Abstract
Purpose
Azoospermia is defined as the absence of spermatozoa in the pellet of a centrifuged semen sample. In fact, when a basic semen analysis fails to detect sperm in the ejaculate, there is still the possibility of detecting rare sperm after centrifugation of the sample and examination of the pellet. In this study, we assessed the role of Cytospin centrifugation in combination with the nuclear fast picroindigocarmine (NF-PIC) staining in identifying sperm in azoospermic samples.
Materials and Methods
Semen samples of 251 men diagnosed as having azoospermia after standard examination were further analyzed by Cytospin centrifugation in combination with NF-PIC staining.
Results
Sperm were detected in 60 men (23.9%), thus changing their diagnosis to cryptozoospermia.
Conclusions
By identifying sperm in the semen of men who were thought to have total azoospermia, the Cytospin NF-PIC test can alter the diagnosis and further treatment of these men.
Keywords: Azoospermia, Centrifugation, Male infertility, Semen, Staining and labeling
INTRODUCTION
Azoospermia, seen in approximately 10% to 15% of all infertile men [1,2,3], is defined as the absence of sperm in at least two different ejaculate samples, including in the centrifuged sediments [4,5,6]. The purpose of centrifugation is to concentrate rare sperm present in the semen into a compact pellet, thus making it possible to detect cryptozoospermia [4,5,6,7]. Since the detection of rare sperm depends on centrifugation, it is possible that using a different method of centrifugation and staining may detect sperm in samples where no sperm were found initially.
The aim of this study is to assess whether using Cytospin centrifugation in combination with nuclear fast picroindigocarmine (NF-PIC) staining can detect sperm in semen samples that were labelled as azoospermic when examined by the standard method recommended by the World Health Organization (WHO) manual [5,6].
MATERIALS AND METHODS
1. Ethics statement
Following approval of the project (IRB # 21-800) by the Institutional Review Board (IRB) of the Cleveland Clinic (Cleveland, OH, USA), the electronic medical record of the Cleveland Clinic was reviewed for the time period between May 2015 and July 2021.
2. Data collection
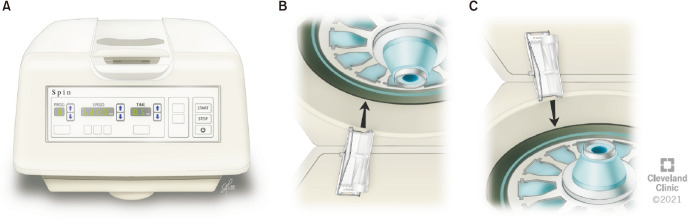
We collected records of azooospermic men who underwent further testing using the Cytospin centrifugation combined with NF-PIC stain test, which was developed in our laboratory [2]. The steps involved in examining the semen sample for the presence of rare spermatozoa are shown in Fig. 1. The outcome of the NF-PIC test was noted as NF-PIC positive if sperm were found, or as NF-PIC negative if no sperm were found. Any additional clinical data available was also recorded for possible secondary analysis.
Fig. 1. Schematics showing steps in examining the semen sample for presence of sperm. NF-PIC: nuclear fast picroindigocarmine.
3. Examination of semen sample
Routine semen analysis was conducted according to WHO recommendations [5]. For examination of the semen sample, 6 µL of a completely liquefied sample was loaded on a fixed 20 µm depth cell counting chamber and observed under a phase contrast microscope using 20× objective and a 10× eyepiece (total magnification of 200) [8]. If no sperm were observed in a wet unspun preparation, the sample was centrifuged at 3,000 g for 15 minutes. The supernatant was discarded and the sperm pellet re-suspended in 50-µL of seminal plasma. Two 6 µL aliquots were loaded on two wells of a fixed cell counting chamber and carefully examined under phase-contrast optics at 200× magnification for the presence of the sperm. A diagnosis of cryptozoospermia was established when sperm were found on examination of the replicates. Diagnosis of azoospermia was confirmed by the absence of sperm on assessment of the replicate wet preparations. If no sperm were observed, the sample was processed for cytocentrifugation.
