Abstract
Purpose:
Quadriceps weakness is common after anterior cruciate ligament (ACL) reconstruction, resulting in prolonged disability and increased risk for re-injury and osteoarthritis. Functional resistance training (FRT) combines resistance training with task-specific training and may prove beneficial in restoring quadriceps strength. The primary purpose of this study was to determine if a walking specific FRT program (e.g., resisted walking) improves knee strength in individuals after ACL reconstruction.
Methods:
Thirty participants were randomized into one of three groups: 1) FRT with a customized knee BRACE applied to the ACL leg, 2) FRT with elastic BAND tethered to the ankle of the ACL leg, or 3) a TARGET MATCH condition where no resistance was externally applied. Participants in all groups received training while walking on a treadmill 2–3 times per week for 8 weeks. Isometric knee extension and flexion strength were measured prior to the start of the intervention (PRE), after the intervention (POST), and 8 weeks after intervention completion (POST-2).
Results:
The BRACE group had greater knee extensor strength compared with the TARGET MATCH group at POST and POST-2 (p<0.05). The BRACE group had greater knee flexor strength than the TARGET MATCH group at POST and POST-2 (p<0.05) and the BAND group at POST (p<0.05).
Conclusions:
FRT applied via a customized knee brace results in improvements in knee extensor and flexor strength after ACL reconstruction. FRT is a beneficial adjuvant to ACL rehabilitation and leads to better strength compared to standard of care.
Keywords: RESISTANCE TRAINING, TASK-SPECIFIC TRAINING, KNEE INJURY, MUSCLE STRENGTH
INTRODUCTION
Profound quadriceps weakness usually develops rapidly after anterior cruciate ligament (ACL) injury and reconstruction. Despite progress made in operative technique and post-operative rehabilitation over the last few decades, many patients have significant quadriceps weakness when they return to activity and beyond (1–5). This chronic quadriceps weakness contributes to knee instability, disability, and increased re-injury rate (6–8). Furthermore, quadriceps weakness early after ACL reconstruction is related to joint space width narrowing four years after ACL reconstruction suggesting that muscle weakness may play a role in the development of post-traumatic osteoarthritis(9), which afflicts ~50% of patients within 15 years of injury (10). Thus, interventions addressing quadriceps weakness are critically needed.
High-intensity resistance training is a powerful stimulus for improving muscle strength, quality, and function (11–14). While ACL rehabilitation programs typically include high-intensity resistance training, complete quadriceps strength recovery after ACL reconstruction has been mostly unattainable. A potential cause for the lack of efficacy of current resistance-based exercise used in ACL rehabilitation is that these exercises are typically performed in a “nonfunctional” manner (i.e., while lying, sitting, or standing in place), which is less than optimal for inducing transfer of benefits to functional activities, such as walking, because of practice specificity (15, 16). Furthermore, incorporation of high-intensity resistance exercises into ACL rehabilitation early after ACL reconstruction is often not done out of concern for potential graft failure, knee laxity, or patellar fracture, despite evidence that it is safe to use (17, 18). Thus, low-load progressive resistance training, when performed using a task-specific approach (i.e., functional resistance training [FRT]), introduced early after surgery could be an alternative method to help combat the problematic quadriceps muscle weakness affecting the ACL reconstructed population.
To perform FRT, particularly during walking, clinicians typically apply weight cuffs to the lower extremity. The advantage of cuffs are that they are a simple low-cost device and research indicates that walking with a weight cuff can increase power of the hip and knee, and muscle activation in neurologically-injured populations (19). The disadvantage is that cuffs are hindered by a low torque-to-weight ratio, which makes achieving substantial resistances unobtainable without excessively large weights (20, 21). To circumvent the known issues with the clinical weight cuff application of FRT that limit strength gains, we have developed two devices: 1) a robotic brace that provides bi-directional resistance to the knee and 2) a pulley system where elastic bands are attached to the ankle and provide resistance during knee extension while in the swing phase of gait. Notably, we have previously shown that FRT with these devices increases thigh muscle activity in computer simulations (22) and in healthy adults (20). The trial conducted here is a natural extension of that work, testing the efficacy of this device in a clinical population with thigh muscle weakness. Thus, the purpose of this randomized clinical trial was to determine the effects of FRT during walking on thigh muscle strength in individuals after ACL reconstruction. A secondary purpose was to determine if one mode of FRT (brace vs elastic band) was more effective at improving muscle strength. We hypothesized that ACL reconstructed individuals who received FRT applied via the brace and/or the elastic bands would have greater knee extensor strength than individuals who did not receive FRT. Further, because the brace provides bi-directional resistance, we hypothesized that individuals who received the brace FRT would also have greater improvements in knee flexor strength than those who received FRT via elastic bands or no FRT.
METHODS
Study Design
This study was a single-center, parallel group, randomized controlled clinical trial (NCT03282565) in which patients who underwent ACL reconstruction were block randomized to one of three groups: 1) FRT with a customized brace (BRACE); 2) FRT with elastic bands (BAND); or 3) a control/target match condition (TARGET MATCH). Neither participants nor outcome assessors were blinded to group assignment. Our outcome measures, isometric knee extension and flexion strength, were assessed at three time points: 1) pre-intervention (~6 weeks after ACL reconstruction) (PRE), 2) post-intervention (within 1 week of completing the 8-week intervention) (POST), and 3) post-intervention 2 (~8 weeks after completing the intervention) (POST-2). All testing/training took place at the University of Michigan within the Orthopaedic Rehabilitation and Biomechanics Laboratory or Neuromuscular and Rehabilitation Robotics Laboratory. The randomization sequence was generated using a web application (www.sealedenvelope.com) by one of the principal investigators (C.K.) and assignment was placed in a password protected excel file located in a secured computer drive that was given to the study team member providing the treatments after enrollment (SRB).
Eligibility Criteria
Participants were eligible for inclusion into the trial if they were between 14 and 40 years of age, suffered an acute ACL rupture, had elected to undergo ACL reconstruction using an autograft, were 6–10 weeks out from their ACL reconstruction, and were willing to participate in the intervention and follow-up testing as outlined in the protocol. Participants were excluded if they had: 1) suffered a prior ACL injury, 2) undergone a prior knee surgery, 3) a bony fracture accompanying their ACL injury, 4) sustained a knee dislocation resulting in their ACL tear, 5) a recent significant injury other than the ACL tear, and/or 6) history of uncontrolled diabetes or hypertension. Potential participants were also asked if they were pregnant or planned to become pregnant in the upcoming months and those responding yes were excluded. All participants reviewed and signed a consent/assent form approved by the University of Michigan Medical Institutional Review Board. Parental consent was obtained if the participant was a minor child.
