Abstract
FGF10, as an FGFR2b-specific ligand, plays a crucial role during cell proliferation, multi-organ development, and tissue injury repair. The developmental importance of FGF10 has been emphasized by the identification of FGF10 abnormalities in human congenital disorders affecting different organs and systems. Single-nucleotide variants in FGF10 or FGF10-involving copy-number variant deletions have been reported in families with lacrimo-auriculo-dento-digital syndrome, aplasia of the lacrimal and salivary glands, or lethal lung developmental disorders. Abnormalities involving FGF10 have also been implicated in cleft lip and palate, myopia, or congenital heart disease. However, the exact developmental role of FGF10 and large phenotypic heterogeneity associated with FGF10 disruption remain incompletely understood. Here, we review human and animal studies and summarize the data on FGF10 mechanism of action, expression, multi-organ function, as well as its variants and their usefulness for clinicians and researchers.
Keywords: Pulmonary diseases, Congenital diseases, FGF10 deficiency
Introduction
The fibroblast growth factor (FGF) signaling pathway plays an essential role in mammalian embryo formation and is crucial for mesenchymal-epithelial communication, contributing to the development of many different organs (Itoh, 2016). FGF signaling is also involved in maintaining biological homeostasis due to the regulation of metabolism and endocrine secretion (Hui et al., 2018). Disruption of the proper functioning of the FGF pathway can cause congenital disorders, metabolic diseases, or cancers (Ornitz & Itoh, 2015; Itoh, 2016).
One of the most important FGF ligands is fibroblast growth factor 10 (FGF10), which plays an essential role in airway branching (Jones, Chong & Bellusci, 2020), functioning of the cardiovascular system (Itoh et al., 2016), and development of the kidney, cecum, thymus, trachea, prostate, mammary gland, adipose tissue, and limb (Itoh, 2016). Pathogenic variants in FGF10 can cause craniofacial defects (Prochazkova et al., 2018), lung disorders (Vincent et al., 2019), myopia (Jiang et al., 2019), limb (Ohuchi et al., 2000) or genitourinary system anomalies (Milunsky et al., 2006), and heart defects (Itoh et al., 2016). Alterations in FGF10 have been associated with cancers, including breast or pancreatic cancer (Dankova et al., 2017; Ndlovu et al., 2018). Complete understanding of the developmental function of FGF10 and how its disruption influences the phenotype is an important but challenging task. Here, we systemize the current knowledge on FGF10, relevant for clinically- and research-focused scientists. We provide an insight into the significance of FGF10 in development by discussing its tissue-specific expression and related phenotypic spectrum in humans.
Survey Methodology
All manuscripts cited in this review were found and analyzed from the PubMed database (https://pubmed.ncbi.nlm.nih.gov/) using the following keywords: FGF family, FGF10 mutations, FGF10 diseases, FGF10 cancers, FGF10 expression, FGF10 role. Articles unrelated to FGF10-linked disorders in humans and mice were excluded.
FGF family and their mechanism of action
The FGF protein family consists of 22 members that, based on the differences in their biochemical nature, amino acid sequence, or evolutionary origin, are divided into seven subfamilies: FGF1, FGF4, FGF7, FGF8, FGF9, FGF11, and FGF19 (Itoh & Ornitz, 2008). Based on their mechanism of action, FGF subfamilies can be further classified as canonical, hormone-like, or intracellular FGFs (Itoh, 2010).
The activation of canonical FGFs depends on their binding to FGF receptors (FGFRs), mediated by heparan sulfate glycosaminoglycan (HSPG), leading to the formation of a ternary FGF-FGFR-HSPG complex on a cell surface (Esko & Selleck, 2002; Lindahl & Li, 2009). In contrast, hormone-like FGFs have a poor affinity for HSPG and require other co-receptors, Klotho proteins, for FGFR activation (Zhang et al., 2015; Prudovsky, 2021).
Canonical FGFs
Canonical FGFs constitute the largest group of FGFs, consisting of FGF1, FGF4, FGF7, FGF8, and FGF9 subfamilies (Giacomini et al., 2021). All but the FGF9 subfamilies are characterized by a paracrine/autocrine secretion mechanism (Imamura, 2014) and are crucial for the development of many organs, including glands and limbs (Zinkle & Mohammadi, 2019). In contrast, members of the FGF9 subfamily act only as paracrine factors and play an essential role in cardiac development and maintenance of cardiac homeostasis (Wang et al., 2018a; Khosravi et al., 2022).
Hormone-like FGFs
Members of the FGF19 subfamily belong to hormone-like FGFs that act as endocrine hormones (Dolegowska et al., 2019). The FGF19 family regulates glucose and lipid metabolism (Beenken & Mohammadi, 2009) by increasing hepatic glycogen synthesis, glucose tolerance, and insulin sensitivity and decreasing gluconeogenesis and hepatic triglyceride content (Fu et al., 2004). It is also essential for the enterohepatic circulation of bile or phosphorus and vitamin D3 homeostasis (Imamura, 2014; Dolegowska et al., 2019).
Intracellular FGFs
Intracellular FGFs from the FGF11 subfamily demonstrate FGFR-independent intracrine activity (Dolegowska et al., 2019). Members of the FGF11 subfamily are involved in neuronal development (Wiedlocha, Haugsten & Zakrzewska, 2021). They regulate voltage-gated sodium channel activity in neurons and are required for axon development, neuronal migration in the cerebral cortex, and microtubules stabilization (Wu et al., 2012; Zhang et al., 2012).
Activation of the FGF10 binding
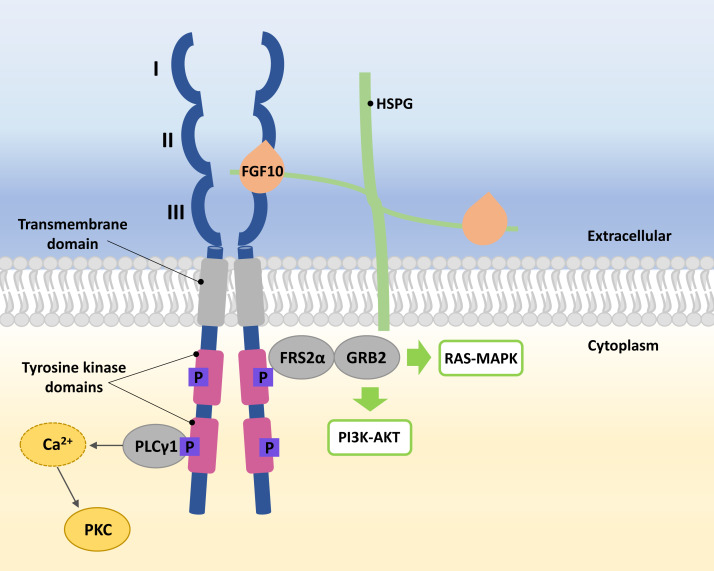
FGFRs are high-affinity trans-membrane surface tyrosine kinase receptors encoded in humans by the FGFR1, FGFR2, FGFR3, FGFR4, and FGFRL1 genes (Katoh & Nakagama, 2014). FGF10 binds specifically to epithelial FGFR2b, characterized by three domains, extracellular, transmembrane, and intracellular tyrosine kinase (Itoh, 2016; Xie et al., 2020). In the extracellular domain of FGFR2b, three immunoglobulin-like subdomains (I, II, and III) are distinguished, where II and III subdomains represent the sites of HSPG and FGF10 ligand binding (Fig. 1) (Itoh, 2016; Ferguson, Smith & Francavilla, 2021).
Figure 1. A simplified scheme of the FGF10/FGFR2b activation.
Numbers I-III indicate immunoglobulin-like subdomains of the FGFR2b extracellular domain, with the FGF10 ligand and HSPG binding sites between subdomains II and III. In the tyrosine kinase domains, the purple square box indicates the phosphorylation sites required for activation of the FGF receptor substrate 2 α (FRS2 α), growth factor receptor-bound protein 2 (GRB2) and phospholipase C gamma 1 (PLC γ1). After phosphorylation of PLC γ1, calcium is released and protein kinase C (PKC) is enabled. Activated FRS2 α and GRB2 lead to activation of RAS-MAPK and PI3K-AKT signaling pathways.
The FGF10 ligand binds to the FGFR2 through HSPG to initiate signaling (Watson & Francavilla, 2018). Ligand–receptor binding triggers dimerization of FGFR2b and phosphorylation of tyrosine residues within its intracellular domains, resulting in the FGFR2b activation (Belov & Mohammadi, 2013; Watson & Francavilla, 2018). Phosphorylated FGFR2b activates FGF receptor substrate 2 α (FRS2 α) and phospholipase C gamma 1 (PLC γ1) (Itoh, 2016; Watson & Francavilla, 2018). Whereas the activated FRS2α enables the recruitment of growth factor receptor-bound protein 2 (GRB2) (Ong et al., 2000; Watson & Francavilla, 2018), leading to the activation of Ras/Raf/mitogen-activated protein kinases (MAPKs) and phosphatidylinositol-3 kinase/protein kinase B (PI3K/AKT) (Ornitz & Itoh, 2015; Dai et al., 2022), PLC γ1 leads to the intracellular calcium release followed by the activation of protein kinase C (PKC) (Marchese et al., 2001; Itoh, 2016; Watson & Francavilla, 2018) (Fig. 1).
Modification of FGF10 signaling occurs through molecular cross-talk between FGF10/FGFR2b and Wnt, retinoic acid, or transforming growth factor β signaling pathways (Xie et al., 2020). Furthermore, the FGF10/FGFR2b pathway can be also regulated by several proteins that are co-expressed with FGF and can either inhibit or enhance the signaling (Fürthauer et al., 2001; Zhao & Zhang, 2001; Tsang et al., 2002; Watson & Francavilla, 2018; Chanda et al., 2019; Böttcher et al., 2004; Xie et al., 2020).
FGF10 expression
In a murine model, high Fgf10 expression was observed in the neural crest-derived mesenchyme of the forming salivary gland, mesenchyme of the developing epithelial bud of the lacrimal gland, and Harder’s gland (Makarenkova et al., 2000; Govindarajan et al., 2000; Teshima, Lourenco & Tucker, 2016).
FGF10 is expressed throughout the human lung parenchyma and partially in airway smooth muscle cells or vasculature from 10 to 21 weeks of gestation (Al Alam et al., 2015; Danopoulos et al., 2019). A constant level of FGF10 transcripts is persistent during the pseudoglandular phase of lung development and increases during the canalicular phase (Al Alam et al., 2015; Danopoulos et al., 2019). The spatial lung Fgf10 expression shows different patterns depending on the branching phases (Hirashima, Iwasa & Morishita, 2009). In the earliest stage of lung branching, elongation mode, Fgf10 expression occurs at a single site in the bud apex region in the axial direction of elongation (Hirashima, Iwasa & Morishita, 2009). During the terminal bifurcation mode, Fgf10 expression localizes into two sites between the bud apex and the lung border, while in the last stage, lateral budding, it appears at sites on either side of the stem where potential budding is located (Hirashima, Iwasa & Morishita, 2009).
