Abstract
Introduction
Measles, one of the most common infections in the world, accounts for more than over 100.000 deaths every year. Measles outbreaks are still ravaging the African continent, and the 2010 Measles outbreak in Zimbabwe is one to be noted, where more than 7754 infections and 517 deaths were reported, ultimately leading to the UN initiation of the vaccination program. COVID-19 could have been delaying the vaccination process in Africa. This article aims to shed the light on the current Measles outbreak in Zimbabwe and how global health organizations are taking measures to fight off this outbreak.
Methodology
Data was collected from online databases PubMed, Science Direct, and the Lancet, as well as news and conferences and press releases on the current measles outbreak. All articles and news related to the measles outbreak in Zimbabwe were taken into consideration.
Results
A measles outbreak was reported earlier in August of 2022, with more than 2000 confirmed cases out of which 157 were reported dead. Since the outbreak this year, cases of measles in Zimbabwe have been rapidly growing. The government in Zimbabwe started a massive vaccination campaign for children in and near the areas where the outbreak is present. Traditional and faith leaders are involved in the campaigns to encourage the public to volunteer to be vaccinated.
Conclusion
Efforts to control the measles outbreak in Zimbabwe are being mitigated by the government as well as the WHO and other global health organizations. With many people refusing the vaccination, this outbreak might not see an end, and more cases, as well as deaths, will increase by the end of the year.
Keywords: Measles, Zimbabwe, Outbreak, Vaccination, Africa
1. Introduction
One of the most infectious illnesses and feared among the younger population in the world is Measles. As of this day, Measles is still responsible for over 100.000 deaths every year [1]. The virus that causes the deadly illness known as measles is a very contagious pathogen. Before the measles vaccine's release in 1963 and widespread immunization, significant outbreaks occurred around every 2–3 years, and measles was thought to be responsible for 2.6 million annual fatalities [2]. Measles outbreaks are still ravaging the African continent. An example would be the 2010 Measles outbreak in Zimbabwe. Between September 2009 and May 2010, Measles was able to spread with 7754 cases and 517 deaths. This horrific tragedy led the United Nations (UN)-backed vaccination program to initiate its operations in Zimbabwe to support the suffering people from this highly contagious and dangerous virus [3]. It is of extreme importance to mention how the existence of novel coronavirus disease 2019 (COVID-19) could have been delaying the vaccination process in the African continent [4].
Hopefully, the light at the end of the tunnel has started to get closer and closer. Measles incidence declined by 66% (from 145 to 49 cases per million people) and fatalities went down by 73% (from 535 600 to 142 300) globally between 2000 and 2018, significantly lowering the disease burden worldwide. The mainstay of measles control and prevention has been the routine Measles-containing-vaccine (MCV) vaccine. MCV is one of the most effective vaccinations ever created, with two doses preventing measles at a 97% rate [5].
Many African nations have also been conducting immunization for Measles. Since 2011, the following countries have maintained measles first dose (MCV1) coverage of 95% or higher: Algeria, Botswana, Gambia, Mauritius, Rwanda, and Seychelles. Only three countries had coverage of 95% or more for the second dose of the measles vaccination in 2015: Algeria, Cape Verde, and Seychelles (MCV2). Only 6 of the 11 nations' 22 supplementary immunization initiatives (SIAs) had administrative coverage lower than 95%. The case-based surveillance performance objectives were only met in all five years by Rwanda and Lesotho [6].
2. Epidemiology and outbreak of Measles in Zimbabwe
Although Zimbabwe lacks documentation of the exact number of measles cases, multiple outbreaks occurred in 1983, 1986, and 1988. Despite advancements in immunization strategies, measles stay endemic to Africa. Although cases have been fluctuating in recent years, outbreaks still occur. According to the National Measles Virology of Zimbabwe (NMVZ), from 2004 to 2009, 3614 case investigations were reported across the whole of Zimbabwe. Of these cases, 92.20% of specimens met World Health Organization (WHO) criteria for laboratory review [7].