4. Preparation of samples for cytocentrifugation (Cytospin)
Cytospin is the process whereby cells are centrifuged to be concentrated in a small area on the microscope slide. This uses a bench-top centrifuge with a specially designed rotor and sample chambers to deposit cells onto a clearly defined area of the slide. In order to perform the Cytospin procedure, we used a Cytospin centrifuge (Cytospin 4; Thermo Scientific, Waltham, MA, USA), single Cytofunnel disposable sample chambers, and metal slide holders, along with sterile saline solution (0.9% sodium chloride), frosted glass slides, and sterile Pasteur transfer pipettes. Residual fluid is absorbed by the sample chamber's filter card, which flattens the cells into a monolayer onto the slide preserving their integrity, and making single cells easier to detect. The slide can then be air-dried, stained and examined. For preparation of the samples, we followed the standard protocol, which is described below.
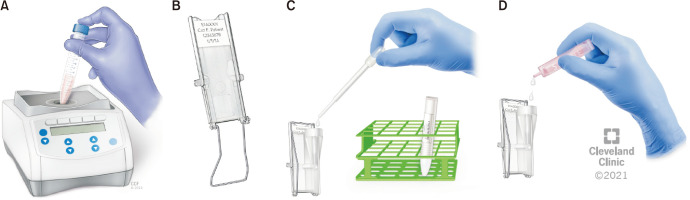
The first steps include turning the Cytospin centrifuge on, lifting the top cover and removing the protective lid on the inside of the centrifuge [2,9]. Frosted slides are first labeled with the patient’s name, medical record number, and date, and then placed into the slide holder (Fig. 2A). The Cytofunnel filter is then placed directly on top of the slide with the frosted side up. Each Cytofunnel filter and slide are paired and then placed into the Cytospin slide holder. After firmly locking with the slide holder's mechanism, the assembled apparatus is positioned upright in the cytocentrifuge slot. Conventionally, slides are labeled as “C” for the Cytospin patient sample, while 1 slide is labeled as “B” for the blank control. The control is prepared in a similar manner as the patient slides, except that it does not include any patient sample. Using a sterile transfer pipette, one drop of the well-mixed patient sample is added into the top opening of the Cytofunnel, followed by one drop of sterile saline in each Cytofunnel. If the specimen is highly viscous, one drop of the semen sample is placed in the Cytospin chamber, and 2 drops of sterile saline are added. For the blank control, two drops of sterile solution are added to the slide, without adding any semen sample (Fig. 3). After the top of the Cytofunnel is securely capped, the assembled slides and Cytofunnel apparatuses are placed into the appropriate slots inside the centrifuge. The protective lid is reinserted inside the centrifuge and locked into place. Next, the top cover is closed and the light on the display comes on to indicate that the cover was properly locked. The sample is centrifuged at 500 g for 10 minutes.
Fig. 2. (A) Cytospin and (B, C) inside view showing the special rotor for proper insertion of the Cytospin slide.
Fig. 3. Preparing for the Cytospin procedure. (A) Mixing the sample. (B) Slide mounted on metal Cytospin slide holder. (C) Droplet of semen sample added to Cytofunnel. (D) Two drops of sterile saline added to Cytofunnel of “blank” control slide.
Precaution should be taken when adding the patient sample to ensure that the fluid is in the horizontal tunnel of the Cytofunnel and not in the vertical cone-shaped part of the tunnel. No more than 0.5 mL of fluid should be used, as this is the maximum amount that the tunnel can hold. If more than 0.5 mL of sample volume is loaded in the cone-shaped vertical portion of the tunnel, it will be forced up the cone during centrifugation and will not get concentrated onto the slide. Caution is also exercised to avoid placing the fingers over the small hole in the center of the closure cap when placing it onto the tunnel. Placing the finger forces the fluid in the horizontal tunnel immediately onto the slide before centrifugation and reduces cell recovery.
After centrifugation, the top cover is opened, and the protective lid and the slide apparatuses are removed. The slide holder with the attached Cytofunnel are laid horizontally on a table. With the slides still locked inside, they are allowed to dry for approximately 5–10 minutes. Next, the Cytofunnel is unlocked, and discarded into a biohazard bin. The slides are allowed to air-dry for an additional 15 minutes before staining, in case fluid remains in the sample chamber after spinning. A quality control slide is also prepared by making a smear of a healthy donor semen sample, which is stained with NF-PIC stain along with the other slides.
5. Preparation of samples for NF-PIC staining
The utility of the NF-PIC staining technique in detecting sperm at small concentrations has been demonstrated by serial dilution of semen samples [10].