FGF10 expression has also been observed in other organs, including human and mouse sclera (Lim et al., 2012) or developing human posterior colon and rectum (Yin et al., 2013). In addition, FGF10 RNA is considered an endogenous marker in the second heart field (Kelly, Brown & Buckingham, 2001).
Role of the FGF10 gene in human morphogenesis
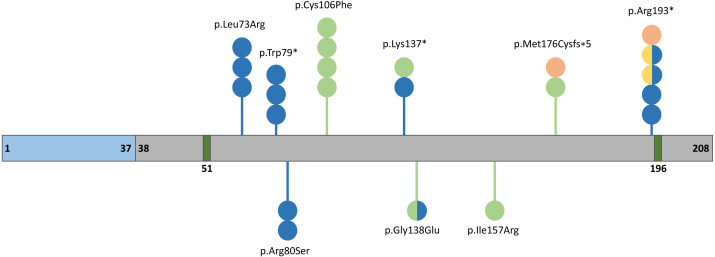
The human FGF10 gene spanning 89 kb consists of three coding exons and maps to the reverse strand of the 5p12 chromosome (Emoto et al., 1997). The FGF10 protein has 23.4 kDa composed of 208 amino acids and comprises a signal peptide (1-37 aa) and an FGF domain (38–208 aa) with two known glycosylation sites (51 and 196 aa) (Fig. 2) (Beenken & Mohammadi, 2009). The secreted FGF10 protein proceeds through the canonical endoplasmic reticulum-Golgi secretory pathway, after which the signal peptide is cleaved (Watson & Francavilla, 2018).
Figure 2. Schematic representation of the FGF10 protein.
Blue, grey, and dark green boxes indicate signal peptide, the FGF10 domain, and glycolysation sites, respectively. Variants identified in patients with lethal lung developmental disorders (LLDD), lacrimo-auriculo-dento-digital syndrome (LADD), aplasia of the lacrimal and salivary glands (ALSG), and risk of chronic obstructive pulmonary disease (COPD) are shown as lollipops and are represented in orange, light green, dark blue, and yellow, respectively. The number of circles in the lollipop represent a number of individuals with a particular variant and two-colored circles indicate patients affected by two different conditions.
The role of FGF10 begins in the gastrulation stage (Thiery et al., 2009). FGF10 is involved in the formation of lacrimal and salivary glands at the embryonic period (Prochazkova et al., 2018; Karasawa et al., 2022) by regulating the progenitor cell population and stimulating gland outgrowth (Chatzeli, Gaete & Tucker, 2017). In adults, FGF10 is critical in maintaining gland homeostasis and/or regeneration (Mauduit et al., 2022).
The FGF10/FGFR2b signaling is also required for lung development and is involved in the induction of several genes responsible for the branching of lung epithelial tubules and alveolar formation (Bellusci et al., 1997; Wang et al., 2018b; Yuan et al., 2018; Yang et al., 2021). In vitro studies have also indicated the involvement of the FGF10 signaling in fluid secretion (Graeff, Wang & McCray, 1999). It also promotes the growth of lung buds (Hines & Sun, 2014). The FGF10 gene initiates lung bud proliferation through mesenchymal-epithelial signaling via the B isoform of FGFR2 (Bellusci et al., 1997; Abler, Mansour & Sun, 2009).
During facial formation, Fgf10 is involved in the development of the palatal shelves, mandible, or teeth (Ohuchi et al., 2000; Prochazkova et al., 2018). It is also important in cranial development and eyelid (Prochazkova et al., 2018) or lens formation (Chaffee et al., 2016). FGF10 is essential for the proliferation of hepatoblasts (Berg et al., 2007), regulation of radial glial cell differentiation, controlling the number of progenitor cells and neurons (Sahara & O’Leary, 2009), adipogenesis (Sakaue et al., 2002), and heart repair mechanisms (Rochais et al., 2014).
Role of FGF10 in diseases
Pathogenic variants in FGF10 can lead to congenital disorders involving the respiratory system as well as the lacrimal and salivary glands (Fig. 2, Table 1) (Vincent et al., 2019). In addition, a number of single-nucleotide variants (SNVs) within FGF10 have been associated with the increased risk of nonsyndromic cleft lip with or without cleft palate (NSCL/P) (Yu et al., 2017), chronic obstructive pulmonary disease (COPD) (Klar et al., 2011; Sun et al., 2021) and myopia (Jiang et al., 2021) (Table 2).
Table 1. List of the coding variants within FGF10 identified in patients with lethal lung developmental disorders, lacrimo-auriculo-dento-digital syndrome, and aplasia of the lacrimal and salivary glands.
| Genetic findings | Diseases | References |
|---|---|---|
| c.577C>T | ALSG, CAD, risk of COPD | Entesarian et al. (2005), Karolak et al. (2019) and Klar et al. (2011) |
| c.467T>G | LADD | Milunsky et al. (2006) |
| c.409A>T | ALSG, LADD | Milunsky et al. (2006) |
| c.240A>C | ALSG | Entesarian et al. (2007) |
| c.413G>A | ALSG, LADD | Entesarian et al. (2007) |
| c.317G>T | LADD | Rohmann et al. (2006) |
| c.237G>A, | ALSG | Seymen et al. (2017) |
| c.526 del | LADD, AcDys | Karolak et al. (2019) |
| c.218T>G | ALSG | Rodrigo et al. (2018) |
| c.68_70del | Risk of CTD | Zhou et al. (2020) |
Notes.
- ALSG
- aplasia of the lacrimal and salivary glands
- LADD
- lacrimo-auriculo-dento-digital syndrome
- AcDys
- acinar dysplasia
- CAD
- congenital alveolar dysplasia
- COPD
- chronic obstructive pulmonary disease
- CTD
- conotruncal defects
Table 2. List of single nucleotide variants identified in FGF10 associated with the risk of nonsyndromic cleft lip with or without cleft palate, chronic obstructive pulmonary disease and myopia.
| Genetic findings | Disease | References |
|---|---|---|
| rs2973644 | risk of COPD | Ren et al. (2013) |
| rs1011814 | risk of COPD | Ren et al. (2013) |
| rs980510 | risk of COPD | Smith et al. (2018) |
| rs10512844 | risk of COPD | Smith et al. (2018) |
| rs10462065 | NSCL/P | Yu et al. (2017) |
| rs10473352 | risk of COPD | Ren et al. (2013) |
| rs339501 | Risk of extreme/high myopia | Hsi et al. (2013) |
| rs12517396 | Risk of extreme/high myopia | Jiang et al. (2019) |
| rs10941679 | Risk of breast cancer | Stacey et al. (2008) |
Notes.
- COPD
- chronic obstructive pulmonary disease
- NSCL/P
- nonsyndromic cleft lip with or without cleft palate
Lacrimo-auriculo-dento-digital syndrome and aplasia of lacrimal and salivary glands
Lacrimo-auriculo-dento-digital syndrome (LADD; MIM#149730) and aplasia of the lacrimal and salivary glands (ALSG; MIM #180920) are rare genetic diseases manifesting with variable expression and inherited in an autosomal dominant manner (Milunsky et al., 2006; Ryu et al., 2020). LADD and ALSG belong to the same phenotypic spectrum; however, LADD patients present a more severe phenotype than individuals with ALSG (Milunsky et al., 2006; Rohmann et al., 2006). In addition to characteristic features observed in both LADD and ALSG patients, including dryness and infections of the eyes and mouth as well as dental caries due to atresia or hypoplasia of the lacrimal and salivary glands (Milunsky et al., 2006; Seymen et al., 2017), patients affected with LADD syndrome often present with facial dysmorphism with ear underdevelopment and hearing loss, anomalies of fingers and toes, kidneys, gastrointestinal symptoms, or respiratory disorders (Ryu et al., 2020). Interestingly, both LADD syndrome and ALSG have a large variability of associated symptoms, even when patients are from the same family and have the same genetic background, making phenotype-genotype correlation challenging (Shams et al., 2007).
LADD syndrome and ALSG are caused by heterozygous SNVs or copy-number variant (CNV) deletions involving the FGF10 gene (Rohmann et al., 2006; Shams et al., 2007). LADD can also be associated with changes affecting FGFRs, FGFR2 and FGFR3 (Rohmann et al., 2006; Shams et al., 2007). In contrast to gain-of-function FGFR2 variants associated with craniosynostosis, LADD-related variants usually lead to a decrease in the activity of FGF10 signaling (Shams et al., 2007).
An ALSG-associated variant c.577C>T (p.Arg193*) in FGF10 was first described in 2005 (Entesarian et al., 2005). A missense variant c.467T>G (p.Ile156Arg) and a heterozygous variant c.409A>T (p.Lys137*) in FGF10 were described in two unrelated LADD patients (Milunsky et al., 2006). In one proband, the pathogenic variant was inherited from her mother with ALSG (Milunsky et al., 2006). A year later, the c.240A>C (p.Arg80Ser) variant was identified in a son and father, both affected by ALSG (Entesarian et al., 2007). A missense de novo variant c.413G>A (p.Gly138Glu) was also detected in patient with ALSG associated with anomalies in the genitourinary system and coronal hypospadias, demonstrating clinical overlap between ALSG and LADD syndrome (Entesarian et al., 2007). The c.218T>G (p.Leu73Arg) variant in FGF10 was reported in three individuals with ALSG from the same family (Rodrigo et al., 2018).
A 53 kb deletion removing exons 2 and 3 of FGF10 was identified in two families with ALSG (Entesarian et al., 2005). Recently, a novel heterozygous 12,158 bp deletion involving the last two exons of the FGF10 gene was identified in a large family with members affected by LADD or pulmonary hypoplasia (Wade et al., 2021).
Based on the molecular findings and association of FGF10 with LADD and ALSG phenotypes it has been postulated that ALSG is a milder form of LADD and not a separate disease entity (Seymen et al., 2017). It is also possible that variable expressivity of FGF10 variants results from other cis or trans genetic variants (Milunsky et al., 2006).
Phenotypes of mice with Fgf10+/− deficiency partially recapitulate the phenotypes observed in humans with FGF10 abnormalities (Entesarian et al., 2005). For example, adult Fgf10+/− mice have shown aplasia of lacrimal glands and hypoplasia of salivary glands, similar to the characteristic features observed in ALSG patients (Entesarian et al., 2005).