In early April of 2022, Manicaland, a province in eastern Zimbabwe, reported an outbreak of measles in Africa, and since then, it has been prevailing in various parts of the country [8]. With this outbreak, measles cases inclined to 400% across Africa due to deferral in immunization [9].
As of Aug 17, 2022, more than 2000 people have been affected by measles. This outbreak has claimed the lives of 157 children, and all of them were unimmunized [10]. The current average population of Zimbabwe is 15 324 398, with a population density of 38 per Km [2] (100 people per mi2), ranked as the 74th most populated country [11]. A congested population lacking enough resources to combat the disease provides a favourable environment for the spreading of measles, a highly contagious viral illness that can easily spread through contact with an infected person. Much of the geographical area of Zimbabwe is occupied by the rural population, which lacks basic awareness about well-timed vaccination of their children and sufficient availability of immunization surveillance, contributing to a major chunk of failure to eliminate measles. In tropical areas, measles outbreaks are associated with rains and many areas of Zimbabwe experience rainfalls throughout the year [1]. These might have contributed to frequent measles outbreaks in Zimbabwe in recent years. However, further studies need to be done to get an insight into the association of measles with climatic variability.
2.1. The trend of Measles during recent past years in Zimbabwe
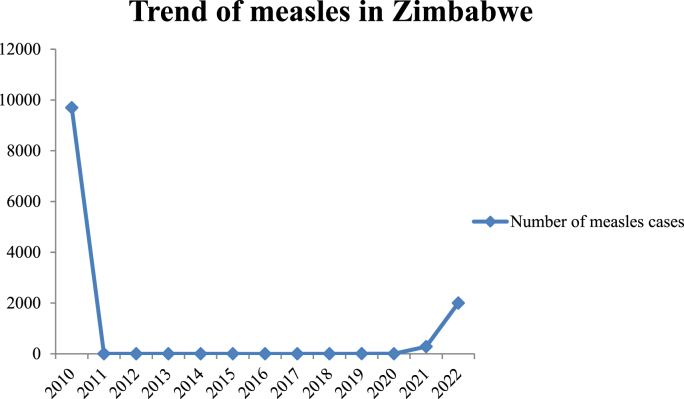
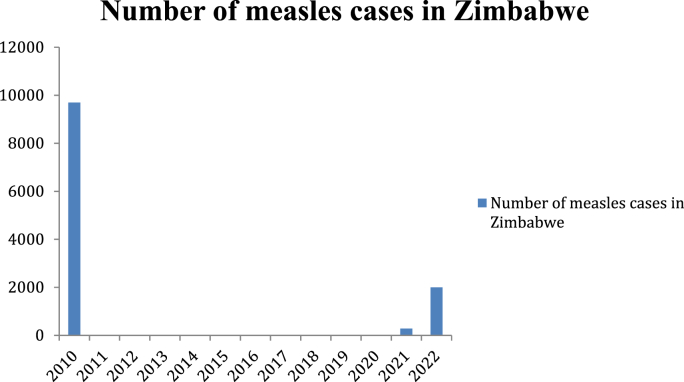
There were 9696 cases in 2010. No cases were reported from 2011 to 2015. In 2016, 2017, and 2018, one case was reported each year. In 2019, 4 cases and 2020, 3 cases were reported. In 2021, 282 cases were reported. The present year reported more than 2000 cases out of which 157 are dead [12]. The situation has raised alarming concerns and a wake-up call to the authorities. Fig. 1 shows the trend and Fig. 2 shows the number of measles cases in recent years in Zimbabwe [3].