Study Participants
One hundred sixty-six patients with an ACL tear from our clinic met inclusion criteria and were contacted about participating in the study (Figure 1). Thirty patients were ultimately consented and were enrolled between May 2018 and February 2020. Four of these thirty individual were unable to complete the study per protocol due to research shutdowns resulting from the COVID-19 pandemic. As such, a total of 26 individuals completed study interventions and testing as expected and their results are reported herein. Demographic information for these 26 individuals is provided in Table 1. A power analysis was performed in G*Power 3.1 prior to the start of the study.(23, 24) It was determined that the sample size (N=30) provided >85% power to detect significant differences between groups with a conservative effect size ‘f’ of 0.33 (partial η2=0.1), correlation between repeated measures of 0.5, and type I error of 5%.
FIGURE 1.
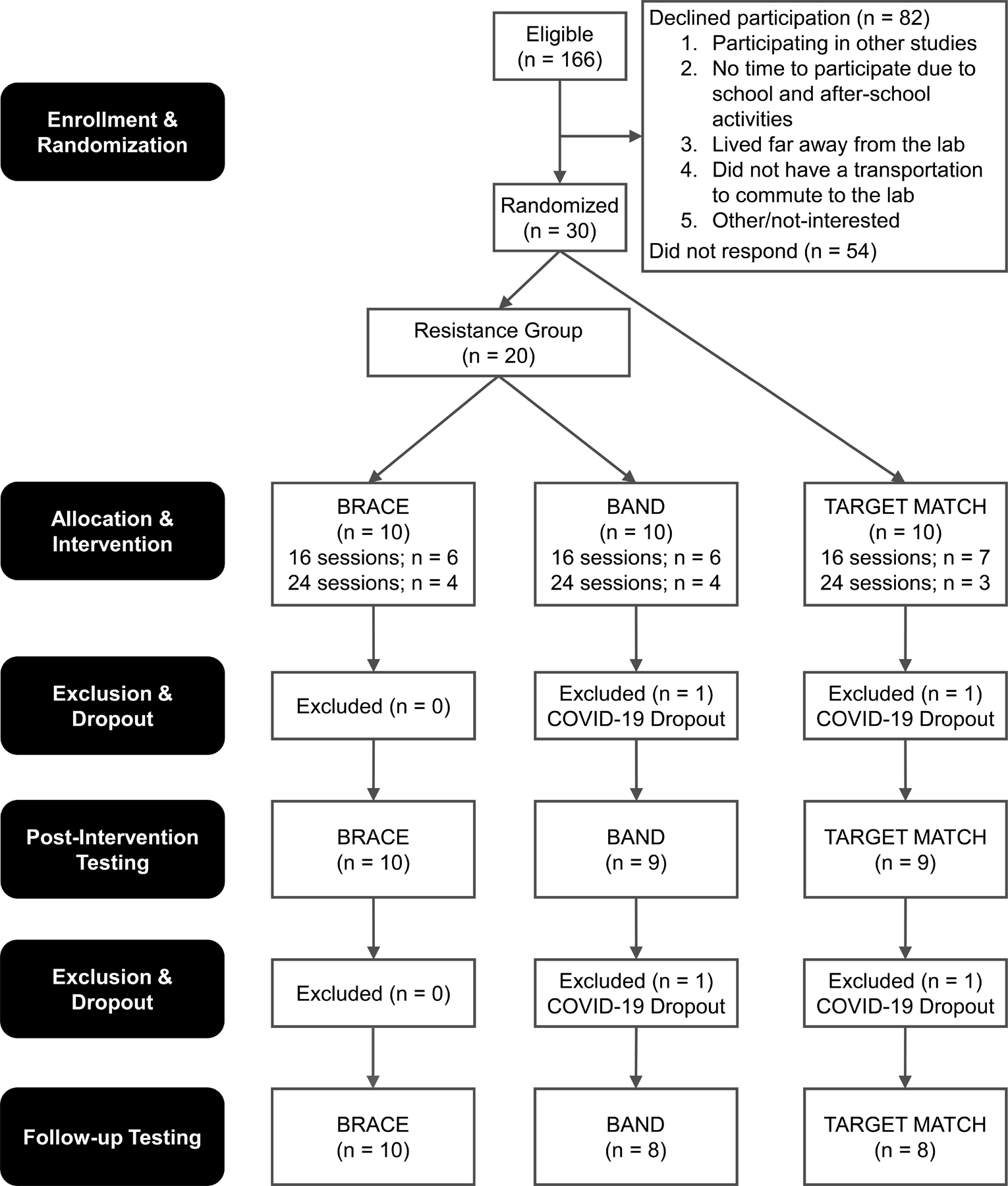
CONSORT (Consolidated Standards of Reporting Trials) diagram illustrating the flow of participants through the study. FRT = Functional Resistance Training
TABLE 1.
Demographic information for participants in BRACE, BAND, and TARGET MATCH groups represented as mean ± standard deviation unless otherwise noted.
| BRACE | BAND | TARGET MATCH | |
|---|---|---|---|
| N at PRE | 10 | 10 | 10 |
| Sex | 6 F, 4 M | 6 F, 4 M | 6 F, 4 M |
| Age (yrs) | 19.6 ± 6.4 | 22.1 ± 4.5 | 20.2 ± 5.3 |
| Height (cm) | 174.0 ± 10.6 | 172.3 ± 7.9 | 169.8 ± 9.0 |
| Mass (kg) | 72.4 ± 12.53 | 70.3 ± 12.2 | 70.2 ± 13.3 |
| Graft | 8 BPTB, 1 HAM, 1 QUAD | 8 BPTB, 2 HAM | 9 BPTB, 1 HAM |
| Time Since Surgery to PRE (wks) | 8.9 ± 2.6 | 9.5 ± 2.5 | 10.3 ± 3.1 |
| Pre-Surgery Tegner median (IQR) | 9 (7–9) | 7 (7–8.5) | 7 (7–8.75) |
| N at POST | 10 | 9 | 9 |
| Sex | 6 F, 4 M | 6 F, 3 M | 5 F, 4 M |
| Graft | 8 BPTB, 1 HAM, 1 QUAD | 7 BPTB, 2 HAM | 8 BPTB, 1 HAM |
| Time Since Surgery to POST (wks) | 18.3 ± 2.6 | 20.1 ± 3.3 | 19.7 ± 4.2 |
| N at POST-2 | 10 | 8 | 8 |
| Sex | 6 F, 4 M | 6 F, 2 M | 4 F, 4 M |
| Graft | 8 BPTB, 1 HAM, 1 QUAD | 6 BPTB, 2 HAM | 7 BPTB, 1 HAM |
| Time Since Surgery to POST-2 (wks) | 27.6 ± 2.6 | 29.2 ± 3.7 | 27.8 ± 3.7 |
BPTB = Bone patellar tendon bone graft, HAM = Hamstring graft, QUAD = Quadriceps tendon graft. No significant differences were noted between groups for age, height, mass, or pre-surgery Tegner activity score (p>0.05).
