0.840 | 0.958 |
| Presubiculum-head-l | 0.011 | −0.156 | 0.159 | 0.848 | 0.958 |
| Parasubiculum-r | −0.006 | −0.125 | 0.099 | 0.926 | 0.958 |
| Parasubiculum-l | −0.031 | −0.140 | 0.033 | 0.434 | 0.855 |
| ML-head-r | 0.029 | −0.110 | 0.179 | 0.692 | 0.886 |
| ML-head-l | 0.025 | −0.126 | 0.183 | 0.684 | 0.886 |
| HATA-r | 0.122 | −0.001 | 0.286 | 0.054 | 0.480 |
| HATA-l | 0.029 | −0.084 | 0.159 | 0.592 | 0.886 |
| GCMLDG-head-r | 0.038 | −0.120 | 0.216 | 0.648 | 0.886 |
| GCMLDG-head-l | 0.045 | −0.082 | 0.191 | 0.448 | 0.855 |
| GCMLDG-body-r | 0.089 | −0.015 | 0.235 | 0.106 | 0.678 |
| GCMLDG-body-l | 0.185 | 0.040 | 0.381 | 0.008* | 0.256 |
| Fissure-r | 0.060 | −0.027 | 0.189 | 0.198 | 0.792 |
| Fissure-l | 0.038 | −0.061 | 0.171 | 0.448 | 0.855 |
| CA4-head-r | 0.059 | −0.127 | 0.263 | 0.506 | 0.886 |
| CA4-head-l | 0.067 | −0.067 | 0.228 | 0.336 | 0.855 |
| CA4-body-r | 0.093 | −0.033 | 0.260 | 0.160 | 0.792 |
| CA4-body-l | 0.156 | 0.013 | 0.339 | 0.030* | 0.480 |
| CA3-head-r | 0.068 | −0.092 | 0.248 | 0.358 | 0.855 |
| CA3-head-l | 0.039 | −0.056 | 0.176 | 0.454 | 0.855 |
| CA3-body-r | −0.004 | −0.106 | 0.099 | 0.958 | 0.958 |
| CA3-body-l | −0.024 | −0.164 | 0.106 | 0.662 | 0.886 |
| CA1-head-r | 0.043 | −0.114 | 0.220 | 0.576 | 0.886 |
| CA1-head-l | 0.032 | −0.126 | 0.211 | 0.666 | 0.886 |
| CA1-body-r | 0.007 | −0.113 | 0.126 | 0.878 | 0.958 |
| CA1-body-l | 0.010 | −0.112 | 0.139 | 0.896 | 0.958 |
Note. The table shows the results of 32 mediation analyses with n = 47. The hippocampal formation subfields that were associated with aerobic fitness were used as mediators between aerobic fitness and short-term verbal memory performance.
Significant p values (<0.05) are written in bold and marked with an asterisk.
ACME average causal mediation effect, CIlow, lower confidence interval, CIhigh higher confidence interval, p uncorrected p value, pfdr fdr-corrected p value.
Table. 6.
Mediation between aerobic fitness, hippocampal formation subfield volumes, and Verbal Learning and Memory Test long-term memory scores.
| Mediator | ACME | CIlow | CIhigh | p | pfdr |
|---|---|---|---|---|---|
| Tail-r | 0.037 | −0.089 | 0.190 | 0.520 | 0.776 |
| Tail-l | 0.043 | −0.080 | 0.202 | 0.530 | 0.776 |
| Subiculum-head-r | −0.060 | −0.233 | 0.068 | 0.366 | 0.776 |
| Subiculum-head-l | −0.128 | −0.316 | −0.009 | 0.020* | 0.640 |
| Subiculum-body-r | 0.028 | −0.043 | 0.133 | 0.486 | 0.776 |
| Subiculum-body-l | 0.027 | −0.061 | 0.148 | 0.546 | 0.776 |
| Presubiculum-head-r | −0.021 | −0.207 | 0.145 | 0.790 | 0.832 |
| Presubiculum-head-l | −0.051 | −0.247 | 0.106 | 0.538 | 0.776 |
| Parasubiculum-r | 0.055 | −0.057 | 0.198 | 0.346 | 0.776 |
| Parasubiculum-l | −0.025 | −0.132 | 0.047 | 0.558 | 0.776 |
| ML-head-r | −0.071 | −0.253 | 0.080 | 0.342 | 0.776 |
| ML-head-l | −0.107 | −0.297 | 0.034 | 0.130 | 0.776 |
| HATA-r | 0.052 | −0.088 | 0.223 | 0.484 | 0.776 |
| HATA-l | −0.023 | −0.146 | 0.094 | 0.682 | 0.832 |
| GCMLDG-head-r | −0.115 | −0.308 | 0.052 | 0.186 | 0.776 |
| GCMLDG-head-l | −0.041 | −0.205 | 0.101 | 0.548 | 0.776 |
| GCMLDG-body-r | 0.062 | −0.057 | 0.217 | 0.322 | 0.776 |
| GCMLDG-body-l | 0.141 | 0.007 | 0.320 | 0.040* | 0.640 |
| Fissure-r | 0.014 | −0.097 | 0.144 | 0.806 | 0.832 |
| Fissure-l | 0.028 | −0.084 | 0.156 | 0.586 | 0.781 |
| CA4-head-r | −0.101 | −0.319 | 0.090 | 0.280 | 0.776 |
| CA4-head-l | −0.020 | −0.192 | 0.127 | 0.768 | 0.832 |
| CA4-body-r | 0.070 | −0.065 | 0.248 | 0.330 | 0.776 |
| CA4-body-l | 0.130 | −0.026 | 0.331 | 0.122 | 0.776 |
| CA3-head-r | −0.107 | −0.298 | 0.069 | 0.216 | 0.776 |
| CA3-head-l | 0.016 | −0.099 | 0.150 | 0.780 | 0.832 |
| CA3-body-r | −0.023 | −0.161 | 0.073 | 0.704 | 0.832 |
| CA3-body-l | 0.023 | −0.106 | 0.166 | 0.702 | 0.832 |
| CA1-head-r | −0.124 | −0.328 | 0.037 | 0.126 | 0.776 |
| CA1-head-l | −0.086 | −0.273 | 0.067 | 0.278 | 0.776 |
| CA1-body-r | −0.055 | −0.202 | 0.060 | 0.352 | 0.776 |
| CA1-body-l | −0.007 | −0.155 | 0.136 | 0.882 | 0.882 |
Note. The 32 mediation analyses with n = 47 are listed. The hippocampal formation subfields that were associated with aerobic fitness were used as mediators between aerobic fitness and long-term memory performance.
Significant p values (<0.05) are written in bold and marked with an asterisk.
ACME average causal mediation effect, CIlow lower confidence interval, CIhigh higher confidence interval, p uncorrected p value, pfdr fdr-corrected p value.
Discussion
