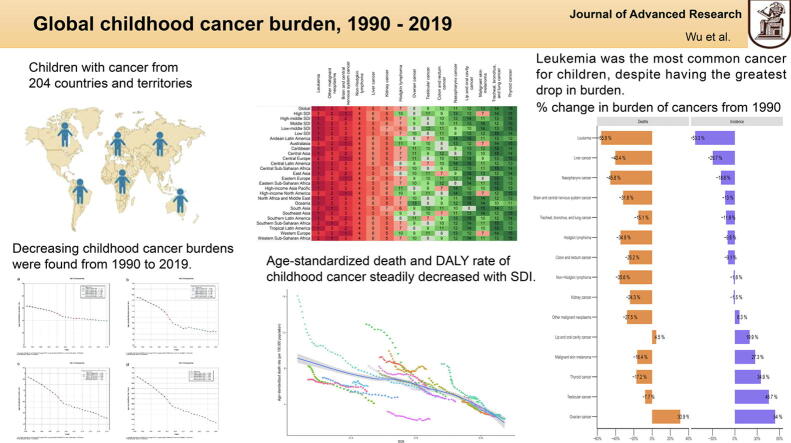
Graphical abstract
Abbreviations: DALYs, disability-adjusted life years; SDI, sociodemographic index; LMICs, low- and middle-income countries; HICs, high-income countries; GBD, Global Burden of Disease; ASRs, age-standardized rates; UIs, uncertainty intervals; APCs, Annual percentage changes; CIs, confidence intervals; ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASDR, age-standardized death rate; brain and CNS, cancer brain and central nervous system cancer; ALL, acute lymphoid leukemia; NHL, non-Hodgkin lymphoma
Keywords: Childhood, Cancer, Burden, Epidemiology, Global burden of disease study
Highlights
-
•
We provided a comprehensive and the latest evaluation of the global childhood cancer burden.
-
•
The childhood cancer burden has been decreasing globally over the last 30 years.
-
•
Age-standardized incidence and prevalence rates of childhood cancer were more notable in higher SDI quintiles.
-
•
Age-standardized death and disability-adjusted life year rates of childhood cancer decreased with SDI.
-
•
Leukemia was still the most common cancer and the leading cause of death among children.
Abstract
Introduction
Cancer is the leading cause of death among children.
Objectives
We report on the latest estimates of the burden of cancer among children at the global, regional, and national levels from 1990 to 2019.
Methods
Based on the Global Burden of Disease Study 2019, children’s cancer data were analyzed by sex, age, year, and location. Age-standardized rates were used to compare the burdens among regions and nations. Joinpoint analysis was applied to assess the temporal trend of the global childhood cancer burden.
Results
In 2019, 291,319 (95% uncertainty interval [UI], 254,239 to 331,993) new cases and 98,834 (86,124 to 113,581) deaths from childhood cancer were documented globally. Further, 8,302,464 (7,230,447 to 9,555,118) DALYs and 1,806,630 (1,567,808 to 2,089,668) prevalent cases were recorded in the same year. Age-standardized incidence and prevalence rates of childhood cancer were greatest in higher SDI settings and increased most significantly in Australasia and Southern Latin America over the last 30 years. However, although age-standardized death and DALY rates of childhood cancer have remarkably decreased in all regions since 1990, countries with a lower SDI showed the highest rates in 2019, particularly in countries in Eastern Sub-Saharan Africa. Among all cancers, leukemia has shown the largest decrease in burden since 1990. Despite this, leukemia was still the most common cancer and the leading cause of death among children in 2019, followed by brain and central nervous system cancer.
Conclusions
On a global scale, the childhood cancer burden has significantly fallen over the last 30 years, but is still higher in lower SDI countries. Effective interventions and collaborations among nations should be facilitated to improve healthcare among children with cancer in countries with lower SDI.
Introduction
Cancer is one of the main causes of death among children, especially in developed countries [1]. Revolutionary advances in cancer diagnosis and treatment have dramatically improved the 5-year survival rate of children with cancer, which has reached approximately 80% in high-income countries (HICs) [2]. In contrast, the 5-year survival rate was just up to 40% in low- and middle-income countries (LMICs), in which over 80% of children with cancer resided [3], [4]. Compared with HICs, LMICs have difficulties in accessing supportive care and insurance coverage and establishing a national cancer control system, thus resulting in a lower survival rate and higher burden of childhood cancer [5], [6].
Despite obtaining better medical care, childhood cancer survivors are still at risk of recurrence and subsequent primary cancers, some chronic disorders, and functional impairments [7]. Meanwhile, childhood cancer survivors with subsequent primary cancers might experience inferior prognosis than those without prior cancers in childhood [8]. Further, as a result of undergoing cancer therapy, patients would face more difficulties, such as increased financial stress due to out-of-pocket medical costs, fewer work opportunities due to physical limitations, and psychological depression and anxiety, all of which lead to decreased quality of life and societal burden [9], [10], [11].
Thus, it is urgent to identify specific childhood cancer burdens and provide more information for local governments to ease this burden. The GBD study 2019 reported the disease burden with 4 indicators, and covered 7333 registries from 204 countries and territories, whereas other studies, including the CONCORD, GLOBOCAN, and International Incidence of Childhood Cancer, reported childhood cancer burden with 1 or 2 indicators and covered lower numbers of registries [12], [13], [14], [15]. Thus, based on the latest data and improved methodology from GBD 2019, we analyzed the global, regional, and national cancer burden among children and their trends from 1990 to 2019.
Methods
Overview
The global burden of childhood cancer (children aged 0−14 years) was obtained from the GBD 2019, which provides an up-to-date and comprehensive analysis of 328 diseases and their 87 risk factors among 204 countries and territories. All countries and territories were classified into 21 regions according to epidemiological similarities and geographical proximity, and grouped into five categories based on the sociodemographic index (SDI; low SDI, low-middle SDI, middle SDI, high-middle SDI, and high SDI). The SDI was a composite indicator that was estimated based on lag-distributed income per capita, the total fertility rate of females aged under 25, and average years of schooling among adults aged 15 and older.
Classification and estimation of childhood cancer burden
Detailed information on burden estimation was described in a previous study [15]. GBD 2019 classified all neoplasms into 30 groups according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD−10] codes C00-D49. In this study, a total of 15 groups of malignant neoplasms were included among children, 14 categorized malignant neoplasms groups, and 1 uncategorized group (other malignant neoplasms). More information on burden estimation is provided in the Supplement.
Statistical analyses
Children aged under 15 were included in our analysis, and childhood cancer burden was analyzed by age, sex, year, and location. In GBD studies, the uncertainty for all estimates were calculated to account for the uncertainty due to primary data sources, modelling uncertainty, data error, and data manipulation [16]. Thus, the uncertainty was quantified and captured statistically in the 95% uncertainty intervals (UIs) for each location and for each estimate. The UIs were calculated from 1000 draw-levels from the posterior distribution of models, and 95% UIs were defined as the 2.5th and 97.5th values of the distribution. Incidence, prevalence, death, disability-adjusted life-years (DALYs), and their corresponding age-standardized rates (ASRs) were reported with 95% uncertainty intervals (UIs) to eliminate the effects caused by differences in population structures. Temporal trends of childhood cancer burdens were estimated using the Joinpoint Regression Model, a set of statistically linear models, which was described in our previous study [17]. The annual percentage changes (APCs) and their 95% confidence intervals (CIs) were also calculated. All analyses were performed using R software (R Core Team, version 3.5.2, Vienna, Austria) and Joinpoint software (version 4.7.0) from the Surveillance Research Program of the US National Cancer Institute. The p-value was estimated at a significance level of 0.05.
Ethics Statement
For GBD studies, a waiver of informed consent was reviewed and approved by the Institutional Review Board of the University of Washington. All the information about ethical standards is available through the official website (http://www.healthdata.org/gbd/2019).
Results
Global childhood cancer burden
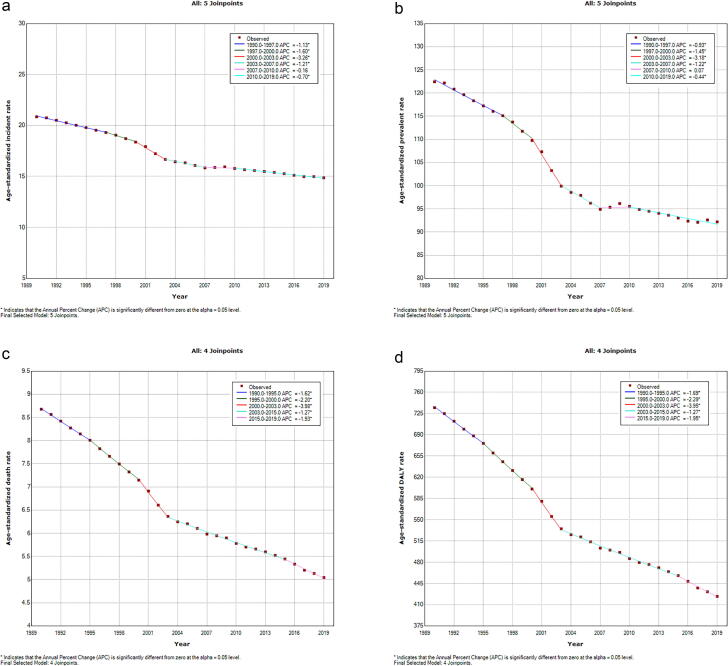
In 2019, 291,319 (95% UI, 254,239 to 331,993) new cases and 98,834 (86,124 to 113,581) deaths of childhood cancer were documented, with 1,806,630 (1,567,808 to 2,089,668) prevalent cases. There were 8,302,464 (7,230,447 to 9,555,118) DALYs recorded in the same year (Table 1). In the context of sex, the incidence and prevalence of childhood cancer were more considerable among boys than girls, so as the deaths and DALYs (Table 1). Further, among all age groups, children aged 1−4 years had the highest childhood cancer incidence, prevalence, death, and DALYs, whereas children under 1 year always had the lowest figures of all these estimates (Supplementary Fig. 1). Over the past 30 years, the global childhood cancer age-standardized incidence, prevalence, death, and DALY rates have markedly decreased. More specifically, as shown in Fig. 1, the global age-standardized incidence rate (ASIR) and age-standardized prevalence rate (ASPR) have significantly decreased since 1990, and the most notable declines were observed between 2000 and 2003 (ASIR: APC = − 3.3% [95% CI, − 4.1% to − 2.4%], p < 0.05; ASPR: APC = − 3.2% [− 4.2% to − 2.1%], p < 0.05). However, ASPR remained stable between 2007 and 2010 and then has been consistently declining in recent 10 years. Similarly, age-standardized death and DALY rates of childhood cancer considerably decreased with different APCs, which were also most remarkable between 2000 and 2003 (age-standardized death rate [ASDR]: APC = − 4.0% [− 4.9% to − 3.1%], p < 0.05; age-standardized DALY rate: APC = − 3.9% [− 4.8% to − 3.1%], p < 0.05) (Fig. 1).