No adverse events were reported by any of the participants. All individuals were undergoing standard of care rehabilitation after their ACL reconstruction during the clinical trial, and this occurred separate from study interventions and was not modified for study purposes. The standard of care ACL rehabilitation exercises were not standardized for study participants and participants could opt to receive care at their location of choice. All but four participants received physical therapy through one health system.
Knee Strength Testing
Maximal voluntary isometric knee extension and flexion torque of both legs were measured with the knee positioned at 60° of knee flexion in a dynamometer (Biodex System 3, Shirley, NY). The strength of non-reconstructed leg was measured first followed by the ACL reconstructed leg (25, 26). An anti-shear device was included on the dynamometer arm. After performing warm-up trials, three maximal trials were performed for each muscle group in an alternating fashion (i.e., extension followed by flexion). Peak torque values were normalized to body mass and the average of the three trials was utilized for data analysis.
Study Interventions/Training
A schema detailing the testing and training sessions can be found in Figure 2. Participants in all study groups reported for training 2–3 x/week, based on their availability, for eight weeks beginning approximately six weeks post-operatively. Six weeks after ACL reconstruction was chosen for initiation of training as it corresponded to when participants (i) had gained adequate neuromuscular control to walk safely with resistance, (ii) were no longer using assistive devices, and (iii) did not have a noticeable antalgic gait. All subjects were compliant with the training and reported either two (N=17; BRACE = 6; BAND = 5; TARGET MATCH = 6) or three times per week (N = 11; BRACE = 4; BAND =4; TARGET MATCH = 3).
FIGURE 2.
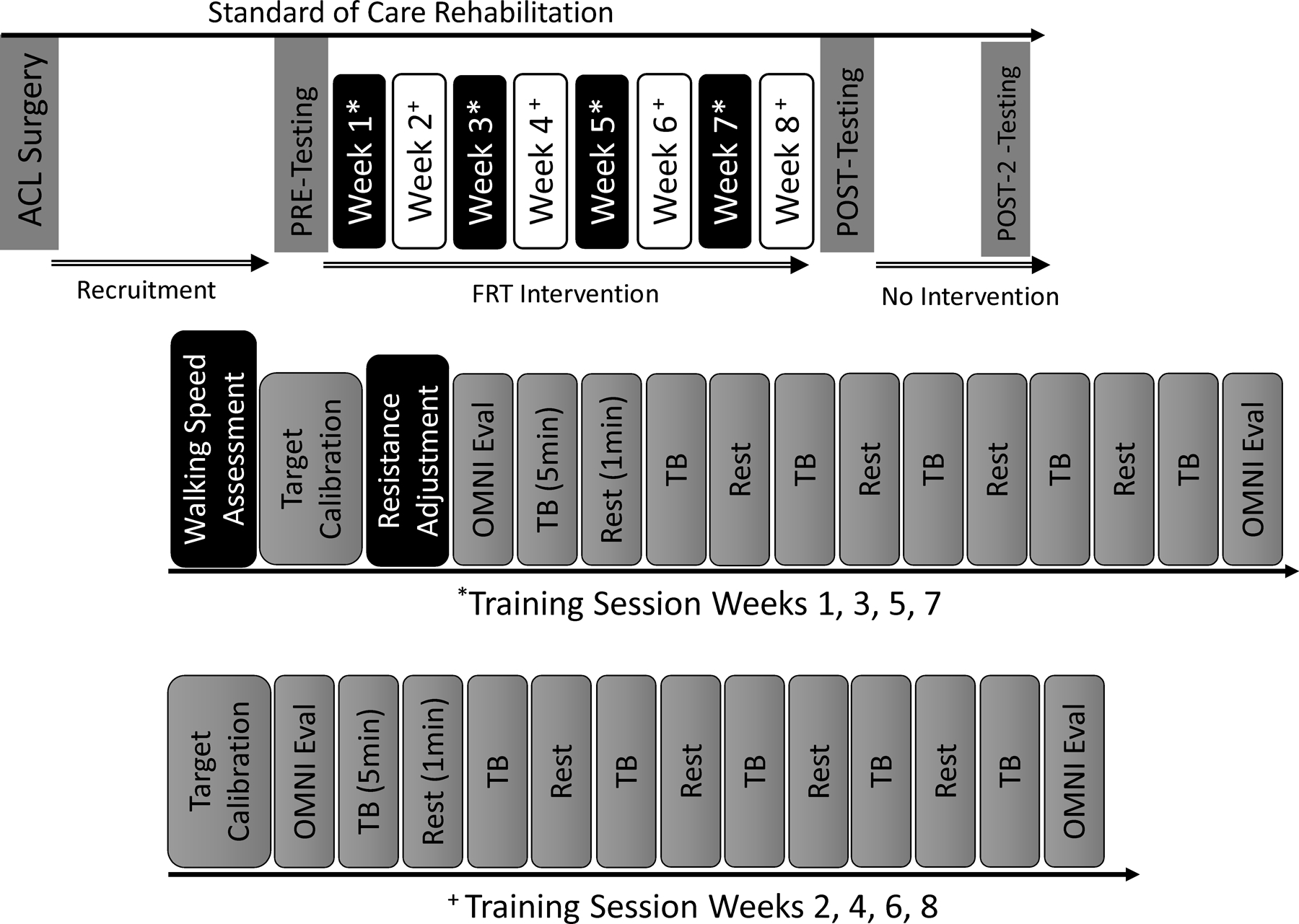
Schematic illustrating the testing and training visits associated with the study. *indicates the timeline of the training session for weeks 1, 3, 5, and 7. + indicates the timeline of the training session weeks 2, 4, 6, 8. TB = training block; Eval = Evaluation
During all training conditions, participants were provided with real-time visual kinematic feedback while they walked on an instrumented treadmill (Bertec; Columbus, OH). To provide this feedback, participants needed to complete a target calibration walking trial during each training session in order to create a target kinematic template which was used during training (27–29). During this trial, participants were asked to walk for 60-seconds at 80% of their preferred overground walking speed (average overground walking speed was assessed during a 10m walk) while equipped with three reflective markers on the lateral side of the ACL reconstructed limb’s hip, knee, and ankle joints. A camera (C920 Webcam, Logitech) was used to track these markers in real-time in order to calculate and obtain ensemble averages of sagittal plane hip and knee joint angles (30). The ensemble averaged trajectories were up-scaled by 30% during the swing phase of gait and displayed as endpoint trajectories (i.e., foot trajectory) alongside the actual, real-time trajectories in front of the participants on a large monitor during the training sessions. The up-scaled trajectories acted as a target for participants to achieve while they walked and was used to ensure that participants were encouraged to increase range of motion during training. The 80% walking speed was used in order to promote a more symmetrical gait pattern and allow for greater loading of the leg muscles.(31) At each training session, participants were reminded to match the target as closely as possible and were cued to do so when necessary. The walking speed was adjusted every other week to account for improvements over the course of the study but were capped at 1.2 m/s.
