Abstract
Objectives:
The COVID-19 pandemic has propelled the use of technology for health care services delivery. Because of inequities in health care and technology access, we investigated the use of telehealth services among racial and ethnic minority groups before and during the COVID-19 pandemic.
Methods:
For this retrospective study, we examined the electronic health records of privately insured patients in the Healthjump database, provided by the COVID-19 Research Database Consortium. We examined 17.98 million unique visit records of 2.93 million patients from March through December 2019 and 22.17 million records of 3.55 million patients from March through December 2020. We conducted a descriptive analysis and used multiple logistic regression to examine differences in the use of telehealth services among 3 racial and ethnic groups: non-Hispanic White, non-Hispanic Black, and Hispanic people.
Results:
Telehealth visits before and during COVID-19 accounted for 8.3% and 10.9% of total visits, respectively, with a peak of 15.5% in April 2020. Pre–COVID-19, Hispanic patients had a significantly lower monthly utilization rate (5.3%) than non-Hispanic White patients (8.4%, P < .001) and non-Hispanic Black patients (10.4%, P = .001). During the pandemic study period, Hispanic patients were 41% less likely than non-Hispanic White patients to have a telehealth visit, controlling for age and sex.
Conclusions:
The likelihood of using telehealth was lower among Hispanic patients than among non-Hispanic White and non-Hispanic Black patients during the pandemic. Culturally sensitive measures are needed to support telehealth use among the Hispanic population.
Keywords: telehealth, health care access, inequity, disparities, COVID-19
The widespread transmission and impact of COVID-19 ushered in unprecedented challenges to public health. To mitigate the spread of COVID-19 and promote public health and safety, public health officials reduced the amount of in-person health care visits. Telehealth services were quickly supported to increase access to care when in-person visits were not in the best interest of public health. Through legislative measures and reimbursement practices, the United States had overwhelming support for telehealth services to facilitate access to care during the COVID-19 pandemic. In March 2020, the Centers for Medicare & Medicaid Services encouraged health professionals to use telehealth to provide access to health care services and granted pay parity between telehealth and in-person visits. 1 However, the support and use for telehealth services must be accompanied by outcomes that contribute to equity in access.
The contribution of technology to support health care access during COVID-19 cannot be underestimated. Telehealth is a promising tool because of its potential to increase access to care by overcoming geographical barriers and provide virtual care; it is increasing in acceptance as the standard of care. 2 The Health Resources & Services Administration defines telehealth as “the use of electronic information and telecommunication technologies to support long-distance clinical health care, patient and professional health-related education, health administration, and public health.” 3 Telehealth includes a range of virtual communications: telephone calls, remote monitoring, and video conferencing. 4 Along with reducing exposure to health care providers and patients, telehealth has been important during the pandemic to improve access to health and social services. 5 However, given the range of health disparities across the United States, it is reasonable to assume that not all people benefit from using telehealth. Strategies to mitigate inequities during COVID-19 must address systemic risk to populations that are vulnerable to adverse health outcomes; without this attention, legislative and reimbursement support for telehealth may not benefit members in society who do not have access to health care services. 6 Communities with low incomes are at greater risk for health inequities than communities with high incomes because of higher rates of chronic conditions, fewer financial resources, and inadequate living conditions. Because of the lack of resources, many people who have low incomes and who identify as a member of a racial or ethnic minority population do not have access to adequate technological support that encourages telehealth use. Despite the overwhelming support for telehealth during the pandemic, it is reasonable to suspect that people who lacked access to telehealth before the COVID-19 pandemic would lack access during the pandemic.
If today’s society is to support public health, equal access to telehealth resources for all people must be a priority. To achieve health equity among racial and ethnic groups, technology-based resources should be comprehensively addressed to ensure that all groups have access to all platforms for care. Previous research suggests that telehealth use is associated with patient age, sex, and race. 7 Several studies suggest that people in racial and ethnic minority groups are less likely than non-Hispanic White people to use technology for health-related purposes.6 -8 Hispanic and non-Hispanic Black people are less likely than non-Hispanic White people to have access to and use health care. 9 These findings are important as we seek to promote telehealth use during a public health crisis without exacerbating health inequities among racial and ethnic minority populations.