Table 1.
Global burden of childhood cancer in 2019 and its annualized change in rates from 1990 to 2019.
| Location | Sex |
Incidence (95%UI) |
Prevalence (95%UI) |
Death (95%UI) |
DALYs (95%UI) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Count | ASIR(per 100,000) | Percentage change in ASIR (%) | Count | ASPR(per 100,000) | Percentage change in ASPR (%) | Count | ASDR(per 100,000) | Percentage change in ASDR (%) | Count | Age-standardized DALY rate(per 100,000) | Percentage change in age-standardized DALY rate (%) | ||
| Global | Both | 291318.88(254238.5 to 331993) | 14.87(12.97 to 16.94) | −28.71(−42.91 to −8.25) | 1806630.42(1567808.33 to 2089668.43) | 92.19(80 to 106.63) | −24.69(−40.52 to −0.18) | 98834.13(86123.63 to 113581.36) | 5.04(4.39 to 5.8) | −41.87(−53.77 to −24.72) | 8302463.84(7230446.89 to 9555118.13) | 423.65(368.95 to 487.57) | −42.34(−54.19 to −25.09) |
| Girl | 133783.48(119203.29 to 149481.67) | 14.11(12.57 to 15.77) | −32.97(−48.09 to −10.28) | 855546.41(758237.2 to 960210.16) | 90.24(79.98 to 101.28) | −30.58(−48.2 to −3.14) | 41414.56(36280.14 to 47089.45) | 4.37(3.83 to 4.97) | −44.34(−55.31 to −26.44) | 3479082.28(3060185.84 to 3959213) | 366.97(322.79 to 417.62) | −44.92(−55.88 to −26.62) | |
| Boy | 157535.4(131489.52 to 186765.36) | 15.57(13 to 18.46) | −24.62(−44.37 to 4.17) | 951084.01(777366.54 to 1145045.38) | 94.01(76.84 to 113.18) | −18.4(−42.75 to 14.23) | 57419.57(48951.63 to 67057.23) | 5.68(4.84 to 6.63) | −40.01(−54.5 to −14.32) | 4823381.57(4113806.41 to 5643512.65) | 476.77(406.63 to 557.83) | −40.38(−54.93 to −14.36) | |
| High SDI | Both | 33560.59(26064.04 to 42749.22) | 20.56(15.96 to 26.18) | −4.32(−17.27 to 12.1) | 264683.48(199315.47 to 345915.41) | 162.12(122.08 to 211.88) | 4.01(−10.23 to 22.17) | 4268.9(3769.36 to 4571.95) | 2.61(2.31 to 2.8) | −41.43(−50.1 to −36.97) | 366509.69(322212.67 to 396657.58) | 224.49(197.36 to 242.96) | −40.46(−49.3 to −35.37) |
| Girl | 14963.53(13270.83 to 16801.5) | 18.83(16.7 to 21.14) | −4.72(−15.57 to 7.14) | 115712.3(101670.96 to 130286.56) | 145.6(127.94 to 163.94) | 2.7(−9.28 to 15.71) | 1939.05(1705.5 to 2063.96) | 2.44(2.15 to 2.6) | −40.31(−48.8 to −35.52) | 166201.41(146695.49 to 178359.14) | 209.14(184.59 to 224.44) | −39.48(−48.07 to −34.43) | |
| Boy | 18597.06(12342.59 to 26413.9) | 22.19(14.73 to 31.52) | −4.01(−21.18 to 18.5) | 148971.18(93268.88 to 219261.25) | 177.79(111.31 to 261.67) | 5.04(−14.06 to 30.36) | 2329.85(2005.73 to 2537.34) | 2.78(2.39 to 3.03) | −42.33(−52.51 to −36.72) | 200308.28(172049.1 to 221739.17) | 239.05(205.33 to 264.63) | −41.25(−51.85 to −35.03) | |
| High-middle SDI | Both | 52642.87(45308.76 to 60903.04) | 21.47(18.48 to 24.84) | −17(−30.93 to 1.46) | 383142.34(323869.56 to 448548.84) | 156.25(132.07 to 182.92) | −3.4(−21.31 to 22.18) | 10407.11(9192.9 to 11528.09) | 4.24(3.75 to 4.7) | −51.9(−59.31 to −42.62) | 881335.02(777006.47 to 981911.43) | 359.41(316.86 to 400.42) | −51.73(−59.35 to −42.17) |
| Girl | 23376.84(20936.11 to 25908.88) | 19.95(17.87 to 22.11) | −22.22(−37.52 to −1.16) | 169955.72(151549.08 to 189498.79) | 145.05(129.34 to 161.73) | −12.16(−31.36 to 16.11) | 4529.63(4091.52 to 4942.41) | 3.87(3.49 to 4.22) | −53.21(−60.42 to −44.83) | 384191.88(345882.55 to 420191.81) | 327.88(295.19 to 358.61) | −53.16(−60.55 to −44.4) | |
| Boy | 29266.03(23080.35 to 35901.16) | 22.86(18.03 to 28.04) | −12.31(−32.09 to 11.61) | 213186.62(163078.01 to 269509.74) | 166.49(127.36 to 210.48) | 5(−21.01 to 35.86) | 5877.48(5029.51 to 6738.31) | 4.59(3.93 to 5.26) | −50.92(−60.53 to −35.06) | 497143.14(425528.38 to 572368.14) | 388.26(332.33 to 447) | −50.65(−60.47 to −34.37) | |
| Middle SDI | Both | 87649.12(78035.26 to 97771.18) | 15.83(14.1 to 17.66) | −32.16(−46.66 to −10.39) | 581582.43(516279.07 to 648458.76) | 105.05(93.26 to 117.14) | −25.25(−42.78 to 8.31) | 25576.09(22703.19 to 28637.01) | 4.62(4.1 to 5.17) | −49.77(−59.71 to −36.62) | 2138536.96(1890422.82 to 2391649.43) | 386.3(341.48 to 432.02) | −50.3(−60.18 to −37.04) |
| Girl | 41501.6(37174.81 to 45794.87) | 15.67(14.04 to 17.29) | −35.05(−49.91 to −10.14) | 281070.61(250987.74 to 311108.85) | 106.14(94.78 to 117.49) | −30.69(−49.22 to 4.2) | 10880.91(9752.2 to 12100.68) | 4.11(3.68 to 4.57) | −52.43(−61.66 to −38.83) | 910980.37(815693.39 to 1013099.84) | 344.03(308.04 to 382.59) | −53.01(−62.12 to −39.29) | |
| Boy | 46147.51(38871.09 to 53755.23) | 15.98(13.46 to 18.61) | −29.25(−50.63 to 4.09) | 300511.82(254860 to 348366.19) | 104.06(88.25 to 120.63) | −19.09(−46.36 to 23.43) | 14695.18(12540.47 to 16974.57) | 5.09(4.34 to 5.88) | −47.69(−60.94 to −22.7) | 1227556.58(1043762.21 to 1417674.66) | 425.06(361.41 to 490.89) | −48.15(−61.42 to −22.71) | |
| Low-middle SDI | Both | 60620.83(50733.8 to 71943.63) | 11.58(9.69 to 13.74) | −28.84(−47.68 to 3.49) | 311943.32(257745.9 to 379633.47) | 59.58(49.23 to 72.51) | −28.82(−49.91 to 10.42) | 27085.13(22743.71 to 31786.68) | 5.17(4.34 to 6.07) | −37.92(−54.26 to −10.5) | 2252684.75(1885779.32 to 2647086.72) | 430.27(360.19 to 505.6) | −38.9(−55.15 to −11.44) |
| Girl | 27984.01(23200.34 to 33334.32) | 11.02(9.14 to 13.13) | −33.92(−53.87 to 3.58) | 153004.63(124948.7 to 188047.61) | 60.27(49.22 to 74.07) | −35.27(−58.27 to 7.45) | 11587.62(9685.83 to 13698.49) | 4.56(3.82 to 5.4) | −40.22(−55.79 to −11.39) | 963586.27(805719.88 to 1137875.12) | 379.56(317.38 to 448.21) | −41.3(−56.7 to −11.96) | |
| Boy | 32636.82(27064.22 to 39327.37) | 12.1(10.04 to 14.58) | −23.82(−48.34 to 22.03) | 158938.68(131014.53 to 196238.71) | 58.94(48.58 to 72.77) | −21.25(−50.54 to 30.54) | 15497.51(12925.88 to 18606.87) | 5.75(4.79 to 6.9) | −36.1(−55.37 to 2.23) | 1289098.49(1075386.44 to 1548880.45) | 478.01(398.77 to 574.34) | −36.99(−56.15 to 1.59) | |
| Low SDI | Both | 55206.62(42558.48 to 69364.14) | 11.67(9 to 14.67) | −30.16(−52.72 to 23.37) | 264093.45(198772.43 to 338392.1) | 55.85(42.03 to 71.56) | −28.56(−53.44 to 34.81) | 31418.5(24504.59 to 39158.48) | 6.64(5.18 to 8.28) | −38.98(−56.97 to −2.5) | 2656809.83(2063544.7 to 3316793.6) | 561.84(436.38 to 701.41) | −39.75(−57.7 to −3.25) |
| Girl | 25858.09(20389.06 to 32647.97) | 11.14(8.78 to 14.06) | −34.63(−58.22 to 26.87) | 135186.47(98074.5 to 179948.59) | 58.24(42.25 to 77.52) | −36.26(−61.94 to 35.52) | 12442.52(10004.43 to 15207.99) | 5.36(4.31 to 6.55) | −37.06(−55.78 to 15.26) | 1051193.35(843254.38 to 1289042.96) | 452.83(363.25 to 555.29) | −38.06(−56.68 to 14.22) | |
| Boy | 29348.53(22105.42 to 37794.03) | 12.19(9.18 to 15.7) | −25.68(−51.59 to 32.57) | 128906.98(96276.07 to 168376.6) | 53.55(39.99 to 69.94) | −18.23(−50.95 to 51.45) | 18975.97(14228.41 to 24386.86) | 7.88(5.91 to 10.13) | −40.14(−59.22 to 1.27) | 1605616.48(1198931.19 to 2071134.28) | 666.96(498.03 to 860.33) | −40.78(−59.7 to 0.48) | |
Abbreviations: UI uncertainty interval; ASIR age-standardized incidence rate; ASDR age-standardized death rate; ASPR age-standardized prevalence rate; DALYs disability-adjusted life-years.