The main finding of our multi-parametric MRI-based study was that higher aerobic fitness levels were associated with higher volumes in the majority of HF subfields, especially in CA1 to CA4, the DG, and the subiculum. In our analyses of HF functional connectivity with the parahippocampal gyrus, no significant results were found for the middle frontal gyrus or cingulate gyrus. In addition, after controlling for the false discovery rate, no stable mediation effects were seen on the impact of relevant associations between aerobic fitness and HF subfield volume on verbal short- and long-term memory performance assessed with the VLMT.
Meta-analyses of randomized clinical trials concluded that aerobic exercise may prevent a decline in total HF volume, but significant results depended on the sample [23] and intervention characteristics [22–25, 64]. Older participants, who are more prone to neurodegeneration, benefitted the most from exercise interventions. Neurodegenerative processes have been suspected also in people with schizophrenia, but findings to date on the effect of exercise on HF volume remain scarce and inconclusive [23, 31, 65]. Within this debate, our study strengthens the notion of a positive relation between aerobic fitness and HF volume in schizophrenia.
The lack of previous cross-sectional studies on the interrelations between HF subfield volumes and aerobic fitness in individuals with schizophrenia complicates direct comparisons. At first glance, our results appear to differ from those of a single interventional study that considered the effects of exercise on the subfield level in participants with schizophrenia and observed no significant increase in the HF subfield volumes of the whole group after three months’ aerobic exercise training [33]. However, a post hoc analysis found a significant effect on CA3 and CA4 volume and functional recovery in about half of the patients under study [66]. Importantly, this trial evaluated the effects of a relatively short-term exercise intervention on HF subfield volumes, whereas our current cross-sectional study targeted the effect of general aerobic fitness, which depends on participants’ longer-term exercise involvement. In accordance with previous studies that demonstrated that longer exercise interventions yield more robust effects [22, 24], the divergent findings on the group level suggest that a greater increase in aerobic fitness could be a critical precondition for effects of exercise on HF volume.
A secondary analysis of the aforementioned study indicated that exercise-induced increases (or smaller decreases) of CA4 and DG volumes were modulated by participants’ individual polygenic risk scores for schizophrenia [67, 68] and by their cell-specific risk scores associated with oligodendrocyte precursor cells and radial glia [69]. When taken together, the former and present findings appear to indicate that aerobic fitness may be related to higher volumes of HF subfields in individuals with schizophrenia and that the underlying neuroplastic processes may be modulated by polygenic burden. In line with the literature on healthy individuals, the strongest effects were shown for CA1 to CA4, the DG, and the subiculum. These subfields are the most vulnerable to volumetric reductions, even at an early stage of schizophrenia [11, 12]. As a consequence, an association between aerobic fitness and total HF volume might be driven by regionally more specific associations within particular subfields. Thus, aerobic fitness might have the potential to mitigate schizophrenia-specific neurodegeneration or failed neuroregeneration, especially in the most affected HF subfields.
Considering the cognitive relevance of relations between aerobic fitness and the HF, our study does not support the hypothesis that aerobic fitness has a positive impact on verbal short- and long-term memory by increasing HF subfield volumes. In individuals with schizophrenia, our study was the first to examine these interrelations cross-sectionally, which again complicates direct comparisons with earlier research. In contrast to our findings, a previous interventional study in participants with schizophrenia reported that enhancements in aerobic fitness were related to increased total HF volume, which in turn was accompanied by improvement in short-term memory as assessed with the VLMT [57]. This interventional study considered only total HF volume, whereas we focused specifically on HF subfields and used a cross-sectional design. In addition, the two studies used different methods to compute HF volumes.