FRT with a Customized Brace
Participants randomized into the BRACE group received progressive FRT while walking on a treadmill using a brace (T Scope Premier Post-Op Knee Brace [Part No 08814], Breg, Grand Prairie, TX) that was custom-fitted with an eddy current brake to provide resistance while walking. Details regarding the brace design can be found elsewhere (20). Briefly, eddy currents are localized circular electric currents within a conductor that can slow or stop a moving object by dissipating kinetic energy, thus providing a non-contact dissipative force that is proportional to and opposite of the velocity of the movement. For this experiment, the eddy current brake allowed the brace to provide scalable resistive torques at the knee during walking.
Participants started each training session by performing a target calibration trial for 1-minute while wearing the brace which applied zero resistance and walking on the treadmill at 80% of their preferred overground walking speed. Following this, each participant performed six blocks of treadmill training at the pre-determined speed at an intensity corresponding to a difficulty level between 5–7 on the OMNI scale (32) (somewhat hard), with each training block lasting for five minutes (30 minutes total). The resistance provided by the brace during training was bi-directional (i.e., during knee flexion and extension). (Figure 3) As described above, real-time kinematic feedback was provided during each training session to ensure that participants maintained proper kinematics. Two minutes of rest were provided between each training block.
FIGURE 3.
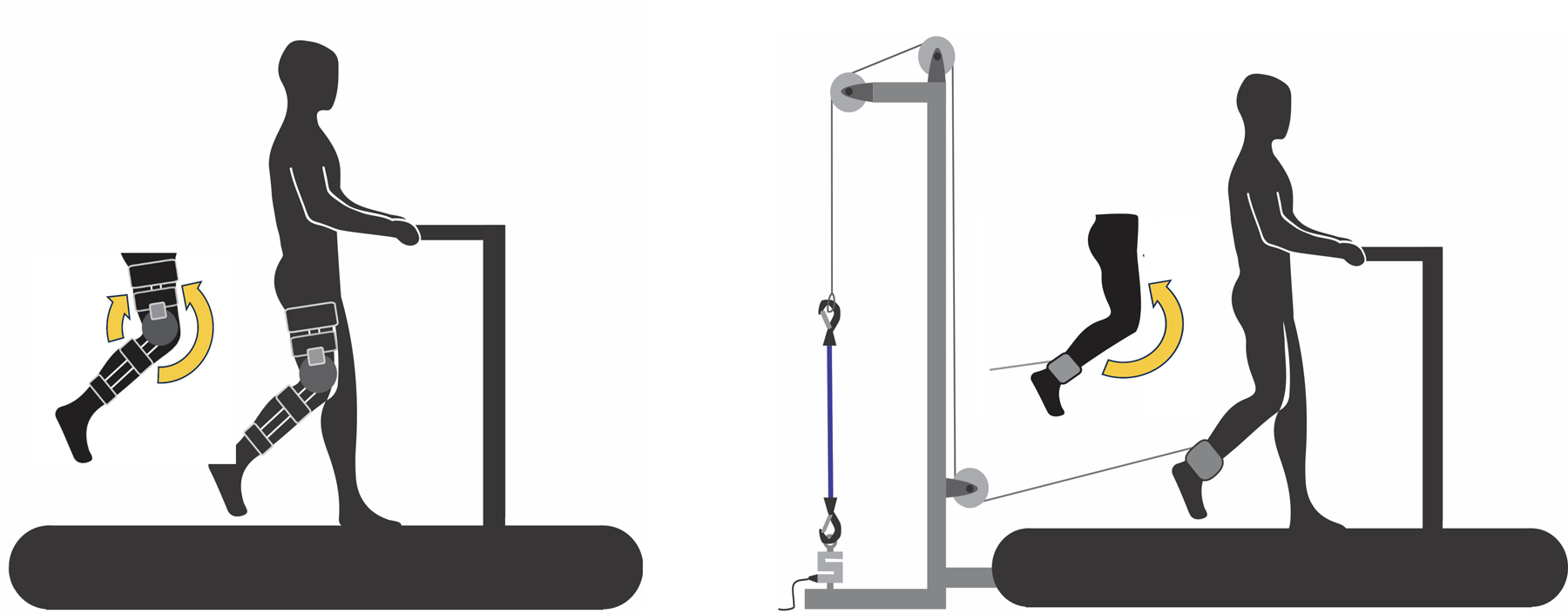
Schematic showing a participant training with the BRACE (left) and the BAND (right). The BRACE provided bi-directional resistance across the knee requiring activation of the quadriceps and hamstrings, while the BAND provided uni-directional resistance during knee extension.
FRT with Elastic Bands
Participants randomized to the BAND group completed training in the same manner as the BRACE group with the exception that a brace was not worn, and the resistance was instead applied through an elastic band pulley system. For participants in this group, training required a single velcro strap to be secured proximal to the ankle malleoli without interfering with the ankle joint marker necessary for creating target trajectories. This strap was attached to a pulley system with embedded elastic band(s) (Theraband, Akron,OH) that applied resistance to the ACL reconstructed leg (Figure 3). The resistance applied was uni-directional resisting the quadriceps musculature during knee extension. As with the BRACE group, resistance was applied/adjusted in the BAND group to meet a perceived effort between 5–7 on the OMNI scale by increasing the stiffness of the elastic bands (e.g., changing the elastic band color and/or the quantity of bands).
Target Match Condition
Participants randomized to the TARGET MATCH condition wore the brace during training but did not receive any resistance. Participants trained for six, 5-minute blocks, while being asked to target match the up-scaled trajectories as was done for the other groups.
Statistical Analysis
Linear mixed models were run for the knee extension (primary outcome) and flexion strength for the ACL reconstructed and non-reconstructed limbs where group (BRACE, BAND, TARGET MATCH) and time (PRE, POST, POST-2) were entered as the independent variables and sex, age, graft type, number of training sessions, and baseline strength were entered as covariates. Sidak multiple comparison procedures were used for post hoc analyses. One-way ANOVAs were used to compare demographics between groups. An alpha level of P≤0.05 was considered significant for all tests. Cohen’s d effect sizes with 95% confidence intervals were calculated for the ACL reconstructed limb between the three study groups. An intent-to-treat analysis could not be performed as data from the four subjects who dropped from the study after randomization could not be collected due to the COVID-19 pandemic (e.g., there were country-wide lockdowns and University research shutdowns preventing our ability to collect outcome measures).
RESULTS
Participant demographics are in Table 1. The OMNI scores for participants in all three groups are provided in Figure 4. Effect sizes for between group comparisons for the ACL reconstructed limb can be found in Table 2. No participants reported any adverse events during testing or training. Additionally, no participants complained of pain or discomfort during training or testing.
