Abstract
Introduction
The hydrogel Scleral Buckle is a soft and pliable subtype of buckles which has been used to repair retinal breaks and detachments externally. This case represents an unusual late orbital complication of the implant.
Case report
A 70 years old male patient presented with drooping right upper lid and eye misalignment, associated with foreign body sensation and discomfort. The patient underwent scleral buckle surgery for a rhegmatogenous retinal detachment 32 years before his presentation using a hydrogel MIRAgel® explant. Orbital imaging showed a large cystic lesion in the superolateral quadrant of the orbit indicating a fluid-filled explant.
Discussion
In patients who were treated with hydrogel MIRAgel® explant for retinal breaks or detachments, detailed ophthalmic history, particular past eye surgery history, and examination, orbital imaging, and good clinical documentation. Serious orbital and neurological conditions need to be ruled out carefully.
Conclusion
Late orbital complications of hydrogel MIRAgel® explant might develop late after surgery and might represent a diagnostic challenge for ophthalmologists.
Keywords: Hydrogel sclera explant, MIRAgel, Buckle complication, Retinal surgery
Highlights
-
•
This report shows the late complications associated with hydrogel MIRAgel® explants.
-
•
These complications might represent diagnostic challenges for physicians and ophthalmologists.
-
•
Proper history, physical examination and orbital imaging help to lead to the correct diagnosis.
1. Introduction
To achieve success in managing rhegmatogenous retinal detachments (RRD), it is needed to localize and seal all retinal breaks which could be found in these cases [1]. In the modern era of retinal surgery, this can be achieved either by external or internal approaches. One of the external approaches is sclera buckle (SB) surgery. In SB, the eyewall is indented toward the vitreous to support and close retinal breaks and relieve the forces of vitreous tractions. Jess first used scleral buckle in 1937 as a temporal measurement attempted to counteract the hypotony secondary to SRF drainage, for which cotton swab was used previously [2]. However, Ernst Custodis was the first surgeon to perform a scleral buckling procedure using an episcleral explant in 1949 [2]. Custodis used a polyviol explant to buckle the sclera. Retinal breaks were treated with diathermy, and a non-drainage subretinal fluid procedure was used. He reported a success rate of 83.3 % in consecutive series of 515 patients [3]. Since then, various materials have been used for scleral buckling, including fascia lata, palmaris tendon, plantaris tendon, knee cartilage, donor sclera, dura mater, polyviol, polyethylene, encircling non-absorbable and absorbable sutures, gelatin, hydrogel, and silicone [4]. In the mid-1980s, the hydrogel buckle came to market (methylacrylate-2-hydroxyethylacrylate) (MIRAgel, Mira) ®. It was promoted because of its soft and pliable characteristics, besides its ability to absorb and release antibiotics made it advantageous due to less infection rates compared to silicon buckles [5]. In addition, it was meant to be hydrated by tissue fluids, allowing it to enlarge postoperatively and increase buckle height. Despite these advantages, many years later after its introduction, rmany side effects were reported, mainly related to hydrolytic degradation of the MIRAgel material; it undergoes progressive swelling even to several times its original size. This can lead to swelling-related complications like ptosis, strabismus, infection around the buckle, sclera erosion, orbital complications, and others [6], [7]. The aim of this report is to document the late complications and the associated diagnostic challenges associated with the hydrogel MIRAgel® explant. This case report is as per the SCARE-2020 criteria [8].