Some studies in healthy participants reported partially positive interrelations between aerobic fitness, HF subfield volumes (CA1, CA3/DG), and improved cognitive functioning [70–72], but associations tended to be weak. Future studies of HF subfield volumes need to include larger sample sizes for robust findings [13] because the positive interrelations between aerobic fitness and HF subfield volumes may hold true only for a subgroup of participants, analogous to the findings on plasticity with other kinds of interventions [73].
Concerning our rs-fMRI analysis, we did not detect associations between aerobic fitness and functional connectivity within the HF or between HF seeds and seeds from the parahippocampal gyrus, middle frontal gyrus, and cingulate gyrus (Table 2). In contrast, a previous study in participants with schizophrenia suggested that exercise-induced increases in hippocampal-prefrontal functional connectivity led to benefits in spatial memory [74], and another exploratory study in young adults at ultrahigh risk for psychosis demonstrated beneficial effects of aerobic exercise only on hippocampal-occipital functional connectivity [75]. However, research on the impact of aerobic fitness and exercise on HF functional connectivity in individuals with schizophrenia is very limited to date, and no comprehensive conclusions can be drawn yet. To our knowledge, our current study is the largest so far to address this research question. In healthy and other clinical populations, several widespread alterations in hippocampal functional connectivity related to aerobic fitness or exercise have been identified, but findings also are inconclusive [22, 28, 64, 76]. Again, differing study populations and methodological differences likely contribute to the discrepancies between findings.
To date, there is still a lack of multiparametric studies that not only examine hippocampal morphology but also attempt to provide further insights by integrating rs-fMRI data. We aimed to address this research gap and to assess not only the relation of aerobic fitness to HF subfield morphology but also the related cognitive impact. One of the major strengths of the present work is that it is one of the first studies in the field to focus on HF subfields with their divergent functions and varying vulnerability in schizophrenia, instead of investigating only total HF volume. In our study, we carefully considered covariables that might be associated with the variables of interest, and we could validate the results of our statistical model in the majority of the robustness checks (see Supplemental Information, Robustness checks of the MMLR). Furthermore, our data were obtained from participants with the same diagnosis and a relatively similar age; this homogeneity is important to avoid confounders, which tend to vary systematically between patient and control groups and within samples of different ages [77].
Our study has several limitations. First, we cannot rule out the presence of additional confounding factors. For example, in female study participants the menstrual cycle phase has been linked to changes in hippocampal connectivity [78] but was not assessed in our study. Second, our analyses required T1-weighted sequences at submillimeter voxel resolution, which were available only from a single study center. Even though our imaging protocol used a very high, state-of-the-art spatial resolution, the spatial resolution might still have been insufficient to assess all relevant anatomical variations [13]. Third, our study was cross-sectional in design, so caution should be exercised when interpreting the results for causality [79]. Fourth, the statistical power of the study was limited, increasing the risk that we missed potential small effects (see Supplemental Information, Post hoc power analyses). Therefore, the current results should be replicated in an independent sample. Last, for practical reasons genetic risk factors and subgroup characteristics were not accounted for in our study but might explain some of the heterogeneity observed [66, 68, 69, 80] and should be included in future investigations. In addition, future studies could use different HF-dependent tasks (for example, tasks targeting spatial memory) to evaluate whether cognitive functions other than verbal memory are more strongly associated with HF morphology.
Because of the key role of the hippocampus in memory formation and the changes in hippocampal volume seen in schizophrenia, we aimed to increase the knowledge about which parts of hippocampal structure and function are particularly interrelated with the effects of exercise. We showed that higher aerobic fitness levels were associated with higher volumes in the majority of HF subfields, with the strongest effects in CA1 to CA4, the DG, and the subiculum. These findings should be further investigated in longitudinal studies. Furthermore, despite the need for cautionary interpretation of our cross-sectional findings, we believe that they hold promise for a deeper understanding of the effects of exercise and the potential application of exercise as an add-on therapeutic approach in people with schizophrenia.
Supplementary information
Acknowledgements
We thank the Clinical Trials Center Cologne (CTC Cologne) for developing the database and performing data management and monitoring. Furthermore, they express their appreciation to the Clinical Open Research Engine (CORE) at the University Hospital LMU (Munich, Germany) for providing the computational infrastructure to run the CPU-intensive MRI analysis pipelines. We also thank Jacquie Klesing, BMedSci (Hons), Board-certified Editor in the Life Sciences (ELS), for editing assistance with the manuscript; Ms. Klesing received compensation for her work from the LMU Munich, Germany. The work was supported by the German Federal Ministry of Education and Research (BMBF) through the research network on psychiatric diseases ESPRIT (Enhancing Schizophrenia Prevention and Recovery through Innovative Treatments; coordinator, Andreas Meyer-Lindenberg; grant number, 01EE1407E) to AML, PF, AH, and AS. Furthermore, the study was supported by the Else Kröner-Fresenius Foundation to PF, AS, and IM (Residency/PhD track of the International Max Planck Research School for Translational Psychiatry [IMPRS-TP]). The “Studienstiftung des deutschen Volkes” provided a PhD scholarship to Lukas Röll.