FIGURE 4.
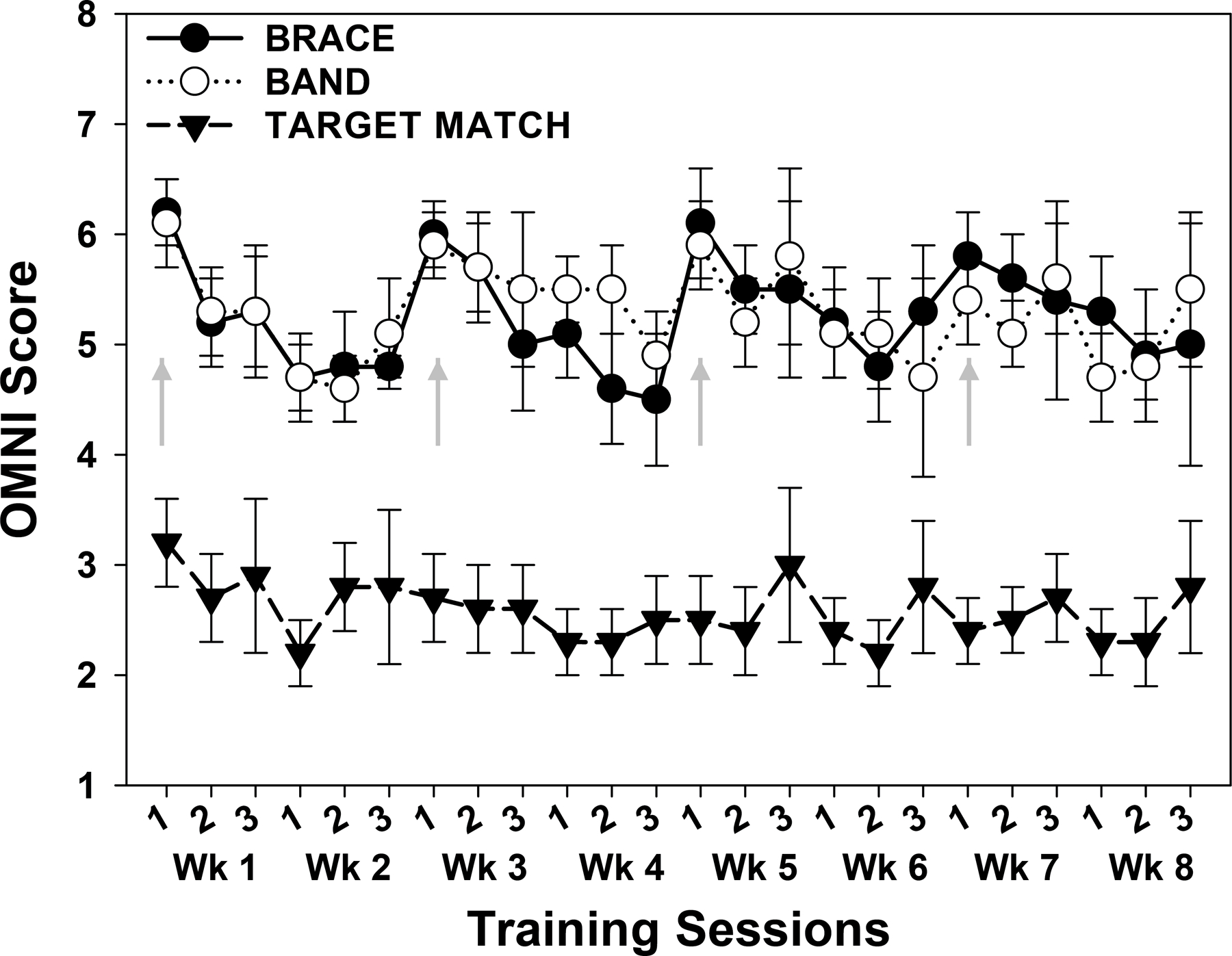
Average OMNI scores for each training session for all three study groups. The OMNI score was used to scale the resistance applied for the BAND and BRACE groups and was adjusted every two weeks. We aimed for BRACE and BAND groups to train between a 5–7 (somewhat difficult) on the OMNI scale. Participants (N=17; BRACE = 6; BAND = 5; TARGET MATCH = 6) completing two sessions a week had resistance adjusted after the second session of weeks 1, 3, 5, and 7. Participants (N = 11; BRACE = 4; BAND =4; TARGET MATCH = 3) completing three sessions a week had resistance adjusted after the third session of weeks 1, 3, 5, and 7. Arrows indicate training sessions during which the resistance was adjusted and increased.
Table 2.
Cohen’s d Effect sizes and (95% Confidence Intervals) comparing groups (BRACE, BAND, TARGET MATCH) at the post-FRT intervention time points (POST and POST-2).
| Group Comparison | Timepoint | ACL Limb Extension Strength | ACL Limb Flexion Strength |
|---|---|---|---|
| BRACE vs. BAND | POST | d= 1.09 (0.13, 2.06) | d= 2.10 (0.98, 3.22) |
| BRACE vs. BAND | POST-2 | d= 0.28 (−0.65, 1.22) | d= 0.77 (−0.19, 1.74) |
| BRACE vs. TARGET MATCH | POST | d= 1.49 (0.47, 2.50) | d= 2.48 (1.29, 3.68) |
| BRACE vs. TARGET MATCH | POST-2 | d= 1.32 (0.29, 2.34) | d= 1.45 (0.41, 2.49) |
| BAND vs. TARGET MATCH | POST | d= 0.45 (−0.49, 1.38) | d= 0.53 (−0.41, 1.47) |
| BAND vs. TARGET MATCH | POST-2 | d= 1.08 (0.03, 2.13) | d= 0.71 (−0.30, 1.72) |
A group x time interaction was noted for knee extensor strength on the ACL reconstructed limb (F=4.381; p=0.007). Post hoc testing revealed that at POST and POST-2 the BRACE group had greater extension strength than the TARGET MATCH group (POST: p=0.008; POST-2: p=0.011), while there was a trend towards significance for the BRACE group to have greater extension strength than the BAND group at POST (p=0.093), but not at POST-2 (p=0.891) (Figure 5). No differences were found between the BAND and TARGET MATCH groups at POST or POST-2 (p>0.05). Furthermore, no group or group x time interaction was noted for the non-reconstructed/uninjured limb (p>0.05). A time main effect (F=5.048; p=0.006) was found for the non-reconstructed limb with knee extension strength being higher at PRE, when compared to POST-2 (p=0.007), but no difference in strength between PRE and POST (p=0.742).
FIGURE 5.
