Abstract
Child maltreatment is associated with asthma in adults. We examined whether lifetime major depressive disorder (MDD) or lifetime generalized anxiety disorder (GAD) mediate an association between child maltreatment and current asthma among 81,105 British adults in the UK Biobank who completed a mental health survey and had complete data on child maltreatment, GAD, MDD, asthma, and relevant covariates but no diagnosis of chronic obstructive pulmonary disease. Child maltreatment was ascertained based on answers to the five questions in the Childhood Trauma Screener. Two mediators, lifetime MDD and GAD, were assessed based on the Composite International Diagnostic Interview Short Form (CIDI-SF). Current asthma was defined as physician-diagnosed asthma and wheeze or whistling in the chest in the previous year. Logistic regression was used for the multivariable analysis of child maltreatment and current asthma, and a mediation analysis was conducted to estimate the contributions of lifetime MDD and lifetime GAD to the child maltreatment-current asthma association. In a multivariable analysis, any child maltreatment was associated with asthma (adjusted odds ratio [aOR]=1.22, 95% confidence interval [CI]=1.15 to 1.28, P<0.01). In a mediation analysis adjusted for household income, educational attainment, smoking status, pack-years of smoking, and other covariates, lifetime GAD and lifetime MDD explained 21.8% and 32.5%, respectively, of the child maltreatment-current asthma association. Similar results were obtained after excluding current smokers and former smokers with ≥10 pack-years of smoking from the mediation analysis. Our findings suggest that GAD and MDD mediate an association between child maltreatment and asthma in adults, independently of smoking.
Summary
In British adults, child maltreatment is significantly associated with current asthma, and lifetime major depression disorder and lifetime generalized anxiety disorder mediates or explains part of this association, independently of smoking.
INTRODUCTION
Asthma affects approximately 339 million people and leads to substantial disability among elderly adults worldwide [1]. In the United Kingdom (U.K.), 4.3 million adults have clinician-diagnosed-and-treated asthma, including approximately 200,000 subjects with severe asthma not responding to usual treatment. The annual economic burden from asthma in the U.K. has been estimated as £1.1 billion [2].
Child maltreatment, an adverse childhood experience (ACE), includes various forms of physical and emotional abuse or neglect and sexual abuse. Worldwide, it is estimated that 25% of adults experienced physical abuse as children, with sexual abuse more prevalent in girls (~20%) than in boys (~7.7%) [3]. In the U.K., the 2019 Crime Survey for England and Wales (CSEW) estimated that approximately 21% of adults aged 18 to 74 years had experienced child maltreatment before age 16 years [4].
ACEs have been predominantly studied in relation to psychosocial outcomes [5, 6], but a growing body of evidence links ACEs to adult risk behaviors, health-related quality of life, and chronic diseases such as asthma [7–9]. ACEs have been associated with increased risk of asthma during adulthood, including adult-onset asthma [10, 11]. This association may be due to chronic stress [12] leading to dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis and/or abnormal expression of genes that regulate relevant autonomic, neuroendocrine, and immunologic responses through epigenetic mechanisms [13, 14].
Although anxiety and depression have been implicated in the pathogenesis of asthma in adults [14–17], it is not known whether these conditions mediate the association between child maltreatment and asthma during adulthood. We hypothesized that child maltreatment would be associated with asthma among British adults participating in the UK Biobank, and that such association would be mediated by lifetime major depressive disorder (MDD) and lifetime generalized anxiety disorder (GAD).
METHODS
Study design and study population
The UK Biobank is a national, prospective, population-based study established to identify determinants of complex diseases and improve the health outcomes of British adults. Approximately 9.2 million individuals aged 40–69 years who lived within 25 miles of twenty-two assessment centers in England, Wales, and Scotland were invited to enter the cohort, and ~500,000 (5.5%) of those 9.2 million people volunteered to participate in the baseline assessment between 2006 and 2010 [18]. Extensive data, including questionnaires, physical measures, and biological samples were collected at baseline, with longitudinal follow-up for a wide range of health-related outcomes [18, 19]. To identify mental health disorders and to examine the detrimental impact of such disorders on both physical disease onset and outcomes in the UK Biobank, an expert working group designed a web-based mental health questionnaire (MHQ) in 2015 [20]. A total of 339,092 participants were subsequently invited to participate in the mental health survey and 157,366 (46% of those emailed) completed the MHQ online in 2017[20]. The UK Biobank was approved by the UK National Health Service National Research Ethics Service (Ref 11/NW/0382) and informed consent was obtained from all participants. Details of the methods, protocols, and definitions used in the study can be found at the UK Biobank website (https://www.ukbiobank.ac.uk/).
The current study was conducted using the UK Biobank Resource under application #43252. The flowchart for selection of participants from the UK Biobank into the current analysis is shown in Supplementary Figure 1. Of the 157,366 participants who responded to the online MHQ, 120,732 were eligible for the analysis, as they reported no diagnosis of chronic obstructive pulmonary disease (COPD) and had complete information on child maltreatment, lifetime MDD or GAD, and asthma status. Compared with these 120,732 participants, the 36,634 participants who responded to the MHQ but were not eligible for this analysis (due to missing data on the exposure and outcome variables) were more likely to be older, female, obese, and former or current smokers; and to have lower household income or educational attainment, current asthma, MDD, GAD, and to report child maltreatment (Supplementary Table 1). Of the 120,732 eligible participants, 81,105 had complete data on all relevant covariates and were thus included in the primary analysis for this study.