2. Case report
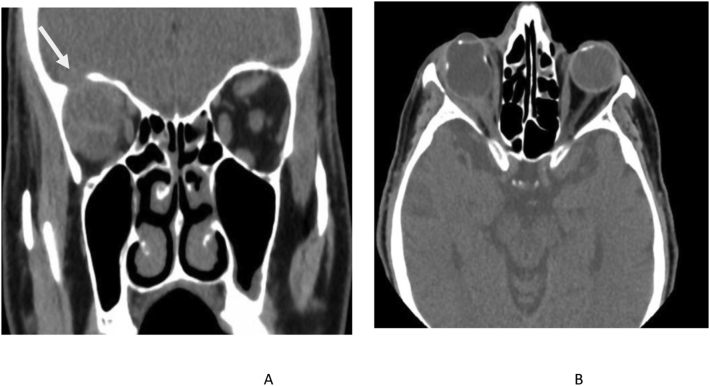
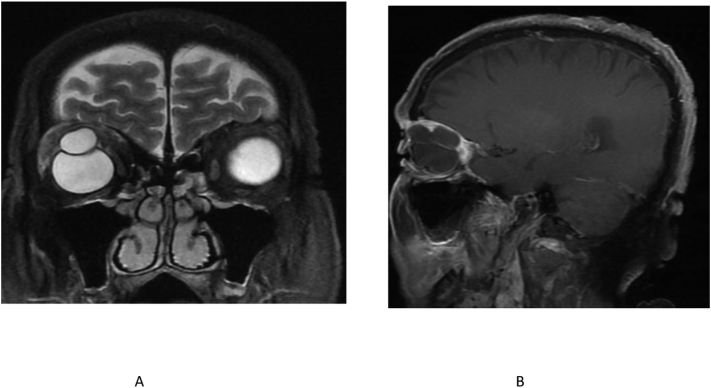
A 70 years old male patient presented to the ophthalmology clinic complaining of a 7-month drooping of the right upper lid and eye misalignment, as well as foreign body sensation and discomfort. No history of trauma or neurological symptoms. The patient underwent scleral buckle surgery for a rhegmatogenous retinal detachment 32 years before his presentation outside our facility. Upon reviewing his old chart, the surgery resulted in retinal reattachment with good postoperative visual recovery. A hydrogel MIRAgel® explant (MIRA, Waltham, MA, USA) was used. Two years later the buckle slightly got enlarged and moved slightly inferiorly displacing the globe. It was considered a consequence of scleral buckle surgery, and no intervention was advised as fibrosis and adhesions had taken place with no signs of migration, exposure, or infection. The patient lost his follow-up until his current presentation. His visual acuity was 20/100 in the right eye, which was the only-seeing eye; there was ptosis (Fig. 1) with limited levator function. The right globe was hypotropic and esotropic, with restriction of eye movement in all directions except adduction. Slit-lamp biomicroscopic examination showed the scleral buckle in the superotemporal fornix, with the overlying conjunctiva appearing intact. No signs of inflammation or globe tenderness, the pupil was normal in size with no relative afferent pupillary defect, the anterior segment was deep and quiet, the intraocular lens was in place in the posterior chamber, and fundoscopy examination showed a myopic flat retina with a superior indentation caused by the explant. The patient underwent a non-contrast CT scan study, and it showed a large cystic lesion in the superolateral quadrants of the orbit surrounding the scleral buckle indenting and deforming the globe superiorly associated with a bone defect in the related part of the orbital roof appearing to erode into the anterior cranial fossa (Fig. 2). Multi-planar magnetic resonance imaging (MRI) of the brain and orbits using fast spin-echo T1 and T2 sequences was performed to delineate the orbital mass better in relation to the globe as well as the intracranial cavity; it also showed a prominent enhancement in the extraconal space in the superior aspect of the right orbit, it was isointense with the extraocular muscles on the T1 images and hyper-intense on T2 imaging (due to increasing in water content of the buckle) with enlargement of the right superior ophthalmic vein. The thinning of the right orbital roof and the dura overlying the right orbit is slightly more prominent than the left, which was most likely reactive (Fig. 3). Given a history of hydrogel buckle surgery and the relationship of the mass to the globe, the mass was presumed to be a scleral hydrogel explant causing these clinical pictures of a space-occupying lesion in orbit. The patient was offered the option of surgical removal of the explant by a vitreoretinal surgeon. As this was his seeing eye and after discussion of the risks and benefits associated with surgical removal, the patient declined to go for a surgical intervention.