Preliminary studies in the early stages of the COVID-19 pandemic indicated substantial differences in telehealth use among racial and ethnic groups. One study concluded that Hispanic and non-Hispanic Black people were less likely than non-Hispanic White people to use telehealth services during the first few months of COVID-19. 10 Likewise, a study in 2020 found that non-Hispanic White people were more likely than Hispanic and non-Hispanic Black people to have telehealth visits, with inconclusive results about Asian people. 11 In a 2021 study, Hispanic patients had the highest rate of missed telehealth audio and video appointments, and non-Hispanic Black patients were more likely than non-Hispanic White patients to complete a telehealth audio visit. 12 Another 2021 study reported that Hispanic and non-Hispanic Black people had significantly lower rates of telemental health use than non-Hispanic White people. 13
In contrast, other studies suggested that Hispanic and non-Hispanic Black people used telehealth at higher rates than non-Hispanic White people and that race or ethnicity was not a substantial factor in telehealth use. 10 A 2021 study found that non-Hispanic Black people were more likely than non-Hispanic White people to have telehealth visits, especially during the first weeks of the COVID-19 pandemic. 14 Two studies (one in 2020 and another in 2021) reported that Asian survey respondents were less likely than non-Hispanic White survey respondents to have a telehealth visit.4,15 Although studies examined telehealth use before COVID-19 and during the first few months of COVID-19, little information on trends in the use of telehealth before and during COVID-19 has been published. Our study objective was to examine the use of telehealth services among racial and ethnic minority groups before and during the pandemic. Findings from this study will improve our understanding of the impact of COVID-19 on telehealth use among racial and ethnic minority groups. It will also help to inform culturally sensitive telehealth programs that may overcome barriers to the use of telehealth.
Methods
Data Source
The COVID-19 Research Database Consortium provided data for this study. The consortium, organized by Datavant, consists of private and public partners across industries to facilitate access to data and support knowledge sharing. 16 The COVID-19 Research Database was established with institutional review board approval from the Western Institutional Review Board and an exemption from patient consent due to the use of HIPAA-certified deidentified data (Health Insurance Portability and Accountability Act of 1996), HIPAA limited data, or non–HIPAA-covered data, with the strong governance measures in place to control access to all data. This exemption covers all research performed in the COVID-19 Research Database. The database reflects a cross-industry collaborative comprising various institutions donating technology resources, health care expertise, and deidentified data to help communities better understand the COVID-19 pandemic. 16 The study period was March–December 2019 and March–December 2020. Healthjump is a part of the partnership that permits access, with approval, to the database. 16 Healthjump is a data management platform that contains patients’ electronic medical record (EMR) data across outpatient and ambulatory settings for privately insured patients. 16 The Healthjump database consists of records from multiple EMR platforms and is standardized to facilitate interoperability.17,18 The database contains EMRs from all regions in the United States; however, limitations exist in representation from New England and West North Central states. 18
Statistical Methods
We examined 17.98 million unique visit records of 2.93 million unique patients from March through December 2019 and 22.17 million unique visit records of 3.55 million unique patients from March through December 2020. The data consisted only of patients who had health visits during the study period, not the entire patient population. We performed a retrospective study on 3 racial and ethnic groups: non-Hispanic White, non-Hispanic Black, and Hispanic. We used R software version 4.1.0 (R Foundation for Statistical Computing) to perform descriptive analysis and multiple logistic regression to examine the study objective. We identified telehealth encounters by looking for encounter (visit) types that contained “tel” to include telephone, televisit, telemedicine, and telehealth. Telehealth definitions are not consistent across studies. Telehealth comprises 2 forms—asynchronous (patient and health care provider do not meet in real time) and synchronous (real-time meeting)—and does not focus only on audio or video modes. Because of rapid changes in telehealth use during COVID-19, it was important that we included all modes of telehealth. 14 The definition of telehealth in this study aligns with other studies that cite synchronous and asynchronous forms when the use of in-person (nontelehealth) visits is being compared as a dichotomous outcome (yes or no to telehealth use).12,14,19 Other studies defined telehealth as telephone, audio, or video visits.7,20
We calculated the percentage of telehealth visits per month among the 3 racial and ethnic groups. We conducted paired t tests to compare the monthly use of telehealth among the groups during the study period, with P < .05 considered significant. In the logistic regression analysis, we adjusted the odds ratios (ORs) of telehealth use for the effects of independent variables, such as race and ethnicity, age group, and sex. We also aggregated visits during the period to the patient level. The dependent variable was a binary variable, whether or not a patient used telehealth during the study period. A patient with ≥1 telehealth visit during the study period was assigned a value of 1 for the dependent variable, otherwise 0. We adjusted the logistic regression analysis with clustered SEs to include the potential effects of the number of visits. Furthermore, we conducted within–age group analysis to examine how sex, race and ethnicity, and year of visit are associated with use of telehealth in each age group.