Child maltreatment
Child maltreatment while growing up was self-reported by participants using the five questions in the Childhood Trauma Screener (CTS), a validated shortened version of the Childhood Trauma Questionnaire (CTQ), a reliable and cost-efficient screening tool for large epidemiologic studies [20, 21]. CTS takes one question from each domain of the CTQ and consists of one 5-point Likert scale item for each type of child maltreatment: physical abuse, emotional abuse, sexual abuse, physical neglect, and emotional neglect. The threshold values on the Likert scale derived from the validation study were used to define the presence or absence of each type of child maltreatment [21, 22]. In this analysis, our primary exposure of interest was any (at least one) type of child maltreatment. In secondary analyses, we examined the association between the number of types of child maltreatment (range=0 to 5) and each type of child maltreatment with asthma.
Outcomes
Current asthma was defined by selection of “asthma” as an answer to the following question: “Has a doctor ever told you that you have had any of the following conditions (you can select more than one answer): 1) blood clot in the leg, 2) blood clot in the lung, 3) emphysema/chronic bronchitis, 4) asthma, 5) hay fever, allergic rhinitis or eczema 6) None of the above” and a “Yes” answer to the question “In the last year, have you ever had wheeze or whistling in the chest?”. Control subjects were participants who did not select “asthma” as an answer to the first question and had no wheeze or whistling in the chest in the prior year. To reduce potential misclassification of COPD or other conditions as current asthma, participants were excluded from the analysis if they reported: physician-diagnosed asthma but no current wheezing, current wheezing but no physician-diagnosed asthma, or physician-diagnosed emphysema/chronic bronchitis.
Psychological factors
Because depression and anxiety were two of the most prevalent mental health disorders among UK Biobank participants [20], we assessed whether lifetime major depressive disorder (MDD) and lifetime generalized anxiety disorder (GAD) could mediate an association between child maltreatment and current asthma. Lifetime (ever) assessment of MDD and GAD was based on the Composite International Diagnostic Interview Short Form (CIDI-SF). The CIDI-SF is a World Health Organization (WHO) instrument for mental health surveys that has been validated and allows comparison between UK Biobank cohort and other cohorts [23] [20]. In brief, lifetime MDD was defined as having at least one core symptom of depression (persistent sadness or a loss of interest) for most or all days over a two-week period plus at least one non-core depressive symptom (feelings of tiredness, weight change, sleep change, difficulty concentrating, feelings of worthlessness, and thoughts of death) with some or a lot of impairment experienced during the worst two-week period of depression or low mood. Lifetime GAD was defined by excessive worrying about a number of issues (occurring most days for six months) that is difficult to control, with three or more somatic symptoms and functional impairment (being restless; being keyed up or on edge; having difficult to keep one’s mind on what s/he is doing; being more irritable than usual; having tense, sore, or aching muscles; and often having trouble falling or staying asleep) [20].
Statistical analysis
Bivariate analyses were conducted using two-sided Wald chi-square tests or t-tests, as appropriate. Logistic regression was used for the multivariable analyses of child maltreatment and current asthma. Known or potential confounders of the relation between child maltreatment and current asthma were included in the multivariable models. All models were adjusted for age, sex, race (Caucasian vs. other), education (college or university degree, A/AS/O/General Certificate of Secondary Education [GCSE] levels or equivalent, and others), annual household income (< £31,000 vs. ≥ £31,000 per year, near the median household income for the UK in 2019)[24], body mass index (BMI), smoking status (never, former, or current), pack-years of cigarette smoking, and serum C-reactive protein (CRP) level. A multiple imputation procedure was used to conduct a sensitivity analysis in 120,732 subjects in the UK Biobank (the 81,105 participants in the current study and 39,627 participants who were eligible but were excluded from this study because of missing data for covariates (see Supplementary Figure 1). In brief, the Markov Chain Monte Carlo (MCMC) method was used to create five imputed data sets, and regression analyses were then repeatedly performed for each of these five data sets. The final parameter estimates were generated by combining five sets of regression coefficients using Rubin’s combining rules [25].
The causal mediation analysis to estimate the total, direct, and indirect effects of exposure to any child maltreatment on physician-diagnosed asthma with lifetime MDD or GAD as mediators is based on a counterfactual framework [26–29]. This approach allows the presence of a significant interaction between the exposure and mediator (suggesting unmeasured confounding), as well as decomposition of the estimated total effect into estimates of direct and indirect effects. A causal diagram of our hypothesized relationship and corresponding assumptions is presented in Supplemental Figure 2. Logistic regression was used to estimate both indirect effects and direct effects in the mediation analysis, while adjusting for potential confounders. The percentage-mediated measure is obtained by dividing the indirect effect by the total effect. Standard errors and percentile bootstrap confidence intervals for effects estimates was computed based on 1000 bootstrap resamples. Repeated single mediator analyses were performed for each mediator (lifetime MDD; lifetime GAD; and having either lifetime MDD, lifetime GAD, or both conditions). All mediation analyses were adjusted for the same covariates as in the main analysis of child maltreatment and current asthma.
All statistical analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC) and two-sided P-values <0.05 were considered significant. The causal mediation analysis was conducted using the SAS CAUSALMED procedure.
RESULTS
Table 1 shows the main characteristics of the 81,105 study participants by asthma status. Compared with control subjects (n=74,707), subjects with current asthma (n=6,398) were significantly more likely to report lifetime MDD (26.2% vs. 17.5%) and lifetime GAD (11.5% vs. 7%), and to have experienced child maltreatment (36.2% vs. 30.6%). There were other statistically significant but smaller differences between subjects with current asthma and control subjects, namely that those with current asthma were younger and more likely to be non-White or non-Caucasian and current smokers, and had lower pack-years of cigarette smoking, higher BMI, and higher serum CRP levels. Approximately one third of all study participants reported having ever experienced child maltreatment.