Author contributions
PF, DH, AML, AS, BM, and AH were involved in the conception and design of the study. IM and LR were involved in acquisition, analysis and interpretation of data, manuscript writing, revision and final approval of the version to be submitted. DK, BP, SS and BEW have assisted with MRI data acquisition and analysis. EW, AR and IP assessed clinical data. ML conducted fitness assessments. All authors were involved in revising the article, read and approved the final version of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Data availability
Imaging data, results from the quality control, the scripts for the whole analysis as well as demographic, physical, clinical and cognitive data files are published on OSF (Identifier: 10.17605/OSF.IO/TR3NX). Additional data will be made available upon request.
Competing interests
AS was an honorary speaker for TAD Pharma and Roche and a member of Roche advisory boards. AH is an editor of the German (DGPPN) schizophrenia treatment guidelines and first author of the WFSBP schizophrenia treatment guidelines; he has been on the advisory boards of and has received speaker fees from Janssen-Cilag, Lundbeck, Recordati, Rovi, and Otsuka. PF is a co-editor of the German (DGPPN) schizophrenia treatment guidelines and a co-author of the WFSBP schizophrenia treatment guidelines; he is on the advisory boards and receives speaker fees from Janssen, Lundbeck, Otsuka, Servier, and Richter. AML has received consultant fees from Boehringer Ingelheim, Elsevier, Brainsway, Lundbeck Int. Neuroscience Foundation, Lundbeck A/S, Sumitomo Dainippon Pharma Co., Academic Medical Center of the University of Amsterdam, Synapsis Foundation-Alzheimer Research Switzerland, IBS Center for Synaptic Brain Dysfunction, Blueprint Partnership, University of Cambridge, Dt. Zentrum für Neurodegenerative Erkrankungen, Zürich University, Brain Mind Institute, L.E.K. Consulting, ICARE Schizophrenia, Science Advances, Fondation FondaMental, v Behring Röntgen Stiftung, The Wolfson Foundation, and Sage Therapeutics; in addition, he has received speaker fees from Lundbeck International Foundation, Paul-Martini-Stiftung, Lilly Deutschland, Atheneum, Fama Public Relations, Institut d’investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Janssen-Cilag, Hertie Stiftung, Bodelschwingh-Klinik, Pfizer, Atheneum, University of Freiburg, Schizophrenia Academy, Hong Kong Society of Biological Psychiatry, Fama Public Relations, Spanish Society of Psychiatry, Italian Society of Biological Psychiatry, Reunions I Ciencia S.L., and Brain Center Rudolf Magnus UMC Utrecht and was awarded the Prix Roger de Spoelberch grant and the CINP Lilly Neuroscience Clinical Research Award 2016. BEW’s spouse is an employee of Siemens Healthineers. IM, LR, DK, BP, IP, ML, AR, EW, DH, BM, and SS report no conflicts of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Isabel Maurus, Lukas Roell.
Supplementary information
The online version contains supplementary material available at 10.1038/s41398-022-02155-x.
References
- 1.Schultz C, Engelhardt M. Anatomy of the hippocampal formation. Front Neurol Neurosci. 2014;34:6–17. doi: 10.1159/000360925. [DOI] [PubMed] [Google Scholar]
- 2.Ota M, Sato N, Hidese S, Teraishi T, Maikusa N, Matsuda H, et al. Structural differences in hippocampal subfields among schizophrenia patients, major depressive disorder patients, and healthy subjects. Psychiatry Res Neuroimaging. 2017;259:54–59. doi: 10.1016/j.pscychresns.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Haukvik UK, Tamnes CK, Söderman E, Agartz I. Neuroimaging hippocampal subfields in schizophrenia and bipolar disorder: A systematic review and meta-analysis. J Psychiatry Res. 2018;104:217–26. doi: 10.1016/j.jpsychires.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 4.Kawano M, Sawada K, Shimodera S, Ogawa Y, Kariya S, Lang DJ, et al. Hippocampal subfield volumes in first episode and chronic schizophrenia. PloS one. 2015;10:e0117785. doi: 10.1371/journal.pone.0117785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lisman J, Buzsáki G, Eichenbaum H, Nadel L, Ranganath C, Redish AD. Viewpoints: how the hippocampus contributes to memory, navigation and cognition. Nat Neurosci. 2017;20:1434–47. doi: 10.1038/nn.4661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zeineh MM, Engel SA, Thompson PM, Bookheimer SY. Dynamics of the hippocampus during encoding and retrieval of face-name pairs. science. 2003;299:577–80. doi: 10.1126/science.1077775. [DOI] [PubMed] [Google Scholar]