Fig. 1.
Right inferior displacement of right globe with fullness of superior sulcus with ptosis and restriction of eye movement.
Fig. 2.
CT scan showed a large cystic lesion in the superolateral quadrants of the orbit (A) superiorly associated with bone rarefaction and bone defect in the related part of orbital roof appearing to erode into the anterior cranial fossa (arrow A), (B) scleral buckle indenting and deforming the globe.
Fig. 3.
MRI of the brain and orbits fast spin-echo T1 and T2 sequences, prominent enhancement in the extraconal space in the superior aspect of the right orbit (A), hyper-intense on T2 imaging (becuase increased in water content of the buckle) (B).
3. Discussion
We believe this case to be the latest and the first report of a hydrogel (MIRAgel®) explant complications causing a bony defect of the orbital roof. It demonstrates the importance of a detailed ophthalmic history, particular past eye surgery history, and examination prior to an investigative workup of the patient, as well as good clinical notes documentation with a good filing system. In the case of hydrogel buckle, very long follow-up advice as complications can happen or get worse even after 30 years after this type of buckle material.
The differential diagnoses of this case include multiple cranial nerve palsies, thyroid eye disease, orbital cellulitis and inflammatory granuloma formation. The possibility of multiple cranial nerve palsies was ruled out because of no history of trauma or neurological symptoms, and no neoplastic lesions were found in brain and orbits. Orbital cellulitis was ruled out based on the clinical findings of no deterioration of vision and no afferent pupillary defects or significant tenderness. Thyroid eye disease was ruled out because there was no thickening of extraocular muscles on orbital imaging. The inflammatory granuloma does not appear cystic and is characterized by the low T2 signal.
Although the hydrogel scleral band is designed to expand in a controlled fashion, long-term complications, including swelling and overexpansion of explant, were reported; this can occur in both short-term and long-term complications [6]. Shields and her colleagues reported Expanding MIRAgel scleral buckle simulating an orbital tumor in four cases; the range was between 12 and 20 years after the primary buckle surgery [9]. However, no bone rarefaction or bone defect of the orbital wall was reported as in our case. Kearney et al. (2004), in a retrospective, a multicentre study, reported a series of 17 eyes of 15 patients with hydrogel buckle surgery between 1984 and 1992, the most common complication reported were pain or discomfort, and external eye inflammation in all patients, three patients in the group with external eye inflammation had poor lid–globe apposition with exposure keratopathy. Mass beneath the conjunctiva or eyelid was observed in 13 of 17 eyes. Diplopia and strabismus were reported in 10 of 17 eyes [7]. One study that compared the complications from different buckling elements found that MIRAgel was reported to present much later (mean, 92 months) compared to solid silicone (mean, 11 months) and silicone sponges (mean, 19 months). The gradual swelling of the MIRAgel led to the restriction of ocular motility and diplopia. Late swelling of MIRAgel buckling elements represents a common indication for buckle removal. However, the rate of buckle infection was much lower with MIRAgel than with other buckling materials [10]. It's also worth mentioning that scleral invasion, and intraocular penetration of MIRAgel may occur many years after placement [11]. Crama and his colleague highlight the difficulties of removing hydrogel buckles and possible complications. Of hydrogel explants removed, 11 % of cases develop intraoperative scleral perforation or retinal redetachment [12].
4. Conclusion
MIRAgel scleral buckle material can enlarge years after primary surgery; representing a diagnostic challenge for ophthalmologists who encounter such cases. Patients usually do not recall details of the retinal surgery. Therefore, meticulous clinical documentation with a good filing system is critical. The importance of recognizing this condition is through careful exclusion of serious orbital and neurological conditions. To our knowledge, this is the first reported case of hydrogel causing a bony defect of orbital wall.
Sources of funding
None.