Lethal lung developmental disorders (LLDD)
Lethal lung developmental disorders (LLDDs) are rare diseases of newborns, characterized by severe respiratory failure, refractory to treatment (Vincent et al., 2019). LLDDs include alveolar capillary dysplasia with misalignment of pulmonary veins (ACDMPV) that is mainly caused by changes within the FOXF1 locus, and acinar dysplasia (AcDys), congenital alveolar dysplasia (CAD), or primary pulmonary hypoplasia (PH) (Vincent et al., 2019). Recent studies have shown that 45% and 20% of AcDys, CAD, or PH is associated with heterozygous SNVs or CNVs involving TBX4 and FGF10, respectively (Vincent et al., 2019). Moreover, a homozygous variant c.764G>A (p.Arg255Gln) in FGFR2 was reported in a neonate with AcDys accompanied by ectrodactyly and inherited from consanguineous parents (Barnett et al., 2016). A heterozygous FGF10 variant c.526del (p.Met176Cysfs*5) has been identified in a patient with AcDys (Karolak et al., 2019). Interestingly, the variant c.577C>T (p.Arg193*), previously detected in a family with ALSG syndrome (Entesarian et al., 2005), was also found in a patient with CAD (Karolak et al., 2019). Additionally, in two unrelated families, patients with severe lethal PH were found to have a heterozygous deletion in 5p12 (∼2.18 Mb and ∼2.32 Mb in size), involving FGF10, inherited from their parents with LADD syndrome who had no evidence of lung disease (Karolak et al., 2019). A similar phenomenon was observed in a Dutch family, in which a proband with PH inherited a heterozygous deletion involving the FGF10 gene from a mother with LADD syndrome (Wade et al., 2021).
The observation of various phenotypes in a single family with the same FGF10 variant suggests a complex model of inheritance (Karolak et al., 2019). It was postulated that haploinsufficiency of FGF10 alone is not sufficient to induce AcDys or CAD, but requires additional genetic modifiers, such as, e.g., non-coding variants (inherited or de novo; rare or common) in regulatory elements (Karolak et al., 2019). Interestingly, in the study described by Karolak et al., all infants with lung disease and coding variants in the FGF10 gene also had at least one non-coding SNV within the lung-specific enhancer ∼70 kb upstream of TBX4 (Karolak et al., 2019).
The lung phenotypes observed in patients with mutations in FGF10 were similar to that observed in mice with FGF10 abnormalities. Homozygous knockout of Fgf10 leads to a severe lung phenotype in mice and to death shortly after birth due to impaired lung morphogenesis (Min et al., 1998; Sekine et al., 1999). Mice without functional Fgfr2 die around implantation, whereas mice deficient in Fgfr2 isoform IIIb survive until birth but die shortly after due to the lack of lungs (Arman et al., 1998; Arman et al., 1999; De Moerlooze et al., 2000). The same lethal phenotype observed in Fgf10−/− and Fgfr2b−/− indicates that FGF10 is active as a specific ligand for FGFR2b (Ohuchi et al., 2000).
Chronic obstructive pulmonary disease (COPD)
COPD is characterized by abnormalities in the lung epithelium and airspace (Klar et al., 2011), which contributes to irreversible and progressive changes in airflow with an impaired response to pathogens (Tashkin et al., 1996; Rabe et al., 2007). About 26% of individuals with defects in airway development have been found to have an increased risk of COPD (Prince, 2018). Therefore, genetic factors may be important in the etiology of this disorder (Molfino, 2004).
A study of two Swedish ALSG/LADD families, including twelve affected members with the heterozygous 53 kb deletion (n = 10) or c.577C>T (p.Arg193*) variant (n = 2) involving FGF10 (Entesarian et al., 2005), showed that haploinsufficiency of FGF10 is associated with compromised lung function and likely a risk factor for COPD (Klar et al., 2011). Another study performed in the Han Chinese population of North China revealed the apparent association of the rs2973644 and rs10473352 variants in FGF10 with COPD, and suggested that rs1011814 might be responsible for the severity of COPD (Ren et al., 2013). Additionally, recent analyses showed that FGF10 variants rs980510 and rs10512844 are associated with the absence of the proper medial-basal airway in smokers, increasing the COPD risk in these individuals (Smith et al., 2018).
Fgf10+/− mice showed reduced lung function similar to that in patients with heterozygous mutations in FGF10 and COPD risk. However, this phenotype may result from the smaller size of Fgf10+/− mice compared to wild-type animals (Klar et al., 2011). Fgf10 expression also occurs in murine airway smooth muscle cells (ASMCs) (Chu et al., 2021). After an injury, the transient expression of Fgf10 in ASMCs may be abnormal for adequate airway epithelial regeneration, and sustained secretion of Fgf10 by ASMCs can cause airway abnormalities resembling the defects observed in human COPD (Chu et al., 2021).
Cleft lip and palate syndrome
Nonsyndromic cleft lip with or without cleft palate (NSCL/P) are common birth defects of complex etiology, occurring in about 1/1000 live births worldwide (Dixon et al., 2011). While environmental factors influence the development of this disorder, it has been suggested that genetic causes also contribute to the formation of cleft lip and palate (CLP) (Riley et al., 2007). FGF10 is one of the members of the FGF family whose signaling pathway is important in craniofacial development and its abnormalities have been associated with clefts in the craniofacial region (Riley et al., 2007). Family-based association testing in the Philippine population with NSCL/P showed borderline significance for two markers: rs1448037 and rs1482685 in FGF10 (Riley et al., 2007). In contrast, subsequent studies conducted in the Polish population did not show any relationship between the cleft lip and palate and the rs1448037 variant in FGF10 (Mostowska et al., 2010). The variant rs10462065, located in proximity to FGF10, was recognized as a possible risk factor for CLP in the Chinese population (Yu et al., 2017). Another study performed in the Chinese population showed a correlation between rs2330542 in FGF10 and rs1946295 in TBX5, or rs7704166 in FGF10 and rs7085073 in FGFR2 that may be etiologically associated with NSCL/P. However, functional studies should be performed to clarify these statistically significant associations (Li et al., 2019). Further evidence indicating that abnormalities in FGF10 can contribute to the development of cleft palate was the identification of a deletion in the intron of FGF10 (chr5:44,347,532-44,347,538) in affected patients (Shi et al., 2009).
Mice studies support the role of FGF10 in the development of CLP in humans.
Fgf10−/− murine mutants show a complete cleft of the secondary palate caused by improper tongue attachment to the anterior palatal shelves and the middle and posterior mandible (Riley et al., 2007). SHH protein has been suggested to stimulate mesenchymal proliferation and was proposed to be a downstream target for the FGF10/FGFR2 pathway (Rice et al., 2004). Abnormal signaling of this epithelial-mesenchymal pathway leads to the development of cleft palate in mice (Rice et al., 2004). Inactivation of Shh in mouse palatal epithelium resulted in a cleavage phenotype resembling that observed in Fgfr10−/− and Fgfr2b−/− animals (Rice et al., 2004). Furthermore, the SHH activation affects the FGFR2 signaling during human craniofacial development (Raju et al., 2021). Thus, disruption of this pathway in humans may also contribute to palate defects.
Myopia
Myopia is one of the most common eye abnormalities identified in humans (Holden et al., 2016). High myopia, characterized by refractive error (RE) ≤ -6 diopters (D) or axial length (AL) ≥ 26 mm (Kempen et al., 2004; Pan, Ramamurthy & Saw, 2012), and extreme myopia, with RE ≤−10.00 D or AL ≥ 30 mm, can lead to pathological changes in the eye, and disturbing vision (Jiang et al., 2019). High myopia can cause glaucoma, retinal detachment, or macular degeneration, resulting in visual impairment (Saw et al., 2005; Jiang et al., 2019). The incidence of myopia varies between populations and gender and also depends on the patient’s age (Rose et al., 2008; Pan, Ramamurthy & Saw, 2012; Hsi et al., 2013).
The rs339501-G allele of FGF10 is a binding site for three different transcription factors and has been identified as a putative risk marker for extreme myopia in the Chinese population living in Taiwan (Hsi et al., 2013). The reporter assay showed that the G risk allele may result in a higher expression of FGF10, suggesting that increased FGF10 expression might enhance susceptibility to myopia (Hsi et al., 2013). However, a study performed in the Japanese population contradicted the findings of these studies in the Chinese population, showing that the rs339501-A is an extreme myopia risk allele (Yoshida et al., 2013). Although initial studies revealed an association of rs399501 with extreme myopia (Hsi et al., 2013), recent analyses showed that rs399501 is also significantly related to high myopia in Han Chinese (Jiang et al., 2021). Additionally, in a Japanese population, it was found that the rs12517396-C and rs10462070-A alleles in FGF10 may be associated with extreme myopia (Yoshida et al., 2013). A subsequent study in a western Chinese population confirmed the association of the rs12517396 and rs10462070 variants in extreme and high myopia (Jiang et al., 2019).
Interestingly, another variant, rs2973644, correlated with a higher risk for myopia (Sun et al., 2019), was also linked with a higher risk for COPD, as mentioned above (Ren et al., 2013). The rs2973644, together with the rs399501 and rs79002828 variants, indicated a risk of high myopia in young Chinese children (Sun et al., 2019). Furthermore, the G risk allele rs2973644 leads to an increase in FGF10 expression as opposed to the protective A allele (Sun et al., 2019).
Bronchopulmonary dysplasia
Bronchopulmonary dysplasia (BPD) is characterized by respiratory failure, lung collapse, or hypoxemia, caused by a deficiency of surfactant coating the inner surface of the lungs due to abnormal lung development during the saccular stage (Coalson, 2003)
It has been shown that activation of Toll-like receptor 2 (TLR2) or Toll-like receptor 4 (TLR4) in mice inhibits the FGF10 expression, resulting in impaired airway morphogenesis (Benjamin et al., 2007) with abnormal myofibroblast positioning at the saccular airway observed in BPD (Benjamin et al., 2007). A subsequent study showed that soluble inflammatory mediators in the tracheal fluid of earlier-born children, through NF- κB, can also inhibit the FGF10 expression resulting in defects in epithelial-mesenchymal interactions during lung development (Benjamin et al., 2010; Carver et al., 2013).
Interestingly, hyperoxia-induced neonatal lung injury was used as a mouse model of BPD to study the effect of Fgf10 deficiency in Fgf10+/− pups (Chao et al., 2017). In normoxia, no mortality was observed in either Fgf10+/+ or Fgf10+/− mice, while in hyperoxia, all Fgf10+/− mice died within 8 days, and all Fgf10+/+ mice were alive (Chao et al., 2017). Analysis of hyperoxic Fgf10+/− lungs showed increased hypoalveolarization and a lower ratio of type II alveolar epithelial cells (AECII) to total Epcam-positive cells compared to lungs in normoxia (Chao et al., 2017). Lower levels of Fgf10 transcripts lead to congenital lung defects with postnatal survival but reduced ability to cope with sublethal hypertoxic injury (Chao et al., 2017). Thus, deficiency of AECII cells caused by decreased level of FGF10 may be an additional complication in BPD patients (Chao et al., 2017). Furthermore, the lungs of Fgf10+/− mice with hyperoxia were characterized by a decreased number of blood vessels with an increase of poorly muscularized vessels (Chao et al., 2019). This may represent an additional feature of the BPD (Chao et al., 2019). However, a recent study showed that overexpression of Fgf10 and administration of rFGF10 rescued alveologenesis defects in transgenic mice (Taghizadeh et al., 2022).
Cancer
FGF10 activates intracellular signaling pathways in several cell types that can lead to cancer cell invasion and proliferation (Watson & Francavilla, 2018). Thus, abnormal regulation of FGF10 may contribute to certain forms of cancer (Itoh, 2016).
