Abstract
Background and aims
The effect of dapagliflozin (DAPA) on the prognosis of patients with acute myocardial infarction (AMI) is unclear. The present study was conducted to evaluate the association between DAPA administration and adverse events in patients with AMI undergoing percutaneous coronary intervention (PCI).
Methods
This single-center retrospective analysis study included a total of 786 patients with AMI from January 2019 to August 2021 who were or were not administered DAPA at discharge. The primary endpoint was the composite of major adverse cardiovascular events (MACE), including overall deaths, heart failure, nonfatal MI, nonfatal stroke, and unplanned repeat revascularization (URR). Differences in the triglyceride glucose (TyG) index and the atherogenic index of plasma (AIP) both during hospitalization and 12 months after discharge (if achievable) were also compared.
Results
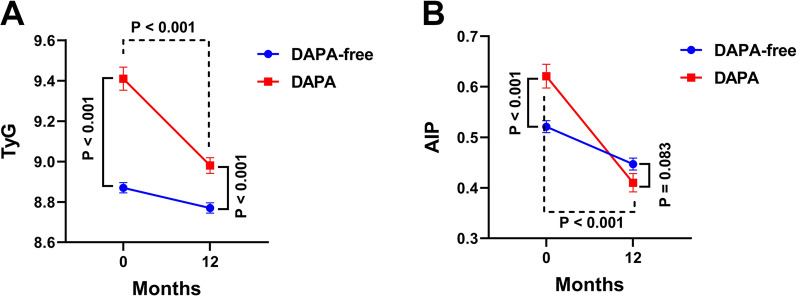
During a median follow-up of 23 months, 130 patients had MACE (118 in the DAPA-free group and 12 in the DAPA group). Kaplan–Meier survival analyses revealed that the cumulative incidence of MACE (log-rank test, p = 0.009), heart failure (p = 0.003), nonfatal MI (p = 0.005), and URR (p = 0.031) was higher in the DAPA-free group. In addition, the multivariate Cox analysis showed that DAPA was significantly associated with the reduced risk of MACE (hazard ratio = 0.170, 95% confidence interval = 0.078–0.373, p < 0.001). Considering each specific adverse event, the DAPA-free group was associated with heart failure, nonfatal MI, and URR in multivariate Cox regression analyses. Stratification analyses suggested that DAPA has a strong protective effect in patients with AMI of advanced age with concomitant diabetes or those who are not on angiotensin receptor enkephalinase inhibitors. Furthermore, the TyG index and AIP of the patients 12 months after DAPA administration at discharge were significantly lower than those during hospitalization.
Conclusions
DAPA is an independent protective factor against MACE and may provide incremental prognostic information in patients with AMI undergoing PCI.
Keywords: DAPA, AMI, MACE, TyG, AIP
Introduction
Despite extensive progress in the field of interventional therapy, the incidence of major adverse cardiovascular events (MACE) in patients with acute myocardial infarction (AMI) is still high. Risk factors such as diabetes, chronic kidney disease (CKD), atrial fibrillation, high coronary disease burden, low ejection fraction, and advanced age may worsen the prognosis of such patients [1–3]. SGLT2 inhibitors (SGLT2i) have been shown to improve cardiorenal endpoints in patients with type 2 diabetes (T2DM), CKD, and chronic heart failure with reduced ejection fraction (HFrEF) [4–6]. The EMPA-REG OUTCOME trial showed that SGLT2i improved the admission rate of cardiovascular mortality and HF in patients with a long-term history of MI [7, 8]. However, it is not clear whether SGLT2i can improve outcomes in patients with AMI.
Considering the residual risk under current treatment strategies and the growing clinical evidence that support the use of SGLT2i, patients with a long term coronary artery disease are more likely to suffer from coexisting SGLT2i indications (such as T2DM or HF). Therefore, it is difficult to directly determine whether the benefit of SGLT2i observed in patients with T2DM or HF may also benefit those with concomitant AMI. Despite the contiguous spectrum of treatments, trials in those with AMI are needed to validate consistent treatment effects. At present, there is a large gap in evidence regarding SGLT2i in the HF risk spectrum of patients with AMI. Previous studies on the benefits of SGLT2i in patients with HF have primarily focused on HF stages A/C/D; however, fewer studies have evaluated HF stage B patients with AMI, i.e., the presence of cardiac structural changes without any clinical signs of HF [9]. However, this population constitutes a considerable proportion of patients with HF. Unfortunately, in previous large-scale studies (EMPA-REG OUTCOME (BI 10,773 [Empagliflozin] Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients), CANVAS (CANagliflozin cardioVascular Assessment Study), CREDENCE (Computed Tomographic Evaluation of Atherosclerotic Determinants of Myocardial Ischemia), and others), these patients were completely excluded at the time of enrollment [7, 10, 11]. Thus, there are several questions regarding the therapeutic efficacy of SGLT2i in patients with AMI that need to be answered via clinical studies.
In the present study, the association between dapagliflozin (DAPA), an SGLT2i, and MACE in patients with AMI undergoing percutaneous coronary intervention (PCI) was explored. In addition, the effects of DAPA on coronary artery disease-related indicators were evaluated.
Patients and methods
Ethics approval
This study was approved by the Committee of Clinical Investigation of The Affiliated Changzhou No.2 People’s Hospital of Nanjing Medical University (2020-KY253-01) and conducted in accordance with the guidelines of the Declaration of Helsinki.