Fig. 1.
Global trends for age-standardized rates (per 100,000 population) of childhood cancer from 1990 to 2019. (a) age-standardized incidence rate; (b) age-standardized prevalence rate; (c) age-standardized death rate; (d) age-standardized DALY rate. Abbreviations: DALY disability-adjusted life-year.
Regional and national childhood cancer burden
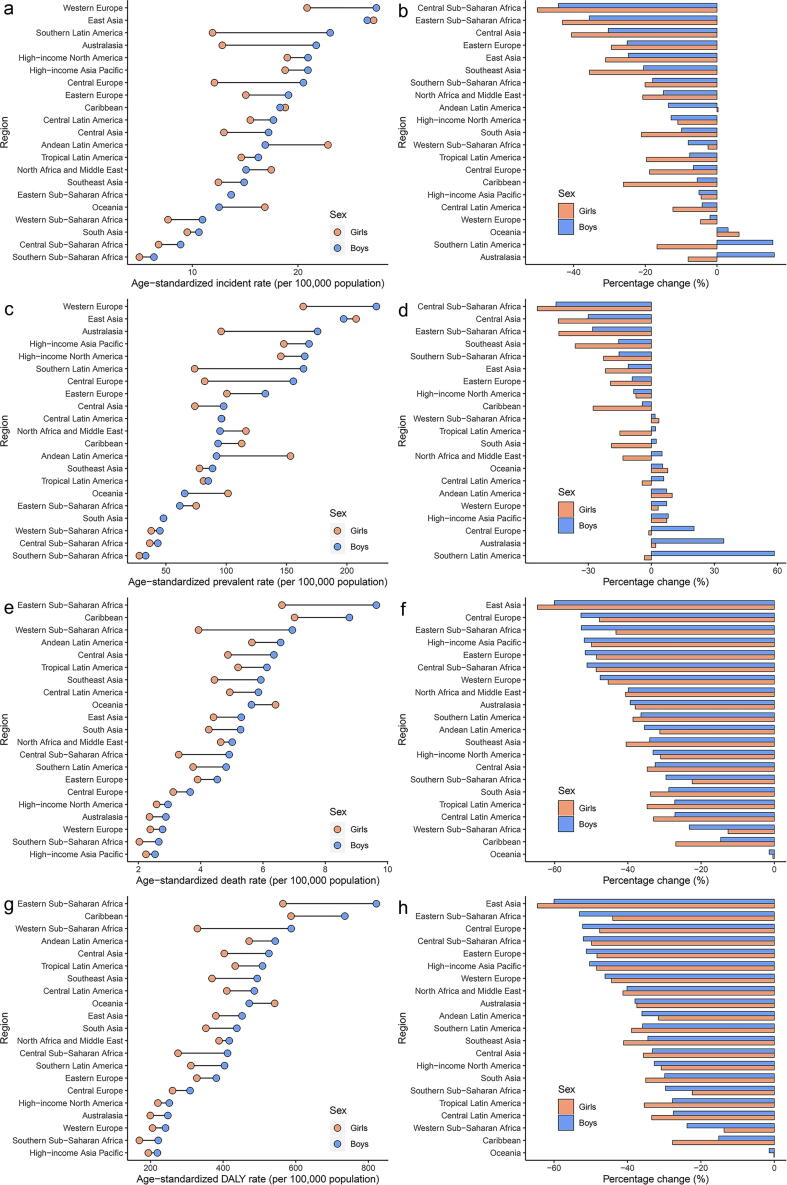
Regionally, in 2019, the highest ASIR and ASPR of childhood cancer were in East Asia, followed by Western Europe, and age-standardized death and DALY rates were highest in Eastern Sub-Saharan Africa, followed by the Caribbean (Fig. 2 and Supplementary Table 1). However, Southern Sub-Saharan Africa showed the lowest age-standardized incidence, prevalence, death, and DALY rates in 2019. Since 1990, the ASIR and ASPR of childhood cancer had been decreasing in most regions, with the greatest decrease being observed in Central Sub-Saharan Africa. However, the greatest increases were observed in Australasia for ASIR and Southern Latin America for ASPR (Fig. 2 and Supplementary Table 1). Regarding age-standardized death and DALY rates, all regions have shown a downward trend over the past 30 years, with the greatest decline being observed in East Asia (Fig. 2 and Supplementary Table 1).
Fig. 2.
Regional age-standardized rates (per 100,000 population) of childhood cancer in 2019 and their percentage changes in rates for different sexes from 1990 to 2019. (a) age-standardized incidence rate in 2019; (b) percentage change in age-standardized incidence rate, 1990−2019; (c) age-standardized prevalence rate in 2019; (d) percentage change in age-standardized prevalence rate, 1990−2019; (e) age-standardized death rate in 2019; (f) percentage change in age-standardized death rate, 1990−2019; (g) age-standardized DALY rate in 2019; (h) percentage change in age-standardized DALY rate, 1990−2019. Abbreviations: DALY disability-adjusted life-year.
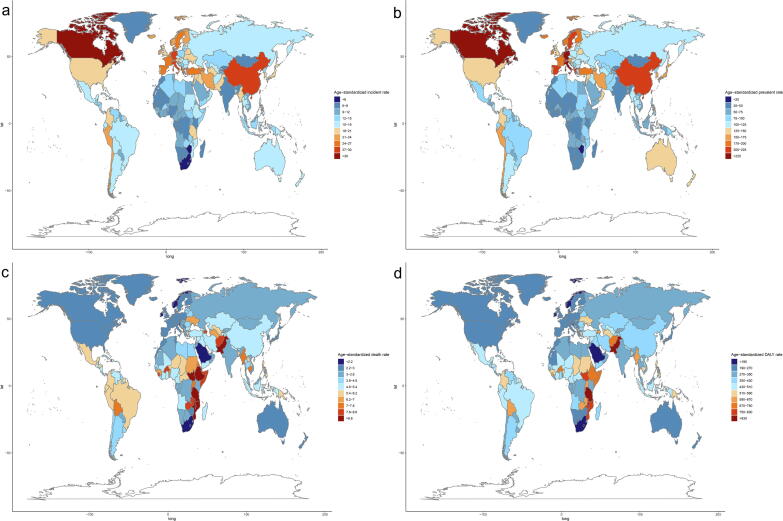
At the national level, in 2019, the highest ASIR and ASPR of childhood cancer were sequentially shown in San Marino, Monaco, Albania, and Canada, whereas Haiti, Malawi, and Tanzania were 3 countries with the highest reported age-standardized death and DALY rates (Fig. 3). Over the past 30 years, over 100 countries have shown decreasing trends in ASIR and ASPR of childhood cancer, and over 180 countries have experienced falling age-standardized death and DALY rates. North Korea showed the highest decrease in ASIR and ASPR, whereas Serbia had the greatest decrease in age-standardized death and DALY rates. Meanwhile, Botswana had the greatest increase in age-standardized incidence, prevalence, death, and DALY rates of childhood cancer among all nations (Supplementary Table 2).
Fig. 3.
National age-standardized rates (per 100,000 population) of childhood cancer for both sexes combined in 2019. (a) age-standardized incidence rate; (b) age-standardized prevalence rate; (c) age-standardized death rate; (d) age-standardized DALY rate. Abbreviations: DALY disability-adjusted life-year. Note: The original data was obtained from the GBD studies. There might be problems in regional division, which however was not the key point for this study.
Childhood cancer burden and SDI
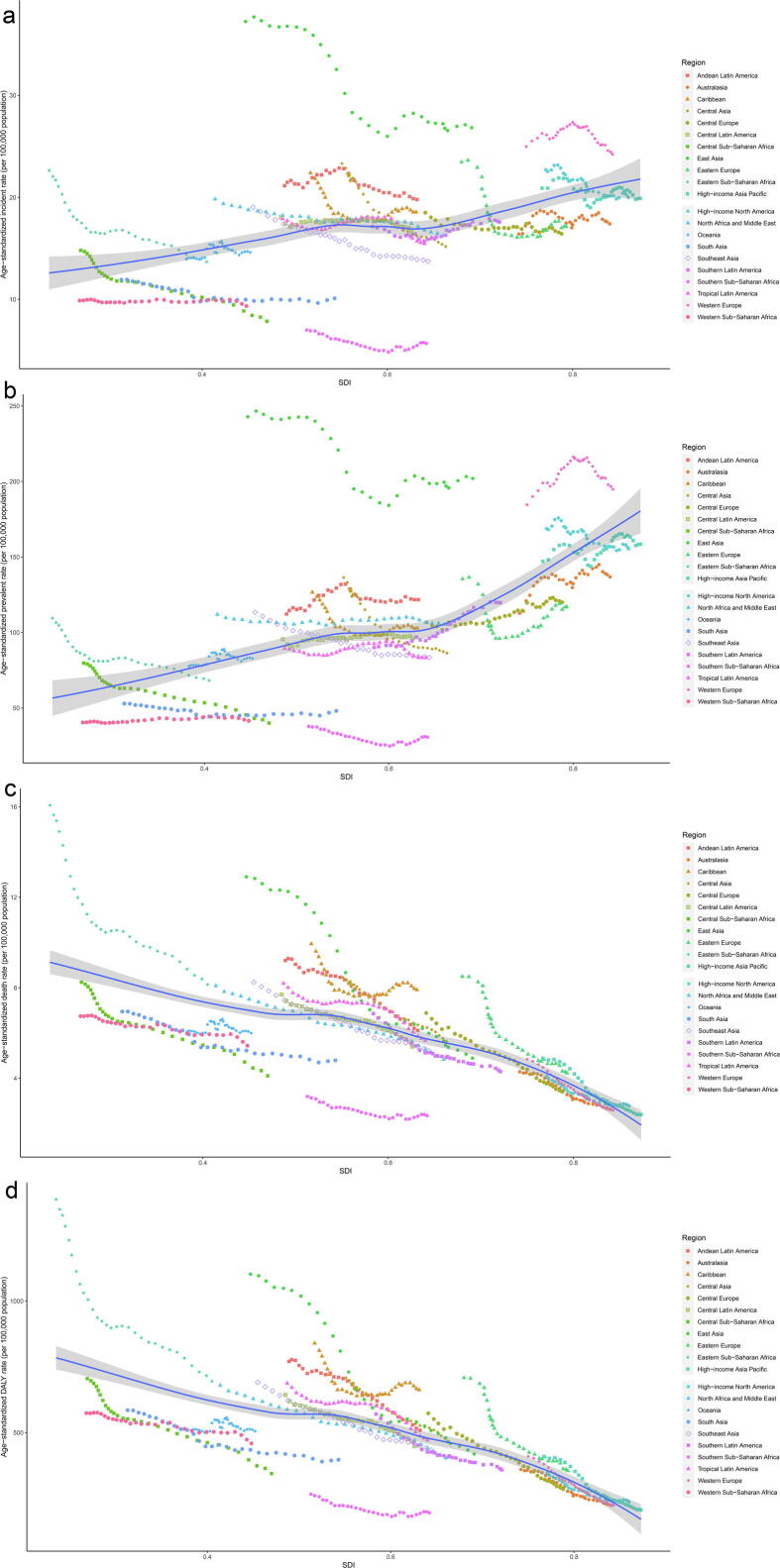
Childhood cancer burden differed substantially based on SDI. As shown in Fig. 4, ASIR and ASPR of childhood cancer were more notable in higher SDI quintiles. ASIR and ASPR of childhood cancer increased with SDI in the expected pattern, but the regional patterns presented great variations. Some regions showed decreasing ASIR and ASPR according to SDI, whereas others showed increasing rates or did not have monotonic associations with SDI. In contrast, the expected pattern and regional patterns showed similar trends in the associations between the SDI and age-standardized death and DALY rates. Age-standardized death and DALY rates markedly decreased according to SDI, with areas with higher SDI showing lower age-standardized death and DALY rates (Fig. 4). Since 1990, age-standardized incidence, death, and DALY rates have decreased in all SDI quintiles (Supplementary Fig. 2). High-middle SDI countries showed the largest decrease in age-standardized death and DALY rates, but low SDI countries showed the lowest declines. However, countries with high SDI showed the lowest decrease in ASIR and even had an increasing ASPR (Table 1 and Supplementary Fig. 2).