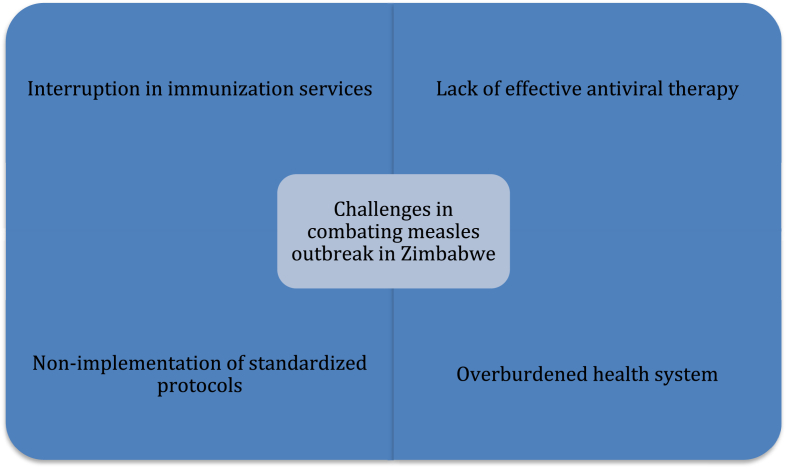
Fig. 3.
depicting challenges in eradicating measles from Zimbabwe.
Fig. 1.
illustrating the trend of measles during recent past years.
Fig. 2.
illustrating the number of measles cases during recent past years.
3. Aetiology of Measles
Measles is an air-born highly contagious preventable systemic disease caused by viral infection with an incubation period between 8 and 11 days after exposure and lasting for an average of 14 days. After the virus enters the host by infecting alveolar macrophages and the dendritic cells of the airway, it replicates in the local lymphatic tissues which are responsible for the systemic infection following the viremia mediated by CD150 positive lymphocytes [13]. It typically has two phase of course. The initial phase is characterized by fever, cough, conjunctivitis, and coryza while the second phase has the typical measles exanthema and the maculopapular rash. The immune suppression following the infection is responsible for most of the complications associated with it [14]. Before the introduction of the vaccine, measles was responsible for 2 million deaths worldwide each year. Children under 5 are still affected by the disease in the era of a safe and effective vaccine [1]. It is caused by an extremely contagious single-stranded RNA virus in the paramyxovirus family called morbillivirus. It directly spreads through contact with infected nasal or oral sections and respiratory air droplets. The virus remains active for up to 2 hours on surfaces and air. Infected individuals will transmit the virus most four days before and after the onset of the rash. Diagnosis is by positive serological test to measles-specific immunoglobulin M. Other diagnostic methods include a 4-fold increase in immunoglobulin G titer, viral culture, and measles RNA test. Unvaccinated children and pregnant women are at increased risk of developing the disease and suffering from the complications. Routine immunization in areas with high disease burden at the age of 9 months and 18 months is an important strategy to decrease morbidity and mortality worldwide [15].
3.1. Current efforts to mitigate Measles in Zimbabwe
The government states that they have started a massive vaccination campaign targeting children aged 6–15 in areas where the outbreak occurred. They are engaging traditional and faith leaders to support that campaign to encourage the public to volunteer to be vaccinated [8].
The WHO's country office in Zimbabwe says that vaccination is the best prevention. As stated, they are strengthening surveillance, ensuring parents, and community members are aware and they report any child who has any symptoms suggesting measles [16].
Also, the opportunities for vaccination are enhanced. Since the virus spreads very quickly, WHO believes that the mass vaccination campaign should not be limited to the country, it should be carried out worldwide.
Efforts to strengthen the vaccination campaign include helping health workers and community leaders communicate actively with caregivers to explain the importance of vaccinations, rectifying gaps in immunization coverage including identifying communities and people who have been missed during the COVID-19 pandemic, implementing country plans to prevent and respond to outbreaks of vaccine-preventable diseases and strengthening immunization systems [17].