Results
Telehealth visits accounted for 8.3% of all visits before the COVID-19 pandemic (March–December 2019) and 10.9% of all visits during the pandemic (March–December 2020) (Table 1). The average number of overall visits per patient (March–December 2019) was approximately 6.6 for non-Hispanic White, 6.5 for non-Hispanic Black, and 4.1 for Hispanic patients. The average number of visits per patient during the pandemic, as compared with before the pandemic, was approximately 2.0% higher among non-Hispanic White patients (6.7 visits), 0.1% lower among non-Hispanic Black patients (6.5 visits), and 0.1% lower among Hispanic patients (4.1 visits). Hispanic patients had fewer visits per person than non-Hispanic White and non-Hispanic Black patients before and during the pandemic.
Table 1.
Description of visits and patients before and during the COVID-19 pandemic, in a study of racial and ethnic differences in the use of telehealth, United States, March–December 2019 and March–December 2020 a
| No. of unique visits | Visits that were telehealth visits, % | No. of unique patients | Patients who used telehealth, % | |||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | 2019 | 2020 |
| Total | 17 983 700 | 22 165 474 | 8.3 | 10.9 | 2 934 389 | 3 549 838 | 12.6 | 18.9 |
| Sex | ||||||||
| Female | 10 730 370 | 13 209 988 | 8.7 | 11.4 | 1 674 006 | 2 022 194 | 13.2 | 19.5 |
| Male | 7 252 379 | 8 954 329 | 7.8 | 10.2 | 1 260 069 | 1 527 332 | 11.8 | 18.2 |
| Unknown | 951 | 1157 | 14.7 | 11.2 | 314 | 312 | 10.0 | 6.6 |
| Race and ethnicity | ||||||||
| Non-Hispanic Black | 2 762 239 | 3 267 344 | 10.5 | 13.4 | 425 249 | 503 691 | 19.6 | 22.1 |
| Hispanic | 2 288 598 | 2 577 688 | 5.4 | 9.1 | 554 777 | 628 099 | 6.7 | 12.8 |
| Non-Hispanic White | 12 932 863 | 16 320 442 | 8.4 | 10.7 | 1 954 363 | 2 418 048 | 12.8 | 19.8 |
Data source: COVID-19 Research Database. 16
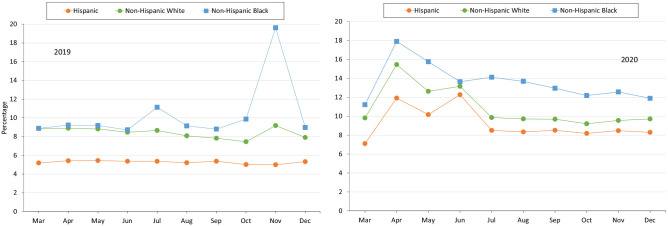
From March through December 2020, the overall mean percentage of telehealth visits per month was 11.1%, and the monthly percentage peaked at 15.5% in April 2020 (Figure 1). In 2019, the overall mean percentage of telehealth visits per month among non-Hispanic Black patients was 10.4%, and the monthly percentage peaked at 19.6% in November (Figure 2). Paired t tests suggest that the overall mean percentage of telehealth visits per month was significantly higher among non-Hispanic Black patients than among non-Hispanic White patients (10.4% vs 8.4%, P = .04) and Hispanic patients (5.3%, P = .001) in 2019. From March through December 2020, the overall mean percentage of telehealth visits per month among non-Hispanic Black patients was 13.6%, and the monthly percentage peaked at 17.9% in April 2020. The paired t test of the differences in the percentage of monthly telehealth visits between non-Hispanic Black and non-Hispanic White patients showed no significant change in disparity during the pandemic (P = .21).