Pancreatic cancer is a common exocrine neoplasm and one of the most deadly diseases (Ndlovu et al., 2018). In a physiological state, FGF10 is involved in the formation of pancreatic epithelial cells (Bhushan et al., 2001; Ndlovu et al., 2018) and maintains undifferentiated pancreatic progenitor cells (Norgaard, Jensen & Jensen, 2003). In contrast, abnormal expression of the FGF7 and FGF10 genes in stromal cells surrounding pancreatic cancer cells have been observed (Ndlovu et al., 2018), indicating the role of FGF7 and FGF10 in cell proliferation (FGF7), migration, and invasion (FGF10) (Ndlovu et al., 2018). Moreover, ectopic expression of FGF10 can cause pancreatic hyperplasticity (Norgaard, Jensen & Jensen, 2003).
FGF10 may also be involved in a subset of human breast cancers (Stacey et al., 2008; Reintjes et al., 2013; Ghoussaini et al., 2016). Studies performed in 2008 identified rs4415084 and rs10941679 variants located approximately 274–317 kb downstream from FGF10 as likely associated with a higher risk of breast cancer (Stacey et al., 2008). While rs4415084 was subsequently excluded from breast cancer causality, the rs10941679-G allele has been associated with a 15% higher risk of estrogen-receptor-positive breast cancer (Ghoussaini et al., 2016). This variant maps to a putative enhancer interacting with the FGF10 promoter regions in breast cancer cell lines, suggesting that it could regulate the FGF10 expression (Stacey et al., 2008; Reintjes et al., 2013; Ghoussaini et al., 2016). Interestingly, FGF10 had strongly increased expression in 10% of breast cancers compared to healthy tissues (Theodorou et al., 2004).
Deregulation of FGF10-related signaling pathways was also associated with gastric cancer (Carino et al., 2021). This assumption was further supported by Wu et al., who indicated that regulatory networks involving FGF10 play an essential role in gastric cancer proliferation, migration, and invasion (Wu, Liu & Zhang, 2022).
Other diseases
Because of its role in orchestrating various developmental processes, abnormalities in FGF10 have also been described in the context of other disorders. However, the importance of FGF10 in these diseases is inconclusive and further studies are required to determine the impact of the FGF10 impairment on some defects.
Among diseases in which the role of FGF10 was not well established are conotruncal defects (CTDs), rare heart diseases with an incidence of 0.1 ‰ in live births that account for ∼25–30% of all non-syndromic congenital heart diseases (Shah et al., 2008; Zhou et al., 2020). Zhou et al. identified two rare heterozygous variants c. 29G>A and c.551G>A in FGF8 in two patients with tetralogy of Fallot and one c.68_70del variant in FGF10 in a patient with complete atrioventricular valve defect, pulmonary valve stenosis, single atrium, and single ventricle (Zhou et al., 2020). Whereas c.29G>A (p.Cys10Ter) in FGF8 and c.68_70del (p.Cys23del) in FGF10 may affect the protein function by reducing their secretion, c.551G>A (p.Arg184His) in FGF8 can negatively impact the proliferation of human cardiomyocytes, leading to CTD (Zhou et al., 2020). However, these assumptions have not been confirmed in subsequent studies.
Another condition that requires further research on FGF10 is anorectal malformation (ARM), including congenital malformations that affect the development of the distal colon (Krüger et al., 2008). Approximately 40–50% of all ARM cases have isolated ARMs, sometimes linked with malformations in the kidneys, the genitourinary system, or other systems (Stoll et al., 2007). The remaining ARM cases are associated with the spectrum of specific genetic syndromes (Draaken et al., 2012). Of note, changes in the FGFR2 gene involved in the FGF10 signaling are known to cause various forms of autosomal dominant craniosynostosis syndrome (Draaken et al., 2012). They are also associated with ARM in patients with Apert syndrome, Pfeiffer syndrome types 1 and 2, Crouzon syndrome, and Beare-Stevenson syndrome (Draaken et al., 2012).
Genetic studies have not confirmed the impact of variants in FGF10 and other genes on ARM development in the screened patients (Krüger et al., 2008; Draaken et al., 2012). However, the lack of association between ARM and FGF10 variants could be the result of a limited number of tested samples or the use of a method that was unable to detect variants in the previously unknown regulatory sequences or non-coding sequences (Draaken et al., 2012). FGF10 is likely a key factor regulating the growth in endoderm or mesenchyme and thus also stimulates the development of the genitourinary system and the anus (Yucel et al., 2004; Fairbanks et al., 2004). Future research should be extended to include additional factors within the WNT/FGF signaling pathway (Draaken et al., 2012).
Summary
FGF10 has diverse functions in organ development and their proper functioning and its alterations have been found to lead to various diseases in humans. Despite advances in understanding the pathways involved in FGF10 regulation and the discovery of new pathogenic variants in the FGF10 gene, there are still many unknowns regarding the exact role of FGF10 abnormalities in the disease etiology. Further studies of the FGF10 gene and its regulatory elements are necessary to expand our knowledge of the involvement of this gene in human diseases.
Acknowledgments
We thank Prof. Paweł Stankiewicz for helpful discussion.
Funding Statement
This work was supported by the grant awarded by the National Science Centre in Poland 2019/35/D/NZ5/02896 (Justyna A. Karolak). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Katarzyna Bzdega conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the article, and approved the final draft.
Justyna A. Karolak conceived and designed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the article, and approved the final draft.
Data Availability
The following information was supplied regarding data availability:
This is a literature review article.
References
- Abler, Mansour & Sun (2009).Abler LL, Mansour SL, Sun X. Conditional gene inactivation reveals roles for Fgf10 and Fgfr2 in establishing a normal pattern of epithelial branching in the mouse lung. Developmental Dynamics. 2009;238:1999–2013. doi: 10.1002/dvdy.22032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Alam et al. (2015).Al Alam D, El Agha E, Sakurai R, Kheirollahi V, Moiseenko A, Danopoulos S, Shrestha A, Schmoldt C, Quantius J, Herold S, Chao C-M, Tiozzo C, De Langhe S, Plikus MV, Thornton M, Grubbs B, Minoo P, Rehan VK, Bellusci S. Evidence for the involvement of fibroblast growth factor 10 in lipofibroblast formation during embryonic lung development. Development. 2015;142:4139–4150. doi: 10.1242/dev.109173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arman et al. (1998).Arman E, Haffner-Krausz R, Chen Y, Heath JK, Lonai P. Targeted disruption of fibroblast growth factor (FGF) receptor 2 suggests a role for FGF signaling in pregastrulation mammalian development. Proceedings of the National Academy of Sciences of the United States of America. 1998;95:5082–5087. doi: 10.1073/pnas.95.9.5082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arman et al. (1999).Arman E, Haffner-Krausz R, Gorivodsky M, Lonai P. Fgfr2 is required for limb outgrowth and lung-branching morphogenesis. Proceedings of the National Academy of Sciences of the United States of America. 1999;96:11895–11899. doi: 10.1073/pnas.96.21.11895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett et al. (2016).Barnett CP, Nataren NJ, Klingler-Hoffmann M, Schwarz Q, Chong C-E, Lee YK, Bruno DL, Lipsett J, McPhee AJ, Schreiber AW, Feng J, Hahn CN, Scott HS. Ectrodactyly and lethal pulmonary acinar dysplasia associated with homozygous FGFR2 mutations identified by exome sequencing. Human Mutation. 2016;37:955–963. doi: 10.1002/humu.23032. [DOI] [PubMed] [Google Scholar]
- Beenken & Mohammadi (2009).Beenken A, Mohammadi M. The FGF family: biology, pathophysiology and therapy. Nature Reviews. Drug Discovery. 2009;8:235–253. doi: 10.1038/nrd2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellusci et al. (1997).Bellusci S, Grindley J, Emoto H, Itoh N, Hogan BL. Fibroblast growth factor 10 (FGF10) and branching morphogenesis in the embryonic mouse lung. Development. 1997;124:4867–4878. doi: 10.1242/dev.124.23.4867. [DOI] [PubMed] [Google Scholar]
- Belov & Mohammadi (2013).Belov AA, Mohammadi M. Molecular mechanisms of fibroblast growth factor signaling in physiology and pathology. Cold Spring Harbor Perspectives in Biology. 2013;5:a015958. doi: 10.1101/cshperspect.a015958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin et al. (2010).Benjamin JT, Carver BJ, Plosa EJ, Yamamoto Y, Miller JD, Liu J-H, Van der Meer R, Blackwell TS, Prince LS. NF-kappaB activation limits airway branching through inhibition of Sp1-mediated fibroblast growth factor-10 expression. Journal of Immunology. 2010;185:4896–4903. doi: 10.4049/jimmunol.1001857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin et al. (2007).Benjamin JT, Smith RJ, Halloran BA, Day TJ, Kelly DR, Prince LS. FGF-10 is decreased in bronchopulmonary dysplasia and suppressed by Toll-like receptor activation. American Journal of Physiology. Lung Cellular and Molecular Physiology. 2007;292:L550–L558. doi: 10.1152/ajplung.00329.2006. [DOI] [PubMed] [Google Scholar]
- Berg et al. (2007).Berg T, Rountree CB, Lee L, Estrada J, Sala FG, Choe A, Veltmaat JM, DeLanghe S, Lee R, Tsukamoto H, Crooks GM, Bellusci S, Wang KS. Fibroblast growth factor 10 is critical for liver growth during embryogenesis and controls hepatoblast survival via beta-catenin activation. Hepatology. 2007;46:1187–1197. doi: 10.1002/hep.21814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhushan et al. (2001).Bhushan A, Itoh N, Kato S, Thiery JP, Czernichow P, Bellusci S, Scharfmann R. Fgf10 is essential for maintaining the proliferative capacity of epithelial progenitor cells during early pancreatic organogenesis. Development. 2001;128:5109–5117. doi: 10.1242/dev.128.24.5109. [DOI] [PubMed] [Google Scholar]