Table 1.
Baseline characteristics of study participants by asthma status
| Characteristics | No (%) of Participants | ||
|---|---|---|---|
| Control subjects (n=74,707) | Current asthma (n=6,398) | P-value* | |
| Age at recruitment, mean (SD), year | 55.3 (7.7) | 54.2 (7.9) | <0.01 |
| Female | 41295 (55.3) | 3603 (56.3) | 0.11 |
| White or Caucasian | 72600 (97.2) | 6179 (96.6) | <0.01 |
| Annual household income < £30,000 | 24681 (33.0) | 2176 (34.0) | 0.11 |
| Education | |||
| College or university degree | 38052 (50.9) | 3251 (50.8) | 0.19 |
| A/AS/O/GCSE levels or equivalent | 28989 (38.8) | 2446 (38.2) | |
| Others | 7666 (10.3) | 701 (11.0) | |
| Body mass index, mean (SD), kg/m2 | 26.4 (4.3) | 27.8 (5.2) | <0.01 |
| Obesity | 12477 (16.8) | 1710 (26.9) | <0.01 |
| Smoking status | |||
| Never | 52835 (70.7) | 4455 (69.6) | <0.01 |
| Former | 18390 (24.6) | 1553 (24.3) | |
| Current | 3482 (4.7) | 390 (6.1) | |
| Pack-years of cigarette smoking, mean (SD) | 5.3 (11.5) | 5.6 (12.0) | 0.04 |
| Serum C-reactive protein, mean (SD), mg/L | 2.0 (3.6) | 2.8 (4.6) | <0.01 |
| Asthma-related hospitalization, ever | - | 214 (3.3) | - |
| Major depressive disorder, lifetime | 13075 (17.5) | 1679 (26.2) | <0.01 |
| Generalized anxiety disorder, lifetime | 5221 (7.0) | 737 (11.5) | <0.01 |
| Any child maltreatment | 22877 (30.6) | 2318 (36.2) | <0.01 |
| Number of child maltreatment types | |||
| None | 51830 (69.4) | 4080 (63.8) | <0.01 |
| One | 14647 (19.6) | 1274 (19.9) | |
| Two | 5125 (6.9) | 564 (8.8) | |
| Three or more | 3105 (4.2) | 480 (7.5) | |
GCSE=General Certificate of Secondary Education.
Comparison of participants with current asthma vs. controls. Control subjects had neither self-reported asthma nor wheezing in the previous year.
The results of the multivariable analysis of child maltreatment and current asthma are shown in Table 2. In this analysis, participants who experienced any child maltreatment had 1.22 times significantly higher odds of current asthma than those who did not. To examine whether more severe child maltreatment is more strongly associated with asthma, we conducted a multivariable analysis of the number of child maltreatment types and current asthma. In this analysis, participants who reported two or more types of child maltreatment had 1.30 to 1.73 times significantly higher odds of asthma than those who did not experience any type of child maltreatment (Table 2). In a separate analysis examining each of the five types of child maltreatment, physical abuse and emotional abuse were more strongly associated with asthma than other types of child maltreatment (Table 3).
Table 2.
Multivariable analysis of child maltreatment and current asthma
| Exposure | All participants | Women | Men |
|---|---|---|---|
| Odds Ratio (95% confidence interval) | |||
| Any child maltreatment | 1.22 (1.15 – 1.28)† | 1.24 (1.15 – 1.33)† | 1.19 (1.09 – 1.29)† |
| Number of child maltreatment types | |||
| None | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| One | 1.07 (1.01 – 1.15)* | 1.06 (0.97 – 1.16) | 1.10 (0.99 – 1.21) |
| Two | 1.30 (1.19 – 1.43)† | 1.33 (1.17 – 1.50)† | 1.28 (1.10 – 1.48)† |
| Three or more | 1.73 (1.56 – 1.92)† | 1.78 (1.57 – 2.01)† | 1.63 (1.34 – 1.97)† |
All models adjusted for age at recruitment, sex (in all participants), race, education, annual household income, body mass index, smoking status, pack-years of cigarette smoking, and serum level of C-reactive protein.
P<0.05,
P <0.01
Table 3.
Multivariable analysis of type of child maltreatment and asthma
| Type of child maltreatment (Not mutually exclusive) | All participants | Women | Men |
|---|---|---|---|
| Odds Ratio (95% Confidence Interval) | |||
| Physical abuse (n=5,885) | 1.44 (1.32 – 1.57)* | 1.48 (1.32 – 1.66)* | 1.40 (1.22 – 1.59)* |
| Emotional abuse (n=6,631) | 1.50 (1.38 – 1.62)* | 1.53 (1.38 – 1.69)* | 1.44 (1.25 – 1.67)* |
| Sexual abuse (n=6,692) | 1.24 (1.14 – 1.36)* | 1.29 (1.16 – 1.43)* | 1.13 (0.95 – 1.33) |
| Physical neglect (n=3,735) | 1.34 (1.20 – 1.49)* | 1.58 (1.39 – 1.81)* | 0.98 (0.81 – 1.19) |
| Emotional neglect (n=16,549) | 1.24 (1.17 – 1.32)* | 1.24 (1.14 – 1.34)* | 1.24 (1.13 – 1.36)* |
All models adjusted for age at recruitment, sex (in all participants), race, education, annual household income, body mass index, smoking status, pack-year of cigarette smoking, and serum level of C-reactive protein.