Fig. 4.
Trends for age-standardized rates (per 100,000 population) of childhood cancer among 21 regions by SDI for both sexes combined from 1990 to 2019. (a) age-standardized incidence rate; (b) age-standardized prevalence rate; (c) age-standardized death rate; (d) age-standardized DALY rate. Abbreviations: SDI sociodemographic index; DALY disability-adjusted life-year.
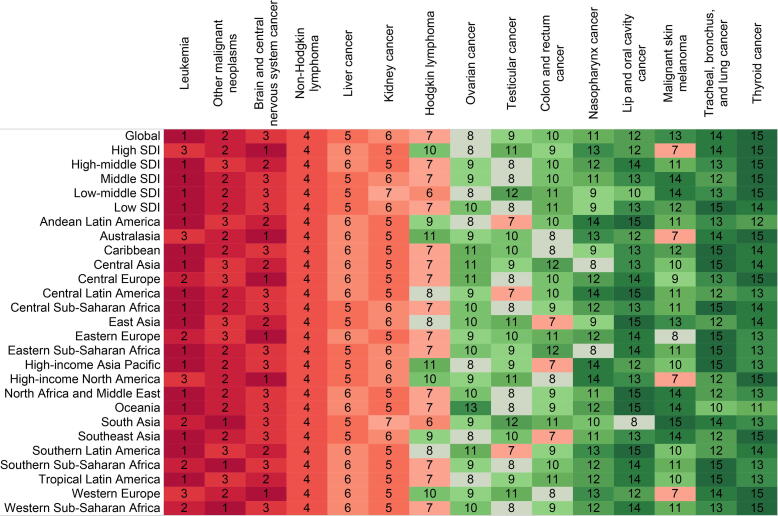
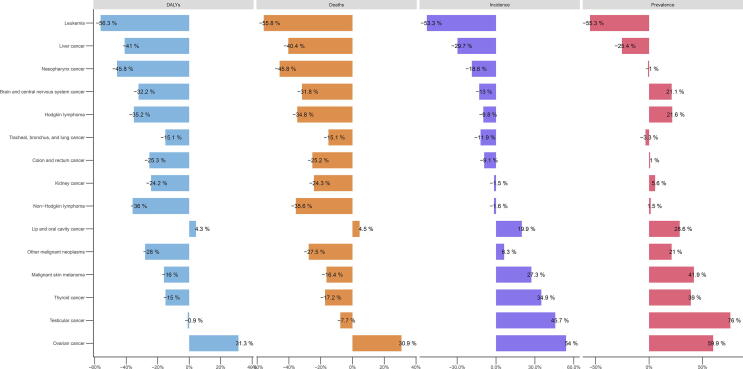
Different cancers burdens among children
In 2019, leukemia was the most common cancer and the most common cause of death and DALYs among children with cancers of both sexes and all ages worldwide. Other three common causes of death among children with cancers included other malignant neoplasms (uncategorized malignant neoplasms), brain and central nervous system (CNS) cancer, and non-Hodgkin lymphoma (NHL) (Table 2). The global, regional, and national ranks of different cancers among children in 2019 are described in Fig. 5 and Supplementary Figs. 3–9. In the last 30 years, leukemia has had the greatest drop in age-standardized incidence, prevalence, death, and DALY rates, whereas ovarian cancer has had the most significant increase in age-standardized incidence, death, and DALY rates (Fig. 6).
Table 2.
Global burden of different childhood cancers in 2019.
| Cancers | Subtypes | Sex |
Incidence (95% UI) |
Prevalence (95% UI) |
Death (95% UI) |
DALY (95% UI) |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| Count | ASIR (per 100,000) | Count | ASPR (per 100,000) | Count | ASDR (per 100,000) | Count | Age-standardized DALY rate (per 100,000) | |||
| Brain and central nervous system cancer | Both | 39932.68(30818.28 to 46720.18) | 2.04(1.57 to 2.38) | 174645.96(135736.86 to 204587.1) | 8.91(6.93 to 10.44) | 19988.32(15399.65 to 23488.92) | 1.02(0.79 to 1.2) | 1666431.54(1287203.73 to 1964915.34) | 85.03(65.68 to 100.26) | |
| Girl | 17675.71(13158.43 to 20776.42) | 1.86(1.39 to 2.19) | 84974.9(62195.09 to 101247.94) | 8.96(6.56 to 10.68) | 8217.52(6304.88 to 9642.08) | 0.87(0.67 to 1.02) | 683871.2(523085.39 to 803542.23) | 72.13(55.17 to 84.76) | ||
| Boy | 22256.97(15992.54 to 27307.38) | 2.2(1.58 to 2.7) | 89671.06(63230.94 to 109152.83) | 8.86(6.25 to 10.79) | 11770.8(8383.43 to 14571.24) | 1.16(0.83 to 1.44) | 982560.34(697329.81 to 1216618.76) | 97.12(68.93 to 120.26) | ||
| Colon and rectum cancer | Both | 1045.95(928.91 to 1167.86) | 0.05(0.05 to 0.06) | 6016.5(5372.81 to 6703.53) | 0.31(0.27 to 0.34) | 468.68(409.84 to 528.59) | 0.02(0.02 to 0.03) | 37651.16(32919.89 to 42604.06) | 1.92(1.68 to 2.17) | |
| Girl | 498.67(437.56 to 559.23) | 0.05(0.05 to 0.06) | 2737.41(2432.97 to 3055.21) | 0.29(0.26 to 0.32) | 225.41(194.38 to 256.42) | 0.02(0.02 to 0.03) | 18055.71(15509.55 to 20574.24) | 1.9(1.64 to 2.17) | ||
| Boy | 547.27(473.09 to 625.71) | 0.05(0.05 to 0.06) | 3279.1(2840.99 to 3742.34) | 0.32(0.28 to 0.37) | 243.27(208.48 to 279.9) | 0.02(0.02 to 0.03) | 19595.45(16746.89 to 22548.64) | 1.94(1.66 to 2.23) | ||
| Hodgkin lymphoma | Both | 4612.98(3691.63 to 5390.26) | 0.24(0.19 to 0.28) | 26443.22(21929 to 30430.65) | 1.35(1.12 to 1.55) | 1728.12(1254.52 to 2101.37) | 0.09(0.06 to 0.11) | 139274.56(100967.31 to 169386.07) | 7.11(5.15 to 8.64) | |
| Girl | 1541.49(1192.67 to 1825.24) | 0.16(0.13 to 0.19) | 10099.02(8077.61 to 11923.3) | 1.07(0.85 to 1.26) | 457.39(310.76 to 576.99) | 0.05(0.03 to 0.06) | 36917.86(25146.57 to 46517.9) | 3.89(2.65 to 4.91) | ||
| Boy | 3071.49(2249.75 to 3795.75) | 0.3(0.22 to 0.38) | 16344.19(12641.32 to 19990.81) | 1.62(1.25 to 1.98) | 1270.72(867.74 to 1636.34) | 0.13(0.09 to 0.16) | 102356.7(69701.41 to 131124.81) | 10.12(6.89 to 12.96) | ||
| Kidney cancer | Both | 12290.89(10539.58 to 14157.48) | 0.63(0.54 to 0.72) | 87149.24(75172.76 to 100004.83) | 4.45(3.84 to 5.1) | 2712.67(2232.78 to 3241.82) | 0.14(0.11 to 0.17) | 234677.39(193009.25 to 280652.88) | 11.97(9.85 to 14.32) | |
| Girl | 6202.57(5340.49 to 7106.01) | 0.65(0.56 to 0.75) | 46054.92(39626.77 to 52958.06) | 4.86(4.18 to 5.59) | 1100.89(948.09 to 1261.88) | 0.12(0.1 to 0.13) | 95452.08(82068.78 to 109419.71) | 10.07(8.66 to 11.54) | ||
| Boy | 6088.32(5112.98 to 7189.89) | 0.6(0.51 to 0.71) | 41094.32(34615.54 to 48195.53) | 4.06(3.42 to 4.76) | 1611.77(1263.83 to 2001.52) | 0.16(0.12 to 0.2) | 139225.31(109055.02 to 173105.84) | 13.76(10.78 to 17.11) | ||
| Leukemia | Total | Both | 106082.25(91352.8 to 123151.35) | 5.41(4.66 to 6.28) | 657563.11(560193.61 to 770510.43) | 33.55(28.59 to 39.32) | 34371.23(29486.26 to 39862.32) | 1.75(1.5 to 2.03) | 2905010.62(2479706.34 to 3374489.69) | 148.24(126.53 to 172.19) |
| Girl | 50253.49(42572.52 to 58960.49) | 5.3(4.49 to 6.22) | 326684.68(270551.94 to 388662.65) | 34.46(28.54 to 41) | 14286.59(12188.03 to 16243.09) | 1.51(1.29 to 1.71) | 1210756.13(1030391.36 to 1381967.23) | 127.71(108.69 to 145.77) | ||
| Boy | 55828.76(45970.42 to 66676.87) | 5.52(4.54 to 6.59) | 330878.43(274439.08 to 405177.79) | 32.71(27.13 to 40.05) | 20084.64(16257.62 to 23847.97) | 1.99(1.61 to 2.36) | 1694254.49(1369307.19 to 2016366.94) | 167.47(135.35 to 199.31) | ||
| Acute lymphoid leukemia | Both | 33898.85(27955.75 to 39249.58) | 1.73(1.43 to 2) | 172648.53(143302.11 to 201255.93) | 8.81(7.31 to 10.27) | 15503.23(12622.8 to 18432.03) | 0.79(0.64 to 0.94) | 1291630.42(1050466.24 to 1539599.85) | 65.91(53.6 to 78.56) | |
| Girl | 14339.96(11276.14 to 17662.17) | 1.51(1.19 to 1.86) | 77698.9(60623.81 to 95823.17) | 8.2(6.39 to 10.11) | 6023.9(4631.95 to 7692.15) | 0.64(0.49 to 0.81) | 502017.96(384196.44 to 645156.01) | 52.95(40.52 to 68.05) | ||
| Boy | 19558.89(15037.39 to 23250.87) | 1.93(1.49 to 2.3) | 94949.63(74098.35 to 114042.4) | 9.39(7.32 to 11.27) | 9479.33(7151.46 to 11441.53) | 0.94(0.71 to 1.13) | 789612.46(593069.98 to 958109.52) | 78.05(58.62 to 94.7) | ||