- Böttcher et al. (2004).Böttcher RT, Pollet N, Delius H, Niehrs C. The transmembrane protein XFLRT3 forms a complex with FGF receptors and promotes FGF signalling. Nature Cell Biology. 2004;6:38–44. doi: 10.1038/ncb1082. [DOI] [PubMed] [Google Scholar]
- Carino et al. (2021).Carino A, Graziosi L, Marchianò S, Biagioli M, Marino E, Sepe V, Zampella A, Distrutti E, Donini A, Fiorucci S. Analysis of gastric cancer transcriptome allows the identification of histotype specific molecular signatures with prognostic potential. Frontiers in Oncology. 2021;11:663771. doi: 10.3389/fonc.2021.663771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver et al. (2013).Carver BJ, Plosa EJ, Stinnett AM, Blackwell TS, Prince LS. Interactions between NF- κB and SP3 connect inflammatory signaling with reduced FGF-10 expression. The Journal of Biological Chemistry. 2013;288:15318–15325. doi: 10.1074/jbc.M112.447318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaffee et al. (2016).Chaffee BR, Hoang TV, Leonard MR, Bruney DG, Wagner BD, Dowd JR, Leone G, Ostrowski MC, Robinson ML. FGFR and PTEN signaling interact during lens development to regulate cell survival. Developmental Biology. 2016;410:150–163. doi: 10.1016/j.ydbio.2015.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanda et al. (2019).Chanda D, Otoupalova E, Smith SR, Volckaert T, De Langhe SP, Thannickal VJ. Developmental pathways in the pathogenesis of lung fibrosis. Molecular Aspects of Medicine. 2019;65:56–69. doi: 10.1016/j.mam.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao et al. (2019).Chao C-M, Moiseenko A, Kosanovic D, Rivetti S, El Agha E, Wilhelm J, Kampschulte M, Yahya F, Ehrhardt H, Zimmer K-P, Barreto G, Rizvanov AA, Schermuly RT, Reiss I, Morty RE, Rottier RJ, Bellusci S, Zhang J-S. Impact of Fgf10 deficiency on pulmonary vasculature formation in a mouse model of bronchopulmonary dysplasia. Human Molecular Genetics. 2019;28:1429–1444. doi: 10.1093/hmg/ddy439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao et al. (2017).Chao C-M, Yahya F, Moiseenko A, Tiozzo C, Shrestha A, Ahmadvand N, El Agha E, Quantius J, Dilai S, Kheirollahi V, Jones M, Wilhem J, Carraro G, Ehrhardt H, Zimmer K-P, Barreto G, Ahlbrecht K, Morty RE, Herold S, Abellar RG, Seeger W, Schermuly R, Zhang J-S, Minoo P, Bellusci S. Fgf10 deficiency is causative for lethality in a mouse model of bronchopulmonary dysplasia. The Journal of Pathology. 2017;241:91–103. doi: 10.1002/path.4834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatzeli, Gaete & Tucker (2017).Chatzeli L, Gaete M, Tucker AS. Fgf10 and Sox9 are essential for the establishment of distal progenitor cells during mouse salivary gland development. Development. 2017;144:2294–2305. doi: 10.1242/dev.146019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu et al. (2021).Chu X, Taghizadeh S, Vazquez-Armendariz AI, Herold S, Chong L, Chen C, Zhang J-S, El Agha E, Bellusci S. Validation of a novel Fgf10Cre−ERT2 knock-in mouse line targeting FGF10Pos cells postnatally. Frontiers in Cell and Developmental Biology. 2021;9:671841. doi: 10.3389/fcell.2021.671841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coalson (2003).Coalson JJ. Pathology of new bronchopulmonary dysplasia. Seminars in neonatology. 2003;8:73–81. doi: 10.1016/s1084-2756(02)00193-8. [DOI] [PubMed] [Google Scholar]
- Dai et al. (2022).Dai H, Zhu M, Li W, Si G, Xing Y. Activation of PI3K/p110 α in the lung mesenchyme affects branching morphogenesis and club cell differentiation. Frontiers in Cell and Developmental Biology. 2022;10:880206. doi: 10.3389/fcell.2022.880206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dankova et al. (2017).Dankova Z, Zubor P, Grendar M, Kapinova A, Zelinova K, Jagelkova M, Gondova A, Dokus K, Kalman M, Lasabova Z, Danko J. Association of single nucleotide polymorphisms in FGF-RAS/MAP signalling cascade with breast cancer susceptibility. General Physiology and Biophysics. 2017;36:565–572. doi: 10.4149/gpb_2017033. [DOI] [PubMed] [Google Scholar]
- Danopoulos et al. (2019).Danopoulos S, Thornton ME, Grubbs BH, Frey MR, Warburton D, Bellusci S, Al Alam D. Discordant roles for FGF ligands in lung branching morphogenesis between human and mouse. The Journal of Pathology. 2019;247:254–265. doi: 10.1002/path.5188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Moerlooze et al. (2000).De Moerlooze L, Spencer-Dene B, Revest JM, Hajihosseini M, Rosewell I, Dickson C. An important role for the IIIb isoform of fibroblast growth factor receptor 2 (FGFR2) in mesenchymal-epithelial signalling during mouse organogenesis. Development. 2000;127:483–492. doi: 10.1242/dev.127.3.483. [DOI] [PubMed] [Google Scholar]
- Dixon et al. (2011).Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: understanding genetic and environmental influences. Nature Reviews. Genetics. 2011;12:167–178. doi: 10.1038/nrg2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolegowska et al. (2019).Dolegowska K, Marchelek-Mysliwiec M, Nowosiad-Magda M, Slawinski M, Dolegowska B. FGF19 subfamily members: FGF19 and FGF21. Journal of Physiology and Biochemistry. 2019;75:229–240. doi: 10.1007/s13105-019-00675-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Draaken et al. (2012).Draaken M, Prins W, Zeidler C, Hilger A, Mughal SS, Latus J, Boemers TM, Schmidt D, Schmiedeke E, Spychalski N, Bartels E, Nöthen MM, Reutter H, Ludwig M. Involvement of the WNT and FGF signaling pathways in non-isolated anorectal malformations: sequencing analysis of WNT3A, WNT5A, WNT11, DACT1, FGF10, FGFR2 and the T gene. International Journal of Molecular Medicine. 2012;30:1459–1464. doi: 10.3892/ijmm.2012.1124. [DOI] [PubMed] [Google Scholar]
- Emoto et al. (1997).Emoto H, Tagashira S, Mattei MG, Yamasaki M, Hashimoto G, Katsumata T, Negoro T, Nakatsuka M, Birnbaum D, Coulier F, Itoh N. Structure and expression of human fibroblast growth factor-10. The Journal of Biological Chemistry. 1997;272:23191–23194. doi: 10.1074/jbc.272.37.23191. [DOI] [PubMed] [Google Scholar]
- Entesarian et al. (2007).Entesarian M, Dahlqvist J, Shashi V, Stanley CS, Falahat B, Reardon W, Dahl N. FGF10 missense mutations in aplasia of lacrimal and salivary glands (ALSG) European Journal of Human Genetics. 2007;15:379–382. doi: 10.1038/sj.ejhg.5201762. [DOI] [PubMed] [Google Scholar]
- Entesarian et al. (2005).Entesarian M, Matsson H, Klar J, Bergendal B, Olson L, Arakaki R, Hayashi Y, Ohuchi H, Falahat B, Bolstad AI, Jonsson R, Wahren-Herlenius M, Dahl N. Mutations in the gene encoding fibroblast growth factor 10 are associated with aplasia of lacrimal and salivary glands. Nature Genetics. 2005;37:125–127. doi: 10.1038/ng1507. [DOI] [PubMed] [Google Scholar]
- Esko & Selleck (2002).Esko JD, Selleck SB. Order out of chaos: assembly of ligand binding sites in heparan sulfate. Annual Review of Biochemistry. 2002;71:435–471. doi: 10.1146/annurev.biochem.71.110601.135458. [DOI] [PubMed] [Google Scholar]
- Fairbanks et al. (2004).Fairbanks TJ, De Langhe S, Sala FG, Warburton D, Anderson KD, Bellusci S, Burns RC. Fibroblast growth factor 10 (Fgf10) invalidation results in anorectal malformation in mice. Journal of Pediatric Surgery. 2004;39:360–365. doi: 10.1016/j.jpedsurg.2003.11.034. [DOI] [PubMed] [Google Scholar]
- Ferguson, Smith & Francavilla (2021).Ferguson HR, Smith MP, Francavilla C. Fibroblast growth factor receptors (FGFRs) and noncanonical partners in cancer signaling. Cells. 2021;10:1201. doi: 10.3390/cells10051201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu et al. (2004).Fu L, John LM, Adams SH, Yu XX, Tomlinson E, Renz M, Williams PM, Soriano R, Corpuz R, Moffat B, Vandlen R, Simmons L, Foster J, Stephan JP, Tsai SP, Stewart TA. Fibroblast growth factor 19 increases metabolic rate and reverses dietary and leptin-deficient diabetes. Endocrinology. 2004;145:2594–2603. doi: 10.1210/en.2003-1671. [DOI] [PubMed] [Google Scholar]
- Fürthauer et al. (2001).Fürthauer M, Reifers F, Brand M, Thisse B, Thisse C. sprouty4 acts in vivo as a feedback-induced antagonist of FGF signaling in zebrafish. Development. 2001;128:2175–2186. doi: 10.1242/dev.128.12.2175. [DOI] [PubMed] [Google Scholar]
- Ghoussaini et al. (2016).Ghoussaini M, French JD, Michailidou K, Nord S, Beesley J, Canisus S, Hillman KM, Kaufmann S, Sivakumaran H, Moradi Marjaneh M, Lee JS, Dennis J, Bolla MK, Wang Q, Dicks E, Milne RL, Hopper JL, Southey MC, Schmidt MK, Broeks A, Muir K, Lophatananon A, Fasching PA, Beckmann MW, Fletcher O, Johnson N, Sawyer EJ, Tomlinson I, Burwinkel B, Marme F, Guénel P, Truong T, Bojesen SE, Flyger H, Benitez J, González-Neira A, Alonso MR, Pita G, Neuhausen SL, Anton-Culver H, Brenner H, Arndt V, Meindl A, Schmutzler RK, Brauch H, Hamann U, Tessier DC, Vincent D, Nevanlinna H, Khan S, Matsuo K, Ito H, Dörk T, Bogdanova NV, Lindblom A, Margolin S, Mannermaa A, Kosma V-M, Wu AH, Van Den Berg D, Lambrechts D, Floris G, Chang-Claude J, Rudolph A, Radice P, Barile M, Couch FJ, Hallberg E, Giles GG, Haiman CA, Marchand LLe, Goldberg MS, Teo SH, Yip CH, Borresen-Dale A-L, Zheng W, Cai Q, Winqvist R, Pylkäs K, Andrulis IL, Devilee P, Tollenaar RAEM, García-Closas M, Figueroa J, Hall P, Czene K, Brand JS, Darabi H, Eriksson M, Hooning MJ, Koppert LB, Li J, Shu X-O, Zheng Y, Cox A, Cross SS, Shah M, Rhenius V, Choi J-Y, Kang D, Hartman M, Chia KS, Kabisch M, Torres D, Luccarini C, Conroy DM, Jakubowska A, Lubinski J, Sangrajrang S, Brennan P, Olswold C, Slager S, Shen C-Y, Hou M-F, Swerdlow A, Schoemaker MJ, Simard J, Pharoah PDP, Kristensen V, Chenevix-Trench G, Easton DF, Dunning AM, Edwards SL. kConFab/AOCS Investigators, NBCS Collaborators Evidence that the 5p12 variant rs10941679 confers susceptibility to estrogen-receptor-positive breast cancer through FGF10 and MRPS30 regulation. American Journal of Human Genetics. 2016;99:903–911. doi: 10.1016/j.ajhg.2016.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacomini et al. (2021).Giacomini A, Grillo E, Rezzola S, Ribatti D, Rusnati M, Ronca R, Presta M. The FGF/FGFR system in the physiopathology of the prostate gland. Physiological Reviews. 2021;101:569–610. doi: 10.1152/physrev.00005.2020. [DOI] [PubMed] [Google Scholar]