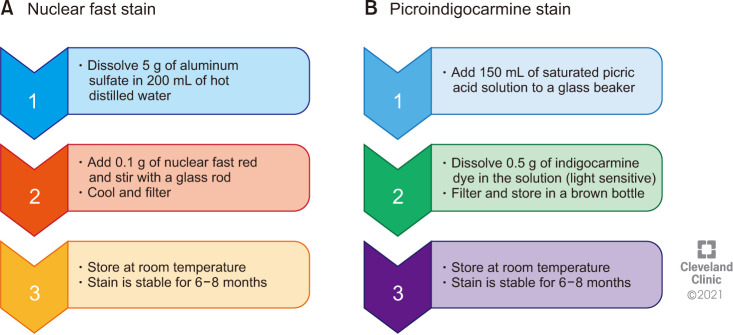
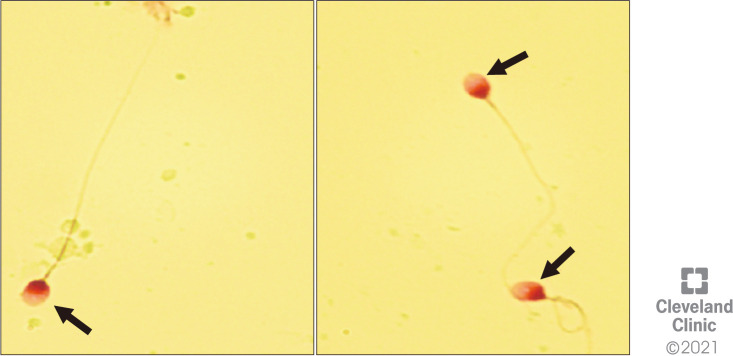
The first step in this procedure includes preparing the NF-PIC staining as shown in Fig. 4. In this study, all the reagents listed in Fig. 4 were supplied by Sigma-Aldrich (St. Louis, MO, USA). Labeled slides for patients, quality control, and blank are placed face-up on the staining rack. By using a sterile Pasteur pipette, a sufficient amount of absolute ethanol (fixative) is used to fully cover each of the slides for 15 minutes (Fig. 5A). The slides are then positioned upright allowing the ethanol to drain off and air-dried for 15 minutes. The slides are laid flat on the staining rack, and a sufficient amount of NF solution is placed to cover each slide for 15 minutes (Fig. 5B). The NF solution from the slide is removed by tilting the slide and the solution is allowed to drain off. The slides are laid flat again on the staining rack, and several drops of PIC staining are placed on the NF-stained slide (Fig. 5C). After 30 seconds of staining with PIC, the excess stain is rinsed off with absolute ethanol, and the slides are allowed to air-dry for 15 minutes. Afterwards, a few drops of Cytoseal mounting media are added, a cover slip is gently placed and allowed to air dry again. The slides are cleaned with lint-free wipes and lens cleaner solution. A drop of immersion oil is placed, and slides are observed for the presence of spermatozoa under a bright-field microscope at 100× magnification (Fig. 6). In this technique, sperm heads stain red and tails green, allowing spermatozoa to be more easily identified when viewed microscopically.
Fig. 4. Schematic of steps in the preparation of (A) nuclear fast stain and (B) picroindigocarmine stain.
Fig. 5. Steps in staining the slides for NF-PIC. (A) Fixing the slides with ethanol for 15 minutes, (B) flooding the slide with nuclear fast stain for 15 minutes, and (C) replacing with picroindigocarmine stain for 30 seconds. NF-PIC: nuclear fast picroindigocarmine.
Fig. 6. The NF-PIC stained slide observed under a bright-field microscope using immersion oil and mounting media. The slide is cleaned with lens cleaner solution or lint-free wipes. NF-PIC: nuclear fast picroindigocarmine.
The results are reported as:
a) No sperm seen: when no sperm are observed after staining.
b) Sperm seen: if sperm with distinct tails (Fig. 7) or only sperm heads are seen.
Fig. 7. Smear showing presence of sperm after NF-PIC staining (magnification, 1,000×). NF stains sperm head pink (indicated by arrow). NF-PIC: nuclear fast picroindigocarmine.
6. Quality control in NF-PIC staining test
A semen sample with normal semen characteristics obtained from a healthy male volunteer is utilized to prepare slides for quality control of NF-PIC staining along with each set of patient slides. The donor slide is first examined and checked for quality of staining. The sperm head should stain pink and the tail green. Once the quality of the stain is considered acceptable, then the patient slides are examined for the presence or absence of sperm.