Ethical approval
This study was exempted from ethical approval by the institutional review board (IRB) at the University of Tabuk.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Registration of research studies
Not applicable.
Ethical statement
The patient health information was HIPPA compliant and the study adhered to the tenets of the Declaration of Helsinki.
Guarantor
Hani AlBalawi, MD
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Hani ALBalawi and Ghada Alanazi = Study concept, Data collection. Naif Alali, Mustafa Magliyah, and Osama Alraddadi = Writing- original draft preparation. Khalid Alsharari = Editing and writing. All the authors read and approved the final manuscript.
Declaration of competing interest
The authors declares that there is no conflict of interest regarding the publication of this article.
Contributor Information
Hani Basher ALBalawi, Email: hb.albalawi@ut.edu.sa.
Naif Mamdouh Alali, Email: nmalali@ut.edu.sa.
References
- 1.Salicone Alberto, Smiddy William E., Venkatraman Anna, Feuer William. Management of retinal detachment when no break is found. Ophthalmology. 2006;113(3):398–403. doi: 10.1016/j.ophtha.2005.10.002. Epub 2006 Jan 10. [DOI] [PubMed] [Google Scholar]
- 2.Wilkinson C.P., Rice T.A. Michels Retinal Detachment. 2nd edn. Mosby; St Louis, MO: 1997. pp. 241–333. [Google Scholar]
- 3.Custodis E. Die behandlung der netzhautablosung durch umschriebene diathermie-koagulation udn einer mittels plombenaufnahung erzeugtren eindellung der sklera im bereich des risses. Klin Mbl Augenheilkd. 1956;129:476–495. [PubMed] [Google Scholar]
- 4.Rizzo S., Genovesi-Ebert F., Allegrini L. ESASO Course Series. 121–126. 2012. Scleral buckling materials. [DOI] [Google Scholar]
- 5.Crama N., Klevering B.J. The removal of hydrogel explants: an analysis of 467 consecutive cases. Ophthalmology. 2016;123(1):32–38. doi: 10.1016/j.ophtha.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 6.Marin J.F., Tolentino F.I., Refojo M.F., Schepens C.L. Long-term complications of the MAI hydrogel intrascleral buckling implant. Arch. Ophthalmol. 1992;110(1):86–88. doi: 10.1001/archopht.1992.01080130088031. [DOI] [PubMed] [Google Scholar]
- 7.Kearney J.J., Lahey J.M., Borirakchanyavat S., et al. Complications of hydrogel explants used in scleral buckling surgery. Am J. Ophthalmol. 2004;137:96–100. doi: 10.1016/s0002-9394(03)00873-0. [DOI] [PubMed] [Google Scholar]
- 8.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. International Journal of Surgery. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 9.Shields C.L., Demirci H., Marr B.P., et al. Expanding MIRAgel scleral buckle simulating an orbital tumor in four cases. Ophthalm Plast Reconstr Surg. 2005;20(1):32–38. doi: 10.1097/01.iop.0000148409.31127.f5. [DOI] [PubMed] [Google Scholar]
- 10.Le Rouic J.F., Bettembourg O., D’Hermies F., et al. Late swelling and removal of MIRAgel buckles: a comparison with silicone indentations. Retina. 2003;23:641–646. doi: 10.1097/00006982-200310000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Rubinstein T.J., Choudhary M.M., Modi Y.S., Ehlers J.P., Perry J.D. Globe loss from intraocular invasion of MIRAgel scleral buckle components. Ophthal. Plast. Reconstr. Surg. 2016;32(5):329–332. doi: 10.1097/iop.0000000000000527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crama N., Klevering B.J. He Removal of hydrogel explants: an analysis of 467 consecutive cases. Ophthalmology. 2016;123(1):32–38. doi: 10.1016/j.ophtha.2015.08.018. Epub 2015 Sep 18. [DOI] [PubMed] [Google Scholar]