- Govindarajan et al. (2000).Govindarajan V, Ito M, Makarenkova HP, Lang RA, Overbeek PA. Endogenous and ectopic gland induction by FGF-10. Developmental Biology. 2000;225:188–200. doi: 10.1006/dbio.2000.9812. [DOI] [PubMed] [Google Scholar]
- Graeff, Wang & McCray (1999).Graeff RW, Wang G, McCray PB. KGF and FGF-10 stimulate liquid secretion in human fetal lung. Pediatric Research. 1999;46:523–529. doi: 10.1203/00006450-199911000-00006. [DOI] [PubMed] [Google Scholar]
- Hines & Sun (2014).Hines EA, Sun X. Tissue crosstalk in lung development. Journal of Cellular Biochemistry. 2014;115:1469–1477. doi: 10.1002/jcb.24811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirashima, Iwasa & Morishita (2009).Hirashima T, Iwasa Y, Morishita Y. Mechanisms for split localization of Fgf10 expression in early lung development. Developmental Dynamics. 2009;238:2813–2822. doi: 10.1002/dvdy.22108. [DOI] [PubMed] [Google Scholar]
- Holden et al. (2016).Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- Hsi et al. (2013).Hsi E, Chen K-C, Chang W-S, Yu M-L, Liang C-L, Juo S-HH. A functional polymorphism at the FGF10 gene is associated with extreme myopia. Investigative Ophthalmology & Visual Science. 2013;54:3265–3271. doi: 10.1167/iovs.13-11814. [DOI] [PubMed] [Google Scholar]
- Hui et al. (2018).Hui Q, Jin Z, Li X, Liu C, Wang X. FGF family: from drug development to clinical application. International Journal of Molecular Sciences. 2018;19:E1875. doi: 10.3390/ijms19071875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imamura (2014).Imamura T. Physiological functions and underlying mechanisms of fibroblast growth factor (FGF) family members: recent findings and implications for their pharmacological application. Biological & Pharmaceutical Bulletin. 2014;37:1081–1089. doi: 10.1248/bpb.b14-00265. [DOI] [PubMed] [Google Scholar]
- Itoh (2010).Itoh N. Hormone-like (endocrine) Fgfs: their evolutionary history and roles in development, metabolism, and disease. Cell and Tissue Research. 2010;342:1–11. doi: 10.1007/s00441-010-1024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itoh (2016).Itoh N. FGF10: a multifunctional mesenchymal-epithelial signaling growth factor in development, health, and disease. Cytokine & Growth Factor Reviews. 2016;28:63–69. doi: 10.1016/j.cytogfr.2015.10.001. [DOI] [PubMed] [Google Scholar]
- Itoh et al. (2016).Itoh N, Ohta H, Nakayama Y, Konishi M. Roles of FGF signals in heart development, health, and disease. Frontiers in Cell and Developmental Biology. 2016;4:110. doi: 10.3389/fcell.2016.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itoh & Ornitz (2008).Itoh N, Ornitz DM. Functional evolutionary history of the mouse Fgf gene family. Developmental Dynamics. 2008;237:18–27. doi: 10.1002/dvdy.21388. [DOI] [PubMed] [Google Scholar]
- Jiang et al. (2019).Jiang L, Luo D, Wang T, Zheng R, Zhai Y, Liu X, Gong B, Wu Z, Yang Y, Yang Z, Shi Y. Evaluation of FGF10 as a candidate gene for high myopia in a Han Chinese population. Eye and Vision. 2019;6:33. doi: 10.1186/s40662-019-0158-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang et al. (2021).Jiang X, Tong T, Xia N, Wu L, Zhang C, Zhang Y, Li R-X. Association study of fibroblast growth factor 10 (FGF10) rs399501 polymorphism with susceptibility to high myopia in a Chinese population. Ophthalmic Genetics. 2021;42:239–242. doi: 10.1080/13816810.2021.1881980. [DOI] [PubMed] [Google Scholar]
- Jones, Chong & Bellusci (2020).Jones MR, Chong L, Bellusci S. Fgf10/Fgfr2b signaling orchestrates the symphony of molecular, cellular, and physical processes required for harmonious airway branching morphogenesis. Frontiers in Cell and Developmental Biology. 2020;8:620667. doi: 10.3389/fcell.2020.620667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karasawa et al. (2022).Karasawa Y, Shinomiya N, Takeuchi M, Ito M. Growth factor dependence of the proliferation and survival of cultured lacrimal gland epithelial cells isolated from late-embryonic mice. Development, Growth & Differentiation. 2022;64:138–149. doi: 10.1111/dgd.12776. [DOI] [PubMed] [Google Scholar]
- Karolak et al. (2019).Karolak JA, Vincent M, Deutsch G, Gambin T, Cogné B, Pichon O, Vetrini F, Mefford HC, Dines JN, Golden-Grant K, Dipple K, Freed AS, Leppig KA, Dishop M, Mowat D, Bennetts B, Gifford AJ, Weber MA, Lee AF, Boerkoel CF, Bartell TM, Ward-Melver C, Besnard T, Petit F, Bache I, Tümer Z, Denis-Musquer M, Joubert M, Martinovic J, Bénéteau C, Molin A, Carles D, André G, Bieth E, Chassaing N, Devisme L, Chalabreysse L, Pasquier L, Secq V, Don M, Orsaria M, Missirian C, Mortreux J, Sanlaville D, Pons L, Küry S, Bézieau S, Liet J-M, Joram N, Bihouée T, Scott DA, Brown CW, Scaglia F, Tsai AC-H, Grange DK, Phillips JA, Pfotenhauer JP, Jhangiani SN, Gonzaga-Jauregui CG, Chung WK, Schauer GM, Lipson MH, Mercer CL, Van Haeringen A, Liu Q, Popek E, Coban Akdemir ZH, Lupski JR, Szafranski P, Isidor B, Le Caignec C, Stankiewicz P. Complex compound inheritance of lethal lung developmental disorders due to disruption of the TBX-FGF pathway. The American Journal of Human Genetics. 2019;104:213–228. doi: 10.1016/j.ajhg.2018.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katoh & Nakagama (2014).Katoh M, Nakagama H. FGF receptors: cancer biology and therapeutics. Medicinal Research Reviews. 2014;34:280–300. doi: 10.1002/med.21288. [DOI] [PubMed] [Google Scholar]
- Kelly, Brown & Buckingham (2001).Kelly RG, Brown NA, Buckingham ME. The arterial pole of the mouse heart forms from Fgf10-expressing cells in pharyngeal mesoderm. Developmental Cell. 2001;1:435–440. doi: 10.1016/s1534-5807(01)00040-5. [DOI] [PubMed] [Google Scholar]
- Kempen et al. (2004).Kempen JH, Mitchell P, Lee KE, Tielsch JM, Broman AT, Taylor HR, Ikram MK, Congdon NG, O’Colmain BJ. Eye Diseases Prevalence Research Group The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Archives of Ophthalmology. 2004;122:495–505. doi: 10.1001/archopht.122.4.495. [DOI] [PubMed] [Google Scholar]
- Khosravi et al. (2022).Khosravi F, Ahmadvand N, Wartenberg M, Sauer H. Induction of stem-cell-derived cardiomyogenesis by fibroblast growth factor 10 (FGF10) and its interplay with Cardiotrophin-1 (CT-1) Biology. 2022;11:534. doi: 10.3390/biology11040534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klar et al. (2011).Klar J, Blomstrand P, Brunmark C, Badhai J, Håkansson HF, Brange CS, Bergendal B, Dahl N. Fibroblast growth factor 10 haploinsufficiency causes chronic obstructive pulmonary disease. Journal of Medical Genetics. 2011;48:705–709. doi: 10.1136/jmedgenet-2011-100166. [DOI] [PubMed] [Google Scholar]
- Krüger et al. (2008).Krüger V, Khoshvaghti M, Reutter H, Vogt H, Boemers TM, Ludwig M. Investigation of FGF10 as a candidate gene in patients with anorectal malformations and exstrophy of the cloaca. Pediatric Surgery International. 2008;24:893–897. doi: 10.1007/s00383-008-2193-x. [DOI] [PubMed] [Google Scholar]
- Li et al. (2019).Li W, Wang M, Zhou R, Wang S, Zheng H, Liu D, Zhou Z, Zhu H, Wu T, Beaty TH. Exploring the interaction between FGF Genes and T-box genes among Chinese nonsyndromic cleft lip with or without cleft palate case-parent trios. Environmental and Molecular Mutagenesis. 2019;60:602–606. doi: 10.1002/em.22286. [DOI] [PubMed] [Google Scholar]
- Lim et al. (2012).Lim W, Kwan JL, Goh LK, Beuerman RW, Barathi VA. Evaluation of gene expression profiles and pathways underlying postnatal development in mouse sclera. Molecular Vision. 2012;18:1436–1448. [PMC free article] [PubMed] [Google Scholar]
- Lindahl & Li (2009).Lindahl U, Li J. Interactions between heparan sulfate and proteins-design and functional implications. International Review of Cell and Molecular Biology. 2009;276:105–159. doi: 10.1016/S1937-6448(09)76003-4. [DOI] [PubMed] [Google Scholar]
- Makarenkova et al. (2000).Makarenkova HP, Ito M, Govindarajan V, Faber SC, Sun L, McMahon G, Overbeek PA, Lang RA. FGF10 is an inducer and Pax6 a competence factor for lacrimal gland development. Development. 2000;127:2563–2572. doi: 10.1242/dev.127.12.2563. [DOI] [PubMed] [Google Scholar]
- Marchese et al. (2001).Marchese C, Felici A, Visco V, Lucania G, Igarashi M, Picardo M, Frati L, Torrisi MR. Fibroblast growth factor 10 induces proliferation and differentiation of human primary cultured keratinocytes. The Journal of Investigative Dermatology. 2001;116:623–628. doi: 10.1046/j.0022-202x.2001.01280.x. [DOI] [PubMed] [Google Scholar]
- Mauduit et al. (2022).Mauduit O, Aure MH, Delcroix V, Basova L, Srivastava A, Umazume T, Mays JW, Bellusci S, Tucker AS, Hajihosseini MK, Hoffman MP, Makarenkova HP. A mesenchymal to epithelial switch in Fgf10 expression specifies an evolutionary-conserved population of ionocytes in salivary glands. Cell Reports. 2022;39:110663. doi: 10.1016/j.celrep.2022.110663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milunsky et al. (2006).Milunsky JM, Zhao G, Maher TA, Colby R, Everman DB. LADD syndrome is caused by FGF10 mutations. Clinical Genetics. 2006;69:349–354. doi: 10.1111/j.1399-0004.2006.00597.x. [DOI] [PubMed] [Google Scholar]