Participants
This was a single-center, retrospective analysis derived from a prospective observational study (ChiCTR1800014583) on patients with AMI undergoing PCI that was conducted between January 2019 and August 2021 at The Affiliated Changzhou No.2 People’s Hospital of Nanjing Medical University. All the enrolled patients have not used SGLT2i drugs before. For this study, patients were consecutively enrolled and followed-up 1 month after discharge and every 3 months thereafter. The general condition, vital signs, hospitalization and medication status were consulted at each follow-up visit, and patients were invited to the outpatient clinic if necessary.
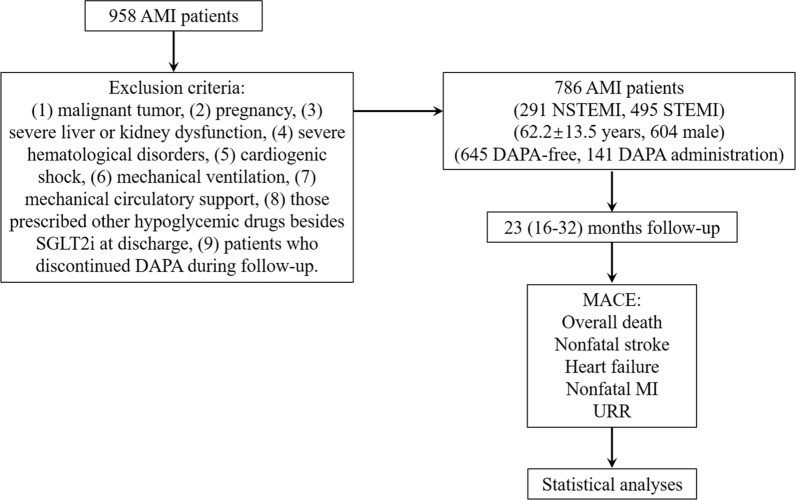
The exclusion criteria of this study were as follows: patients with malignant tumor, pregnancy, severe liver or kidney dysfunction, severe hematological disorders, cardiogenic shock, mechanical ventilation, mechanical circulatory support, those prescribed other hypoglycemic drugs besides SGLT2i at discharge and patients who discontinued DAPA during follow-up. A considerable number of DM patients were excluded, and most of the selected DM patients were in the early stage of DM, mainly relying on diet control and exercise. Severe liver dysfunction was considered as elevated serum transaminases, severely elevated serum bilirubin, decreased albumin concentration and coagulation disorders. Severe kidney dysfunction was considered as CKD stage IV or V. Severe hematological disorders were defined as multiple myeloma, lymphoma, myelodysplastic syndrome or leukemia (Fig. 1).
Fig. 1.
Study flow. Patients selection, exclusion criteria, follow-up and the definition of MACE
Data retrieval
Demographic information, clinical characteristics, clinical events, medical histories, treatment, laboratory examinations, and medical instrument inspection records during hospitalization were retrieved from the hospital’s electronic medical record system.
In this study, arrhythmia (within 1 week of admission) was defined as at least one episode of atrial fibrillation, atrial flutter, ventricular fibrillation, or ventricular flutter. Hypertension was considered as a systolic blood pressure of > 140 mmHg and/or diastolic blood pressure (DBP) of > 90 mmHg and/or receiving antihypertension treatment. A fasting plasma glucose of > 7.0 mmol/L, casual plasma glucose of > 11.1 mmol/L, 2-h blood glucose of > 11.1 mmol/L after an oral glucose tolerance test, and/or use of antidiabetic medicine were considered to indicate diabetes.
The Gensini score was used to assess the severity of coronary artery disease and calculated as shown previously [12]. The atherogenic index of plasma (AIP) was defined as the logarithm to the base 10 of the ratio of fasting plasma triglyceride (TG) (mg/dL) to high-density lipoprotein cholesterol (HDL-C) [log (TG/HDL-C)], and the TG glucose (TyG) index was calculated as Ln (fasting TG (mg/dL) × fasting blood glucose (mg/dL) / 2).
Information on MACE was obtained via telephone calls or from the medical records system. The primary endpoint was the composite of MACE, including overall deaths, HF, nonfatal MI, nonfatal stroke, and unplanned repeat revascularization (URR). HF was diagnosed as per the typical symptoms, signs, and laboratory tests, including orthopnea, acute pulmonary edema, and brain natriuretic peptide (BNP) testing. MI was considered as [1] symptoms of ischemic chest pain; [2] a characteristic ST-T dynamic evolution on the electrocardiogram, or with abnormal q waves; [3] serum myocardial enzyme spectrum increased and decreased. Nonfatal MI was diagnosed as new pathological Q waves in ≥ 2 contiguous electrocardiogram leads according to the previous study [13]. Patients with an acute ischemic cerebral vascular event were diagnosed with stroke, and any nonstaged revascularization after PCI was considered URR (Fig. 1).
Statistical analyses
All data were subjected to a normal distribution test and are expressed as the mean ± standard deviation for approximately normally distributed data and as the median (interquartile range) for skewed continuous data. Continuous variables between two groups were compared using Student’s t-test or the Mann–Whitney U-test according to their distribution. The chi-squared test was used for comparing categorical variables between the groups. Cumulative incidence curves were visualized using the Kaplan–Meier analyses, and the log-rank test was performed. Cox proportional hazard analyses with six models were performed to detect any independent risk factors by computing the hazard ratio with a 95% confidence interval (CI). Subgroup analyses according to the factors of age, sex, hypertension, diabetes, low-density lipoprotein cholesterol (LDL-C), and angiotensin receptor enkephalinase inhibitor (ARNI) administration were performed. All tests were two tailed, and p values < 0.05 were considered significant. All statistical analyses were performed using SPSS software 22.0 (SPSS Inc., Chicago, IL, USA).