| Acute myeloid leukemia | Both | 12549.8(10452.38 to 15108.48) | 0.64(0.53 to 0.77) | 31058.47(25662 to 37750.92) | 1.58(1.31 to 1.93) | 7133.74(5987.05 to 8530.04) | 0.36(0.31 to 0.44) | 594716.8(497574.03 to 713624.47) | 30.35(25.39 to 36.41) | |
| Girl | 5491.27(4414.54 to 7041.43) | 0.58(0.47 to 0.74) | 15473.43(12045.22 to 20376.07) | 1.63(1.27 to 2.15) | 2903.57(2370.66 to 3686.49) | 0.31(0.25 to 0.39) | 241031.01(196528.11 to 309039.44) | 25.42(20.73 to 32.6) | ||
| Boy | 7058.52(5341.32 to 9107.39) | 0.7(0.53 to 0.9) | 15585.04(11612.29 to 20252.1) | 1.54(1.15 to 2) | 4230.17(3240.1 to 5472.62) | 0.42(0.32 to 0.54) | 353685.78(270144.37 to 456757.06) | 34.96(26.7 to 45.15) | ||
| Chronic myeloid leukemia | Both | 3309.27(2240.68 to 4986.88) | 0.17(0.11 to 0.25) | 9329.23(6801.09 to 13239.65) | 0.48(0.35 to 0.68) | 1964.5(1284.51 to 3031.38) | 0.1(0.07 to 0.15) | 166325.52(107565.83 to 258378.33) | 8.49(5.49 to 13.18) | |
| Girl | 1314.82(934.36 to 1828.44) | 0.14(0.1 to 0.19) | 3982.78(2977.72 to 5142.66) | 0.42(0.31 to 0.54) | 756.43(498.98 to 1103.92) | 0.08(0.05 to 0.12) | 63665.39(41649.49 to 93711.15) | 6.72(4.39 to 9.88) | ||
| Boy | 1994.46(1171.69 to 3342.7) | 0.2(0.12 to 0.33) | 5346.45(3387.44 to 8525.65) | 0.53(0.33 to 0.84) | 1208.07(695.46 to 2054.53) | 0.12(0.07 to 0.2) | 102660.13(58010.87 to 176106.34) | 10.15(5.73 to 17.41) | ||
| Other leukemia | Both | 56324.33(46771.89 to 68839.35) | 2.87(2.39 to 3.51) | 444526.88(370151.95 to 543686.54) | 22.68(18.89 to 27.74) | 9769.76(7898.45 to 12048.56) | 0.5(0.4 to 0.61) | 852337.89(688008.17 to 1057097.59) | 43.49(35.11 to 53.94) | |
| Girl | 29107.44(21609.33 to 36932.55) | 3.07(2.28 to 3.9) | 229529.57(170843.35 to 289954.6) | 24.21(18.02 to 30.58) | 4602.69(3287.51 to 5901.7) | 0.49(0.35 to 0.62) | 404041.77(285965.51 to 517863.93) | 42.62(30.16 to 54.62) | ||
| Boy | 27216.9(21955.3 to 34464.78) | 2.69(2.17 to 3.41) | 214997.32(172815.85 to 272136.25) | 21.25(17.08 to 26.9) | 5167.07(4175.27 to 6715.65) | 0.51(0.41 to 0.66) | 448296.12(362590.46 to 584832.78) | 44.31(35.84 to 57.81) | ||
| Lip and oral cavity cancer | Both | 1085.75(923.03 to 1268.71) | 0.06(0.05 to 0.06) | 5930.52(5059.31 to 6901.89) | 0.3(0.26 to 0.35) | 336.68(280.12 to 395.72) | 0.02(0.01 to 0.02) | 26907.89(22480.62 to 31513.69) | 1.37(1.15 to 1.61) | |
| Girl | 663.82(551.95 to 786.99) | 0.07(0.06 to 0.08) | 3748.11(3133.24 to 4451.61) | 0.4(0.33 to 0.47) | 189.56(154.48 to 228.24) | 0.02(0.02 to 0.02) | 15167.52(12330.32 to 18220.55) | 1.6(1.3 to 1.92) | ||
| Boy | 421.93(353.38 to 503.32) | 0.04(0.03 to 0.05) | 2182.42(1834.65 to 2610.15) | 0.22(0.18 to 0.26) | 147.12(121.53 to 176.35) | 0.01(0.01 to 0.02) | 11740.37(9702.1 to 14084.32) | 1.16(0.96 to 1.39) | ||
| Liver cancer | Total | Both | 3718.97(2962.31 to 4785.39) | 0.19(0.15 to 0.24) | 5850.74(4354.24 to 7849.8) | 0.3(0.22 to 0.4) | 3289.71(2673.07 to 3938.99) | 0.17(0.14 to 0.2) | 274538.2(222377.62 to 330244.74) | 14.01(11.35 to 16.85) |
| Girl | 1704.16(1314.04 to 2194.89) | 0.18(0.14 to 0.23) | 2776.53(2022.71 to 3744.11) | 0.29(0.21 to 0.39) | 1530.2(1199.55 to 1876.35) | 0.16(0.13 to 0.2) | 128243.56(100199.41 to 157558.28) | 13.53(10.57 to 16.62) | ||
| Boy | 2014.81(1606.85 to 2676.88) | 0.2(0.16 to 0.26) | 3074.22(2314.47 to 4122.71) | 0.3(0.23 to 0.41) | 1759.51(1413.94 to 2120.99) | 0.17(0.14 to 0.21) | 146294.64(116795.81 to 177602.79) | 14.46(11.54 to 17.56) | ||
| Liver cancer due to hepatitis B | Both | 557.28(431.1 to 705.77) | 0.03(0.02 to 0.04) | 978.06(761.24 to 1234.24) | 0.05(0.04 to 0.06) | 338.26(258.03 to 431.66) | 0.02(0.01 to 0.02) | 25987.69(19832.44 to 33124.62) | 1.33(1.01 to 1.69) | |
| Girl | 146.22(105.51 to 197.5) | 0.02(0.01 to 0.02) | 262.43(192.99 to 351.82) | 0.03(0.02 to 0.04) | 92.72(65.61 to 126.12) | 0.01(0.01 to 0.01) | 7123.38(5044.12 to 9685.06) | 0.75(0.53 to 1.02) | ||
| Boy | 411.06(323.51 to 521.57) | 0.04(0.03 to 0.05) | 715.63(565.95 to 902.28) | 0.07(0.06 to 0.09) | 245.54(189.38 to 314.29) | 0.02(0.02 to 0.03) | 18864.31(14538.17 to 24134.76) | 1.86(1.44 to 2.39) | ||
| Liver cancer due to hepatitis C | Both | 18.04(9.55 to 32.04) | 0(0 to 0) | 32.21(17.31 to 56.57) | 0(0 to 0) | 12.17(5.93 to 23.09) | 0(0 to 0) | 934.7(456 to 1770.57) | 0.05(0.02 to 0.09) | |
| Girl | 8.6(4.56 to 15.09) | 0(0 to 0) | 15.45(8.27 to 26.82) | 0(0 to 0) | 6.52(3.39 to 11.65) | 0(0 to 0) | 500.16(260.46 to 894.75) | 0.05(0.03 to 0.09) | ||
| Boy | 9.43(4.75 to 17.07) | 0(0 to 0) | 16.76(8.71 to 29.85) | 0(0 to 0) | 5.66(2.34 to 11.49) | 0(0 to 0) | 434.54(180.47 to 882.54) | 0.04(0.02 to 0.09) | ||
| Liver cancer due to other causes | Both | 3143.65(2431.36 to 4121.66) | 0.16(0.12 to 0.21) | 4840.48(3416.07 to 6827.28) | 0.25(0.17 to 0.35) | 2939.27(2354.87 to 3566.06) | 0.15(0.12 to 0.18) | 247615.81(197534.22 to 301311.93) | 12.64(10.08 to 15.38) | |
| Girl | 1549.33(1179.98 to 2023.76) | 0.16(0.12 to 0.21) | 2498.65(1743.65 to 3482.44) | 0.26(0.18 to 0.37) | 1430.96(1113.12 to 1763.82) | 0.15(0.12 to 0.19) | 120620.01(93575.04 to 149246.83) | 12.72(9.87 to 15.74) | ||
| Boy | 1594.32(1226.92 to 2195.53) | 0.16(0.12 to 0.22) | 2341.83(1650.08 to 3393.88) | 0.23(0.16 to 0.34) | 1508.31(1198.72 to 1845.05) | 0.15(0.12 to 0.18) | 126995.79(100543.93 to 155366.94) | 12.55(9.94 to 15.36) | ||
| Malignant skin melanoma | Both | 1829.41(1154.92 to 3411.94) | 0.09(0.06 to 0.17) | 14860.13(9088.48 to 29155.69) | 0.76(0.46 to 1.49) | 289.89(212.49 to 443.93) | 0.01(0.01 to 0.02) | 24832.81(17814.51 to 38239.23) | 1.27(0.91 to 1.95) | |
| Girl | 1070(611.24 to 1956.99) | 0.11(0.06 to 0.21) | 9008.71(4959.02 to 16932.47) | 0.95(0.52 to 1.79) | 137.95(99.13 to 214.19) | 0.01(0.01 to 0.02) | 11934.91(8371.17 to 19148.51) | 1.26(0.88 to 2.02) | ||
| Boy | 759.41(495.57 to 2040.11) | 0.08(0.05 to 0.2) | 5851.42(3760.31 to 17376.22) | 0.58(0.37 to 1.72) | 151.95(105.18 to 277.7) | 0.02(0.01 to 0.03) | 12897.91(8815.73 to 23967.53) | 1.27(0.87 to 2.37) | ||