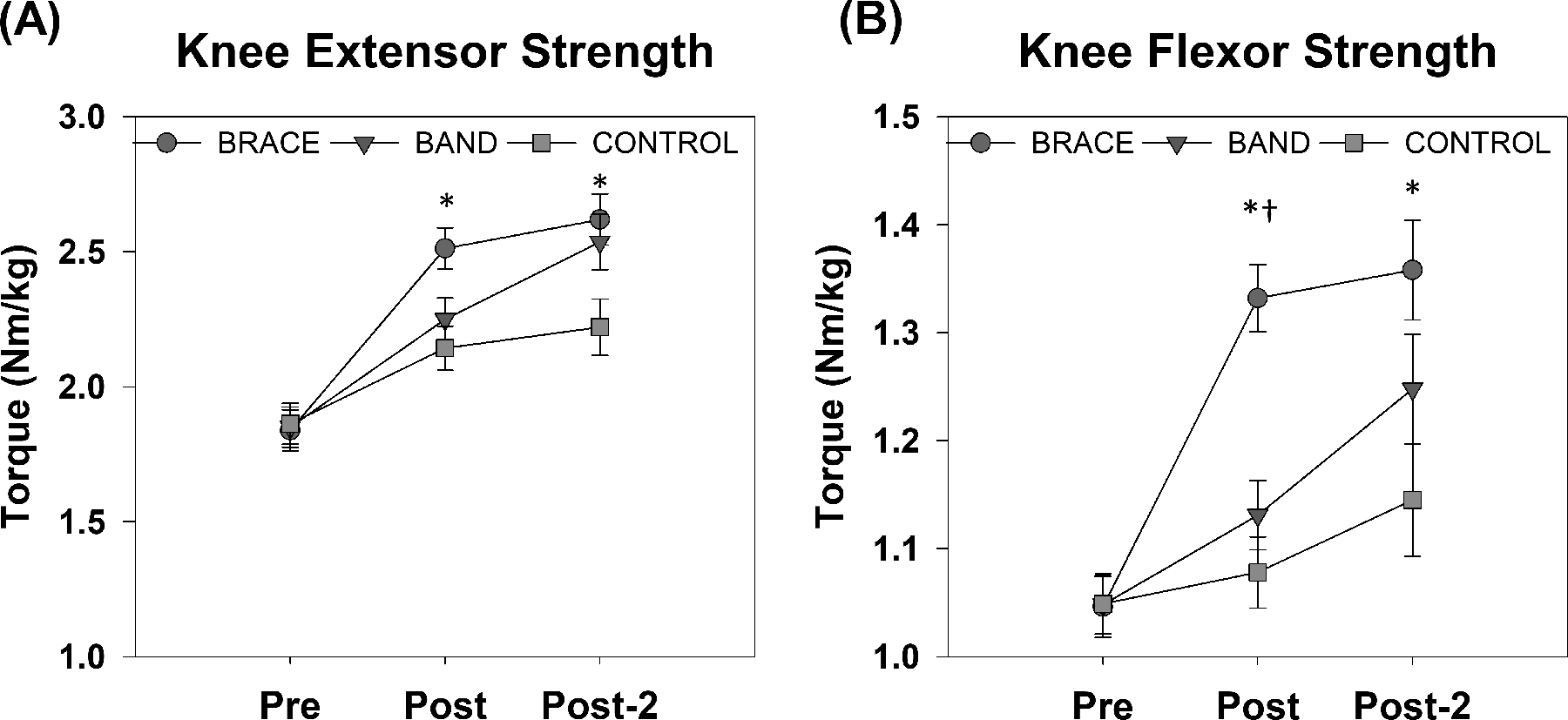
Knee extensor strength (A) and knee flexor strength (B) for the BRACE, BAND, and TARGET MATCH groups prior to intervention (PRE), immediately post-intervention (POST), and approximately 8 weeks after the intervention (POST-2). *indicates that the BRACE group was significantly different than the TARGET MATCH group. † indicates that BRACE group was significantly different than the BAND group.
A group x time interaction was noted for knee flexor strength on the ACL reconstructed limb (F=6.201; p<0.003). Post hoc testing showed that the BRACE group had greater knee flexion strength than the BAND (p=0.011) and TARGET MATCH (p=0.002) groups at POST but was only stronger than the TARGET MATCH group at POST-2 (TARGET MATCH p=0.014; BAND: p=0.319) (Figure 5). No difference in knee flexor strength was noted between the BAND and TARGET MATCH groups at the POST or POST-2 timepoints (p>0.05). Furthermore, no group or group x time interaction was noted for the non-reconstructed (p>0.05). A time main effect (F=11.160; p<0.001) was noted for the non-reconstructed limb whereby flexion strength decreased from PRE to POST (p<0.001) and PRE to POST-2 (p=0.003).
DISCUSSION
This study examined whether FRT could be used as an intervention early in the rehabilitation process to improve thigh muscle strength after ACL reconstruction. As hypothesized, we discovered that knee extensor and flexor strength can be improved after ACL reconstruction by implementing FRT. However, we did find that completing FRT with the custom-designed brace produced better results than FRT applied with elastic bands. Overall, these results support that FRT could supplement traditional rehabilitation after ACL reconstruction to improve thigh muscle strength.
Restoration of quadriceps muscle strength after ACL reconstruction represents a clinical conundrum that requires resolution to maximize knee joint health. Thus, the finding that FRT (BRACE) when delivered alongside traditional ACL rehabilitation resulted in greater quadriceps strength compared to traditional rehabilitation alone (TARGET MATCH) suggests that FRT is a promising approach to aid in re-establishing quadriceps strength after ACL reconstruction. ACL reconstruction participants in the FRT BRACE group realized, on average, a 42% increase in strength from pre- to post-intervention, while the TARGET MATCH group only realized an 18% change. Previous work in ACL reconstruction patients comparing a group receiving FRT during walking to a group receiving no FRT, failed to show improvements in thigh muscle strength.(33) Direct comparison of our work to this prior study is difficult due to the different brace design, resistance dosage, and time of brace application. Any one of these differences could account for the disparate results between studies. The improvements in quadriceps strength in the BRACE group of our study might be the result of higher quadriceps activation while training with our brace device. We have shown previously that the brace used in the current study improves quadriceps activation in both healthy adults (20) and those with stroke (34). Thus, similar effects (i.e., increased quadriceps activation) might have occurred in the ACL reconstruction patients randomized to the BRACE group during the eight weeks of FRT. An increase in quadriceps activation during FRT could have translated into the improvements in quadriceps strength noted for the BRACE group.