Results
A total of 786 patients with a median follow-up of 23 months (interquartile range: 16–32 months) were included in the study; their mean age was 62 ± 14 years and 604 (76.8%) patients were men. The baseline characteristics of the participants are summarized in Table 1. Higher proportion of patients who received DAPA had hypertension or diabetes. These patients also had higher BNP and HbA1c levels as well as larger left ventricular end-diastolic diameters but lower HDL-C, creatine phosphokinase, and left ventricular ejection fraction levels. In angiography, patients with DAPA intervention had a higher Gensini score. With regard to drugs, higher proportion of patients who received DAPA also received ARNI and mineralocorticoid receptor antagonist at discharge.
Table 1.
Baseline characteristics of the study population
| Characteristics | DAPA-free (n = 645) | DAPA (n = 141) | P value |
|---|---|---|---|
| Age (years) | 62.5 ± 13.5 | 60.6 ± 13.6 | 0.894 |
| Sex, male, n (%) | 497 (77.1) | 105 (74.5) | 0.452 |
| BMI (kg/m2) | 24.4 ± 3.9 | 26.2 ± 4.1 | 0.885 |
| Smoking, n (%) | 319 (49.5) | 63 (44.7) | 0.281 |
| Hypertension, n (%) | 393 (60.9) | 104 (73.8) | 0.005 |
| Diabetes, n (%) | 96 (14.9) | 96 (68.1) | < 0.001 |
| Cerebral infarction, n (%) | 40 (6.2) | 8 (5.7) | 0.867 |
| In-hospital arhythmia, n (%) | 47 (7.3) | 12 (8.5) | 0.628 |
| In-hospital AHF, n (%) | 57 (8.8) | 14 (9.9) | 0.694 |
| Length of stay (days) | 8 (6.8–9) | 8 (7–10) | 0.220 |
| STEMI, n (%) | 396 (61.4) | 99 (70.2) | 0.050 |
| Stenting/POBA, n (%) | 627 (97.2) | 136 (96.5) | 0.398 |
| Multivessel disease, n (%) | 616 (95.5) | 130 (92.2) | 0.106 |
| Gensini score | 42 (21–69) | 49 (34–80) | 0.002 |
| Biochemical test | |||
| ALP (U/L) | 76.5 ± 25.6 | 77.9 ± 20.5 | 0.658 |
| UA (umol/L) | 331 (280–400) | 324 (246–393) | 0.112 |
| LDL-C (mmol/L) | 2.58 ± 0.88 | 2.77 ± 0.89 | 0.946 |
| HDL-C (mmol/L) | 1.06 ± 0.30 | 1.01 ± 0.26 | 0.023 |
| TC (mmol/L) | 4.3 ± 1.1 | 4.6 ± 1.4 | 0.677 |
| TG (mmol/L) | 1.42 (1.05–1.99) | 1.76 (1.23–2.42) | 0.132 |
| BNP (pg/mL) | 330 (99–1120) | 521 (145–1985) | < 0.001 |
| CPK (U/L) | 534 (133–1446) | 486 (185–1276) | 0.028 |
| CK-MB (U/L) | 51.4 (21.2–123.1) | 52.4 (21.9–109.9) | 0.055 |
| HBDH (U/L) | 351 (196–672) | 337 (198–571) | 0.338 |
| HbA1c (%) | 6.2 ± 1.2 | 7.9 ± 1.7 | < 0.001 |