- 7.Eldridge LL, Engel SA, Zeineh MM, Bookheimer SY, Knowlton BJ. A dissociation of encoding and retrieval processes in the human hippocampus. J Neurosci. 2005;25:3280–6. doi: 10.1523/JNEUROSCI.3420-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raz N, Lindenberger U, Rodrigue KM, Kennedy KM, Head D, Williamson A, et al. Regional brain changes in aging healthy adults: general trends, individual differences and modifiers. Cereb Cortex. 2005;15:1676–89. doi: 10.1093/cercor/bhi044. [DOI] [PubMed] [Google Scholar]
- 9.van Erp TG, Hibar DP, Rasmussen JM, Glahn DC, Pearlson GD, Andreassen OA, et al. Subcortical brain volume abnormalities in 2028 individuals with schizophrenia and 2540 healthy controls via the ENIGMA consortium. Mol Psychiatry. 2016;21:547–53. doi: 10.1038/mp.2015.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falkai P, Malchow B, Wetzestein K, Nowastowski V, Bernstein H-G, Steiner J, et al. Decreased oligodendrocyte and neuron number in anterior hippocampal areas and the entire hippocampus in schizophrenia: a stereological postmortem study. Schizophrenia Bull. 2016;42:S4–S12. doi: 10.1093/schbul/sbv157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park MTM, Jeon P, Khan AR, Dempster K, Chakravarty MM, Lerch JP, et al. Hippocampal neuroanatomy in first episode psychosis: A putative role for glutamate and serotonin receptors. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021;110:110297. doi: 10.1016/j.pnpbp.2021.110297. [DOI] [PubMed] [Google Scholar]
- 12.Ho NF, Iglesias JE, Sum MY, Kuswanto CN, Sitoh YY, De Souza J, et al. Progression from selective to general involvement of hippocampal subfields in schizophrenia. Mol Psychiatry. 2017;22:142–52. doi: 10.1038/mp.2016.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakahara S, Matsumoto M, van Erp TGM. Hippocampal subregion abnormalities in schizophrenia: A systematic review of structural and physiological imaging studies. Neuropsychopharmacol Rep. 2018;38:156–66. doi: 10.1002/npr2.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakahara S, Turner JA, Calhoun VD, Lim KO, Mueller B, Bustillo JR, et al. Dentate gyrus volume deficit in schizophrenia. Psychological Med. 2020;50:1267–77. doi: 10.1017/S0033291719001144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boyer P, Phillips JL, Rousseau FL, Ilivitsky S. Hippocampal abnormalities and memory deficits: new evidence of a strong pathophysiological link in schizophrenia. Brain Res Rev. 2007;54:92–112. doi: 10.1016/j.brainresrev.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 16.Talamini LM, Meeter M, Elvevåg B, Murre JM, Goldberg TE. Reduced parahippocampal connectivity produces schizophrenia-like memory deficits in simulated neural circuits with reduced parahippocampal connectivity. Arch Gen Psychiatry. 2005;62:485–93. doi: 10.1001/archpsyc.62.5.485. [DOI] [PubMed] [Google Scholar]
- 17.Guo JY, Ragland JD, Carter CS. Memory and cognition in schizophrenia. Mol Psychiatry. 2019;24:633–42. doi: 10.1038/s41380-018-0231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Antoniades M, Schoeler T, Radua J, Valli I, Allen P, Kempton MJ, et al. Verbal learning and hippocampal dysfunction in schizophrenia: A meta-analysis. Neurosci Biobehav Rev. 2018;86:166–75. doi: 10.1016/j.neubiorev.2017.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Francis AN, Seidman LJ, Tandon N, Shenton ME, Thermenos HW, Mesholam-Gately RI, et al. Reduced subicular subdivisions of the hippocampal formation and verbal declarative memory impairments in young relatives at risk for schizophrenia. Schizophrenia Res. 2013;151:154–7. doi: 10.1016/j.schres.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 20.Mathew I, Gardin TM, Tandon N, Eack S, Francis AN, Seidman LJ, et al. Medial temporal lobe structures and hippocampal subfields in psychotic disorders: findings from the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP) study. JAMA Psychiatry. 2014;71:769–77. doi: 10.1001/jamapsychiatry.2014.453. [DOI] [PubMed] [Google Scholar]
- 21.Yasuda K, Yamada S, Uenishi S, Ikeda N, Tamaki A, Ohoshi Y, et al. Hippocampal subfield volumes and cognitive function in schizophrenia and mood disorders. Neuropsychobiology. 2022;3:1–11. doi: 10.1159/000521102. [DOI] [PubMed] [Google Scholar]