Figure 1.
Number and percentage of unique telehealth visits per month before and during the COVID-19 pandemic, United States, March–December 2019 and March–December 2020. Data include patients who had a health visit during the study period. Data source: COVID-19 Research Database. 16
Figure 2.
Use of telehealth per month, by race and ethnicity, before and during the COVID-19 pandemic, United States, March–December 2019 and March–December 2020. Data include patients who had a health visit during the study period. Data source: COVID-19 Research Database. 16
In the pre–COVID-19 period, the overall mean percentage of telehealth visits per month was significantly lower among Hispanic patients (5.3%) than among non-Hispanic White patients (8.4%, P < .001) and non-Hispanic Black patients (10.4%, P = .001). During the pandemic, Hispanic patients increased their use of telehealth to an average of 9.2%. The paired t test of the differences in the percentage of monthly telehealth visits between Hispanic and non-Hispanic White patients suggests that the disparity decreased during the pandemic (mean of differences: 3.0% in 2019, 1.7% in 2020; P < .001). However, the percentage of monthly telehealth visits among Hispanic patients was still significantly lower than among non-Hispanic White (10.9%) and non-Hispanic Black (13.6%) patients.
The results of the logistic regression showed a significant association between telehealth use and each predictor (P < .01 for all) (Table 2). Hispanic patients were less likely than non-Hispanic White patients to have a telehealth visit in the pre–COVID-19 period (OR = 0.48; 95% CI, 0.47-0.48). During the pandemic, the OR increased to 0.59 (95% CI, 0.58-0.59), suggesting that the disparity narrowed. However, in 2020, Hispanic patients were still 41% less likely than non-Hispanic White patients to have a telehealth visit after accounting for the effects of sex and age. Non-Hispanic Black patients were more likely than non-Hispanic White patients to have a telehealth visit pre–COVID-19 (OR = 1.59; 95% CI, 1.58-1.60) and during the pandemic (OR = 1.12; 95% CI, 1.12-1.13). In general, male patients had lower odds than female patients of using telehealth pre–COVID-19 (OR = 0.89; 95% CI, 0.88-0.90) and during the pandemic (OR = 0.92; 95% CI, 0.92-0.93). Patients in younger age groups (<18, 18-44, 45-64 years) were more likely to use telehealth than patients aged ≥65 years.
Table 2.
Odds ratios of using telehealth before and during the COVID-19 pandemic, by age, sex, and race and ethnicity, United States, March–December 2019 and March–December 2020 a
| Odds ratio (95% CI) b | ||
|---|---|---|
| Characteristic | March–December 2019 | March–December 2020 |
| Age, y | ||
| <18 | 1.24 (1.22-1.25) | 0.96 (0.95-0.97) |
| 18-44 | 1.47 (1.46-1.48) | 1.29 (1.28-1.30) |
| 45-64 | 1.22 (1.20-1.23) | 1.14 (1.13-1.15) |
| ≥65 | 1 [Reference] | 1 [Reference] |
| Sex | ||
| Male | 0.89 (0.88-0.90) | 0.92 (0.92-0.93) |
| Female | 1 [Reference] | 1 [Reference] |
| Race and ethnicity | ||
| Non-Hispanic Black | 1.59 (1.58-1.61) | 1.12 (1.117-1.13) |
| Hispanic | 0.48 (0.47-0.48) | 0.59 (0.58-0.59) |
| Non-Hispanic White | 1 [Reference] | 1 [Reference] |
Data source: COVID-19 Research Database. 16
All coefficient P values are < .01, as determined by multiple logistic regression.