| Ccr (ml/min) | 66 ± 43 | 69 ± 33 | 0.917 |
| Ultrasonic cardiogram | |||
| LA (mm) | 3.9 ± 0.5 | 4.0 ± 0.5 | 0.553 |
| LV (mm) | 5.1 ± 0.5 | 5.3 ± 0.6 | 0.015 |
| EF (%) | 53 ± 9 | 49 ± 10 | 0.021 |
| Pharmacological intervention | |||
| β-block, n (%) | 364 (56.4) | 81 (57.4) | 0.817 |
| ACEI/ARB, n (%) | 213 (33.0) | 39 (27.7) | 0.218 |
| ARNI, n (%) | 126 (19.5) | 42 (29.8) | 0.007 |
| MRA, n (%) | 50 (7.8) | 16 (11.3) | < 0.001 |
Values are shown as the means ± SD, median (interquartile range) or percentage
BMI body mass index, POBA plain old balloon angioplasty, ALP alkaline phosphatase, UA uric acid, LDL-C low-density lipoprotein cholesterol, HDL-C high-density lipoprotein cholesterol, TC total cholesterol, TG triglycerides, BNP brain natriuretic peptide, CPK creatine phosphokinase, CK-MB creatine kinase-MB, HDBH hydroxybutyrate dehydrogenase, Ccr creatinine clearance rate, LA left atrium, LV left ventricle, EF ejection factor, ARNI angiotensin receptor-neprilysin inhibitor, MRA mineralocorticoid receptor antagonist
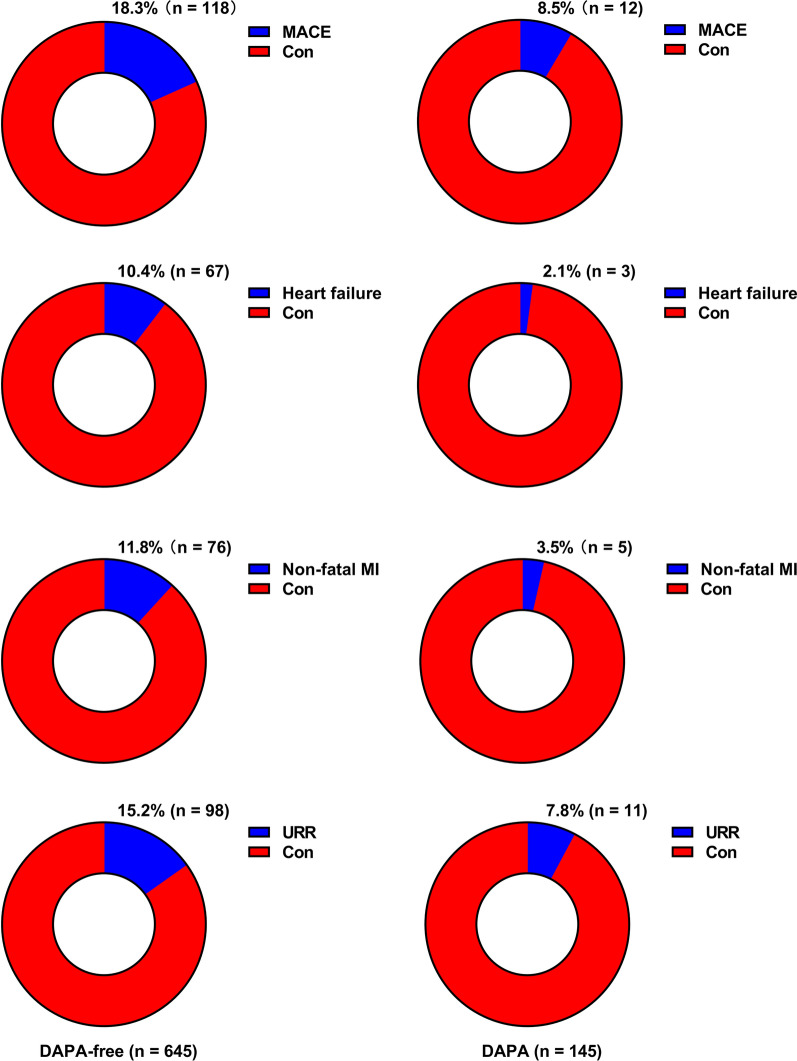
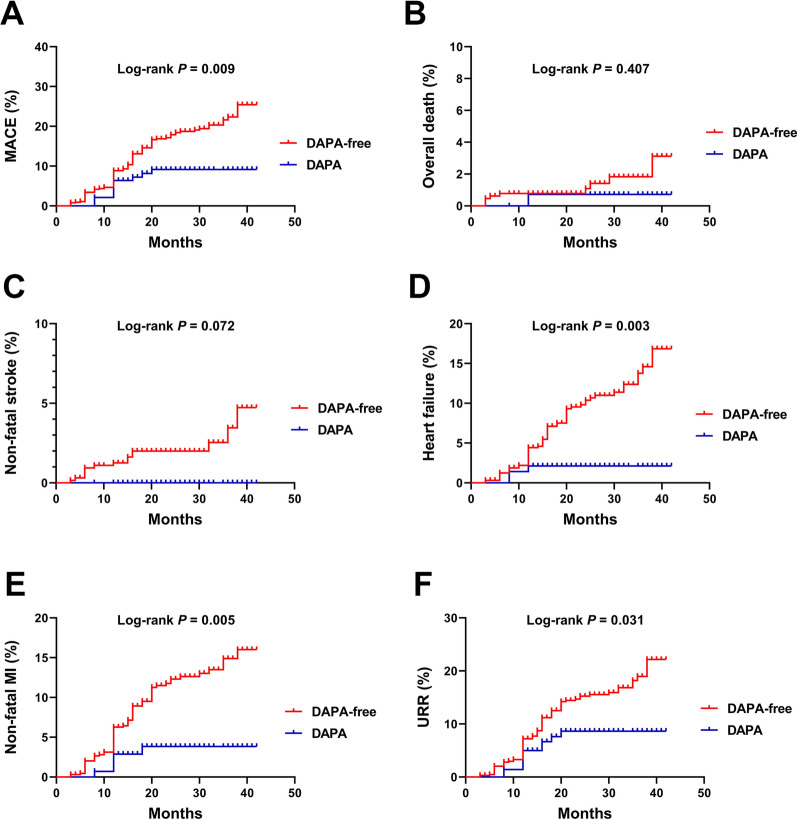
At follow-up, more patients without DAPA administration had MACE. Moreover, a higher percentage of these patients had HF, nonfatal MI, and URR (all p < 0.05) (Table 2 and Fig. 2). Kaplan–Meier survival analysis revealed that the cumulative incidence of MACE increased without DAPA therapy (log-rank test, p = 0.009) (Fig. 3). Considering each component of MACE, patients without DAPA administration at discharge had a higher cumulative incidence of HF (p = 0.003), nonfatal MI (p = 0.005), and URR (p = 0.031) (Fig. 3).
Table 2.
Adverse cardiovascular events according to the DAPA administration during follow-up
| Adverse Cardiovascular events | DAPA-free | DAPA | P value |
|---|---|---|---|
| n = 645 | n = 141 | ||
| MACE, n (%) | 118 (18.3) | 12 (8.5) | 0.018 |
| Overall death, n (%) | 9 (1.4) | 1 (0.7) | 0.440 |
| Heart failure, n (%) | 67 (10.4) | 3 (2.1) | < 0.001 |
| Non-fatal MI, n (%) | 76 (11.8) | 5 (3.5) | 0.001 |
| Non-fatal stroke, n (%) | 15 (2.3) | 0 (0) | 0.050 |
| URR, n (%) | 98 (15.2) | 11 (7.8) | 0.012 |
The MACE was defined as the composite of overall death, HF, non-fatal MI, non-fatal stroke, and URR
MACE major adverse cardiovascular events; MI myocardial infarction; URR unplanned repeat revascularization
Fig. 2.