- 22.Aghjayan SL, Lesnovskaya A, Esteban-Cornejo I, Peven JC, Stillman CM, Erickson KI. Aerobic exercise, cardiorespiratory fitness, and the human hippocampus. Hippocampus. 2021;31:817–44. doi: 10.1002/hipo.23337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Firth J, Stubbs B, Vancampfort D, Schuch F, Lagopoulos J, Rosenbaum S, et al. Effect of aerobic exercise on hippocampal volume in humans: a systematic review and meta-analysis. NeuroImage. 2018;166:230–8. doi: 10.1016/j.neuroimage.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 24.Wilckens KA, Stillman CM, Waiwood AM, Kang C, Leckie RL, Peven JC, et al. Exercise interventions preserve hippocampal volume: A meta-analysis. Hippocampus. 2021;31:335–47. doi: 10.1002/hipo.23292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wittfeld K, Jochem C, Dörr M, Schminke U, Gläser S, Bahls M, et al. Cardiorespiratory fitness and gray matter volume in the temporal, frontal, and cerebellar regions in the general population. Mayo Clin Proc. 2020;95:44–56. doi: 10.1016/j.mayocp.2019.05.030. [DOI] [PubMed] [Google Scholar]
- 26.Voss MW, Weng TB, Burzynska AZ, Wong CN, Cooke GE, Clark R, et al. Fitness, but not physical activity, is related to functional integrity of brain networks associated with aging. NeuroImage. 2016;131:113–25. doi: 10.1016/j.neuroimage.2015.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ikuta T, Loprinzi PD. Association of cardiorespiratory fitness on interhemispheric hippocampal and parahippocampal functional connectivity. Eur J Neurosci. 2019;50:1871–7. doi: 10.1111/ejn.14366. [DOI] [PubMed] [Google Scholar]
- 28.Stillman CM, Uyar F, Huang H, Grove GA, Watt JC, Wollam ME, et al. Cardiorespiratory fitness is associated with enhanced hippocampal functional connectivity in healthy young adults. Hippocampus. 2018;28:239–47. doi: 10.1002/hipo.22827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci USA. 2011;108:3017–22. doi: 10.1073/pnas.1015950108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pereira AC, Huddleston DE, Brickman AM, Sosunov AA, Hen R, McKhann GM, et al. An in vivo correlate of exercise-induced neurogenesis in the adult dentate gyrus. Proc Natl Acad Sci USA. 2007;104:5638–43. doi: 10.1073/pnas.0611721104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van der Stouwe E, Van Busschbach J, De Vries B, Cahn W, Aleman A, Pijnenborg G. Neural correlates of exercise training in individuals with schizophrenia and in healthy individuals: A systematic review. NeuroImage: Clin. 2018;19:287–301. doi: 10.1016/j.nicl.2018.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Malchow B, Keller K, Hasan A, Dorfler S, Schneider-Axmann T, Hillmer-Vogel U, et al. Effects of Endurance Training Combined With Cognitive Remediation on Everyday Functioning, Symptoms, and Cognition in Multiepisode Schizophrenia Patients. Schizophr Bull. 2015;41:847–58. doi: 10.1093/schbul/sbv020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Malchow B, Keeser D, Keller K, Hasan A, Rauchmann BS, Kimura H, et al. Effects of endurance training on brain structures in chronic schizophrenia patients and healthy controls. Schizophrenia Res. 2016;173:182–91. doi: 10.1016/j.schres.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 34.Maurus I, Hasan A, Schmitt A, Roeh A, Keeser D, Malchow B, et al. Aerobic endurance training to improve cognition and enhance recovery in schizophrenia: design and methodology of a multicenter randomized controlled trial. Europ Archives Psychiatry Clin Neurosci. 2020;2:315–324. doi: 10.1007/s00406-020-01175-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Faude O, Kindermann W, Meyer T. Lactate threshold concepts: how valid are they? Sports Med (Auckl, NZ) 2009;39:469–90. doi: 10.2165/00007256-200939060-00003. [DOI] [PubMed] [Google Scholar]
- 36.Li X, Morgan PS, Ashburner J, Smith J, Rorden C. The first step for neuroimaging data analysis: DICOM to NIfTI conversion. J Neurosci Methods. 2016;264:47–56. doi: 10.1016/j.jneumeth.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 37.Gorgolewski KJ, Auer T, Calhoun VD, Craddock RC, Das S, Duff EP, et al. The brain imaging data structure, a format for organizing and describing outputs of neuroimaging experiments. Sci Data. 2016;3:1–9. doi: 10.1038/sdata.2016.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reuter M, Rosas HD, Fischl B. Highly accurate inverse consistent registration: a robust approach. Neuroimage. 2010;53:1181–96. doi: 10.1016/j.neuroimage.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ségonne F, Dale AM, Busa E, Glessner M, Salat D, Hahn HK, et al. A hybrid approach to the skull stripping problem in MRI. Neuroimage. 2004;22:1060–75. doi: 10.1016/j.neuroimage.2004.03.032. [DOI] [PubMed] [Google Scholar]
- 40.Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33:341–55. doi: 10.1016/S0896-6273(02)00569-X. [DOI] [PubMed] [Google Scholar]