4. Challenges encountered
Since the detection of the first case in August 2022, cases of measles in Zimbabwe have been rapidly growing. Depreciation in standard delivery of immunization services in various regions of Zimbabwe and delays in scheduling mass immunizations have led to a toll in cases [18]. Cracks in various African regions' immunization strategies have contributed to maintaining a high incidence of measles. The health ministry of Harare, Zimbabwe, blames religious denominations who have been against immunizations [10]. These religious sects have a staunch belief in the self-proclaimed healing benefits and are hard to convince of vaccination. Emphasis on educating this particular group of people needs to be addressed. Sadly many children of Zimbabwe have neither been monitored for growth nor vaccinated and thus have been a favourite target for measles [19]. No proven antiviral therapy is available, and supportive care is currently the only option for managing measles. Vaccine protocols must be continuously upgraded to prevent incline cases. Zimbabwe, a developing country, faces limited resources for collecting and transporting specimens to maintain the cold chain, which has been an obstacle to adequate sample collection and prompt detection of the correct number of affected patients. Most surveillance systems in Zimbabwe do not meet the criteria of standardized protocols devised for case detection of measles, which fails to correctly identify the exact number of the present and emerging infected patients, which results in many cases going unreported yet contributing to the spread of this disease. Shortage of medications and the increasing number of strikes by healthcare professionals have put tension on Zimbabwe's already fragile healthcare system and needs to be addressed [20]. Rigorous implementation of surveillance strategies and development of concord in laboratory evaluation is the need of the hour to timely detect smaller outbreaks and end the transmission of measles [21]. These encountered challenges are illustrated in Fig. 1.
5. Recommendations
Since the flare-up of Measles during this Pandemic, endeavours have been utilized in battling against it [39]. Extra government monetary help must be given through inoculation awards to state and nearby wellbeing offices to upgrade the immunization conveyance foundation (eg, proficient staff and local area outreach labourers). These assets must be appropriated to regions most out of luck, especially enormous urban communities [22]. New approaches must guarantee that assets are utilized to further develop current inoculation arrangements as opposed to filling in for present status and neighbourhood endeavours. Energetic endeavours ought to be made, including regulation if vital, to guarantee that guarantors give or repay to inoculation as a component of their essential medical advantages bundle and that all overseen medical services frameworks, including wellbeing support associations, give routine immunization administrations [[23], [24], [25], [26], [27], [28]].
Hence, respective companies must survey inoculation levels of clients served by individual suppliers as a proportion of value and guarantee consistency with standard necessities. Particular organizations ought to give either be given antibodies through the public area or be sufficiently repaid for the expense of buying immunizations and their organization [[29], [30], [31], [32], [33], [34], [35]]. To diminish these expenses, immunizations utilized by individual organizations have to be bought at low agreement costs. Great projects have to more readily consent to government direction to put forth forceful attempts to select families; enlist and hold medical services suppliers; give arrangement planning and transportation help and lay out a suggested well-youngster visit plan that keeps the rules [[36], [37], [38], [39]]. Wellbeing divisions have to contact volunteer gatherings and local area-based associations to construct grassroots help for sufficient assets for inoculation and to improve neighbourhood demands for, and prioritization of vaccination. The ongoing public and local area level endeavours to assemble public attention to the significance of preschool inoculation and the adequacy of immunizations and their well-being ought to be escalated [39].
6. Conclusion
Efforts to control the measles outbreak in Zimbabwe are being mitigated by the government as well as the WHO and other global health organizations. Vaccination remains the number one salvation to put an end to this deadly outbreak. However with many people refusing the vaccination, this outbreak might not see an end, and more cases, as well as deaths, will increase by the end of the year. More efforts should be done in increasing awareness among the public to get vaccinated should be done, and vaccinations should be made available for the biggest number of people as much as possible.
Ethical approval
Not Applicable.
Please state any sources of funding for your research
None.
Author contribution
Olivier Uwishema: Conceptualization, Project administration, Writing-review and Designing. Christin Berjaoui: Collection and assembly of data. Olivier Uwishema: Reviewed and edited the first draft, supervisor. Christin Berjaoui: Reviewed and edited the second draft. Jack Wellington MSc (LSHTM) FGMS: Reviewed and edited the final draft, Supervisor.
Consent
Not Applicable.
Registration of research studies
-
1.
Name of the registry: Not Applicable
-
2.
Unique Identifying number or registration ID: Not Applicable
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): Not Applicable
Guarantor
Olivier Uwishema; Principal Investigator (PI)
Declaration of competing of interest
No conflicts of interest declared.