Presentation of adverse cardiovascular events during follow-up
Fig. 3.
Cumulative incidence plots of MACE and each component of MACE stratified by the DAPA administration. A MACE; B overall death; C non-fatal stroke; D heart failure; E non-fatal MI; F URR. MACE: major adverse cardiovascular events; MI: myocardial infarction; URR: unplanned repeat revascularization.
DAPA administration at discharge was significantly associated with a lower risk of MACE in both univariate and multivariate Cox regression analyses (p < 0.05 for all models) (Table 3). Furthermore, considering each specific adverse event, DAPA administration was associated with the reduced risk of HF, nonfatal MI, and URR in both univariate and multivariate Cox regression analyses (Table 4).
Table 3.
Univariate and multivariate Cox proportional hazard analyses for the MACE according to the DAPA administration
| HR | 95% CI | P value | ||
|---|---|---|---|---|
| Model 1 | DAPA-free | Reference | ||
| DAPA | 0.470 | 0.259–0.851 | 0.013 | |
| Model 2 | DAPA-free | Reference | ||
| DAPA | 0.480 | 0.265–0.871 | 0.016 | |
| Model 3 | DAPA-free | Reference | ||
| DAPA | 0.440 | 0.233–0.833 | 0.012 | |
| Model 4 | DAPA-free | Reference | ||
| DAPA | 0.426 | 0.225–0.808 | 0.009 | |
| Model 5 | DAPA-free | Reference | ||
| DAPA | 0.422 | 0.223–0.800 | 0.008 | |
| Model 6 | DAPA-free | Reference | ||
| DAPA | 0.391 | 0.193–0.792 | 0.009 | |
| Model 7 | DAPA-free | Reference | ||
| DAPA | 0.388 | 0.192–0.785 | 0.008 | |
Model 1: Unadjusted
Model 2: Adjusted for age, sex
Model 3: Model 2 + smoking, hypertension, diabetes, cerebral infarction
Model 4: Model 3 + STEMI/NSTEMI + PCI details (stenting/POBA, multivessel disease or not)
Model 5: Model 4 + in-hospital AHF, in-hospital arhythmia
Model 6: Model 5 + HDL-C, LDL-C, TC, TG, AIP, TyG, CPK, CK-MB, HBDH, BNP, HbA1c
Model 7: Model 6 + β-block at discharge, ACEI/ARB at discharge, ARNI at discharge, MRA at discharge
Table 4.
Univariate and multivariate Cox proportional hazard analyses for adverse prognosis according to the DAPA administration
| Univariate analyses | Multivariate analyses | |||||||
|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | |||
| Heart failure | DAPA-free | Reference | Reference | |||||
| DAPA | 0.206 | 0.065–0.655 | 0.007 | 0.114 | 0.030–0.439 | 0.002 | ||
| Non-fatal MI | DAPA-free | Reference | Reference | |||||
| DAPA | 0.301 | 0.122–0.743 | 0.009 | 0.129 | 0.043–0.387 | < 0.001 | ||
| URR | DAPA-free | Reference | Reference | |||||
| DAPA | 0.514 | 0.276–0.959 | 0.036 | 0.172 | 0.075–0.394 | < 0.001 | ||
Multivariate analyses were based on model 7 in Table 3
MI myocardial infarction, URR unplanned repeat revascularization
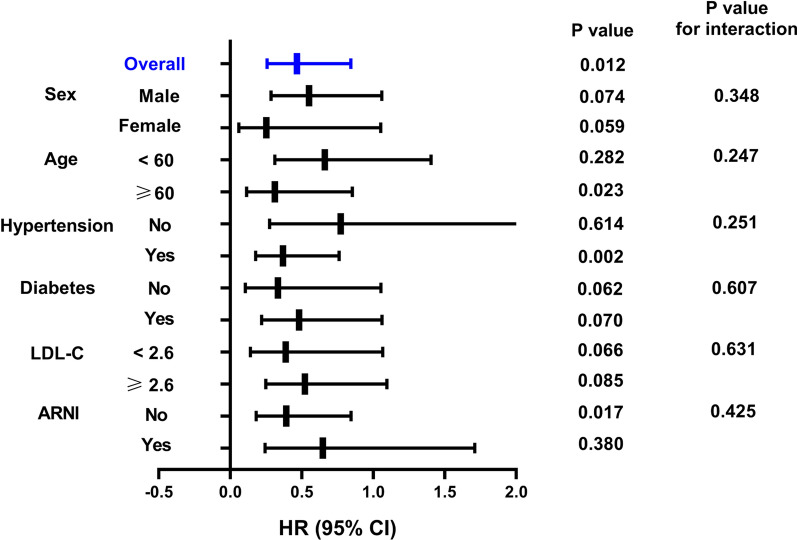
As shown in Fig. 4, when stratified by age, the occurrence rate of MACE in patients aged > 60 years in the DAPA group was 0.312-fold lower than that in the DAPA-free group (95% CI, 0.114–0.854, p = 0.023). In patients with hypertension, the risk of MACE in the DAPA group was 0.369-fold lower than that in the DAPA-free group (95% CI, 0.178–0.362, p = 0.002). The predictive values in patients without hypertension were not statistically significant. For patients without ARNI at discharge, the risk of MACE in the DAPA group was 0.392-fold lower than that in the DAPA-free group (95% CI, 0.182–0.845, p = 0.017). However, in the subgroup that received ARNI treatment, no statistically significant difference was observed with respect to the use of DAPA for predicting MACE. Besides, when stratified by sex, diabetes, or LDL-C levels, no significant differences in MACE were found between the DAPA and DAPA-free groups.