7. Statistical analysis
Descriptive statistics were used to present the outcome of the NF-PIC technique with positive results (sperm detected) being reported as percentage of total number of samples tested (MedCalc Statistical Software, ver. 17.8; MedCalc Software, Ostend, Belgium).
RESULTS
During the study period, 251 azoospermic men were tested using Cytospin and NF-PIC staining. Of these 251 samples, sperm were detected in 60 (23.9%) patients while 191/251 (76.1%) were negative for sperm (Table 1).
Table 1. Distribution of 251 azoospermic men tested by NF-PIC staining and 46 men who opted for sperm retrieval by mTESE or cTESE for NOA.
| Subject | Total subjects with azoospermia (n=251) | ||
|---|---|---|---|
| NF-PIC positive | NF-PIC negative | ||
| Patient | 60 (23.9) | 191 (76.1) | |
| Undergo surgery | 13 | 33 | |
| Surgery+ | 9 (69.2) | 13 (39.4) | |
| Surgery- | 4 (30.8) | 20 (60.6) | |
Values are presented as number (%) or number only.
cTESE: conventional testicular sperm extraction, mTESE: microsurgical testicular sperm extraction, NF-PIC: nuclear fast picroindigocarmine, NOA: nonobstructive azoospermia, Surgery+: sperm seen, Surgery-: no sperm seen.
Of the 251 men who did not show sperm in the initial semen analysis, only 46 men (18.3%) opted for further therapy at the Cleveland Clinic, and underwent microdissection testicular sperm extraction (mTESE) for sperm extraction and intracytoplasmic sperm injection (ICSI). These included 13 men in whom sperm had been detected by NF-PIC, and sperm were found on mTESE in 9/13 (69.2%) of them. The remaining 33 patients did not show sperm after NF-PIC testing. Clinical details of testicular histology, fertilization and pregnancy rates were not available.
DISCUSSION
An accurate diagnosis of azoospermia is important to establish the etiology of the infertility and plan appropriate management options [2,11]. When no sperm are detected in the initial semen evaluation, the sample has to be centrifuged and the pellet examined. The 4th, 5th, and 6th editions of the WHO manual [4,5,6] adopted the definition of azoospermia as first proposed by Eliasson et al [12] in 1981: “no spermatozoa found in the sediment of a centrifuged sample”. The American Urological Association (AUA) defines azoospermia as the absence of sperm from at least two separate centrifuged semen samples, with “no sperm after centrifugation at 3,000 g for 15 minutes and examination of the pellet” [13]. The American Society for Reproductive Medicine (ASRM) guidelines for evaluation of azoospermia diagnose azoospermia when no spermatozoa can be detected on high-powered microscopic examination of a pellet after centrifugation of the seminal fluid on at least two separate occasions [14,15].
Centrifugation helps concentrate rare sperm into a small pellet in order to increase the chances of their detection. The importance of this was demonstrated by Jaffe et al [16] who reported that 22.8% of men with non-obstructive azoospermia and 18.6% of men who had been operated for obstructive azoospermia, with no sperm seen on wet mount light microscopy, had spermatozoa in the pellet produced by centrifugation at 200 g for 10 minutes. Interestingly, sperm were found in the pellet of one sample but not in the pellet from a second sample in 41.2% of the obstructive azoospermic group and 11.8% of the non-obstructive group.
The Cytospin technology used in this study is unique in sedimenting the sample into a small (32 mm2) easily identifiable area for NF-PIC staining [9,17]. Cytospin was originally developed by Shandon and later bought by the company Thermo Scientific. This is an instrument suited for cell concentration by sediment analysis of many fluids. Initially, it was used to analyze the presence of exfoliated germ cells in semen samples for the identification of carcinoma of the testis in situ.
Different centrifugation speeds and times have been used to detect the presence or absence of sperm [17,18,19,20,21] (Table 2), with variable results depending on the centrifugation time and speed [16,22] and volume of the pellet examined. Although WHO 5th Edition recommendation for spinning the neat sample at 3,000 g for 15 minutes was based on the study published by Corea et al [5,19], speed or time was not recommended by the authors of that study. In their study, Corea et al [19] demonstrated that no sperm were seen in the pellets produced at 600 g for 10 minutes. When the supernatant, obtained from the 600 g step, was further centrifuged at 1,000 g for 15 minutes, sperm could be found in the pellet of this sample. The 1,000 g supernatant was then centrifuged at 3,000 g for 15 minutes but no additional sperm were found. Their study concluded that semen samples labelled as azoospermic as per initial wet mount microscopy examination should be centrifuged at a minimum of 1,000 g for 15 minutes to allow adequate sperm detection.