- 41.Fischl B, Salat DH, van der Kouwe AJ, Makris N, Ségonne F, Quinn BT, et al. Sequence-independent segmentation of magnetic resonance images. Neuroimage. 2004;23:S69–84. doi: 10.1016/j.neuroimage.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 42.Sled JG, Zijdenbos AP, Evans AC. A nonparametric method for automatic correction of intensity nonuniformity in MRI data. IEEE Trans Med Imaging. 1998;17:87–97. doi: 10.1109/42.668698. [DOI] [PubMed] [Google Scholar]
- 43.Fischl B, Liu A, Dale AM. Automated manifold surgery: constructing geometrically accurate and topologically correct models of the human cerebral cortex. IEEE Trans Med Imaging. 2001;20:70–80. doi: 10.1109/42.906426. [DOI] [PubMed] [Google Scholar]
- 44.Ségonne F, Pacheco J, Fischl B. Geometrically accurate topology-correction of cortical surfaces using nonseparating loops. IEEE Trans Med Imaging. 2007;26:518–29. doi: 10.1109/TMI.2006.887364. [DOI] [PubMed] [Google Scholar]
- 45.Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage. 1999;9:179–94. doi: 10.1006/nimg.1998.0395. [DOI] [PubMed] [Google Scholar]
- 46.Dale AM, Sereno MI. Improved localizadon of cortical activity by combining EEG and MEG with MRI cortical surface reconstruction: a linear approach. J Cogn Neurosci. 1993;5:162–76. doi: 10.1162/jocn.1993.5.2.162. [DOI] [PubMed] [Google Scholar]
- 47.Fischl B, Dale AM. Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci USA. 2000;97:11050–5. doi: 10.1073/pnas.200033797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Esteban O, Markiewicz CJ, Blair RW, Moodie CA, Isik AI, Erramuzpe A, et al. fMRIPrep: a robust preprocessing pipeline for functional MRI. Nat Methods. 2019;16:111–6. doi: 10.1038/s41592-018-0235-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pruim RHR, Mennes M, van Rooij D, Llera A, Buitelaar JK, Beckmann CF. ICA-AROMA: A robust ICA-based strategy for removing motion artifacts from fMRI data. NeuroImage. 2015;112:267–77. doi: 10.1016/j.neuroimage.2015.02.064. [DOI] [PubMed] [Google Scholar]
- 50.Parkes L, Fulcher B, Yücel M, Fornito A. An evaluation of the efficacy, reliability, and sensitivity of motion correction strategies for resting-state functional MRI. NeuroImage. 2018;171:415–36. doi: 10.1016/j.neuroimage.2017.12.073. [DOI] [PubMed] [Google Scholar]
- 51.Esteban O, Birman D, Schaer M, Koyejo OO, Poldrack RA, Gorgolewski KJ. MRIQC: Advancing the automatic prediction of image quality in MRI from unseen sites. PLoS One. 2017;12:e0184661. doi: 10.1371/journal.pone.0184661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Raamana P, Theyers A, Selliah T, Bhati P, Arnott S, Hassel S, et al. Visual QC Protocol for FreeSurfer cortical parcellations from anatomical MRI. preprint at: https://www.biorxiv.org/content/10.1101/2020.09.07.286807v5.full 2020.
- 53.Iglesias JE, Augustinack JC, Nguyen K, Player CM, Player A, Wright M, et al. A computational atlas of the hippocampal formation using ex vivo, ultra-high resolution MRI: Application to adaptive segmentation of in vivo MRI. NeuroImage. 2015;115:117–37. doi: 10.1016/j.neuroimage.2015.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.O’Brien LM, Ziegler DA, Deutsch CK, Frazier JA, Herbert MR, Locascio JJ. Statistical adjustments for brain size in volumetric neuroimaging studies: some practical implications in methods. Psychiatry Res. 2011;193:113–22. doi: 10.1016/j.pscychresns.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fan L, Li H, Zhuo J, Zhang Y, Wang J, Chen L, et al. The Human Brainnetome Atlas: A New Brain Atlas Based on Connectional Architecture. Cereb Cortex. 2016;26:3508–26. doi: 10.1093/cercor/bhw157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Helmstaedter C, Wietzke J, Lutz MT. Unique and shared validity of the “Wechsler logical memory test”, the “California verbal learning test”, and the “verbal learning and memory test” in patients with epilepsy. Epilepsy Res. 2009;87:203–12. doi: 10.1016/j.eplepsyres.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 57.Pajonk FG, Wobrock T, Gruber O, Scherk H, Berner D, Kaizl I, et al. Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry. 2010;67:133–43. doi: 10.1001/archgenpsychiatry.2009.193. [DOI] [PubMed] [Google Scholar]
- 58.RStudio Team. RStudio: Integrated development environment for R. RStudio, PBC: Boston, MA, 2020.
- 59.R Core Team. R: A language and environment for statistical computing. In: Computing RFfS (ed). R Foundation for Statistical Computing: Vienna, Austria, 2021.
- 60.Leucht S, Samara M, Heres S, Davis JM. Dose equivalents for antipsychotic drugs: The DDD method. Schizophr Bull. 2016;42:90–94. doi: 10.1093/schbul/sbv167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McArtor DB MVLM: Multivariate Linear Model with Analytic p-Values. R package version 0.1.42017.