P <0.01.
After imputing data for missing covariates, we repeated the multivariable analysis of child maltreatment and current asthma in all eligible participants (n=120,732). This sensitivity analysis yielded similar results to those from the analysis that excluded participants with missing covariates (Supplementary Table 2).
Since findings from prior studies have suggested potential sex differences in the long-term health consequences of child maltreatment [30, 31], we repeated the multivariable analysis after stratification by sex. In this analysis, child maltreatment was significantly associated with current asthma in both women and men, but the observed associations were stronger in women than in men (Tables 2 and 3). In a sensitivity analysis, we repeated the multivariable analysis of child maltreatment and asthma after excluding those who reported having been diagnosed with asthma before age 18 years, obtaining similar results (Supplementary Table 3).
To reduce potential misclassification of COPD as asthma and to account for potential effects of smoking on asthma, we repeated the analyses of current asthma after excluding current smokers and former smokers with ≥10 pack-years of smoking from the analysis. These analyses yielded similar results to those including all participants (Table 4).
Table 4.
Multivariable analysis of child maltreatment and current asthma in never smokers and former smokers with < 10 pack-years of cigarette smoking
| Exposure | All participants (n=64,486) |
Women (n=37,152) |
Men (27,334) |
|---|---|---|---|
| Odds Ratio (95% Confidence Interval) | |||
| Any child maltreatment | 1.19 (1.12 – 1.26)† | 1.22 (1.13 – 1.33)† | 1.14 (1.03 – 1.25)* |
| Numbers of child maltreatment type | |||
| None | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| One | 1.08 (0.99 – 1.16) | 1.09 (0.99 – 1.20) | 1.06 (0.94 – 1.19) |
| Two | 1.24 (1.11 – 1.39)† | 1.24 (1.08 – 1.43)† | 1.26 (1.06 – 1.51)* |
| Three or more | 1.66 (1.46 – 1.88)† | 1.73 (1.49 – 2.01)† | 1.48 (1.15 – 1.90)† |
All models adjusted for age at recruitment, sex (in all participants), race, education, annual household income, body mass index, pack-years of cigarette smoking, and serum level of C-reactive protein.
P<0.05,
P <0.01
Supplementary Table 4 shows the results of the analysis of child maltreatment and lifetime MDD or lifetime GAD (potential mediators). In this analysis, any child maltreatment was significantly associated with increased odds of lifetime MDD and lifetime GAD, with stronger effect estimates observed for three or more types of child maltreatment.
Next, we performed a mediation analysis to assess whether the association between child maltreatment and current asthma was mediated through lifetime MDD or lifetime GAD. For ease of exposition and interpretation, we conducted a repeated single mediator analysis (Figure 1). In this analysis, lifetime MDD (panel A) and lifetime GAD (panel B) were each significant mediators of the child maltreatment-asthma association, explaining 32.5% and 21.8%, respectively, of the estimated effects. Having lifetime MDD and/or lifetime GAD explained 38.2% of the child maltreatment and asthma association (panel C). In this mediation analysis, the estimated natural direct effect of child maltreatment on asthma remained significant.
Figure 1.
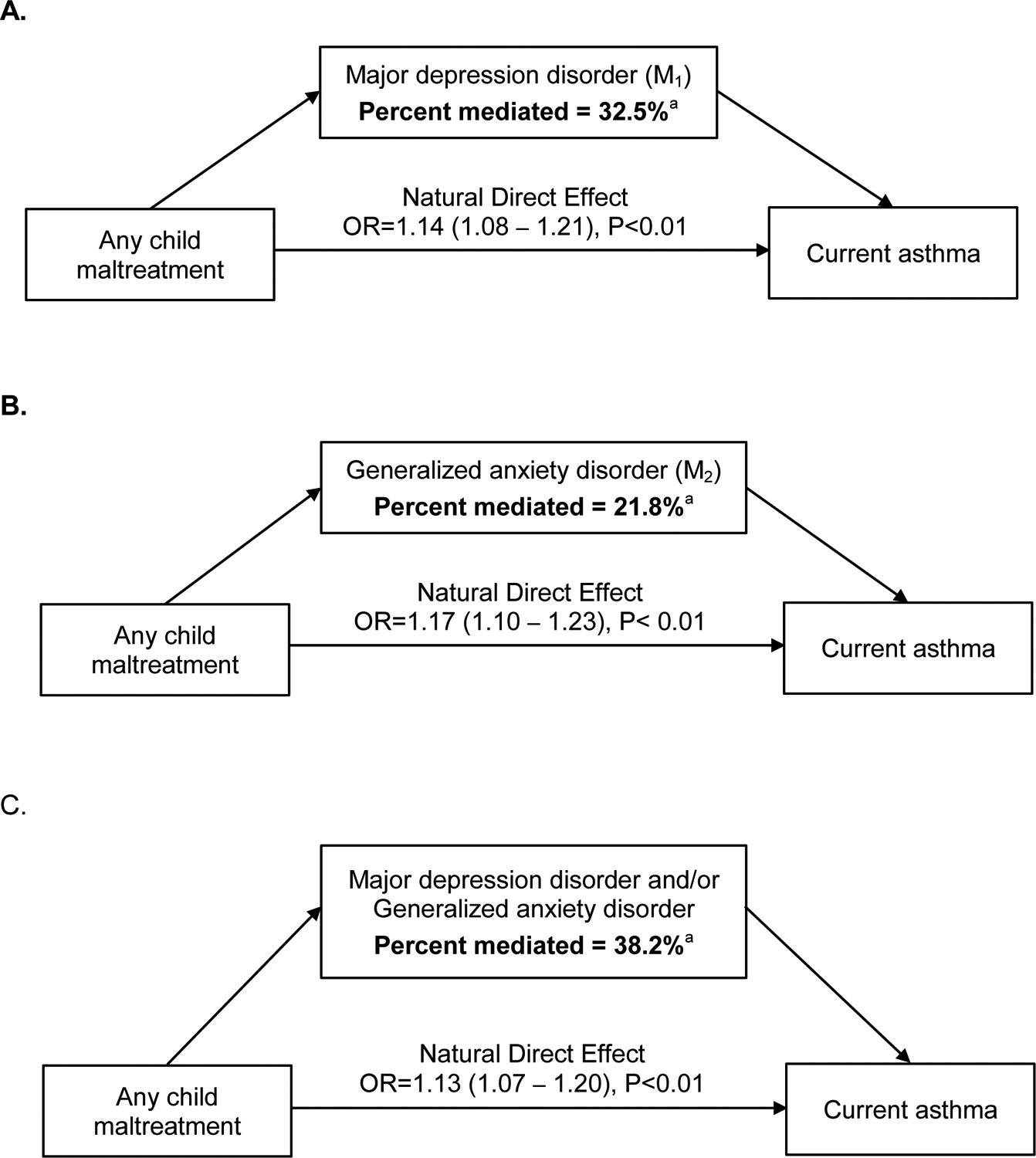
Mediation analysis for any child maltreatment, major depression disorder (mediator, M1), generalized anxiety disorder (M2), major depression disorder or generalized anxiety disorder and current asthma. Mediation analyses were performed for major depression disorder (panel A), generalized anxiety disorder (panel B), and join effect for major depression or generalized anxiety disorder (panel C) separately.
Models adjusted for age at recruitment, sex, race, education, annual household income, body mass index, smoking status, pack-years of cigarette smoking, and serum level of C-reactive protein. aP <0.01