Table 2. Centrifugation speed and time used to confirm azoospermia.
| Reference | Centrifugation | Comment | |
|---|---|---|---|
| Speed | Time (min) | ||
| [18] | 1,000 g | 15 | After centrifugation motility can be lost |
| [2] | 300 g | 7 | Sample centrifuged at 300 g for 7 minutes |
| Cytospin 500 g | 10 | Cytospin at 500 g for 10 minutes | |
| [16] | 200 g | 10 | Whole pellet examined under high-power fields. 18.6% of men with OA and 22.8% of men with NOA before centrifugation had spermatozoa in the pellet |
| [4,5,6] | 3,000 g | 15 | Based on the study by Corea et al [19] |
| [21] | 1,000 g | 15 | Sample centrifuged at least 1,000 g for 15 minutes and the pellet examined under the 40× objective using phase contrast optics |
| [19] | 600 g | 10 | Step 1: Study reported no sperm in the pellets produced at 600 g |
| 1,000 g | 15 | Step 2: Detected spermatozoa in the 600 g supernatants when centrifuged at 1,000 g | |
| 3,000 g | 15 | Step 3: No further sperm-containing samples detected by centrifuging the 1,000 g supernatant at 3,000 g for 15 minutes | |
| The authors concluded that 1,000 g for 15 minutes was adequate for detecting sperm | |||
| [20] | 700 g | 15 | Samples retrieved from NOA patients had positive results in 53.6% after NF-PIC staining |
| Samples retrieved from suspected OA patients had positive results in 14.3% after NF-PIC staining | |||
| [17] | 3,000 g | 15 | Initial detection of sperm |
| 2,000 g | 15 | When no sperm was detected, sample was then prepared by microcentrifugation and stained with NF-PIC for detecting presence of sperm | |
| Concluded that centrifugation at 3,000 g damaged the sperm integrity | |||
NF-PIC: nuclear fast picroindigocarmine, NOA: nonobstructive azoospermia, OA: obstructive azoospermia.
NF-PIC staining after centrifugation for detecting the presence of sperm in an azoospermic sample was first reported in 1998 [2] when the authors could detect sperm in the semen of 9/20 (45%) men with histologically proven testicular failure. The utility of NF-PIC staining was also demonstrated by Tanil et al [20], who compared the outcomes between examination of pelleted semen by wet mount phase contrast microscopy and after NF-PIC staining. Sperm were found in 14.3% of the pellets examined under phase contrast microscopy and in 53.6% of the samples examined after NF-PIC staining. In our present study, comprising of a larger sample size (n=251), sperm were found in 23.9% of men who had been diagnosed as azoospermic using the standard methodology [5].
Alternatively, in a study by Monteiro et al [17], the samples were centrifuged at 3,000 g for 15 minutes. In samples where no sperm were detected, a modified micro-centrifugation technique was used, where the sample was further centrifuged at 2,000 g for 15 minutes. The entire pellet was then spread on a 4×6 mm area of the slide, and stained with NF-PIC. In their study, 148 azoospermic samples were examined and 21 samples (14.2%) were identified as sperm-positive [17].
Some studies have recommended using modified supersensitive fluorescent assays to determine the presence of sperm in azoospermic samples [23,24].
Detection of rare sperm in samples that have been labelled azoospermic has important clinical implications in diagnosis and further management. First, it rules out complete obstruction as a cause of the azoospermia, and establishes a diagnosis of cryptozoospermia due to testicular failure (excepting a rare case of partial obstruction). Second, it suggests that, on the day of oocyte pick-up, the IVF laboratory could conduct an extended search for sperm in the ejaculate for use in ICSI [25]. Third, the detection of rare sperm in the ejaculate may predict a higher chance of sperm retrieval if mTESE is performed. In fact, Alrabeeah et al [26] reported sperm recovery by mTESE in 23 of 24 (95.8%) men with cryptozoospermia. In our study sperm were recovered in 69.2% of apparently azoospermic men when some sperm were detected by NF-PIC. However, these numbers are too small to draw any definitive conclusions.