- 62.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. mediation: R Package for Causal Mediation Analysis. 2014. 2014;59:38. [Google Scholar]
- 63.Wickham H. ggplot2: Elegant Graphics for Data Analysis. New York: Springer; 2016. [Google Scholar]
- 64.Li MY, Huang MM, Li SZ, Tao J, Zheng GH, Chen LD. The effects of aerobic exercise on the structure and function of DMN-related brain regions: a systematic review. Int J Neurosci. 2017;127:634–49. doi: 10.1080/00207454.2016.1212855. [DOI] [PubMed] [Google Scholar]
- 65.Hvid LG, Harwood DL, Eskildsen SF, Dalgas U. A critical systematic review of current evidence on the effects of physical exercise on whole/regional grey matter brain volume in populations at risk of neurodegeneration. Sports Med. 2021;51:1651–71. doi: 10.1007/s40279-021-01453-6. [DOI] [PubMed] [Google Scholar]
- 66.Falkai P, Maurus I, Schmitt A, Malchow B, Schneider-Axmann T, Röll L, et al. Improvement in daily functioning after aerobic exercise training in schizophrenia is sustained after exercise cessation. Eur Arch Psychiatry Clin Neurosci. 2021;271:1201–3. doi: 10.1007/s00406-021-01282-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Consortium SWGotPG. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7. doi: 10.1038/nature13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Papiol S, Popovic D, Keeser D, Hasan A, Schneider-Axmann T, Degenhardt F, et al. Polygenic risk has an impact on the structural plasticity of hippocampal subfields during aerobic exercise combined with cognitive remediation in multi-episode schizophrenia. Transl Psychiatry. 2017;7:e1159. doi: 10.1038/tp.2017.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Papiol S, Keeser D, Hasan A, Schneider-Axmann T, Raabe F, Degenhardt F, et al. Polygenic burden associated to oligodendrocyte precursor cells and radial glia influences the hippocampal volume changes induced by aerobic exercise in schizophrenia patients. Transl Psychiatry. 2019;9:1–8. doi: 10.1038/s41398-019-0618-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kern KL, Storer TW, Schon K. Cardiorespiratory fitness, hippocampal subfield volumes, and mnemonic discrimination task performance in aging. Hum Brain Mapp. 2021;42:871–92. doi: 10.1002/hbm.25259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nauer RK, Dunne MF, Stern CE, Storer TW, Schon K. Improving fitness increases dentate gyrus/CA3 volume in the hippocampal head and enhances memory in young adults. Hippocampus. 2020;30:488–504. doi: 10.1002/hipo.23166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Prathap S, Nagel BJ, Herting MM. Understanding the role of aerobic fitness, spatial learning, and hippocampal subfields in adolescent males. Sci Rep. 2021;11:9311. doi: 10.1038/s41598-021-88452-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hamada M, Rothwell JC Neurophysiology of rTMS: important caveats when interpreting the results of therapeutic interventions. Therapeutic rTMS in Neurology. Springer 2016, pp1–10.
- 74.Schwartz B, Teslovich T, You X, Cho J, Schooler N, Kokkinos P, et al. An exploratory study of exercise-related effects on memory and hippocampal connectivity in schizophrenia. Clin Schizophr Relat Psychoses. 10.3371/CSRP.SCWO.061518 2018. [DOI] [PMC free article] [PubMed]
- 75.Dean DJ, Bryan AD, Newberry R, Gupta T, Carol E, Mittal VA. A supervised exercise intervention for youth at risk for psychosis: an open-label pilot study. J Clin Psychiatry. 2017;78:e1167–e1173. doi: 10.4088/JCP.16m11365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Huang X, Zhao X, Cai Y, Wan Q. The cerebral changes induced by exercise interventions in people with mild cognitive impairment and Alzheimer’s disease: A systematic review. Arch Gerontol Geriatr. 2022;98:104547. doi: 10.1016/j.archger.2021.104547. [DOI] [PubMed] [Google Scholar]
- 77.Weinberger DR, Radulescu E. Finding the elusive psychiatric “lesion” with 21st-century neuroanatomy: a note of caution. Am J psychiatry. 2016;173:27–33. doi: 10.1176/appi.ajp.2015.15060753. [DOI] [PubMed] [Google Scholar]
- 78.Pletzer B, Harris T-A, Scheuringer A, Hidalgo-Lopez E. The cycling brain: menstrual cycle related fluctuations in hippocampal and fronto-striatal activation and connectivity during cognitive tasks. Neuropsychopharmacol. 2019;44:1867–75. doi: 10.1038/s41386-019-0435-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rohrer JM. Thinking clearly about correlations and causation: Graphical causal models for observational data. Adv Methods Pract Psychological Sci. 2018;1:27–42. doi: 10.1177/2515245917745629. [DOI] [Google Scholar]
- 80.Erickson KI, Banducci SE, Weinstein AM, MacDonald AW, III, Ferrell RE, Halder I, et al. The brain-derived neurotrophic factor Val66Met polymorphism moderates an effect of physical activity on working memory performance. Psychological Sci. 2013;24:1770–9. doi: 10.1177/0956797613480367. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Imaging data, results from the quality control, the scripts for the whole analysis as well as demographic, physical, clinical and cognitive data files are published on OSF (Identifier: 10.17605/OSF.IO/TR3NX). Additional data will be made available upon request.