References
- 1.Moss W.J. Measles. The Lancet. 2017;390(10111):2490–2502. doi: 10.1016/S0140-6736(17)31463-0. https://pubmed.ncbi.nlm.nih.gov/28673424/ [DOI] [PubMed] [Google Scholar]
- 2.WHO Measels. August 2022. https://www.who.int/news-room/fact-sheets/detail/measles Accessed on the 23rd of.
- 3.Annual report on the use of cerf grants Zimbabwe. United nations CERF wed, 12/01/2010. https://cerf.un.org/sites/default/files/resources/ANNUAL%20REPORT-%20Zimbabwe_FINAL_WEB.pdf Available at:
- 4.Guha-Sapir D., Moitinho de Almeida M., Keita M., Greenough G., Bendavid E. COVID-19 policies: remember measles. Sci. 2020;369(6501) doi: 10.1126/science.abc8637. https://www.science.org/doi/full/10.1126/science.abc8637 261–261. [DOI] [PubMed] [Google Scholar]
- 5.Gastañaduy P.A., Goodson J.L., Panagiotakopoulos L., Rota P.A., Orenstein W.A., Patel M. Measles in the 21st century: progress toward achieving and sustaining elimination. J. Infect. Dis. 2021;224(12 Suppl 2):S420–s428. doi: 10.1093/infdis/jiaa793. https://academic.oup.com/jid/article/224/Supplement_4/S420/6378081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masresha B., Luce R., Shibeshi M., et al. Status of measles elimination in eleven countries with high routine immunisation coverage in the WHO african region. J Immunol Sci. 2018:140–144. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6372061/ Suppl. [PMC free article] [PubMed] [Google Scholar]
- 7.Ruhanya V., Moyo S.R. Measles laboratory-based surveillance in Zimbabwe during 2004-2009. Germs. 2012;2(2):36–42. doi: 10.11599/germs.2012.1012. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3882865/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mutsaka F. Measles outbreak in Zimbabwe kills 157 unvaccinated children. The Washington Post2022. https://www.washingtonpost.com/world/measles-outbreak-in-zimbabwe-kills-157-unvaccinated-children/2022/08/17/95320f70-1e1a-11ed-9ce6-68253bd31864_story.html Available at:
- 9.More than 150 children dead in Zimbabwe measles outbreak [press release] VOA News. August 16, 2022:2022. https://www.voanews.com/a/children-s-death-toll-rises-in-zimbabwe-measles-outbreak-/6704160.html Available at: [Google Scholar]
- 10.Zimbabwe's measles outbreak claims 157 lives [press release] VOA News. August 17, 2022:2022. https://www.voanews.com/a/zimbabwe-s-measles-outbreak-claims-157-lives/6705349.html Available at: [Google Scholar]
- 11.Zimbabwe population. Worldometers. https://www.worldometers.info/world-population/zimbabwe-population/ Available at:
- 12.Measles reported cases Knoema. https://knoema.com/atlas/Zimbabwe/topics/Health/Communicable-Diseases/Measles-cases?mode=amp Available at:
- 13.de Vries R.D., Mesman A.W., Geijtenbeek T.B., Duprex W.P., de Swart R.L. The pathogenesis of measles. Curr. Opin. Virol. 2012;2(3):248–255. doi: 10.1016/j.coviro.2012.03.005. https://www.sciencedirect.com/science/article/pii/S1879625712000491?casa_token=fF0VwGfr6egAAAAA: QYSJkS0wtL49IrPV67YkrhtXzjmragAuanrf9PI0Uy_zoFEFUtBiws1M0kQocwSA23ksVhsNHdqN [DOI] [PubMed] [Google Scholar]
- 14.Jeuck J.C. Die Einführung der Masernimpfung in der BRD 1960-1980 im Spiegel medizinischer Fachjournale und der Laienpresse. Dissertation, Köln, Universität zu Köln. 2017;2017 https://coronadatencheck.com/wp-content/uploads/2020/04/Jeuck_2017-03-02.pdf [Google Scholar]
- 15.Leung G.K., Ho Y. About this journal. Hong Kong Med. J. 2018;24(4):384–390. doi: 10.12809/hkmj187346. https://www.hkmj.org/abstracts/v24n5/512.htm [DOI] [PubMed] [Google Scholar]