- Min et al. (1998).Min H, Danilenko DM, Scully SA, Bolon B, Ring BD, Tarpley JE, De Rose M, Simonet WS. Fgf-10 is required for both limb and lung development and exhibits striking functional similarity to Drosophila branchless. Genes & Development. 1998;12:3156–3161. doi: 10.1101/gad.12.20.3156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molfino (2004).Molfino NA. Genetics of COPD. Chest. 2004;125:1929–1940. doi: 10.1378/chest.125.5.1929. [DOI] [PubMed] [Google Scholar]
- Mostowska et al. (2010).Mostowska A, Hozyasz KK, Wojcicki P, Biedziak B, Paradowska P, Jagodzinski PP. Association between genetic variants of reported candidate genes or regions and risk of cleft lip with or without cleft palate in the polish population. Birth Defects Research. Part A, Clinical and Molecular Teratology. 2010;88:538–545. doi: 10.1002/bdra.20687. [DOI] [PubMed] [Google Scholar]
- Ndlovu et al. (2018).Ndlovu R, Deng L-C, Wu J, Li X-K, Zhang J-S. Fibroblast growth factor 10 in pancreas development and pancreatic cancer. Frontiers in Genetics. 2018;9:482. doi: 10.3389/fgene.2018.00482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norgaard, Jensen & Jensen (2003).Norgaard GA, Jensen JN, Jensen J. FGF10 signaling maintains the pancreatic progenitor cell state revealing a novel role of Notch in organ development. Developmental Biology. 2003;264:323–338. doi: 10.1016/j.ydbio.2003.08.013. [DOI] [PubMed] [Google Scholar]
- Ohuchi et al. (2000).Ohuchi H, Hori Y, Yamasaki M, Harada H, Sekine K, Kato S, Itoh N. FGF10 acts as a major ligand for FGF receptor 2 IIIb in mouse multi-organ development. Biochemical and Biophysical Research Communications. 2000;277:643–649. doi: 10.1006/bbrc.2000.3721. [DOI] [PubMed] [Google Scholar]
- Ong et al. (2000).Ong SH, Guy GR, Hadari YR, Laks S, Gotoh N, Schlessinger J, Lax I. FRS2 proteins recruit intracellular signaling pathways by binding to diverse targets on fibroblast growth factor and nerve growth factor receptors. Molecular and Cellular Biology. 2000;20:979–989. doi: 10.1128/MCB.20.3.979-989.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornitz & Itoh (2015).Ornitz DM, Itoh N. The fibroblast growth factor signaling pathway. Wiley Interdisciplinary Reviews. Developmental Biology. 2015;4:215–266. doi: 10.1002/wdev.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan, Ramamurthy & Saw (2012).Pan C-W, Ramamurthy D, Saw S-M. Worldwide prevalence and risk factors for myopia. Ophthalmic & Physiological Optics. 2012;32:3–16. doi: 10.1111/j.1475-1313.2011.00884.x. [DOI] [PubMed] [Google Scholar]
- Prince (2018).Prince LS. FGF10 and human lung disease across the life spectrum. Frontiers in Genetics. 2018;9:517. doi: 10.3389/fgene.2018.00517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochazkova et al. (2018).Prochazkova M, Prochazka J, Marangoni P, Klein OD. Bones, glands, ears and more: the multiple roles of FGF10 in craniofacial development. Frontiers in Genetics. 2018;9:542. doi: 10.3389/fgene.2018.00542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prudovsky (2021).Prudovsky I. Cellular mechanisms of FGF-stimulated tissue repair. Cells. 2021;10:1830. doi: 10.3390/cells10071830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabe et al. (2007).Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, Van Weel C, Zielinski J. Global initiative for chronic obstructive lung disease Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. American Journal of Respiratory and Critical Care Medicine. 2007;176:532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- Raju et al. (2021).Raju GT, Bhaskar LVKS, Gurramkonda VB, Hussain SA, Paul SFD. Genetic variations at 10q26 regions near FGFR2 gene and its association with non-syndromic cleft lip with or without cleft palate. International Journal of Pediatric Otorhinolaryngology. 2021;143:110648. doi: 10.1016/j.ijporl.2021.110648. [DOI] [PubMed] [Google Scholar]
- Reintjes et al. (2013).Reintjes N, Li Y, Becker A, Rohmann E, Schmutzler R, Wollnik B. Activating somatic FGFR2 mutations in breast cancer. PLOS ONE. 2013;8:e60264. doi: 10.1371/journal.pone.0060264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren et al. (2013).Ren J, Feng K, Wang P, Peng W, Jia H, Liu K, Lu H. Relationship between the gene polymorphism in fibroblast growth factor-10 and susceptibility to chronic obstructive pulmonary disease 220 cases. Chinese Journal of Tuberculosis and Respiratory Diseases. 2013;36:935–939. [PubMed] [Google Scholar]
- Rice et al. (2004).Rice R, Spencer-Dene B, Connor EC, Gritli-Linde A, McMahon AP, Dickson C, Thesleff I, Rice DPC. Disruption of Fgf10/Fgfr2b-coordinated epithelial-mesenchymal interactions causes cleft palate. The Journal of Clinical Investigation. 2004;113:1692–1700. doi: 10.1172/JCI20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley et al. (2007).Riley BM, Mansilla MA, Ma J, Daack-Hirsch S, Maher BS, Raffensperger LM, Russo ET, Vieira AR, Dodé C, Mohammadi M, Marazita ML, Murray JC. Impaired FGF signaling contributes to cleft lip and palate. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:4512–4517. doi: 10.1073/pnas.0607956104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochais et al. (2014).Rochais F, Sturny R, Chao C-M, Mesbah K, Bennett M, Mohun TJ, Bellusci S, Kelly RG. FGF10 promotes regional foetal cardiomyocyte proliferation and adult cardiomyocyte cell-cycle re-entry. Cardiovascular Research. 2014;104:432–442. doi: 10.1093/cvr/cvu232. [DOI] [PubMed] [Google Scholar]
- Rodrigo et al. (2018).Rodrigo MJ, Idoipe M, Izquierdo S, Satue M, Mateo A, Sanchez A, Garcia-Martin E, Pablo L. New pathogenic variant in the FGF10 gene in the agenesis of lacrimal and salivary gland syndrome: Ophthalmological and genetic study. Ophthalmic Genetics. 2018;39:125–128. doi: 10.1080/13816810.2017.1381976. [DOI] [PubMed] [Google Scholar]
- Rohmann et al. (2006).Rohmann E, Brunner HG, Kayserili H, Uyguner O, Nürnberg G, Lew ED, Dobbie A, Eswarakumar VP, Uzumcu A, Ulubil-Emeroglu M, Leroy JG, Li Y, Becker C, Lehnerdt K, Cremers CWRJ, Yüksel-Apak M, Nürnberg P, Kubisch C, Kubisch C, Schlessinger J, Van Bokhoven H, Wollnik B. Mutations in different components of FGF signaling in LADD syndrome. Nature Genetics. 2006;38:414–417. doi: 10.1038/ng1757. [DOI] [PubMed] [Google Scholar]
- Rose et al. (2008).Rose KA, Morgan IG, Smith W, Burlutsky G, Mitchell P, Saw S-M. Myopia, lifestyle, and schooling in students of Chinese ethnicity in Singapore and Sydney. Archives of Ophthalmology. 2008;126:527–530. doi: 10.1001/archopht.126.4.527. [DOI] [PubMed] [Google Scholar]
- Ryu et al. (2020).Ryu YH, Kyun Chae J, Kim J-W, Lee S. Lacrimo-auriculo-dento-digital syndrome: a novel mutation in a Korean family and review of literature. Molecular Genetics & Genomic Medicine. 2020;8:e1412. doi: 10.1002/mgg3.1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahara & O’Leary (2009).Sahara S, O’Leary DDM. Fgf10 regulates transition period of cortical stem cell differentiation to radial glia controlling generation of neurons and basal progenitors. Neuron. 2009;63:48–62. doi: 10.1016/j.neuron.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakaue et al. (2002).Sakaue H, Konishi M, Ogawa W, Asaki T, Mori T, Yamasaki M, Takata M, Ueno H, Kato S, Kasuga M, Itoh N. Requirement of fibroblast growth factor 10 in development of white adipose tissue. Genes & Development. 2002;16:908–912. doi: 10.1101/gad.983202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saw et al. (2005).Saw S-M, Gazzard G, Shih-Yen EC, Chua W-H. Myopia and associated pathological complications. Ophthalmic & Physiological Optics. 2005;25:381–391. doi: 10.1111/j.1475-1313.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- Sekine et al. (1999).Sekine K, Ohuchi H, Fujiwara M, Yamasaki M, Yoshizawa T, Sato T, Yagishita N, Matsui D, Koga Y, Itoh N, Kato S. Fgf10 is essential for limb and lung formation. Nature Genetics. 1999;21:138–141. doi: 10.1038/5096. [DOI] [PubMed] [Google Scholar]
- Seymen et al. (2017).Seymen F, Koruyucu M, Toptanci IR, Balsak S, Dedeoglu S, Celepkolu T, Shin TJ, Hyun H-K, Kim Y-J, Kim J-W. Novel FGF10 mutation in autosomal dominant aplasia of lacrimal and salivary glands. Clinical Oral Investigations. 2017;21:167–172. doi: 10.1007/s00784-016-1771-x. [DOI] [PubMed] [Google Scholar]
- Shah et al. (2008).Shah GS, Singh MK, Pandey TR, Kalakheti BK, Bhandari GP. Incidence of congenital heart disease in tertiary care hospital. Kathmandu University Medical Journal. 2008;6:33–36. [PubMed] [Google Scholar]
- Shams et al. (2007).Shams I, Rohmann E, Eswarakumar VP, Lew ED, Yuzawa S, Wollnik B, Schlessinger J, Lax I. Lacrimo-auriculo-dento-digital syndrome is caused by reduced activity of the fibroblast growth factor 10 (FGF10)-FGF receptor 2 signaling pathway. Molecular and Cellular Biology. 2007;27:6903–6912. doi: 10.1128/MCB.00544-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi et al. (2009).Shi M, Mostowska A, Jugessur A, Johnson MK, Mansilla MA, Christensen K, Lie RT, Wilcox AJ, Murray JC. Identification of microdeletions in candidate genes for cleft lip and/or palate. Birth Defects Research. Part A, Clinical and Molecular Teratology. 2009;85:42–51. doi: 10.1002/bdra.20571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith et al. (2018).Smith BM, Traboulsi H, Austin JHM, Manichaikul A, Hoffman EA, Bleecker ER, Cardoso WV, Cooper C, Couper DJ, Dashnaw SM, Guo J, Han MK, Hansel NN, Hughes EW, Jacobs DR, Kanner RE, Kaufman JD, Kleerup E, Lin C-L, Liu K, Lo Cascio CM, Martinez FJ, Nguyen JN, Prince MR, Rennard S, Rich SS, Simon L, Sun Y, Watson KE, Woodruff PG, Baglole CJ, Barr RG. MESA Lung and SPIROMICS investigators Human airway branch variation and chronic obstructive pulmonary disease. Proceedings of the National Academy of Sciences of the United States of America. 2018;115:E974–E981. doi: 10.1073/pnas.1715564115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacey et al. (2008).Stacey SN, Manolescu A, Sulem P, Thorlacius S, Gudjonsson SA, Jonsson GF, Jakobsdottir M, Bergthorsson JT, Gudmundsson J, Aben KK, Strobbe LJ, Swinkels DW, Van Engelenburg KCA, Henderson BE, Kolonel LN, Le Marchand L, Millastre E, Andres R, Saez B, Lambea J, Godino J, Polo E, Tres A, Picelli S, Rantala J, Margolin S, Jonsson T, Sigurdsson H, Jonsdottir T, Hrafnkelsson J, Johannsson J, Sveinsson T, Myrdal G, Grimsson HN, Sveinsdottir SG, Alexiusdottir K, Saemundsdottir J, Sigurdsson A, Kostic J, Gudmundsson L, Kristjansson K, Masson G, Fackenthal JD, Adebamowo C, Ogundiran T, Olopade OI, Haiman CA, Lindblom A, Mayordomo JI, Kiemeney LA, Gulcher JR, Rafnar T, Thorsteinsdottir U, Johannsson OT, Kong A, Stefansson K. Common variants on chromosome 5p12 confer susceptibility to estrogen receptor-positive breast cancer. Nature Genetics. 2008;40:703–706. doi: 10.1038/ng.131. [DOI] [PubMed] [Google Scholar]