In addition to the immediate gains in knee extensor strength realized by the BRACE group, these participants also demonstrated sustained gains in knee extensor strength approximately eight weeks after the FRT intervention. Specifically, the BRACE group had a 48% increase in strength from baseline and a 5% increase in strength from POST at the POST-2 testing timepoint, while the TARGET MATCH group demonstrated a 24% and 5% increase in strength at those respective timepoints. Maintenance of strength gains or continued improvement in strength after the FRT intervention would be expected as standard of care rehabilitation continued, which includes resistance exercises targeting the quadriceps. It is also possible that the BRACE group adopted muscle activation patterns after training that resembled those adopted while wearing the FRT brace and therefore continued to walk with greater quadriceps activation after FRT ended. We contend the former explanation is more likely as aftereffects, at least from one session or FRT training, are short-lived and typically washout in minutes.(20, 34) Furthermore, if quadriceps activation continued to be increased in the BRACE group we might expect greater knee extensor strength gains from the POST to POST-2 time points in the BRACE group, compared with the TARGET MATCH group, but this was not the case (both BRACE and TARGETMATCH had a 5% increase in strength from POST to POST-2).
We were surprised that the BAND group did not realize significant gains in knee extensor strength when compared to the TARGET MATCH group. The elastic band device used to deliver FRT is designed to isolate/target the quadriceps during the swing phase of gait. A musculoskeletal model has shown that applying FRT using elastic bands, like we have done here, increases activation of the quadriceps musculature upwards of 190% when compared with normal, unresisted walking.(22) As such, we had expected that the resistance applied to the quadriceps via the elastic bands would lead to improvements in knee extensor strength. There are a few potential explanations for why strength differences were not noted. First, quadriceps activation during the resisted walking using the elastic bands may have been less than expected. ACL patients may have activated the hip flexors more and the quadriceps less than our model predicted to minimize anterior tibial translation. Second, the resistance provided by the elastic bands may have not been enough to translate to strength gains. Third, our sample size may have been too small. Regardless, our data support resistance applied via the brace is the preferred method to deliver FRT.
Knee flexion strength also improved significantly in the BRACE group compared with the BAND and TARGET MATCH groups at POST. The BRACE group realized strength gains >30% from baseline to POST, while the BAND and TARGET MATCH groups demonstrated a less than 10% change at POST (BAND = 6%; TARGET MATCH = 8%). Furthermore, the change in knee flexion strength for the BRACE group remained higher at POST-2 (34% increase from PRE) when compared to the TARGET MATCH (17% increase from PRE). The custom brace is designed to provide bi-directional resistance during knee flexion and extension and as such this result is not surprising. In our previous work in healthy participants, hamstring activation was increased several folds during resisted walking with a brace compared to unresisted walking, providing support that the hamstrings are more active during this type of FRT, which could lead to strength gains. While restoration of hamstring strength is usually achieved after ACL reconstruction from standard rehabilitation, the task-specific nature of this strength training may translate better to biomechanical improvements/efficiencies during walking or other functional tasks and thus may be of greater benefit. Future work should focus on the relationship between strength gains noted here and the resultant biomechanical adaptations.
A small decline in the non-reconstructed limb knee flexion strength was noted between the PRE and POST and PRE and POST-2 time points for all study participants. We attribute this finding to the fact that ACL rehabilitation primarily focuses on strengthening the muscles of the ACL limb and thus without stimuli (e.g., resistance exercise) to maintain or increase knee flexion strength it decreased over time.
This study is the first to illustrate the feasibility of an 8-week FRT training intervention. The FRT delivered with the brace was not only effective, but participants did not report any discomfort or pain with the brace/training and no adverse events occurred during the trial. This suggests that FRT can be delivered safely to patients after ACL reconstruction. The brace also has the advantage of being portable and participants/patients could wear it outside of the lab to complete FRT, which could potentially increase compliance in a clinical setting. Furthermore, the brace could also be used during other tasks such as squatting, stair climbing, etc. which could lead to improved transfer of benefits to these types of activities.
This work is not without limitations. First, while a power analysis was conducted prior to the start of the study and we enrolled an adequate number of participants, four participants were unable to complete the study. Thus, sample size may have not been adequate to detect all differences. We encourage future studies with larger sample sizes to determine if FRT with the elastic band can improve strength like FRT with the brace. Like was mentioned above, the training load for the brace and the band was not quantitatively calculated as is typically done in training studies. Instead, participants trained at a perceived level of difficulty using the OMNI scale. Calculating the resistance provided by the BRACE and BAND is quite complicated and not clinically feasible which is why we utilized a perceived level of difficulty. We provide in the Supplemental Appendix (see Supplemental Digital Content, SDC 1) a calculation to estimate the torque/resistance provided by each device and sample data in a single participant from both the BRACE and BAND groups so the resistance provided by these devices could be visualized. Finally, the resistance level for the BRACE group was limited by the participant’s knee flexor strength, as the absolute strength of the knee flexors is typically lower than the knee extensors. As a result, the load experienced by the quadriceps muscle during FRT could have been lower than the hamstring muscles, which could explain greater differences in the flexor strength. Future studies should evaluate if modifying the BRACE to provide uni-directional resistance could better target the quadriceps muscles.
Prior to implementing FRT using the devices described here into clinical practice more research is necessary. In particular, large-scale clinical trials demonstrating their effectiveness should be conducted. Further, trials which refine the dosage necessary to realize effects are also warranted. Further, the gearbox (BaneBots P60) used in the knee brace has a rated torque limit of 47.5 N·m. While this was sufficient for many individuals, we have experienced several gearbox breakages over the course of the study due to repeated use. As a result, more powerful custom-designed gearboxes with higher torque limits might be needed for repeated use in the clinic. We do believe that once future studies are completed, widespread dissemination of these devices and their use in the clinical setting is very feasible.
CONCLUSIONS
Eight weeks of FRT while walking with a brace providing bi-directional resistance leads to immediate and sustained improvements in thigh muscle strength after ACL reconstruction. Further, the strength gains realized through FRT remained eight weeks after the completion of the training, suggesting FRT can lead to longer-term improvements in muscle function. Overall, the gains in knee extensor strength realized by the BRACE group highlight the potential value of incorporating FRT into ACL rehabilitation. FRT could prove to be an asset to restoring quadriceps strength to acceptable levels prior to return to activity to aid in preventing re-injury and the onset of post-traumatic OA.
Supplementary Material
Acknowledgements:
This work was supported by the National Institute of Child Health and Human Development of the National Institutes of Health (Grant # R21 HD092614). CK has patents on some of the FRT devices used in this study. None of the other authors report any conflict of interest for the current study. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The results of the present study do not constitute endorsement by the American College of Sports Medicine.
Funding Source
This work was supported by the National Institute of Child Health and Human Development of the National Institutes of Health (Grant # R21 HD092614). CK has patents on some of the FRT devices used in this study.
Footnotes
Conflict of Interest
None of the other authors report any conflict of interest for the current study. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The results of the present study do not constitute endorsement by the American College of Sports Medicine.