The within–age group analysis suggested that sex, race and ethnicity, and year of visit were significantly associated with use of telehealth in each age group (P < .01 for all), except for sex in the group aged <18 years (P = .16) (Table 3). Hispanic patients in the group aged ≥65 years were least likely (OR = 0.40; 95% CI, 0.40-0.41) to have a telehealth visit. The OR increased in younger groups of Hispanic patients. Non-Hispanic Black patients were most likely (OR = 1.36; 95% CI, 1.35-1.38) to have a telehealth visit in the group aged 18-44 years. All age groups showed higher ORs of having telehealth visits during the pandemic than before COVID-19.
Table 3.
Odds ratios of using telehealth before and during the COVID-19 pandemic within each age group, by sex, race and ethnicity, and year, United States, March–December 2019 and March–December 2020 a
| Age group, y b | ||||
|---|---|---|---|---|
| Characteristic | ≥65 | 45-64 | 18-44 | <18 |
| Sex | ||||
| Male | 0.97 (0.96-0.98) | 0.93 (0.92-0.94) | 0.81 (0.80-0.81) | 1.01 (1.00-1.02) c |
| Female | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Race and ethnicity | ||||
| Non-Hispanic Black | 1.33 (1.31-1.34) | 1.33 (1.32-1.34) | 1.36 (1.35-1.38) | 1.06 (1.04-1.08) |
| Hispanic | 0.40 (0.40-0.41) | 0.54 (0.53-0.55) | 0.62 (0.61-0.62) | 0.69 (0.68-0.71) |
| Non-Hispanic White | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Year | ||||
| 2020 | 1.78 (1.77-1.80) | 1.64 (1.63-1.65) | 1.52 (1.51-1.53) | 1.33 (1.32-1.35) |
| 2019 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
Data source: COVID-19 Research Database. 16 All values are odds ratio (95% CI).
All coefficient P values are <.01, unless otherwise noted, as determined by multiple logistic regression.
P = .16.
Discussion
The COVID-19 pandemic propelled an extraordinary need to use telehealth systems to provide health-related services in a way that mitigates the spread of infection. The analysis presented here demonstrates trends in telehealth use before and during the pandemic. Hispanic patients in our study were significantly less likely than non-Hispanic White and non-Hispanic Black patients to have telehealth visits before the pandemic. Hispanic patients remained significantly less likely than non-Hispanic White and non-Hispanic Black patients to use telehealth visits. Throughout the study period, non-Hispanic Black patients were significantly more likely than non-Hispanic White patients to use telehealth visits.
The results of our study have several implications for participation in telehealth care delivery. We saw an overall rise in the number of telehealth visits among all people regardless of their racial and ethnic identification. The increase in telehealth use aligns with prior research.4,15,21,22 Studies reported that the number of telemedicine visits significantly increased during the pandemic, while the number of in-office visits declined.4,15,21,22 Two studies noted that telehealth use was higher among female patients than among male patients, similar to our study.4,15 Decreased telehealth use among Hispanic people was also reported by Reed et al, Wegermann et al, and Campos-Castillo and Anthony.7,12,14 However, Weber et al found that Hispanic people had higher odds of using telehealth than non-Hispanic Black people. 23 Non-Hispanic Black people were more likely to use telehealth before than during COVID-19. Campos-Castillo and Anthony suggested that the heightened perceived intensity of the pandemic’s threat promoted telehealth use among non-Hispanic Black people. 14 Chunara et al indicated that the uptake in telehealth access was due to the increased access by young non-Hispanic Black females who were concerned about COVID-19. 19 Researchers stated that non-Hispanic Black females were also sicker than their non-Hispanic White female counterparts when they sought care.14,19
Hispanic people collectively rank as the largest ethnic minority group in the United States, and this group is expected to grow. However, the rate of telehealth use among Hispanic people is lower than the rate among other racial and ethnic groups. 24 Hispanic people may have unique barriers to accessing technology-enabled resources due to acculturation and language. 25 Studies suggest that people with limited English proficiency use telehealth (telephone or video visits) less frequently than people who are proficient in English. 26 Overall, in our study, Hispanic patients had fewer visits per patient than non-Hispanic White and non-Hispanic Black patients (telehealth or in person). Prior research suggested that health literacy, language barriers, and the occupations of many Hispanic adults (often low-wage hourly jobs) create hurdles for health care visits.27,28 Non-Hispanic Black patients had fewer visits per patient in 2019 than in 2020, but their use of telehealth services increased. Edward et al found that non-Hispanic Black patients’ use of health care services has declined since 2012. 28 Although it is beyond the scope of this study, further research is warranted to investigate potential racial and ethnic disparities in overall health care use and their impact on telehealth adoption among people who identify as members of racial or ethnic minority groups.