- Stoll et al. (2007).Stoll C, Alembik Y, Dott B, Roth MP. Associated malformations in patients with anorectal anomalies. European Journal of Medical Genetics. 2007;50:281–290. doi: 10.1016/j.ejmg.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Sun et al. (2019).Sun W, Li Y, Li J, Zhang X, Feng Q, Zhang Z, Kang J, Huang X. Cytokine fibroblast growth factor 10 (FGF10) polymorphisms are associated with risk of myopia in young children. Journal of Cellular Biochemistry. 2019;120:15241–15247. doi: 10.1002/jcb.28790. [DOI] [PubMed] [Google Scholar]
- Sun et al. (2021).Sun XW, Lin YN, Ding YJ, Li SQ, Li HP, Li QY. Bronchial variation: anatomical abnormality may predispose chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease. 2021;16:423–431. doi: 10.2147/COPD.S297777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taghizadeh et al. (2022).Taghizadeh S, Chao C-M, Guenther S, Glaser L, Gersmann L, Michel G, Kraut S, Goth K, Koepke J, Heiner M, Vazquez-Armendariz AI, Herold S, Samakovlis C, Weissmann N, Ricci F, Aquila G, Boyer L, Ehrhardt H, Minoo P, Bellusci S, Rivetti S. FGF10 triggers De Novo alveologenesis in a bronchopulmonary dysplasia model: impact on resident mesenchymal niche cells. Stem Cells. 2022;40:605–617. doi: 10.1093/stmcls/sxac025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tashkin et al. (1996).Tashkin DP, Altose MD, Connett JE, Kanner RE, Lee WW, Wise RA. Methacholine reactivity predicts changes in lung function over time in smokers with early chronic obstructive pulmonary disease. The Lung Health Study Research Group. American Journal of Respiratory and Critical Care Medicine. 1996;153:1802–1811. doi: 10.1164/ajrccm.153.6.8665038. [DOI] [PubMed] [Google Scholar]
- Teshima, Lourenco & Tucker (2016).Teshima THN, Lourenco SV, Tucker AS. Multiple cranial organ defects after conditionally knocking out Fgf10 in the neural crest. Frontiers in Physiology. 2016;7:488. doi: 10.3389/fphys.2016.00488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theodorou et al. (2004).Theodorou V, Boer M, Weigelt B, Jonkers J, Van der Valk M, Hilkens J. Fgf10 is an oncogene activated by MMTV insertional mutagenesis in mouse mammary tumors and overexpressed in a subset of human breast carcinomas. Oncogene. 2004;23:6047–6055. doi: 10.1038/sj.onc.1207816. [DOI] [PubMed] [Google Scholar]
- Thiery et al. (2009).Thiery JP, Acloque H, Huang RYJ, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Tsang et al. (2002).Tsang M, Friesel R, Kudoh T, Dawid IB. Identification of Sef, a novel modulator of FGF signalling. Nature Cell Biology. 2002;4:165–169. doi: 10.1038/ncb749. [DOI] [PubMed] [Google Scholar]
- Vincent et al. (2019).Vincent M, Karolak JA, Deutsch G, Gambin T, Popek E, Isidor B, Szafranski P, Le Caignec C, Stankiewicz P. Clinical, histopathological, and molecular diagnostics in lethal lung developmental disorders. American Journal of Respiratory and Critical Care Medicine. 2019;200:1093–1101. doi: 10.1164/rccm.201903-0495TR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade et al. (2021).Wade EM, Parthasarathy P, Mi J, Morgan T, Wollnik B, Robertson SP, Cundy T. Deletion of the last two exons of FGF10 in a family with LADD syndrome and pulmonary acinar hypoplasia. European Journal of Human Genetics. 2021;30(4):480–484. doi: 10.1038/s41431-021-00902-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2018a).Wang S, Li Y, Jiang C, Tian H. Fibroblast growth factor 9 subfamily and the heart. Applied Microbiology and Biotechnology. 2018a;102:605–613. doi: 10.1007/s00253-017-8652-3. [DOI] [PubMed] [Google Scholar]
- Wang et al. (2018b).Wang J, Liu H, Gao L, Liu X. Impaired FGF10 signaling and epithelial development in experimental lung hypoplasia with esophageal atresia. Frontiers in Pediatrics. 2018b;6:109. doi: 10.3389/fped.2018.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson & Francavilla (2018).Watson J, Francavilla C. Regulation of FGF10 signaling in development and disease. Frontiers in Genetics. 2018;9:500. doi: 10.3389/fgene.2018.00500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiedlocha, Haugsten & Zakrzewska (2021).Wiedlocha A, Haugsten EM, Zakrzewska M. Roles of the FGF-FGFR signaling system in cancer development and inflammation. Cells. 2021;10:2231. doi: 10.3390/cells10092231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu et al. (2012).Wu QF, Yang L, Li S, Wang Q, Yuan XB, Gao X, Bao L, Zhang X. Fibroblast growth factor 13 is a microtubule-stabilizing protein regulating neuronal polarization and migration. Cell. 2012;149:1549–1564. doi: 10.1016/j.cell.2012.04.046. [DOI] [PubMed] [Google Scholar]
- Wu, Liu & Zhang (2022).Wu Z, Liu P, Zhang G. Identification of circRNA-miRNA-immune-related mRNA regulatory network in gastric cancer. Frontiers in Oncology. 2022;12:816884. doi: 10.3389/fonc.2022.816884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie et al. (2020).Xie Y, Su N, Yang J, Tan Q, Huang S, Jin M, Ni Z, Zhang B, Zhang D, Luo F, Chen H, Sun X, Feng JQ, Qi H, Chen L. FGF/FGFR signaling in health and disease. Signal Transduction and Targeted Therapy. 2020;5:181. doi: 10.1038/s41392-020-00222-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang et al. (2021).Yang L, Zhou F, Zheng D, Wang D, Li X, Zhao C, Huang X. FGF/FGFR signaling: from lung development to respiratory diseases. Cytokine & Growth Factor Reviews. 2021;62:94–104. doi: 10.1016/j.cytogfr.2021.09.002. [DOI] [PubMed] [Google Scholar]
- Yin et al. (2013).Yin SJ, Tang XB, Li FF, Zhang T, Yuan ZW, Wang WL, Bai YZ. Spatiotemporal expression of fibroblast growth factor 10 in human hindgut and anorectal development. Cells, Tissues, Organs. 2013;198:28–34. doi: 10.1159/000351472. [DOI] [PubMed] [Google Scholar]
- Yoshida et al. (2013).Yoshida M, Meguro A, Okada E, Nomura N, Mizuki N. Association study of fibroblast growth factor 10 (FGF10) polymorphisms with susceptibility to extreme myopia in a Japanese population. Molecular Vision. 2013;19:2321–2329. [PMC free article] [PubMed] [Google Scholar]
- Yu et al. (2017).Yu Y, Zuo X, He M, Gao J, Fu Y, Qin C, Meng L, Wang W, Song Y, Cheng Y, Zhou F, Chen G, Zheng X, Wang X, Liang B, Zhu Z, Fu X, Sheng Y, Hao J, Liu Z, Yan H, Mangold E, Ruczinski I, Liu J, Marazita ML, Ludwig KU, Beaty TH, Zhang X, Sun L, Bian Z. Genome-wide analyses of non-syndromic cleft lip with palate identify 14 novel loci and genetic heterogeneity. Nature Communications. 2017;8:14364. doi: 10.1038/ncomms14364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan et al. (2018).Yuan T, Volckaert T, Chanda D, Thannickal VJ, De Langhe SP. Fgf10 signaling in lung development, homeostasis, disease, and repair after injury. Frontiers in Genetics. 2018;9:418. doi: 10.3389/fgene.2018.00418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yucel et al. (2004).Yucel S, Liu W, Cordero D, Donjacour A, Cunha G, Baskin LS. Anatomical studies of the fibroblast growth factor-10 mutant, Sonic Hedge Hog mutant and androgen receptor mutant mouse genital tubercle. Advances in Experimental Medicine and Biology. 2004;545:123–148. doi: 10.1007/978-1-4419-8995-6_8. [DOI] [PubMed] [Google Scholar]
- Zhang et al. (2012).Zhang X, Bao L, Yang L, Wu Q, Li S. Roles of intracellular fibroblast growth factors in neural development and functions. Science China Life Sciences. 2012;55:1038–1044. doi: 10.1007/s11427-012-4412-x. [DOI] [PubMed] [Google Scholar]
- Zhang et al. (2015).Zhang F, Yu L, Lin X, Cheng P, He L, Li X, Lu X, Tan Y, Yang H, Cai L, Zhang C. Minireview: Roles of Fibroblast Growth Factors 19 and 21 in Metabolic Regulation and Chronic Diseases. Molecular Endocrinology. 2015;29:1400–1413. doi: 10.1210/me.2015-1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao & Zhang (2001).Zhao Y, Zhang ZY. The mechanism of dephosphorylation of extracellular signal-regulated kinase 2 by mitogen-activated protein kinase phosphatase 3. The Journal of Biological Chemistry. 2001;276:32382–32391. doi: 10.1074/jbc.M103369200. [DOI] [PubMed] [Google Scholar]
- Zhou et al. (2020).Zhou S, Wang Q, Meng Z, Peng J, Zhou Y, Song W, Wang J, Chen S, Sun K. Mutations in fibroblast growth factor (FGF8) and FGF10 identified in patients with conotruncal defects. Journal of Translational Medicine. 2020;18:283. doi: 10.1186/s12967-020-02445-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinkle & Mohammadi (2019).Zinkle A, Mohammadi M. Structural biology of the FGF7 subfamily. Frontiers in Genetics. 2019;10:102. doi: 10.3389/fgene.2019.00102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The following information was supplied regarding data availability:
This is a literature review article.