| Nasopharynx cancer | Both | 1119.89(994.15 to 1251.81) | 0.06(0.05 to 0.06) | 6301.74(5638 to 7038.31) | 0.32(0.29 to 0.36) | 437.87(374.77 to 503.38) | 0.02(0.02 to 0.03) | 34736.47(29805.47 to 39827.45) | 1.77(1.52 to 2.03) | |
| Girl | 481.05(424.24 to 541.25) | 0.05(0.04 to 0.06) | 2787.05(2481.13 to 3127.38) | 0.29(0.26 to 0.33) | 164.36(136.9 to 194.27) | 0.02(0.01 to 0.02) | 13090.3(10943.64 to 15475.21) | 1.38(1.15 to 1.63) | ||
| Boy | 638.84(547.34 to 753.9) | 0.06(0.05 to 0.07) | 3514.68(3003.5 to 4155.61) | 0.35(0.3 to 0.41) | 273.51(230.32 to 324.1) | 0.03(0.02 to 0.03) | 21646.17(18271.4 to 25641.03) | 2.14(1.81 to 2.53) | ||
| Non-Hodgkin lymphoma | Both | 14792.67(12072.59 to 18722.38) | 0.75(0.62 to 0.96) | 26551.9(20517.9 to 33518.96) | 1.35(1.05 to 1.71) | 5825.11(5052 to 6688.4) | 0.3(0.26 to 0.34) | 482430.01(418444.58 to 553689.66) | 24.62(21.35 to 28.25) | |
| Girl | 5359.35(4297.12 to 6719.57) | 0.57(0.45 to 0.71) | 3336.89(2093.98 to 5136.9) | 0.35(0.22 to 0.54) | 2083.84(1797.8 to 2401.87) | 0.22(0.19 to 0.25) | 172342.48(148925.07 to 198152.88) | 18.18(15.71 to 20.9) | ||
| Boy | 9433.32(7732.26 to 11887.43) | 0.93(0.76 to 1.18) | 23215(18118.75 to 29391.52) | 2.29(1.79 to 2.91) | 3741.26(3221.12 to 4346.19) | 0.37(0.32 to 0.43) | 310087.53(266397.25 to 360193.96) | 30.65(26.33 to 35.6) | ||
| Other malignant neoplasms | Both | 80604.32(71268 to 92038.42) | 4.11(3.64 to 4.7) | 531221.74(461520.37 to 619863.6) | 27.11(23.55 to 31.63) | 27913.56(23421.58 to 32944.7) | 1.42(1.2 to 1.68) | 2346447.92(1965435.5 to 2775193.82) | 119.73(100.29 to 141.61) | |
| Girl | 44181.75(39014.45 to 50294.68) | 4.66(4.12 to 5.31) | 297330.12(260511.07 to 344885.97) | 31.36(27.48 to 36.38) | 12284.9(10389.11 to 14742.24) | 1.3(1.1 to 1.56) | 1033732.33(873530.61 to 1239676.39) | 109.04(92.14 to 130.76) | ||
| Boy | 36422.57(30789.23 to 42819.95) | 3.6(3.04 to 4.23) | 233891.61(193443.81 to 282781.58) | 23.12(19.12 to 27.95) | 15628.66(12877.71 to 18675.06) | 1.54(1.27 to 1.85) | 1312715.6(1079167.31 to 1574185.59) | 129.76(106.67 to 155.6) | ||
| Ovarian cancer | Both | 2512.34(2057.64 to 3032.04) | 0.13(0.1 to 0.15) | 17151.82(14031.61 to 20593.02) | 0.88(0.72 to 1.05) | 537.67(435.83 to 661.62) | 0.03(0.02 to 0.03) | 43335.58(35221.16 to 53336.66) | 2.21(1.8 to 2.72) | |
| Girl | 2512.34(2057.64 to 3032.04) | 0.27(0.22 to 0.32) | 17151.82(14031.61 to 20593.02) | 1.81(1.48 to 2.17) | 537.67(435.83 to 661.62) | 0.06(0.05 to 0.07) | 43335.58(35221.16 to 53336.66) | 4.57(3.72 to 5.63) | ||
| Boy | - | - | - | - | - | - | - | - | ||
| Testicular cancer | Both | 19053.23(8524.9 to 32528.23) | 0.97(0.44 to 1.66) | 144776.67(58191.66 to 260600.81) | 7.39(2.97 to 13.3) | 526.68(390.13 to 925.54) | 0.03(0.02 to 0.05) | 53259.16(39910.82 to 88520.34) | 2.72(2.04 to 4.52) | |
| Girl | - | - | - | - | - | - | - | - | ||
| Boy | 19053.23(8524.9 to 32528.23) | 1.88(0.84 to 3.22) | 144776.67(58191.66 to 260600.81) | 14.31(5.75 to 25.76) | 526.68(390.13 to 925.54) | 0.05(0.04 to 0.09) | 53259.16(39910.82 to 88520.34) | 5.26(3.94 to 8.75) | ||
| Thyroid cancer | Both | 2356.08(2090.89 to 2632.29) | 0.12(0.11 to 0.13) | 21112.83(18705.31 to 23572.4) | 1.08(0.95 to 1.2) | 198.67(173.88 to 225.86) | 0.01(0.01 to 0.01) | 16864.72(14720.79 to 19145.17) | 0.86(0.75 to 0.98) | |
| Girl | 1497.98(1304.32 to 1703.8) | 0.16(0.14 to 0.18) | 13557.36(11802.61 to 15414.02) | 1.43(1.24 to 1.63) | 95.13(81.66 to 110.2) | 0.01(0.01 to 0.01) | 8261.68(7114.36 to 9638.84) | 0.87(0.75 to 1.02) | ||
| Boy | 858.1(743.43 to 983.64) | 0.08(0.07 to 0.1) | 7555.46(6554.01 to 8661.13) | 0.75(0.65 to 0.86) | 103.53(88.61 to 119.84) | 0.01(0.01 to 0.01) | 8603.04(7344.58 to 9947.05) | 0.85(0.73 to 0.98) | ||
| Tracheal, bronchus, and lung cancer | Both | 281.46(247.6 to 320.7) | 0.01(0.01 to 0.02) | 516.99(456.72 to 583.08) | 0.03(0.02 to 0.03) | 209.28(184.19 to 237.05) | 0.01(0.01 to 0.01) | 16065.79(14127.22 to 18208.64) | 0.82(0.72 to 0.93) | |
| Girl | 141.09(123.08 to 161.06) | 0.01(0.01 to 0.02) | 270.72(237.42 to 306.31) | 0.03(0.03 to 0.03) | 103.15(88.94 to 118.27) | 0.01(0.01 to 0.01) | 7920.93(6831.28 to 9084.78) | 0.84(0.72 to 0.96) | ||
| Boy | 140.37(119.71 to 162.67) | 0.01(0.01 to 0.02) | 246.27(210.39 to 283.6) | 0.02(0.02 to 0.03) | 106.13(91.09 to 123.94) | 0.01(0.01 to 0.01) | 8144.86(6988.29 to 9501.26) | 0.81(0.69 to 0.94) | ||
Abbreviations: UI uncertainty interval; ASIR age-standardized incidence rate; ASDR age-standardized death rate; ASPR age-standardized prevalence rate; DALYs disability-adjusted life-years.
Fig. 5.
Childhood cancers ranked by number of deaths for both sexes combined, globally and regionally, 2019.
Fig. 6.
Percentage changes in age-standardized rates (per 100,000 population) of childhood cancers for both sexes combined from 1990 to 2019. (a) age-standardized DALY rate; (b) age-standardized death rate; (c) age-standardized incidence rate; (d) age-standardized prevalence rate. Abbreviations: DALY disability-adjusted life-year.
The types of cancer among children vary according to age. Children aged over 5 years can be affected by all types of cancer, while tracheal, bronchus, and lung cancer was rare in children and occurred exclusively among children aged 10−14 years (Supplementary Fig. 10). However, besides the 4 common causes of death mentioned above for all aged children with cancer, children aged 1−4 years can be affected by the other five types of cancers, including Hodgkin lymphoma, kidney cancer, liver cancer, malignant skin cancer, and testicular cancer, among which Hodgkin lymphoma did not occur in children under 1 year (Supplementary Fig. 10).
Global top 3 cancers among children
We now present a more specific account of the global top three cancers burdens among children. Our ranking was based on the number of deaths caused by different cancers, and excluding the “other malignant neoplasms.”