We repeated the mediation analyses after excluding current smokers and former smokers with ≥10 pack-years of smoking, obtaining similar results (Supplementary Figure 3). In a separate sensitivity analysis, we repeated the mediation analysis for MDD after additional adjustment for use of antidepressants in the model, obtaining similar results (data not shown).
Because child maltreatment has been associated with smoking and nicotine dependence [32], we further assessed whether cigarette smoking mediates the estimated effects of child maltreatment on asthma. In this secondary analysis, we did not find that current or former smoking (≥10 pack-years) significantly mediated the estimated effects of child maltreatment on asthma (percent mediated by smoking in an analysis unadjusted for lifetime MDD and lifetime GAD=2.3%, P=0.27; percent mediated by smoking in an analysis adjusted for lifetime MDD and lifetime GAD=1.3%, P=0.63).
DISCUSSION
In this study of British adults who participated in the UK Biobank, child maltreatment was directly associated with current asthma, and lifetime GAD and lifetime MDD were significant mediators of this association. Indeed, GAD explained 21.5% and MDD explained 32.8% of the child maltreatment-current asthma association. Taken together, lifetime MDD and/or lifetime GAD explained 38.2% of the observed association.
Consistent with our overall results for child maltreatment and asthma, studies of U.S. adults (18 years and older) and Canadian adults showed that greater adversity in childhood was associated with increased prevalence of current or lifetime asthma [11, 33]. Moreover, a dose-response relationship between the severity or frequency of child maltreatment and asthma has been reported in some prior studies [34–36]. In addition, we report that any child maltreatment and the number of types of child maltreatment are associated with asthma in both men and women, with slightly higher effect estimates in women than in men. Although we found an association between certain types of child maltreatment (physical neglect and sexual abuse) in women but not in men, this may be partly due to limited statistical power (e.g., only 117 men with asthma reported physical neglect during childhood).
In contrast to our negative findings for any mediating effects of smoking on the child maltreatment-asthma association, a meta-analysis including 11 studies estimated that any ACE was associated with 1.32 times increased odds of asthma in adulthood, but that the strength of the observed association was markedly decreased after accounting for the mediating effects of smoking [10]. In a separate study of Finnish adults, subjects with multiple ACEs had 1.26 times higher risk of adult-onset asthma than those who reported one or no ACEs, with risk factors such as severe life events and smoking mediating the ACE–asthma association by 29% and 15% [37]. Unlike those prior reports, the current study focused only on child maltreatment and had data on MDD and GAD and a more comprehensive assessment of cigarette smoking (e.g., pack-years).
Child maltreatment increases the risk of depression and stress-related disorders such as anxiety [30, 38], which have in turn been associated with incident asthma in adults [39, 40]. In a multinational study, childhood adversity and early-onset depressive or anxiety disorders were independently associated with adult-onset asthma [36]. To our knowledge, this is the first study to show that lifetime MDD and lifetime GAD are significant mediators of the association between child maltreatment and current asthma in adults, and that such mediation effects are independent of and not explained by cigarette smoking. Child maltreatment often precedes the development of GAD or MDD, and we obtained similar results after excluding subjects whose asthma was diagnosed before age 18 years from the analysis. Thus, our assumptions for the mediation analysis are reasonable and our findings can be confirmed in longitudinal studies with data on the age of onset of GAD and MDD. As new methods become available, such studies could also assess multiple potential mediators of the child maltreatment-asthma association.