Public Health Implications
While public health policy promotes the use of telehealth, a disparity in use among members of racial and ethnic minority groups persists. Prior research suggests that when health care providers employ telehealth technologies, people who engage with the technology show an improvement in smoking cessation, medication adherence, counseling attendance, and hypertension management. 29 Inequitable access to telehealth will eventually lead to suboptimal health outcomes such as complications and death. Without patient engagement, people who have decreased access to health care services will experience a greater divide in health equity. This divide is concerning because we have aggressively moved toward technology-enabled care delivery models and will continue to advance technology for the foreseeable future.
We can promote access to telehealth services by increasing access to health insurance. A previous study indicated that Hispanic people were more concerned about lack of health insurance than the physical absence of the physician, confidentiality, and privacy. 30 Second, by increasing access to health insurance, we promote access to health care providers and, subsequently, telehealth. Hispanic people are less likely than non-Hispanic White people to have a primary care provider. 28 Having a primary source of care affects access to telehealth because many telehealth services may require primary care referral. 26 Third, our findings have implications for promoting the use of culturally sensitive telehealth to promote equity in access. As such, it may be necessary for supportive programs and interventions to address barriers to telehealth in some communities.
Strengths and Limitations
Our study used a unique population-based data source and conducted a comprehensive evaluation of the relationship between race and ethnicity and telehealth use. It updates telehealth studies that were conducted during the early stages of the pandemic. However, the results of our study should be considered in light of some limitations. First, this study identified a patient sample by using the EMR in the Healthjump database and is subject to limitations of administrative databases. Second, our sample consisted of patients with private health insurance and may not be generalizable to other patient groups, such as those with traditional Medicare or Medicaid coverage. Third, the prevalence of telehealth visits among all visits varied among studies because of the use of different data sources. Jaffe et al identified 0.2% of all visits as telehealth visits in March 2019 and 1.9% in March 2020 by using Kantar’s Claritis database. 15 Patel et al examined outpatient visits in the OptumLabs Data Warehouse and reported that 30.1% of all visits were telehealth visits. 31 Jaffe et al examined race, ethnicity, and sex but did not find these factors to be significantly associated with telehealth use; the authors identified outpatient visits by using Medicare’s expanded list of outpatient Current Procedural Terminology codes. We used the code for encounter type in the Healthjump database, which may be one cause for the discrepancy in telehealth percentages. 15 The spike in November 2019 was caused by an abnormally increased number of encounters recorded by 1 service provider (clients and patients are blinded in the dataset). Although we attempted to adequately differentiate among types of telehealth used during telehealth visits, we found the visit type “tel” to be more reliable than Current Procedural Terminology codes.
Conclusion
Our study identified an unfavorable trend in the use of telehealth among Hispanic patients. Future studies need to examine factors that contribute to low rates of telehealth use in this group. Factors such as demographic characteristics, geography, socioeconomic characteristics, education levels, culture, and health behaviors may contribute to the low levels of use among racial and ethnic minority populations. By investigating these factors, we will be able to determine the factors that contribute to the digital divide that may deepen health inequities. These findings will assist community leaders and policy makers to provide a more robust public health infrastructure that supports access to technology and enhances health care equity among racial and ethnic minority communities. While the use of telehealth is an important consideration to overcome digital inequities, future studies should also specify disparities among types of telehealth and their effects on quality outcomes.