Leukemia
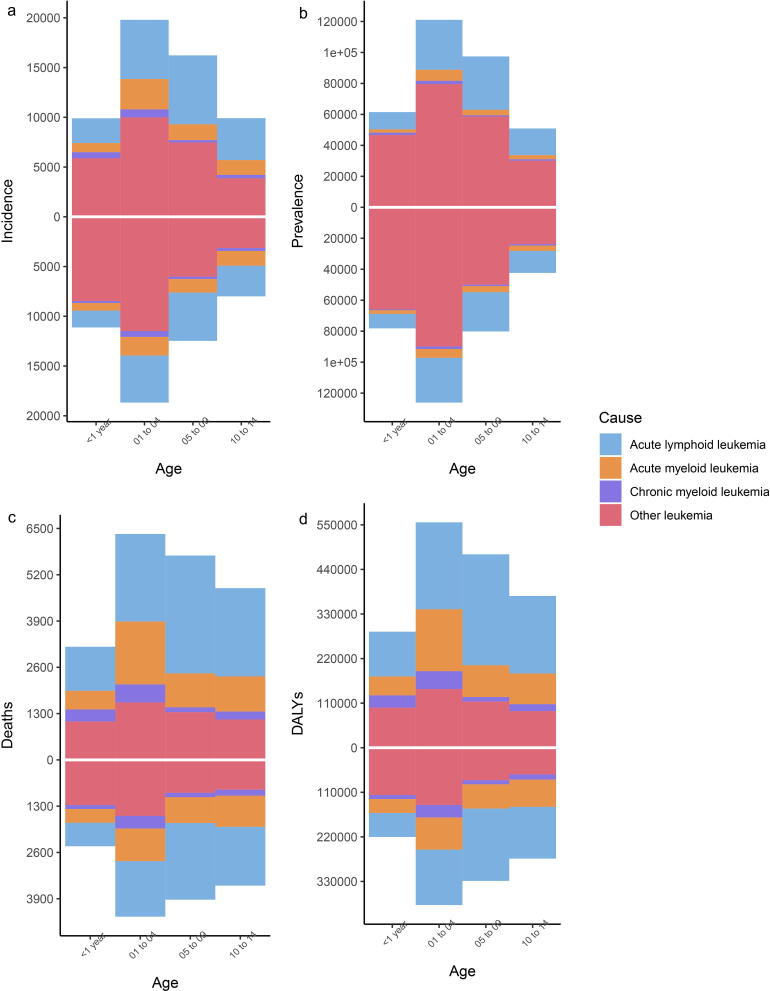
In 2019, 106,082 (91,353 to 123,151) incident cases and 34,371 (29,486 to 39,862) deaths from leukemia were recorded worldwide (Table 2). In the same year, there were 657,563 (560,194 to 770,510) prevalent cases and 2,905,011 (2,479,706 to 3,374,489) DALYs reported globally. Compared with girls, boys are more likely to develop leukemia (with higher incidence and prevalence) and had higher death and DALYs. Among the different age groups, the incidence, prevalence, death, and DALYs of leukemia were highest among children aged 1−4 years. However, the incidence and prevalence of leukemia were lowest among children aged < 1 year, but deaths and DALYs were lowest among children aged 10−14 years (Fig. 7). In terms of subtypes, acute lymphoid leukemia (ALL) contributed to most deaths and DALYs and had the second-highest incidence and prevalence for children, following uncategorized leukemia, which is the sum of other different subtypes of leukemia (Table 2). In 2019, the highest ASIR and ASPR of leukemia occurred in high-middle SDI settings, whereas the highest age-standardized death and DALY rates were observed in low SDI settings. Among the 21 regions, East Asia had the highest ASIR and ASPR in 2019, but the Caribbean and Eastern Sub-Saharan Africa showed the highest age-standardized death and DALY rates, respectively (Supplementary Table 3). Over the last 30 years, leukemia burden has decreased significantly in all regions, except for ASIR and ASPR in Oceania, which had the largest number of countries with an increasing leukemia burden (Supplementary Tables 3 and 4).
Fig. 7.
Distributions of different leukemia sub-types among children with different age and sex. The upper column in each group is data for boys, and the lower column in each group is data for girls. (a) incidence; (b) prevalence; (c) deaths; (d) DALYs. Abbreviations: DALYs disability-adjusted life-years.
Brain and central nervous system cancer
In 2019, 39,933 (30,818 to 46,720) incident cases and 19,988 (15,400 to 23,489) deaths of brain and CNS cancer were documented globally, with 174,646 (135,737 to 204,587) prevalent cases (Table 2). Meanwhile, 1,666,432 (1,287,204 to 1,964,915) DALYs were recorded in the same year (Table 2). The age-standardized incidence, death, and DALY rates of brain and CNS cancer were modestly higher among boys than girls (Supplementary Table 5). Regarding age groups, the incidence and prevalence of brain and CNS cancer were highest among children aged 1−4 years, whereas the number of deaths and DALYs were greatest among children aged 5−9 years (Supplementary Table 5). In 2019, the highest ASIR and ASPR were observed in high SDI settings, which also had the lowest age-standardized death and DALY rates. However, the highest age-standardized death and DALY rates occurred in high-middle SDI settings. Meanwhile, the lowest ASIR and ASPR were found in low SDI settings (Supplementary Table 5). Among the 21 regions, East Asia had the highest ASIR in 2019, and Tropical Latin America had the highest age-standardized death and DALY rates. The lowest age-standardized incidence, prevalence, death, and DALY rates of brain and CNS cancer occurred in Southern Sub-Saharan Africa. Over the last 30 years, East Asia has shown the greatest decrease in age-standardized death and DALY rates, while the Caribbean has shown the largest increase in age-standardized incidence, death, and DALY rates of brain and CNS cancer, with a large number of countries with increasing burdens (Supplementary Table 5 and 6).
Non-Hodgkin lymphoma
In 2019, 14,793 (12,073 to 18,722) incident cases and 5,825 (5,052 to 6,688) deaths from NHL were recorded globally, with 26,552 (20,518 to 33,519) prevalent cases. The global DALYs of NHL were 482,430 (418,445 to 553,690) in 2019 (Table 2). Regarding sex, the age-standardized incidence, prevalence, death, and DALY rates of NHL were higher in boys compared to girls (Supplementary Table 7). NHL did not affect children aged under 1 year but resulted in the greatest number of deaths and DALYs among children aged 1−4 years. (Supplementary Table 7). In 2019, low SDI settings showed the lowest ASIR and ASPR of NHL but the highest age-standardized death and DALY rates. However, the highest ASIR and ASPR were observed in the high-middle SDI settings, and the lowest age-standardized death and DALY rates were observed in high SDI settings (Supplementary Table 7). Among 21 regions, the Caribbean showed the highest age-standardized incidence, deaths, and DALY rates of NHL, and the second-highest ASPR, following Andean Latin America. In the last 30 years, the global burden of NHL has had a notable drop in all five SDI quintiles and 173 countries have experienced decreasing age-standardized death and DALY rates (Supplementary Table 8). The most significant decrease was observed in high SDI settings, with the greatest decrease in ASIR being reported in Eastern Europe and the greatest decrease in age-standardized death and DALY rates appearing in the high-income Asia Pacific (Supplementary Tables 7 and 8). Meanwhile, South Asia had the greatest increase in ASIR and ASPR, and Central Asia showed the largest increase in age-standardized death and DALY rates during the past 30 years (Supplementary Table 7).
Discussion
To the best of our knowledge, this study is the latest and most comprehensive analysis of global, regional, and national cancer burden among children under 15 years of age during the past 30 years. Childhood cancers are relatively rare compared to other childhood diseases [18]. However, childhood cancers have long-term effects on survivors, leading to financial hardship and an elevated risk of subsequent neoplasms and chronic complications [9]. According to our study, there were 291.3 thousand new cases and 98.8 thousand deaths of childhood cancers occurring worldwide in 2019, with a prevalence of 1.8 million and DALYs of 8.3 million. Consistent with previous studies, this study showed that, since 1990, there has been a global decline in the number of deaths and DALYs due to childhood cancers [19], which is possibly due to more accurate diagnoses and better cancer treatments in recent years. However, according to the estimation of the Lancet Oncology Commission, 13.7 million cases will be diagnosed and 11.1 million children will die due to childhood cancers in the next 30 years [20], thus posing a huge challenge to children’s health and social development.
The childhood cancer burden differed substantially among regions and nations according to SDI. Compared with the countries with low SDI, the ASIR and ASPR of childhood cancer were more notable in higher SDI quintiles, and only the high SDI quintile showed an increase in ASPR since 1990. In contrast, the age-standardized death and DALY rates of childhood cancer markedly decreased with SDI, and the declines in lower SDI settings were lower than those in high SDI settings. In HICs, advanced screening facilities, medical care systems, and easier access to health care have led to increased incidence and downward trends in deaths and disability [19], [21]. However, most children with cancer live in LMICs, which only possess less than 5% of global resources for cancer care and control [22], thus causing elevated death and disability rates. Inadequate healthcare infrastructures in LMICs also resulted in delayed diagnosis, underdiagnosis, suboptimal supportive care of childhood cancers, and a low level of social development which in turn results in a lack of awareness, cultural and educational barriers, and coexisting harsh conditions such as malnutrition and infections [23], [24]. As our results showed, the ASIR and ASPR of childhood cancer showed large variations among regions, indicating the factors other than sociodemographic development may also play vital roles in the childhood cancer burden. It is important to note that ethnicity-related genetic variants and environmental risks exposure can also cause great differences in disease burden between regions and nations [25], [26]. Future collaborations among regions are needed to incorporate medical advances in high-income countries to LMICs and improve their health care capacity [4], [27].
Despite significant declines in burden, leukemia, brain, and CNS cancer were the most common cancer and the top three causes of death and DALYs among children with cancer, especially for children aged 1−4 years. In our study, except for unspecified leukemia, ALL was the most common subtype of leukemia for children, which is consistent with the previous study [28]. As mentioned above, multiple factors including genetic risk factors, such as congenital syndromes and gene variants, and environmental risks such as pesticide exposure, ionizing radiation, and infections [29], can help to interpret the elevated risks of ALL among children. We also found that ALL was still the leading cause of deaths and DALYs for children with leukemia, and the age-standardized death and DALY rates were more striking in countries with low SDI. Following medical advancements in the treatment of leukemia, the 5-year survival rate of children with leukemia, and particularly for children with ALL, has dramatically improved, reaching around 90% in developed countries [30]. Nonetheless, in developing countries, children with leukemia tend to have higher mortality and higher relapse rate, possibly due to inadequate supportive care and limited financial resources in these countries [31].
For brain and CNS cancer, we found that the ASIR among children was highest in high SDI settings. This elevated incidence of brain and CNS cancer might be mainly attributed to improvements in diagnosis due to the introduction of CT and magnetic resonance imaging in HICs since the 1980s [32], [33]. As a previous study reported, due to the advanced medical care and improved therapies, children with brain and CNS cancer in higher SDI countries have a higher survival rate [34]. However, our results showed that age-standardized deaths and DALY rates were greatest in high-middle SDI settings, but lowest in countries with low SDI, where also had the lowest ASIR of the brain and CNS cancer among children. This discrepancy might indicate that the results cannot be explained only by SDI, which possibly involves more factors, such as genetic differences and environmental factors. For example, as previously reported, brain and CNS cancer were more common among white populations than the Asian or African populations [35]. Different etiological factors of the brain and CNS cancer have been demonstrated in a previous study [36]. Further studies are needed to focus on the potential risks of childhood cancers and their burden distribution among different regions.
Compared with the previous GBD study that analyzed cancer burden among children and adolescents [18], we provide a more specific and comprehensive analysis of cancer burden among children aged 0−14 years only. We also provide detailed information on the top 3 causes of death among children with cancer. Despite considerable efforts to provide a comprehensive analysis, limitations still exist in this study. First, the cancer burden among children might be underestimated in LMICs where the cancer registration systems might cover only a small number of people [37]. Therefore, our results should be interpreted with caution. Second, ethnic or genetic factors can greatly impact the distribution of cancer among children in different regions and countries. However, different ethnic populations cannot be accessed through GBD studies, and so ethnicity information should be collected and analyzed in future studies. Third, except for the top 3 cancers of deaths among children, burdens of other cancers and their subtypes among children were not provided in detail in this study, which could be completed in further studies.