Depression and anxiety resulting from child maltreatment may cause or worsen asthma through abnormal neuroendocrine (i.e., dysfunction of the HPA, persistent secretion of cortisol and catecholamines) and autonomic nervous system responses, leading to altered immune responses and airway inflammation [41]. Moreover, recent evidence suggests that chronic stress can alter the expression of genes that predispose to asthma or regulate treatment responses (i.e., those for the glucocorticoid receptor (GR) and the ß2-adrenergic receptor (ADRB2) in youth with asthma) [42, 43]. In addition, adults who experienced child maltreatment are often exposed to other risk factors for asthma, including poverty, an unhealthy diet, and air pollution [15].
Child maltreatment has been linked to long-term changes in immune system programming. In a meta-analysis, adults who reported child maltreatment had increased circulating levels of CRP, interleukin (IL)-6, and tumor necrosis factor (TNF)-α [44]. In another study using latent class analyses of 4,874 adults aged 35–82 years, ACE class was associated with neurodevelopmental and mental disorders, chronic inflammatory diseases, atopy, and increased circulating levels of IL-1β [45]. Moreover, child maltreatment was associated with increased production of reactive oxygen species (ROS), higher level of oxidative stress, increased mitochondrial activity, and increased levels of pro-inflammatory cytokines (IL-1β, IL-6, and TNF-α) in a study of 30 women aged 22 to 44 years [46].
Based on identifiability assumptions for a counterfactual framework [47], our mediation model assumed no confounding of the MDD/GAD-asthma relation by child maltreatment, as well as no unmeasured confounders of the relation between: child maltreatment (exposure) and asthma (outcome), MDD/GAD (mediator) and asthma, or child maltreatment and MDD/GAD (Supplemental Figure 2). We lack data on some potential confounders (e.g., air pollution, living conditions, and parental asthma), and unmeasured confounding is further suggested by our finding of a significant interaction between child maltreatment and MDD or GAD (Uc, shown in Supplemental Figure 2). Thus, our total effect estimate may be biased away from the null. However, we adjusted the mediation analysis for measured potential confounders and found no evidence of direct confounding of the MDD/GAD-asthma relation by child maltreatment. Although all causal models have limitations, our findings warrant further validation.
We acknowledge additional study limitations. First, we cannot exclude selection bias or collider bias, as there were differences in the frequencies of the outcome (current asthma), exposure (child maltreatment), and mediators (GAD and MDD) of interest between those who were and were not eligible for the current analysis [48]. However, selection bias is unlikely as the sole explanation for our results, given prior reports of an association between child maltreatment and asthma in other populations and our finding of a dose-response relationship, as well as similar results in a mediation analysis excluding all current smokers and former smokers with ≥10 pack-years of smoking. Second, a “healthy volunteer” bias has been suggested for the UK Biobank, and thus our findings may not be generalizable to the British population at large [49]. However, the pattern and prevalence of mental health disorders among MHQ respondents in the UK Biobank (n=157,366) are similar to those among participants in the Health Survey for England (HSE, n=3272), a survey designed to monitor trends of the nation’s health [20]. Third, recall bias is expected in a retrospective study and underreporting is common for sensitive information such as child maltreatment [50]. On the other hand, overreporting may occur among participants with depression due to biased recollection of negative memories that tend to skew interpretation of ambiguous personal scenarios in favor of negative experiences [51]. Nevertheless, our results are consistent with those from prior studies in several independent populations. Lastly, potential misclassification or under-reporting of asthma is possible, as current asthma was self-reported. However, misclassification of COPD as asthma is an unlikely explanation for our findings, as we obtained similar results in analyses restricted to never smokers or former smokers with <10 pack-years of smoking.
In summary, our findings suggest that lifetime MDD and lifetime GAD partly explain a link between child maltreatment and current asthma in middle-aged and older British adults in the UK Biobank, independently of cigarette smoking. Taken together with a growing body of literature, our results suggest that clinicians caring for adults with asthma should be aware of potential co-morbidities such as depression and anxiety disorders, particularly in those with a history of child maltreatment.
Supplementary Material
Funding sources:
This study was conducted using the UK Biobank Resource under application number 43252. Dr. Celedón’s contribution was supported by grants HL117191, HL152475, and MD011764 from the U.S. National Institutes of Health. The contributions of Drs. Yueh-Ying Han, Wei Chen, and Qi Yan were supported by NIH grants MD011764 (Y-Y.H), HL150431 (W.C.) and HL138098 (Q.Y).
Conflicts of interest:
Dr. Celedón has received research materials from GSK and Merck (inhaled steroids) and Pharmavite (vitamin D and placebo capsules), to provide medications free of cost to participants in NIH-funded studies, unrelated to this work. The other authors have no conflicts of interest to declare.