Despite the removal of regulatory and reimbursement barriers to telehealth, we found that trends in the use of telehealth were largely unchanged from the pre–COVID-19 period to the COVID-19 period. Groups that used telehealth before the pandemic were more likely than groups that did not use telehealth before the pandemic to use telehealth during the pandemic. By identifying groups that are not accessing telehealth, we recommended strategies and policy interventions to educate and direct resources to racial and ethnic minority groups to promote the use of telemedicine services. The pandemic has highlighted the importance of digital platforms in health care access. Without proactive interventions that are culturally sensitive, barriers that existed before the pandemic will remain after the pandemic. Increasing access to telehealth must go beyond policy promulgation and include actionable interventions that encourage racial and ethnic minority groups to use telehealth.
Acknowledgments
The authors thank the COVID-19 Research Database Consortium for their support during this project.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Cynthia White-Williams, PhD, MHA, PT  https://orcid.org/0000-0002-8344-7427
https://orcid.org/0000-0002-8344-7427
References
- 1. Centers for Medicare & Medicaid Services. Telehealth. Accessed June 25, 2021. https://www.medicare.gov/coverage/telehealth [PubMed]
- 2. Centers for Disease Control and Prevention. Telehealth and telemedicine. Updated July 8, 2020. Accessed June 25, 2021. https://www.cdc.gov/phlp/publications/topic/telehealth.html
- 3. HealthIT.gov. What is telehealth? How is telehealth different from telemedicine? October 17, 2019. Accessed December 12, 2021. https://www.healthit.gov/faq/what-telehealth-how-telehealth-different-telemedicine
- 4. Zhang D, Shi L, Han X, et al. Disparities in telehealth utilization during the COVID-19 pandemic: findings from a nationally representative survey in the United States. J Telemed Telecare. Published online October 11, 2021. doi: 10.1177/1357633X211051677 [DOI] [PubMed] [Google Scholar]
- 5. Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382(18):1679-1681. doi: 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 6. Peek ME, Simons RA, Parker WF, Ansell DA, Rogers SO, Edmonds BT. COVID-19 among African Americans: an action plan for mitigating disparities. Am J Public Health. 2021;111(2):286-292. doi: 10.2105/AJPH.2020.305990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Reed ME, Huang J, Graetz I, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open. 2020;3(6):e205873. doi: 10.1001/jamanetworkopen.2020.5873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mitchell UA, Chebli PG, Ruggiero L, Muramatsu N. The digital divide in health-related technology use: the significance of race/ethnicity. Gerontologist. 2019;59(1):6-14. doi: 10.1093/geront/gny138 [DOI] [PubMed] [Google Scholar]
- 9. Ray R, Sewell AA, Gilbert KL, Roberts JD. Missed opportunity? Leveraging mobile technology to reduce racial health disparities. J Health Polit Policy Law. 2017;42(5):901-924. doi: 10.1215/03616878-3940477 [DOI] [PubMed] [Google Scholar]
- 10. Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. Published online October 21, 2020. doi: 10.1177/1357633X20963893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Smith CB, Bhardwaj AS. Disparities in the use of telehealth during the COVID-19 pandemic. J Clin Oncol. 2020;38(29):87. doi: 10.1200/JCO.2020.38.29_suppl.87 [DOI] [Google Scholar]
- 12. Wegermann K, Wilder JM, Parish A, et al. Racial and socioeconomic disparities in utilization of telehealth in patients with liver disease during COVID-19. Dig Dis Sci. 2022;67(1):93-99. doi: 10.1007/s10620-021-06842-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ruprecht MM, Wang X, Johnson AK, et al. Evidence of social and structural COVID-19 disparities by sexual orientation, gender identity, and race/ethnicity in an urban environment. J Urban Health. 2021;98(1):27-40. doi: 10.1007/s11524-020-00497-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Campos-Castillo C, Anthony D. Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: a secondary analysis of a US survey of internet users from late March. J Am Med Inform Assoc. 2021;28(1):119-125. doi: 10.1093/jamia/ocaa221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jaffe DH, Lee L, Huynh S, Haskell TP. Health inequalities in the use of telehealth in the United States in the lens of COVID-19. Popul Health Manag. 2020;23(5):368-377. doi: 10.1089/pop.2020.0186 [DOI] [PubMed] [Google Scholar]