Limitations of current study
Despite the interesting findings of the current study, few limitations are noted. First, the retrospective nature of this study precluded us from including a control group of patients that used different cytocentrifugation or staining techniques. Second, we have limited follow-up data related to the reproductive outcome of the study population which prevents any conclusion on the role of the NF-PIC technique in predicting the reproductive outcomes of surgically retrieved sperm.
CONCLUSIONS
In men diagnosed with azoospermia by the standard recommended laboratory procedure, a few sperm may yet be identified in the semen following additional centrifugation and staining, thus changing the diagnosis to cryptozoospermia. This has significant clinical implications. In this study, we have demonstrated the utility of Cytospin microcentrifugation combined with NF-PIC staining. The method presented here is simple and rapid, can be implemented by any laboratory, and can be recommended as a useful additional step in the evaluation of azoospermia. Comparison with other methods of centrifugation and staining should be performed in future to determine the best technique for identifying rare sperm in the semen.
Acknowledgements
Authors are thankful to the artist Ken Kula from the Cleveland Clinic’s Center for Medical Art & Photography for his help with the illustrations.
Footnotes
Conflict of Interest: The authors have nothing to disclose.
Funding: The study was supported by the American Center for Reproductive Medicine.
- Conceptualization: AA, RKS, SG.
- Writing – original draft: all the authors.
- Writing – review & editing: all the authors.
Data Sharing Statement
The data analyzed for this study have been deposited in HARVARD Dataverse and are available at https://doi.org/10.7910/DVN/XEKP0P
References
- 1.Jarow JP, Espeland MA, Lipshultz LI. Evaluation of the azoospermic patient. J Urol. 1989;142:62–65. doi: 10.1016/s0022-5347(17)38662-7. [DOI] [PubMed] [Google Scholar]
- 2.Hendin BN, Patel B, Levin HS, Thomas AJ, Jr, Agarwal A. Identification of spermatozoa and round spermatids in the ejaculates of men with spermatogenic failure. Urology. 1998;51:816–819. doi: 10.1016/s0090-4295(98)00007-7. [DOI] [PubMed] [Google Scholar]
- 3.Gudeloglu A, Parekattil SJ. Update in the evaluation of the azoospermic male. Clinics (Sao Paulo) 2013;68(Suppl 1):27–34. doi: 10.6061/clinics/2013(Sup01)04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4th ed. Cambridge: Cambridge University Press; 1999. [Google Scholar]
- 5.World Health Organization (WHO) WHO laboratory manual for the examination and processing of human semen. 5th ed. Geneva: WHO; 2010. [Google Scholar]
- 6.World Health Organization (WHO) WHO laboratory manual for the examination and processing of human semen. 6th ed. Geneva: WHO; 2021. [Google Scholar]
- 7.Aziz N. The importance of semen analysis in the context of azoospermia. Clinics (Sao Paulo) 2013;68(Suppl 1):35–38. doi: 10.6061/clinics/2013(Sup01)05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agarwal A, Gupta S, Sharma R. In: Andrological evaluation of male infertility: a laboratory guide. Agarwal A, Gupta S, Sharma R, editors. Cham: Springer; 2016. Basic semen analysis; pp. 39–46. [Google Scholar]
- 9.Agarwal A, Gupta S, Sharma R. Agarwal A, Gupta S, Sharma R. Andrological evaluation of male infertility: a laboratory guide. Cham: Springer; 2016. Cytospin procedure and nuclear fast red and picroindigocarmine staining procedure for azoospermic sample; pp. 85–91. [Google Scholar]
- 10.Leubitz SS, Savage RA. Sensitivity of picroindigocarmine/nuclear fast red (PIC/NF) stain for detection of spermatozoa: a serial dilution study of human ejaculate. Am J Clin Pathol. 1984;81:90–93. doi: 10.1093/ajcp/81.1.90. [DOI] [PubMed] [Google Scholar]