REFERENCES
- 1.Global Asthma Network. The Global Asthma Report 2018. Auckland, New Zealand, 2018. [Google Scholar]
- 2.Asthma UK. Asthma facts and statistics. 2020. [cited 2021 July 22]; Available from: https://www.asthma.org.uk/about/media/facts-and-statistics/
- 3.World Helath Organization. Child maltreatment. Geneva, Switzerland, 2020. [Google Scholar]
- 4.Office for National Statistics. Child abuse extent and nature, England and Wales: year ending March 2019. London, England, 2020. [Google Scholar]
- 5.Nelson EC, Heath AC, Madden PA, Cooper ML, Dinwiddie SH, Bucholz KK, Glowinski A, McLaughlin T, Dunne MP, Statham DJ, Martin NG. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes: results from a twin study. Arch Gen Psychiatry 2002: 59(2): 139–145. [DOI] [PubMed] [Google Scholar]
- 6.Anda RF, Brown DW, Felitti VJ, Bremner JD, Dube SR, Giles WH. Adverse childhood experiences and prescribed psychotropic medications in adults. Am J Prev Med 2007: 32(5): 389–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chanlongbutra A, Singh GK, Mueller CD. Adverse Childhood Experiences, Health-Related Quality of Life, and Chronic Disease Risks in Rural Areas of the United States. J Environ Public Health 2018: 2018: 7151297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, Dunne MP. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2017: 2(8): e356–e366. [DOI] [PubMed] [Google Scholar]
- 9.Merrick MT, Ford DC, Ports KA, Guinn AS, Chen J, Klevens J, Metzler M, Jones CM, Simon TR, Daniel VM, Ottley P, Mercy JA. Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention - 25 States, 2015–2017. MMWR Morb Mortal Wkly Rep 2019: 68(44): 999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopes S, Hallak JEC, Machado de Sousa JP, Osorio FL. Adverse childhood experiences and chronic lung diseases in adulthood: a systematic review and meta-analysis. Eur J Psychotraumatol 2020: 11(1): 1720336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhan N, Glymour MM, Kawachi I, Subramanian SV. Childhood adversity and asthma prevalence: evidence from 10 US states (2009–2011). BMJ Open Respir Res 2014: 1(1): e000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Exley D, Norman A, Hyland M. Adverse childhood experience and asthma onset: a systematic review. Eur Respir Rev 2015: 24(136): 299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenberg SL, Miller GE, Brehm JM, Celedon JC. Stress and asthma: novel insights on genetic, epigenetic, and immunologic mechanisms. J Allergy Clin Immunol 2014: 134(5): 1009–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Landeo-Gutierrez J, Forno E, Miller GE, Celedon JC. Exposure to Violence, Psychosocial Stress, and Asthma. Am J Respir Crit Care Med 2020: 201(8): 917–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wisnivesky JP, Markowitz SB, James S, Stone K, Dickens B, Busse P, Crowley L, Federman A, Katz C, Gonzalez A. Comorbid posttraumatic stress disorder and major depressive disorder are associated with asthma morbidity among World Trade Center workers. Ann Allergy Asthma Immunol 2021: 126(3): 278–283. [DOI] [PubMed] [Google Scholar]
- 16.Goodwin RD, Fischer ME, Goldberg J. A twin study of post-traumatic stress disorder symptoms and asthma. Am J Respir Crit Care Med 2007: 176(10): 983–987. [DOI] [PubMed] [Google Scholar]
- 17.Han YY, Forno E, Marsland AL, Miller GE, Celedon JC. Depression, Asthma, and Bronchodilator Response in a Nationwide Study of US Adults. J Allergy Clin Immunol Pract 2016: 4(1): 68–73 e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, Liu B, Matthews P, Ong G, Pell J, Silman A, Young A, Sprosen T, Peakman T, Collins R. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 2015: 12(3): e1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.UK Biobank. Key documents for a large-scale prospective epidemiological resource. [cited 2020 Feb 4]; Available from: http://www.ukbiobank.ac.uk/key-documents/
- 20.Davis KAS, Coleman JRI, Adams M, Allen N, Breen G, Cullen B, Dickens C, Fox E, Graham N, Holliday J, Howard LM, John A, Lee W, McCabe R, McIntosh A, Pearsall R, Smith DJ, Sudlow C, Ward J, Zammit S, Hotopf M. Mental health in UK Biobank - development, implementation and results from an online questionnaire completed by 157 366 participants: a reanalysis. BJPsych Open 2020: 6(2): e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glaesmer H, Schulz A, Hauser W, Freyberger HJ, Brahler E, Grabe HJ. [The childhood trauma screener (CTS) - development and validation of cut-off-scores for classificatory diagnostics]. Psychiatr Prax 2013: 40(4): 220–226. [DOI] [PubMed] [Google Scholar]
- 22.Walker EA, Gelfand A, Katon WJ, Koss MP, Von Korff M, Bernstein D, Russo J. Adult health status of women with histories of childhood abuse and neglect. Am J Med 1999: 107(4): 332–339. [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU. The World Health Organization composite international diagnostic interview short-form (CIDI-SF). Int J Methods Psychiatr Res 1998: 7: 171–185. [Google Scholar]
- 24.Office for National Statistics. Average household income, UK: financial year ending 2019. London, England, 2020. [Google Scholar]
- 25.Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley & Sons, New York, U.S., 1987. [Google Scholar]
- 26.VanderWeele TJ. Mediation Analysis: A Practitioner’s Guide. Annu Rev Public Health 2016: 37: 17–32. [DOI] [PubMed] [Google Scholar]
- 27.Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods 2013: 18(2): 137–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Valente MJ, Rijnhart JJM, Smyth HL, Muniz FB, MacKinnon DP. Causal Mediation Programs in R, Mplus, SAS, SPSS, and Stata. Struct Equ Modeling 2020: 27(6): 975–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.VanderWeele TJ. A unification of mediation and interaction: a 4-way decomposition. Epidemiology 2014: 25(5): 749–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gallo EAG, Munhoz TN, Loret de Mola C, Murray J. Gender differences in the effects of childhood maltreatment on adult depression and anxiety: A systematic review and meta-analysis. Child Abuse Negl 2018: 79: 107–114. [DOI] [PubMed] [Google Scholar]