Fig. 4.
Subgroup analyses of DAPA for MACE
As AIP and the TyG index are associated with MACE in patients with AMI undergoing PCI [14, 15], the effects of DAPA administration on AIP and the TyG index 12 months after discharge were evaluated. As shown in Fig. 5, AIP and the TyG index in the DAPA group were significantly higher than those in the hospitalized DAPA-free group. After 12 months, AIP and the TyG index were significantly decreased with DAPA administration, particularly due to the effect of DAPA on AIP.
Fig. 5.
Effects of DAPA on TyG and AIP index. TyG (A) and AIP (B) index were calculated in hospital and 12 months post-discharge
Discussion
The present study was conducted to evaluate the association between DAPA intervention and MACE in patients with AMI undergoing PCI. The results showed that DAPA administration was associated with reduced MACE in patients with AMI, particularly in patients with advanced age and hypertension and in those who did not receive ARNI. Moreover, the study revealed that DAPA administration significantly decreased AIP and the TyG index 12 months after discharge.
Current treatment guidelines and expert consensus generally state that SGLT2i should be avoided whenever possible during acute progression, including in acute MI, to avoid hypovolemia, hypotension, ketoacidosis, or acute kidney injury. However, in clinical trials on acute and chronic HF, the risk of these adverse events in the SGLT2i treatment group was uncommon and not significantly higher than that in the placebo group [6, 16]. Another safety concern during the perioperative management of patients with AMI is the repeated use of angiographic contrast agents during PCI, which may cause contrast-associated acute kidney injury. Considering the effect of SGLT2i on the afferent arteriole tone, they may cause a small reduction in the glomerular filtration rate. However, there is sufficient evidence suggesting that SGLT2i stabilize long-term renal function in patients with T2DM, CKD, and HFrEF, thereby providing a rationale for their safe use in patients with underlying renal impairment during AMI [17, 18]. Based on the yet unclear relationship between SGLT2i and the prognosis of patients with AMI, 786 patients with AMI admitted for PCI in a single center who were followed-up after discharge were retrospective analyzed. The analysis revealed that the use of DAPA is biased toward patients with T2DM; however, early intervention with SGLT2i is still preferred for some non-T2DM patients with AMI in the acute phase. In addition, the study revealed that the use of DAPA is biased toward patients with more adverse cardiovascular factors, which to a certain extent suggests that patients with AMI with more underlying diseases are more suitable for early intervention with SGLT2i.
In the median follow-up of 23 months (follow-up is being continued), the reported cases of overall deaths and nonfatal stroke were few; thus, there was a lack of statistical significance between the DAPA and DAPA-free groups. Therefore, in the Cox subgroup analyses, overall deaths and nonfatal stroke were not analyzed separately. Kaplan–Meier survival and Cox regression analyses indicated that early intervention with DAPA could reduce the occurrence of total MACE events, HF, nonfatal MI, and URR. Studies have shown that advanced age and hypertension are highly correlated with MACE [19] and that early intervention with ARNI has a protective effect on the prognosis of patients with AMI, particularly in the prognosis of patients with AMI complicated with HFrEF [20]. In the present study, subgroup analysis further suggested that the early intervention of DAPA significantly reduces MACE events in patients with advanced age and hypertension or those who did not receive ARNI. Because this was a single-center study, the number of included cases is small and the retrospective analysis cannot avoid the interference of exposure factors. However, the study results provide some idea about the relationship between the early intervention of SGLT2i and prognosis of patients with AMI.
It has been shown that dapagliflozin improves micro- and macrovascular endothelial function compared to glibenclamide, regardless of glycemic control in patients with T2DM and subclinical carotid atherosclerotic disease [21] and ameliorates angiotensin II-induced cardiac remodeling by regulating the transforming growth factor-beta1/Smad signaling in a non-glucose-lowering dependent manner [22]. Moreover, dapagliflozin induces vasodilation in resistance-size mesenteric arteries by stimulating smooth muscle cell KV7 ion channels [23] and attenuates advanced glycation end product-induced inflammation and apoptosis through activating AMP-activated protein kinase- mammalian target of rapamycin mediated autophagy pathway in podocytes [24]. The mechanisms of the efficacy of SGLT2i in AMI include the attenuation of neurohormonal activation, cardiomyocyte necrosis, and reperfusion injury. In addition, coronary blood flow and ventricular load are improved by enhancing the endothelial function and vasodilation, thereby improving myocardial energy metabolism as well as contractility and other functions. The ultimate effect of SGLT2i is the reversal of cardiac enlargement, abnormal rhythm, and myocardial fibrosis and the improvement of heart failure. In addition to the heart, it can indirectly improve the cardiorenal axis and improve the prognosis of patients by decreasing the intraglomerular pressure and increasing erythropoietin production [25–28]. Considering that glucose and lipid metabolisms are closely associated with endothelial phenotype stability, myocardial fibrosis, and myocardial cell necrosis, changes in the TyG index and AIP, the two indicators related to glucose and lipid metabolisms, were tracked to reveal the possible scope of SGLT2i action. The results revealed that the use of DAPA at discharge significantly reduced the TyG index and AIP for up to 12 months. Although the two indices also decreased in the DAPA-free group, this may have occurred because of the action of statin. It is not difficult to infer from results shown in Fig. 3 that the effect of DAPA combined with statin is significantly better than that of statin alone. This suggests that the target of DAPA may not be limited to glucose metabolism but may also have regulatory effects on lipid metabolism. A recent study has shown that SGLT2i has no significant effect on plasma PCSK9 levels, suggesting that it is safe for a possible combination therapy in the future [29].