- 16.Beliefs Religious. Terrain hampering measles immunization program in Zimbabwe [press release] VOA News. May 15, 2022 https://www.voanews.com/a/religious-beliefs-terrain-hampering-measles-immunization-program-in-zimbabwe/6574199.html [Google Scholar]
- 17.UNICEF and WHO warn of perfect storm of conditions for measles outbreaks, affecting children. WHO and UNICEF. https://www.who.int/news/item/27-04-2022-unicef-and-who-warn-of–perfect-storm–of-conditions-for-measles-outbreaks–affecting-children Available at:
- 18.Masresha B.G., Luce R., Jr., Shibeshi M.E., et al. The performance of routine immunization in selected African countries during the first six months of the COVID-19 pandemic. Pan Afr. Med. J. 2020;37(Suppl 1) doi: 10.11604/pamj.supp.2020.37.1.26107. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7733346/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Press Conference Update on the state of measles outbreaks and control strategies in Zimbabwe [press release] United Nat. Off. Coordination. Hum. Affairs (OCHA) Mar 2010;29 https://reliefweb.int/report/zimbabwe/press-conference-update-state-measles-outbreaks-and-control-strategies-zimbabwe Available at: [Google Scholar]
- 20.Zimbabwe blames measles surge on sect gatherings after 80 children die [press release] Swissinfo. August 14, 2022 https://www.swissinfo.ch/eng/reuters/zimbabwe-blames-measles-surge-on-sect-gatherings-after-80-children-die/47826700 Available at: [Google Scholar]
- 21.Sniadack D.H., Crowcroft N.S., Durrheim D.N., Rota P. Roadmap to elimination-standard measles and rubella surveillance. Wkly. Epidemiol. Rec. 2017;9:10–92. https://apps.who.int/iris/rest/bitstreams/1080744/retrieve Available at: [PubMed] [Google Scholar]
- 22.Henderson D.A., Dunston F.J., Fedson D.S., et al. The measles epidemic: the problems, barriers, and recommendations. JAMA. 1991;266(11):1547–1552. https://www.sciencedirect.com/science/article/pii/S204908012201024X [PubMed] [Google Scholar]
- 23.Uwishema O., Alshareif B., Yousif M., Omer M., Sablay A., Tariq R., Zahabioun A., Mwazighe R.M., Onyeaka H. Lassa fever amidst the COVID-19 pandemic in Africa: a rising concern, efforts, challenges, and future recommendations. J. Med. Virol. 2021;93(12):6433–6436. doi: 10.1002/jmv.27219. [DOI] [PubMed] [Google Scholar]
- 24.Uwishema O., Chalhoub E., Torbati T., David S.C., Khoury C., Ribeiro L., Nasrallah Y., Bekele B.K., Onyeaka H. Rift Valley fever during the COVID-19 pandemic in Africa: a double burden for Africa's healthcare system. Health Sci. Rep. 2022;5(1):e468. doi: 10.1002/hsr2.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Uwishema O., Nnagha E.M., Chalhoub E., Nchasi G., Mwazighe R.M., Akin B.T., Adanur I., Onyeaka H. Dengue fever outbreak in Cook Island: a rising concern, efforts, challenges, and future recommendations. J. Med. Virol. 2021;93(11):6073–6076. doi: 10.1002/jmv.27223. [DOI] [PubMed] [Google Scholar]
- 26.Uwishema O., Elebesunu E.E., Bouaddi O., Kapoor A., Akhtar S., Effiong F.B., Chaudhary A., Onyeaka H. Poliomyelitis amidst the COVID-19 pandemic in Africa: efforts, challenges and recommendations. Clin. Epidemiol. Global Heal. 2022;16 doi: 10.1016/j.cegh.2022.101073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uwishema O., Onyeaka H., Badri R., Yücel A.N., Korkusuz A.K., Ajagbe A.O., Abuleil A., Chaaya C., Alhendawi B., Chalhoub E. The understanding of Parkinson's disease through genetics and new therapies. Brain. Behav. 