- 11.Cocuzza M, Alvarenga C, Pagani R. The epidemiology and etiology of azoospermia. Clinics (Sao Paulo) 2013;68(Suppl 1):15–26. doi: 10.6061/clinics/2013(Sup01)03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eliasson R, Burger H, de Kretser D. In: The testis. Burger HG, De Kretser DM, editors. New York: Raven Press; 1981. Analysis of semen; pp. 381–399. [Google Scholar]
- 13.Jarow J, Sigman M, Kolettis PN, Lipshultz LR, McClure RD, Nangia AK, et al. The evaluation of the azoospermic male [Internet] Linthicum (MD): American Urological Association; c2010. [cited 2021 Oct 26]. Available from: https://www.auanet.org/guidelines/archived-documents/azoospermic-male-best-practice-statement . [Google Scholar]
- 14.Practice Committee of American Society for Reproductive Medicine in collaboration with Society for Male Reproduction and Urology. Evaluation of the azoospermic male. Fertil Steril. 2008;90(5 Suppl):S74–S77. doi: 10.1016/j.fertnstert.2008.08.092. [DOI] [PubMed] [Google Scholar]
- 15.Practice Committee of the American Society for Reproductive Medicine in collaboration with the Society for Male Reproduction and Urology. Evaluation of the azoospermic male: a committee opinion. Fertil Steril. 2018;109:777–782. doi: 10.1016/j.fertnstert.2018.01.043. [DOI] [PubMed] [Google Scholar]
- 16.Jaffe TM, Kim ED, Hoekstra TH, Lipshultz LI. Sperm pellet analysis: a technique to detect the presence of sperm in men considered to have azoospermia by routine semen analysis. J Urol. 1998;159:1548–1550. doi: 10.1097/00005392-199805000-00038. [DOI] [PubMed] [Google Scholar]
- 17.Monteiro RA, Pariz JR, Pieri Pde C, Hallak J. An easy, reproducible and cost-effective method for andrologists to improve the laboratory diagnosis of nonobstructive azoospermia: a novel microcentrifugation technique. Int Braz J Urol. 2016;42:132–138. doi: 10.1590/S1677-5538.IBJU.2015.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mortimer D. Laboratory standards in routine clinical andrology. Reprod Med Rev. 1994;3:97–111. [Google Scholar]
- 19.Corea M, Campagnone J, Sigman M. The diagnosis of azoospermia depends on the force of centrifugation. Fertil Steril. 2005;83:920–922. doi: 10.1016/j.fertnstert.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 20.Tanil CT, Queiroz PQ, Braga DPAF, Pasqualotto FF, Iaconelli A, Jr, Borges E., Jr NF-PICS identification of spermatozoa in ejaculated samples previously diagnosed as azoospermia: a prognosis for TESA's recovery spermatozoa. Fertil Steril. 2007;88(Suppl 1):S376 [Google Scholar]
- 21.Nordic Association for Andrology, European Society of Human Reproduction and Embryology-Special Interest Group on Andrology (NAFA, ESHRE-SIGA); NAFA, ESHRE-SIGA, editors. Manual on basic semen analysis 2002. Oxford: Oxford University Press; 2002. Semen analysis - overview; pp. 1–6. [Google Scholar]
- 22.Lindsay KS, Floyd I, Swan R. Classification of azoospermic samples. Lancet. 1995;345:1642. doi: 10.1016/s0140-6736(95)90150-7. [DOI] [PubMed] [Google Scholar]
- 23.Cooper TG, Hellenkemper B, Jonckheere J, Callewaert N, Grootenhuis AJ, Kersemaekers WM, et al. Azoospermia: virtual reality or possible to quantify? J Androl. 2006;27:483–490. doi: 10.2164/jandrol.05210. [DOI] [PubMed] [Google Scholar]
- 24.Centola GM. Determination of male infertility: is the 2010 WHO reference range helpful or confusing? Fertil Steril. 2012;98:1416–1417. doi: 10.1016/j.fertnstert.2012.08.029. [DOI] [PubMed] [Google Scholar]
- 25.Miller N, Biron-Shental T, Pasternak Y, Belenky M, Shefi S, Itsykson P, et al. Fertility outcomes after extended searches for ejaculated spermatozoa in men with virtual azoospermia. Fertil Steril. 2017;107:1305–1311. doi: 10.1016/j.fertnstert.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Alrabeeah K, Wachter A, Phillips S, Cohen B, Al-Hathal N, Zini A. Sperm retrieval outcomes with microdissection testicular sperm extraction (micro-TESE) in men with cryptozoospermia. Andrology. 2015;3:462–466. doi: 10.1111/andr.12000. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data analyzed for this study have been deposited in HARVARD Dataverse and are available at https://doi.org/10.7910/DVN/XEKP0P