Limitations
First, this was a single center study based on the Chinese population, and DAPA was not validated in other populations. Second, long-term evaluation was not conducted. Third, the predictive value of DAPA based on the factors measured at discharge could not be determined. Finally, we did not perform propensity score matching due to the small sample size included.
Conclusions
DAPA was a reliable and independent protective factor against MACE in patients with AMI undergoing PCI.
Acknowledgements
Not applicable.
Author contributions
YZ drafted the manuscript. JLZ contributed to the case collection and database organization. XJY and LS were responsible for statistical analysis of the data. FFW and YJ contributed to the conception and design of this article. All authors read and approved the final manuscript.
Funding
This work was supported by the Changzhou Health and Wellness Committee Research Project (CQ20210122) and the Changzhou Health and Wellness Committee Research Project (ZD202112).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Committee of Clinical Investigation of The Affiliated Changzhou No.2 People’s Hospital of Nanjing Medical University (2020-KY253-01) and conducted in accordance with the guidelines of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yuan Ji, Email: jiyuan1213@aliyun.com.
Fang-fang Wang, Email: lightyearwff@163.com.
References
- 1.Upur H, Li JL, Zou XG, Hu YY, Yang HY, Abudoureyimu A, et al. Short and long-term prognosis of admission hyperglycemia in patients with and without diabetes after acute myocardial infarction: a retrospective cohort study. Cardiovasc Diabetol. 2022;21(1):114. doi: 10.1186/s12933-022-01550-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao Y, Lu X, Wan F, Gao L, Lin N, He J, et al. Disruption of circadian rhythms by shift work exacerbates reperfusion injury in myocardial infarction. J Am Coll Cardiol. 2022;79(21):2097–2115. doi: 10.1016/j.jacc.2022.03.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hashimoto Y, Ozaki Y, Kan S, Nakao K, Kimura K, Ako J, et al. Impact of chronic kidney disease on in-hospital and 3-year clinical outcomes in patients with acute myocardial infarction treated by contemporary percutaneous coronary intervention and optimal medical therapy—insights from the J-MINUET study. Circ J. 2021;85(10):1710–1718. doi: 10.1253/circj.CJ-20-1115. [DOI] [PubMed] [Google Scholar]
- 4.Sacre JW, Magliano DJ, Shaw JE. Clinical utility of cardiovascular risk scores for identification of people with type 2 diabetes more likely to benefit from either GLP-1 receptor agonist or SGLT2 inhibitor therapy. Diabetes care. 2022;45:1900. doi: 10.2337/dc21-1929. [DOI] [PubMed] [Google Scholar]
- 5.Wei W, Liu J, Chen S, Xu X, Guo D, He Y, et al. Sodium glucose cotransporter Type 2 inhibitors improve cardiorenal outcome of patients with coronary artery disease: a meta-analysis. Front Endocrinol. 2022;13:850836. doi: 10.3389/fendo.2022.850836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al Rifai M, Newby LK, Nair AP, Misra A, Rogers JG, Fedson S, et al. SGLT-2 inhibitors for patients with heart failure: what have we learned recently? Curr Atheroscler Rep. 2022;24(8):627–634. doi: 10.1007/s11883-022-01038-2. [DOI] [PubMed] [Google Scholar]
- 7.Sharma A, Ofstad AP, Ahmad T, Zinman B, Zwiener I, Fitchett D, et al. Patient phenotypes and SGLT-2 inhibition in type 2 diabetes: insights from the EMPA-REG OUTCOME trial. JACC Heart failure. 2021;9(8):568–577. doi: 10.1016/j.jchf.2021.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Kaku K, Wanner C, Anker SD, Pocock S, Yasui A, Mattheus M, et al. The effect of empagliflozin on the total burden of cardiovascular and hospitalization events in the Asian and non-Asian populations of the EMPA-REG OUTCOME trial of patients with type 2 diabetes and cardiovascular disease. Diabetes Obes Metab. 2022;24(4):662–674. doi: 10.1111/dom.14626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Furtado RHM, et al. Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose Cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus. Circulation. 2019;139(17):2022–2031. doi: 10.1161/CIRCULATIONAHA.118.038868. [DOI] [PubMed] [Google Scholar]
- 10.Yu J, Arnott C, Neuen BL, Heersprink HL, Mahaffey KW, Cannon CP, et al. Cardiovascular and renal outcomes with canagliflozin according to baseline diuretic use: a post hoc analysis from the CANVAS Program. ESC heart failure. 2021;8(2):1482–1493. doi: 10.1002/ehf2.13236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yu J, Li J, Leaver PJ, Arnott C, Huffman MD, Udell JA, et al. Effects of canagliflozin on myocardial infarction: a post hoc analysis of the CANVAS programme and CREDENCE trial. Cardiovasc Res. 2022;118(4):1103–1114. doi: 10.1093/cvr/cvab128. [DOI] [PubMed] [Google Scholar]