Conclusions
In conclusion, our study provides a comprehensive evaluation of the distribution of childhood cancer burden and its 30-year changing patterns on a global scale. Although globally childhood cancer burden has been decreasing during the past 30 years, countries with lower SDI settings have still shown higher burdens. Further, despite showing decreasing burdens, leukemia, brain, and CNS cancers were still the most common cancers and the leading causes of death among children. Thus, we hope that this study can provide detailed information for policymakers to allocate resources, implement effective measures, and facilitate collaboration between regions to improve cancer care in lower-income countries. Moreover, our study highlights the need for future studies on advanced therapies and childhood cancer prevention strategies.
Compliance with Ethics Requirements
For Global Burden of Disease study, a waiver of informed consent was reviewed and approved by the Institutional Review Board of the University of Washington. All the information about ethical standards is available through the official website (http://www.healthdata.org/gbd/2019).
Ethics approval and consent to participate
Not applicable.
Availability of data and materials
All data are accessible through the GBD query tool (http://www.healthdata.org/gbd/2019).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We highly appreciated the work of the Global Burden of Disease Study 2019 collaborators for providing the most comprehensive analysis of different diseases on a global scale.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jare.2022.06.001.
Contributor Information
Jun Lyu, Email: lyujun2019@163.com.
Zhijun Dai, Email: dzj0911@126.com.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Siegel R.L., Miller K.D., Fuchs H.E., Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- 2.Gatta G., Botta L., Rossi S., Aareleid T., Bielska-Lasota M., Clavel J., et al. Childhood cancer survival in Europe 1999–2007: results of EUROCARE−5–a population-based study. Lancet Oncol. 2014;15(1):35–47. doi: 10.1016/S1470-2045(13)70548-5. [DOI] [PubMed] [Google Scholar]
- 3.Bhakta N., Force L.M., Allemani C., Atun R., Bray F., Coleman M.P., et al. Childhood cancer burden: a review of global estimates. Lancet Oncol. 2019;20(1):e42–e53. doi: 10.1016/S1470-2045(18)30761-7. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez-Galindo C., Friedrich P., Alcasabas P., Antillon F., Banavali S., Castillo L., et al. Toward the cure of all children with cancer through collaborative efforts: pediatric oncology as a global challenge. J Clin Oncol: Official J Am Soc Clin Oncol. 2015;33(27):3065–3073. doi: 10.1200/JCO.2014.60.6376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta S., Rivera-Luna R., Ribeiro R.C., Howard S.C. Pediatric oncology as the next global child health priority: the need for national childhood cancer strategies in low- and middle-income countries. PLoS Med. 2014;11(6):e1001656. doi: 10.1371/journal.pmed.1001656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olbara G., Martijn H.A., Njuguna F., Langat S., Martin S., Skiles J., et al. Influence of health insurance status on childhood cancer treatment outcomes in Kenya. Support Care Cancer. 2020;28(2):917–924. doi: 10.1007/s00520-019-04859-1. [DOI] [PubMed] [Google Scholar]
- 7.Landier W., Skinner R., Wallace W.H., Hjorth L., Mulder R.L., Wong F.L., et al. Surveillance for late effects in childhood cancer survivors. J Clin Oncol. 2018;36(21):2216–2222. doi: 10.1200/JCO.2017.77.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown AL, Arroyo VM, Agrusa JE, Scheurer ME, Gramatges MM, Lupo PJ. Survival disparities for second primary malignancies diagnosed among childhood cancer survivors: A population-based assessment. 2019. 125(20): p. 3623−3630 [DOI] [PMC free article] [PubMed]
- 9.Nathan P.C., Henderson T.O., Kirchhoff A.C., Park E.R., Yabroff K.R. Financial hardship and the economic effect of childhood cancer survivorship. J Clin Oncology : Official J Am Soc Clin Oncol. 2018;36(21):2198–2205. doi: 10.1200/JCO.2017.76.4431. [DOI] [PubMed] [Google Scholar]
- 10.Robison L.L., Hudson M.M. Survivors of childhood and adolescent cancer: life-long risks and responsibilities. Nat Rev Cancer. 2014;14(1):61–70. doi: 10.1038/nrc3634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brinkman T.M., Zhu L., Zeltzer L.K., Recklitis C.J., Kimberg C., Zhang N., et al. Longitudinal patterns of psychological distress in adult survivors of childhood cancer. Br J Cancer. 2013;109(5):1373–1381. doi: 10.1038/bjc.2013.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allemani C., Matsuda T., Di Carlo V., Harewood R., Matz M., Nikšić M., et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD−3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 14.Steliarova-Foucher E., Colombet M., Ries L.A.G., Moreno F., Dolya A., Bray F., et al. International incidence of childhood cancer, 2001–10: a population-based registry study. Lancet Oncol. 2017;18(6):719–731. doi: 10.1016/S1470-2045(17)30186-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vos T., Lim S.S., Abbafati C., Abbas K.M., Abbasi M., Abbasifard M., et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Majid E, Dean TJ, Alan DL, Colin DM, Christopher JLM. Global burden of disease and risk factors. 2006, World Bank Group.
- 17.Yang S.i., Lin S., Li N.a., Deng Y., Wang M., Xiang D., et al. Burden, trends, and risk factors of esophageal cancer in China from 1990 to 2017: an up-to-date overview and comparison with those in Japan and South Korea. J Hematol Oncol. 2020;13(1) doi: 10.1186/s13045−020−00981−4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The global burden of childhood and adolescent cancer in 2017: an analysis of the Global Burden of Disease Study 2017. The Lancet. Oncology, 2019. 20(9): p. 1211−1225. [DOI] [PMC free article] [PubMed]
- 19.Smith M.A., Altekruse S.F., Adamson P.C., Reaman G.H., Seibel N.L. Declining childhood and adolescent cancer mortality. Cancer. 2014;120(16):2497–2506. doi: 10.1002/cncr.28748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Atun R., Bhakta N., Denburg A., Frazier A.L., Friedrich P., Gupta S., et al. Sustainable care for children with cancer: a Lancet Oncology Commission. Lancet Oncol. 2020;21(4):e185–e224. doi: 10.1016/S1470-2045(20)30022-X. [DOI] [PubMed] [Google Scholar]
- 21.Shah A., Coleman M.P. Increasing incidence of childhood leukaemia: a controversy re-examined. Br J Cancer. 2007;97(7):1009–1012. doi: 10.1038/sj.bjc.6603946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yaris N., Mandiracioglu A., Büyükpamukcu M. Childhood cancer in developing countries. Pediatr Hematol Oncol. 2004;21(3):237–253. doi: 10.1080/08880010490276971. [DOI] [PubMed] [Google Scholar]
- 23.Graetz DE, Garza M, Rodriguez-Galindo C, Mack JW. Pediatric cancer communication in low- and middle-income countries: A scoping review. 2020. 126(23): p. 5030−5039 [DOI] [PubMed]
- 24.Brand NR, Qu LG. Delays and barriers to cancer care in low- and middle-income countries: a systematic review. 2019. 24(12): p. e1371-e1380 [DOI] [PMC free article] [PubMed]
- 25.Valery P.C., Moore S.P., Meiklejohn J., Bray F. International variations in childhood cancer in indigenous populations: a systematic review. Lancet Oncol. 2014;15(2):e90–e103. doi: 10.1016/S1470-2045(13)70553-9. [DOI] [PubMed] [Google Scholar]
- 26.Murray C.J.L., Aravkin A.Y., Zheng P., Abbafati C., Abbas K.M., Abbasi-Kangevari M., et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ribeiro R.C., Antillon F., Pedrosa F., Pui C.-H. Global pediatric oncology: lessons from partnerships between high-income countries and low- to mid-income countries. J Clin Oncol. 2016;34(1):53–61. doi: 10.1200/JCO.2015.61.9148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miranda-Filho A., Piñeros M., Ferlay J., Soerjomataram I., Monnereau A., Bray F. Epidemiological patterns of leukaemia in 184 countries: a population-based study. Lancet Haematol. 2018;5(1):e14–e24. doi: 10.1016/S2352-3026(17)30232-6. [DOI] [PubMed] [Google Scholar]
- 29.Malard F., Mohty M. Acute lymphoblastic leukaemia. Lancet. 2020;395(10230):1146–1162. doi: 10.1016/S0140-6736(19)33018-1. [DOI] [PubMed] [Google Scholar]
- 30.Pulte D., Gondos A., Brenner H. Improvement in survival in younger patients with acute lymphoblastic leukemia from the 1980s to the early 21st century. Blood. 2009;113(7):1408–1411. doi: 10.1182/blood-2008-06-164863. [DOI] [PubMed] [Google Scholar]
- 31.Abdelmabood S., Fouda A.E., Boujettif F., Mansour A. Treatment outcomes of children with acute lymphoblastic leukemia in a middle-income developing country: high mortalities, early relapses, and poor survival. J Pediatr (Rio J) 2020;96(1):108–116. doi: 10.1016/j.jped.2018.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoffman S., Propp J.M., McCarthy B.J. Temporal trends in incidence of primary brain tumors in the United States, 1985–1999. Neuro Oncol. 2006;8(1):27–37. doi: 10.1215/S1522851705000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davis D.L., Hoel D., Percy C., Ahlbom A., Schwartz J. Is brain cancer mortality increasing in industrial countries? Ann N Y Acad Sci. 1990;609:191–204. doi: 10.1111/j.1749-6632.1990.tb32067.x. [DOI] [PubMed] [Google Scholar]
- 34.Eriksson M., Kahari J., Vestman A., Hallmans M., Johansson M., Bergenheim A.T., et al. Improved treatment of glioblastoma - changes in survival over two decades at a single regional Centre. Acta Oncol. 2019;58(3):334–341. doi: 10.1080/0284186X.2019.1571278. [DOI] [PubMed] [Google Scholar]
- 35.Ostrom Q.T., Gittleman H., Truitt G., Boscia A., Kruchko C., Barnholtz-Sloan J.S. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2011–2015. Neuro Oncol. 2018;20(suppl_4):iv1–iv86. doi: 10.1093/neuonc/noy131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ostrom Q.T., Fahmideh M.A., Cote D.J., Muskens I.S., Schraw J.M., Scheurer M.E., et al. Risk factors for childhood and adult primary brain tumors. Neuro Oncol. 2019;21(11):1357–1375. doi: 10.1093/neuonc/noz123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Valsecchi M.G., Steliarova-Foucher E. Cancer registration in developing countries: luxury or necessity? Lancet Oncol. 2008;9(2):159–167. doi: 10.1016/S1470-2045(08)70028-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.