- 16. COVID19researchdatabase.org. COVID-19 Research Database. Accessed May 12, 2021. https://covid19researchdatabase.org
- 17. Ziedan E, Simon KI, Wing C. Effects of state COVID-19 closure policy on non–COVID-19 health care utilization. National Bureau of Economic Research. July 2020. Accessed December 10, 2021. https://www.nber.org/papers/w27621 [Google Scholar]
- 18. Anderson TS, O’Donoghue AL, Dechen T, Herzig SJ, Stevens JP. Trends in telehealth and in-person transitional care management visits during the COVID-19 pandemic. J Am Geriatr Soc. 2021;69(10):2745-2751. doi: 10.1111/jgs.17329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chunara R, Zhao Y, Chen J, et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc. 2021;28(1):33-41. doi: 10.1093/jamia/ocaa217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reay RE, Looi JC, Keightley P. Telehealth mental health services during COVID-19: summary of evidence and clinical practice. Australas Psychiatry. 2020;28(5):514-516. doi: 10.1177/1039856220943032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cantor JH, McBain RK, Pera MF, Bravata DM, Whaley CM. Who is (and is not) receiving telemedicine care during the COVID-19 pandemic? Am J Prev Med. 2021;61(3):434-438. doi. 10.1016/j.amepre.2021.01.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Whaley CM, Pera MF, Cantor J, et al. Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA Netw Open. 2020;3(11):e2024984. doi: 10.1001/jamanetworkopen.2020.24984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Weber E, Miller SJ, Astha V, Janevic T, Benn E. Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J Am Med Inform Assoc. 2020;27(12):1949-1954. doi: 10.1093/jamia/ocaa216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Martinez M, Perle JG. Reaching the Latino population: a brief conceptual discussion on the use of telehealth to address healthcare disparities for the large and growing population. J Technol Behav Sci. 2019;4(3):267-273. doi: 10.1007/s41347-019-00088-9 [DOI] [Google Scholar]
- 25. Agate S. Unlocking the power of telehealth: increasing access and services in underserved, urban areas. Harvard J Hispan Policy. 2017;29:85-96. [Google Scholar]
- 26. Rodriguez JA, Saadie A, Schwamm LH, Bates DW, Samal L. Disparities in telehealth use among California patients with limited English proficiency. Health Aff (Millwood). 2021;40(3):487-495. doi: 10.1377/hlthaff.2020.00823 [DOI] [PubMed] [Google Scholar]
- 27. Perreira KM, Allen C, Oberlander J. Access to health insurance and health care for Hispanic children in the United States. Ann Am Acad Polit Soc Sci. 2021;696(1):223-244. doi: 10.1177/00027162211050007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Edward J, Morris S, Mataoui F, Granberry P, Williams MV, Torres I. The impact of health and health insurance literacy on access to care for Hispanic/Latino communities. Public Health Nurs. 2018;35(3):176-183. doi: 10.1111/phn.12385 [DOI] [PubMed] [Google Scholar]
- 29. Crilly P, Kayyali R. A systematic review of randomized controlled trials of telehealth and digital technology use by community pharmacists to improve public health. Pharmacy (Basel). 2020;8(3):137. doi: 10.3390/pharmacy8030137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sohn H. Racial and ethnic disparities in health insurance coverage: dynamics of gaining and losing coverage over the life-course. Popul Res Policy Rev. 2017;36(2):181-201. doi: 10.1007/s11113-016-9416-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Patel SY, Mehrota A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff (Millwood). 2021;40(2):349-358. doi: 10.1377/hlthaff.2020.01786 [DOI] [PMC free article] [PubMed] [Google Scholar]