- 12.Wu Z, Cui H, Li W, Zhang Y, Liu L, Liu Z, et al. Comparison of three non-insulin-based insulin resistance indexes in predicting the presence and severity of coronary artery disease. Front Cardiovasc Med. 2022;9:918359. doi: 10.3389/fcvm.2022.918359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han K, Shi D, Yang L, Wang Z, Li Y, Gao F, et al. Prognostic value of systemic inflammatory response index in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Ann Med. 2022;54(1):1667–1677. doi: 10.1080/07853890.2022.2083671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu Z, Liu L, Wang W, Cui H, Zhang Y, Xu J, et al. Triglyceride-glucose index in the prediction of adverse cardiovascular events in patients with premature coronary artery disease: a retrospective cohort study. Cardiovasc Diabetol. 2022;21(1):142. doi: 10.1186/s12933-022-01576-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng Y, Li C, Yang J, Seery S, Qi Y, Wang W, et al. Atherogenic index of plasma for non-diabetic, coronary artery disease patients after percutaneous coronary intervention: a prospective study of the long-term outcomes in China. Cardiovasc Diabetol. 2022;21(1):29. doi: 10.1186/s12933-022-01459-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jhalani NB. Clinical Considerations for use of SGLT2 inhibitor therapy in patients with heart failure and reduced ejection fraction: a review. Adv Ther. 2022;39(8):3472–3487. doi: 10.1007/s12325-022-02169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thiele K, Rau M, Hartmann NK, Möller M, Möllmann J, Jankowski J, et al. Empagliflozin reduces markers of acute kidney injury in patients with acute decompensated heart failure. ESC Heart Failure. 2022;9(4):2233–2238. doi: 10.1002/ehf2.13955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vukadinović D, Abdin A, Anker SD, Rosano GMC, Mahfoud F, Packer M, et al. Side effects and treatment initiation barriers of sodium-glucose cotransporter 2 inhibitors in heart failure: a systematic review and meta-analysis. Eur J Heart Failure. 2022 doi: 10.1002/ejhf.2584. [DOI] [PubMed] [Google Scholar]
- 19.Martinez-Sanchez FD, Medina-Urrutia AX, Jorge-Galarza E, Martínez-Alvarado MDR, Reyes-Barrera J, Osorio-Alonso H, et al. Effect of metabolic control on recurrent major adverse cardiovascular events and cardiovascular mortality in patients with premature coronary artery disease. Results of the genetics of atherosclerotic disease study. Nutr Metab Cardiovas Dis: NMCD. 2022 doi: 10.1016/j.numecd.2022.06.0. [DOI] [PubMed] [Google Scholar]
- 20.She J, Lou B, Liu H, Zhou B, Jiang GT, Luo Y, et al. ARNI versus ACEI/ARB in reducing cardiovascular outcomes after myocardial infarction. ESC Heart Failure. 2021;8(6):4607–4616. doi: 10.1002/ehf2.13644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sposito AC, Breder I, Soares AAS, Kimura-Medorima ST, Munhoz DB, Cintra RMR, et al. Dapagliflozin effect on endothelial dysfunction in diabetic patients with atherosclerotic disease: a randomized active-controlled trial. Cardiovasc Diabetol. 2021;20(1):74. doi: 10.1186/s12933-021-01264-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Lin X, Chu Y, Chen X, Du H, Zhang H, et al. Dapagliflozin: a sodium-glucose cotransporter 2 inhibitor, attenuates angiotensin II-induced cardiac fibrotic remodeling by regulating TGFβ1/Smad signaling. Cardiovasc Diabetol. 2021;20(1):121. doi: 10.1186/s12933-021-01312-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hasan A, Menon SN, Zerin F, Hasan R. Dapagliflozin induces vasodilation in resistance-size mesenteric arteries by stimulating smooth muscle cell K(V)7 ion channels. Heliyon. 2022;8(5):e09503. doi: 10.1016/j.heliyon.2022.e09503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang L, Liang B, Li J, Zhang X, Chen H, Sun J, et al. Dapagliflozin alleviates advanced glycation end product induced podocyte injury through AMPK/mTOR mediated autophagy pathway. Cell Signal. 2022;90:110206. doi: 10.1016/j.cellsig.2021.110206. [DOI] [PubMed] [Google Scholar]
- 25.Mone P, Varzideh F, Jankauskas SS, Pansini A, Lombardi A, Frullone S, et al. SGLT2 Inhibition via empagliflozin improves endothelial function and reduces mitochondrial oxidative stres insights from frail hypertensive and diabetic patients. Hypertension (Dallas, Tex : 1979). 2022;79(8):1633–43. doi: 10.1161/HYPERTENSIONAHA.122.19586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moellmann J, Mann PA, Kappel BA, Kahles F, Klinkhammer BM, Boor P, et al. The SGLT2 inhibitor ertugliflozin modifies the signature of cardiac substrate metabolism and reduces cardiac mTOR-signaling, endoplasmic reticulum stress and apoptosis. Diabetes, Obes Metab. 2022 doi: 10.1111/dom.14814. [DOI] [PubMed] [Google Scholar]
- 27.Jiang K, Xu Y, Wang D, Chen F, Tu Z, Qian J, et al. Cardioprotective mechanism of SGLT2 inhibitor against myocardial infarction is through reduction of autosis. Protein Cell. 2022;13(5):336–359. doi: 10.1007/s13238-020-00809-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Antlanger M, Domenig O, Kaltenecker CC, Kovarik JJ, Rathkolb V, Müller MM, et al. Combined sodium glucose co-transporter-2 inhibitor and angiotensin-converting enzyme inhibition upregulates the renin-angiotensin system in chronic kidney disease with type 2 diabetes: Results of a randomized, double-blind, placebo-controlled exploratory trial. Diabetes Obes Metab. 2022;24(5):816–826. doi: 10.1111/dom.14639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tricò D, Raggi F, Distaso M, Ferrannini E, Solini A. Effect of empagliflozin on plasma proprotein convertase subtilisin/kexin type 9 (PCSK9) in patients with type 2 diabetes. Diabetes Res Clin Pract. 2022;190:109983. doi: 10.1016/j.diabres.2022.109983. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.