SUPPLEMENTAL DIGITAL CONTENT
SDC 1: FRT Strength_Appendix 1.docx – Appendix
REFERENCES
- 1.Curran MT, Bedi A, Kujawa M, Palmieri-Smith R. A cross-sectional examination of quadriceps strength, biomechanical function, and functional performance from 9 to 24 months after anterior cruciate ligament reconstruction. Am J Sports Med 2020;48(10):2438–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hunnicutt JL, McLeod MM, Slone HS, Gregory CM. Quadriceps neuromuscular and physical function after anterior cruciate ligament reconstruction. J Athl Train 2020;55(3):238–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuenze C, Pietrosimone B, Lisee C et al. Demographic and surgical factors affect quadriceps strength after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2019;27(3):921–30. [DOI] [PubMed] [Google Scholar]
- 4.Lisee C, Lepley AS, Birchmeier T, O’Hagan K, Kuenze C. Quadriceps strength and volitional activation after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Sports Health 2019;11(2):163–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med 2008;27(3):405–24, vii-ix. [DOI] [PubMed] [Google Scholar]
- 6.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 2004;50(10):3145–52. [DOI] [PubMed] [Google Scholar]
- 7.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med 2016;50(13):804–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pietrosimone B, Lepley AS, Harkey MS et al. Quadriceps strength predicts self-reported function post-ACL reconstruction. Med Sci Sports Exerc 2016;48(9):1671–7. [DOI] [PubMed] [Google Scholar]
- 9.Tourville TW, Jarrell KM, Naud S, Slauterbeck JR, Johnson RJ, Beynnon BD. Relationship between isokinetic strength and tibiofemoral joint space width changes after anterior cruciate ligament reconstruction. Am J Sports Med 2014;42(2):302–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 2007;35(10):1756–69. [DOI] [PubMed] [Google Scholar]
- 11.Damas F, Phillips S, Vechin FC, Ugrinowitsch C. A review of resistance training-induced changes in skeletal muscle protein synthesis and their contribution to hypertrophy. Sports Med 2015;45(6):801–7. [DOI] [PubMed] [Google Scholar]
- 12.Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 2009;37(5):890–7. [DOI] [PubMed] [Google Scholar]
- 13.Petterson SC, Mizner RL, Stevens JE et al. Improved function from progressive strengthening interventions after total knee arthroplasty: a randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum 2009;61(2):174–83. [DOI] [PubMed] [Google Scholar]
- 14.Lepley LK, Wojtys EM, Palmieri-Smith RM. Combination of eccentric exercise and neuromuscular electrical stimulation to improve quadriceps function post-ACL reconstruction. Knee 2015;22(3):270–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams G, Kahn M, Randall A. Strength training for walking in neurologic rehabilitation is not task specific: a focused review. Am J Phys Med Rehabil 2014;93(6):511–22. [DOI] [PubMed] [Google Scholar]
- 16.Manini T, Marko M, VanArnam T et al. Efficacy of resistance and task-specific exercise in older adults who modify tasks of everyday life. J Gerontol A Biol Sci Med Sci 2007;62(6):616–23. [DOI] [PubMed] [Google Scholar]
- 17.Piva SR, Childs JD, Klucinec BM, Irrgang JJ, Almeida GJ, Fitzgerald GK. Patella fracture during rehabilitation after bone-patellar tendon-bone anterior cruciate ligament reconstruction: 2 case reports. J Orthop Sports Phys Ther 2009;39(4):278–86. [DOI] [PubMed] [Google Scholar]
- 18.Nichols ZW, O’Brien D, White SG. Is resistance training intensity adequately prescribed to meet the demands of returning to sport following anterior cruciate ligament repair? A systematic review. BMJ Open Sport Exerc Med 2021;7(3):e001144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duclos C, Nadeau S, Bourgeois N, Bouyer L, Richards CL. Effects of walking with loads above the ankle on gait parameters of persons with hemiparesis after stroke. Clin Biomech (Bristol, Avon) 2014;29(3):265–71. [DOI] [PubMed] [Google Scholar]
- 20.Washabaugh EP, Claflin ES, Gillespie RB, Krishnan C. A Novel application of eddy current braking for functional strength training during gait. Ann Biomed Eng 2016;44(9):2760–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Washabaugh EP. Functional Resistance Training During Walking: Design, Testing, and Evaluation of Passive and Semi-Passive Wearable Devices for Providing Targeted Resistance to the Leg During Gait. Michigan: University of Michigan; 2021.
- 22.Washabaugh EP, Augenstein TE, Krishnan C. Functional resistance training during walking: Mode of application differentially affects gait biomechanics and muscle activation patterns. Gait Posture 2020;75:129–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 2009;41(4):1149–60. [DOI] [PubMed] [Google Scholar]
- 24.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39(2):175–91. [DOI] [PubMed] [Google Scholar]
- 25.Krishnan C, Theuerkauf P. Effect of knee angle on quadriceps strength and activation after anterior cruciate ligament reconstruction. J Appl Physiol (1985) 2015;119(3):223–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Snyder-Mackler L, De Luca PF, Williams PR, Eastlack ME, Bartolozzi AR 3rd. Reflex inhibition of the quadriceps femoris muscle after injury or reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am 1994;76(4):555–60. [DOI] [PubMed] [Google Scholar]
- 27.Krishnan C. Learning and interlimb transfer of new gait patterns are facilitated by distributed practice across days. Gait Posture 2019;70:84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krishnan C, Dharia AK, Augenstein TE et al. Learning new gait patterns is enhanced by specificity of training rather than progression of task difficulty. J Biomech 2019;88:33–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krishnan C, Washabaugh EP, Reid CE, Althoen MM, Ranganathan R. Learning new gait patterns: Age-related differences in skill acquisition and interlimb transfer. Exp Gerontol 2018;111:45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krishnan C, Washabaugh EP, Seetharaman Y. A low cost real-time motion tracking approach using webcam technology. J Biomech 2015;48(3):544–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garcia SA, Brown SR, Koje M, Krishnan C, Palmieri-Smith RM. Gait asymmetries are exacerbated at faster walking speeds in individuals with acute anterior cruciate ligament reconstruction. J Orthop Res 2022;40(1):219–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Utter AC, Robertson RJ, Green JM, Suminski RR, McAnulty SR, Nieman DC. Validation of the Adult OMNI Scale of perceived exertion for walking/running exercise. Med Sci Sports Exerc 2004;36(10):1776–80. [DOI] [PubMed] [Google Scholar]
- 33.Rocchi JE, Labanca L, Luongo V, Rum L. Innovative rehabilitative bracing with applied resistance improves walking pattern recovery in the early stages of rehabilitation after ACL reconstruction: a preliminary investigation. BMC Musculoskelet Disord 2020;21(1):644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Washabaugh EP, Krishnan C. A wearable resistive robot facilitates locomotor adaptations during gait. Restor Neurol Neurosci 2018;36(2):215–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