2022;12(5):e2577. doi: 10.1002/brb3.2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Uwishema O., Ayoub G., Badri R., Onyeaka H., Berjaoui C., Karabulut E., Anis H., Sammour C., Mohammed Yagoub F., Chalhoub E. Neurological disorders in HIV: hope despite challenges. Immun. Inflammation. Dis. 2022;10(3):e591. doi: 10.1002/iid3.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greene L., Uwishema O., Nicholas A., Kapoor A., Berjaoui C., Adamolekun E., Khoury C., Mohammed F., Onyeaka H. Crimean-Congo haemorrhagic fever during the COVID-19 pandemic in Africa: efforts, recommendations and challenges at hand. African journal of emergency medicine. Revue africaine de la medecine d'urgence. 2022;12(2):117–120. doi: 10.1016/j.afjem.2022.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun J., Uwishema O., Kassem H., Abbass M., Uweis L., Rai A., El Saleh R., Adanur I., Onyeaka H. Ebola Virus Outbreak Return. Democratic Repub. Congo.: Urgent. Rising. Concern. Ann. Med. Surg. 2022 doi: 10.1016/j.amsu.2022.103958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adekunbi O., Uwishema O., Adanur I., Onyeaka H. Prospect of acute hepatitis E virus outbreak in the context of the COVID-19 Pandemic in Africa: a contingency plan. Ann. Med. Surg. 2022 doi: 10.1016/j.amsu.2022.104084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Uwishema O., Berjaoui C., Correia I., Anis H., Karabulut E., Essayli D., Mhanna M., Oluyemisi A. Current management of acute ischemic stroke in Africa: a review of the literature. Eur. J. Neurol. 2022 doi: 10.1111/ene.15495. 10.1111/ene.15495. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 33.Uwishema O., Mahmoud A., Sun J., Correia I., Bejjani N., Alwan M., Nicholas A., Oluyemisi A., Dost B. Is Alzheimer's disease an infectious neurological disease? A review of the literature. Brain and behavior, e2728. Adv. Online Pub. 2022 doi: 10.1002/brb3.2728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pradhan, Umesh Aishwarya, et al. “A review of stem cell therapy: an emerging treatment for dementia in alzheimer's and Parkinson's disease.” brain and behavior. August. 2022 doi: 10.1002/brb3.2740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Uwishema, Olivier, et al. “The impact of COVID-19 on patients with neurological disorders and their access to healthcare in Africa: a review of the literature.”. Brain. Behav. August. 2022 doi: 10.1002/brb3.2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Uwishema O., Mahmoud A., Wellington J., Mohammed S.M., Yadav T. DerbiehM, Arab S, Kolawole B, A review on acute, severe hepatitis of unknown origin in children: a call forconcern. Ann. Med. Surg. 2022 doi: 10.1016/j.amsu.2022.104457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Uwishema O., Adekunbi O., Peñamante C.A., Bekele B.K., Khoury C., MhannaM Nicholas A., Adanur I., Dost B., Onyeaka H. The burden of monkeypox virus amidst the Covid-19pandemic in Africa: a double battle for Africa. Ann. Med. Surg. 2022 doi: 10.1016/j.amsu.2022.104197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Uwishema O., Taylor C., Lawal L., Hamiidah N., Robert I., Nasir A., Chalhoub E., Sun J., Akin B.T., Adanur I., Mwazighe R.M., Onyeaka H. The syndemic burden of HIV/AIDS in Africa amidst the COVID-19 pandemic. Immun. Inflammation. Dis. 2022;10(1):26–32. doi: 10.1002/iid3.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Uwishema O., Adriano L.F., Torbati T., Onyeaka H. Measles crisis in Africa amidst the COVID-19 pandemic: delayed measles vaccine administration may cause a measles outbreak in Africa. J. Med. Virol. 2021;93(10):5697–5699. doi: 10.1002/jmv.27150. [DOI] [PubMed] [Google Scholar]