- 31.Thompson MP, Kingree JB, Desai S. Gender differences in long-term health consequences of physical abuse of children: data from a nationally representative survey. Am J Public Health 2004: 94(4): 599–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cammack AL, Haardorfer R, Suglia SF. Associations between child maltreatment, cigarette smoking, and nicotine dependence in young adults with a history of regular smoking. Ann Epidemiol 2019: 40: 13–20 e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ospina MB, Serrano-Lomelin JA, Amjad S, Hicks A, Giesbrecht GF. Latent factors of adverse childhood experiences and adult-onset asthma. J Dev Orig Health Dis 2021: 12(1): 50–57. [DOI] [PubMed] [Google Scholar]
- 34.Coogan PF, Wise LA, O’Connor GT, Brown TA, Palmer JR, Rosenberg L. Abuse during childhood and adolescence and risk of adult-onset asthma in African American women. J Allergy Clin Immunol 2013: 131(4): 1058–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Banerjee D, Gelaye B, Zhong QY, Sanchez SE, Williams MA. Childhood abuse and adult-onset asthma among Peruvian women. J Asthma 2018: 55(4): 430–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scott KM, Von Korff M, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, Haro JM, Kessler RC, Kovess V, Ono Y, Ormel J, Posada-Villa J. Childhood adversity, early-onset depressive/anxiety disorders, and adult-onset asthma. Psychosom Med 2008: 70(9): 1035–1043. [DOI] [PubMed] [Google Scholar]
- 37.Lietzen R, Suominen S, Sillanmaki L, Virtanen P, Virtanen M, Vahtera J. Multiple adverse childhood experiences and asthma onset in adulthood: Role of adulthood risk factors as mediators. J Psychosom Res 2021: 143: 110388. [DOI] [PubMed] [Google Scholar]
- 38.Gardner MJ, Thomas HJ, Erskine HE. The association between five forms of child maltreatment and depressive and anxiety disorders: A systematic review and meta-analysis. Child Abuse Negl 2019: 96: 104082. [DOI] [PubMed] [Google Scholar]
- 39.de la Hoz RE, Jeon Y, Miller GE, Wisnivesky JP, Celedon JC. Post-traumatic Stress Disorder, Bronchodilator Response, and Incident Asthma in World Trade Center Rescue and Recovery Workers. Am J Respir Crit Care Med 2016: 194(11): 1383–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brunner WM, Schreiner PJ, Sood A, Jacobs DR Jr., Depression and risk of incident asthma in adults. The CARDIA study. Am J Respir Crit Care Med 2014: 189(9): 1044–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tiwari A, Gonzalez A. Biological alterations affecting risk of adult psychopathology following childhood trauma: A review of sex differences. Clin Psychol Rev 2018: 66: 69–79. [DOI] [PubMed] [Google Scholar]
- 42.Miller GE, Chen E. Life stress and diminished expression of genes encoding glucocorticoid receptor and beta2-adrenergic receptor in children with asthma. Proc Natl Acad Sci U S A 2006: 103(14): 5496–5501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brehm JM, Ramratnam SK, Tse SM, Croteau-Chonka DC, Pino-Yanes M, Rosas-Salazar C, Litonjua AA, Raby BA, Boutaoui N, Han YY, Chen W, Forno E, Marsland AL, Nugent NR, Eng C, Colon-Semidey A, Alvarez M, Acosta-Perez E, Spear ML, Martinez FD, Avila L, Weiss ST, Soto-Quiros M, Ober C, Nicolae DL, Barnes KC, Lemanske RF Jr., Strunk RC, Liu A, London SJ, Gilliland F, Sleiman P, March M, Hakonarson H, Duan QL, Kolls JK, Fritz GK, Hu D, Fani N, Stevens JS, Almli LM, Burchard EG, Shin J, McQuaid EL, Ressler K, Canino G, Celedon JC. Stress and Bronchodilator Response in Children with Asthma. Am J Respir Crit Care Med 2015: 192(1): 47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-alpha. Mol Psychiatry 2016: 21(5): 642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ajdacic-Gross V, Mutsch M, Rodgers S, Tesic A, Muller M, Seifritz E, Wagner EN, von Kanel R, Landolt MA, Steinemann N, von Wyl V, Castelao E, Strippoli MF, Glaus J, Vandeleur C, Marques-Vidal PM, Vollenweider P, Preisig M. A step beyond the hygiene hypothesis-immune-mediated classes determined in a population-based study. BMC Med 2019: 17(1): 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boeck C, Koenig AM, Schury K, Geiger ML, Karabatsiakis A, Wilker S, Waller C, Gundel H, Fegert JM, Calzia E, Kolassa IT. Inflammation in adult women with a history of child maltreatment: The involvement of mitochondrial alterations and oxidative stress. Mitochondrion 2016: 30: 197–207. [DOI] [PubMed] [Google Scholar]
- 47.Naimi AI, Kaufman JS, MacLehose RF. Mediation misgivings: ambiguous clinical and public health interpretations of natural direct and indirect effects. Int J Epidemiol 2014: 43(5): 1656–1661. [DOI] [PubMed] [Google Scholar]
- 48.Munafo MR, Tilling K, Taylor AE, Evans DM, Davey Smith G. Collider scope: when selection bias can substantially influence observed associations. Int J Epidemiol 2018: 47(1): 226–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, Collins R, Allen NE. Comparison of Sociodemographic and Health-Related Characteristics of UK Biobank Participants With Those of the General Population. Am J Epidemiol 2017: 186(9): 1026–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scott KM, Smith DA, Ellis PM. A population study of childhood maltreatment and asthma diagnosis: differential associations between child protection database versus retrospective self-reported data. Psychosom Med 2012: 74(8): 817–823. [DOI] [PubMed] [Google Scholar]
- 51.Dalgleish T, Werner-Seidler A. Disruptions in autobiographical memory processing in depression and the emergence of memory therapeutics. Trends Cogn Sci 2014: 18(11): 596–604. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


