Abstract
Objective
The modified Stoppa combined with iliac fossa approach has gained increasing popularity. Although early clinical outcomes have been satisfactory, extensive long‐term clinical outcomes are relatively scarce. The purpose of this study was to evaluate the medium‐ and long‐term outcomes of this approach for complex acetabular fractures.
Methods
This was a retrospective study involving 57 patients with complex acetabular fractures from January 2009 to January 2016. All fractures were treated with the modified Stoppa combined with iliac fossa approach. Follow‐up was at least 5 years. Primary outcome measures, including quality of reduction and clinical outcomes, were recorded by an independent observer. Secondary outcome measures included time to surgery, surgical time, intraoperative blood loss, and perioperative complications.
Results
Fifty‐seven patients (range, 18–80 years) included 46 males and 11 females. There were 32 cases on the left side and 25 cases on the right side. The most common associated injury was pulmonary contusion. According to the Judet–Letournel classification, there were 27 both‐column fractures, 16 anterior column with posterior hemitransverse fractures and 14 T‐type fractures. The average time from injury to surgery was 7.3 days. The average intraoperative blood loss and transfusion were 750.9 ml and 564.3 ml, respectively. All fractures healed within 6 months after surgery. The average follow‐up time was 7.7 years, and there was no loss of follow‐up. The quality of reduction was graded as anatomical in 23 cases (40.4%), imperfect in 22 cases (38.6%), and poor in 12 cases (21.0%). According to grading system of Merle d’ Aubigne and Postel, clinical outcomes at 1 year follow‐up were excellent in 17 cases (29.8%), good in 25 cases (43.9%), fair in four cases (7.0%), and poor in 11 cases (19.3%). The excellent and good rate was 73.7% and the difference was not statistically significant compared with the clinical outcomes at the last follow‐up. Intraoperative complications included four cases of obturator nerve injury and two cases of vascular injury. Postoperative complications included one case of wound delayed healing, two cases of deep vein thrombosis, two cases of avascular necrosis of femoral head, three cases of heterotopic ossification and five cases of post‐traumatic arthritis. Only one of these patients underwent reoperation for femoral head necrosis.
Conclusions
The modified Stoppa combined with iliac fossa approach can achieve satisfactory reduction quality and hip function. It might be a valuable alternative to the ilioinguinal approach for the surgical management of acetabular fractures.
Keywords: Complex acetabular fracture, Follow‐up, Iliac fossa approach, Modified Stoppa approach, Open reduction and internal fixation
The modified Stoppa combined with Iliac Fossa (mS + IF) approach alone for complex acetabular fractures can obtained satisfactory radiological and clinical outcomes. The mS + IF approach is a good choice of surgical approach for the treatment of complex acetabular fractures with anterior approach alone.
Introduction
Acetabular fracture is located at the apex of the pyramid of orthopedic trauma and its treatment has always been a challenge for orthopedic trauma surgeons. The learning curve is relatively steep due to its unique anatomical characteristics. Conservative treatment has a poor prognosis and surgical treatment has become the consensus to manage such injury. Early restoration of anatomic relationship of the hip and firm fixation may contribute to good results. 1 , 2 , 3
In the course of surgical treatment, the choice of surgical approach is the primary consideration. An appropriate surgical approach should allow for full exposure of the fracture site to facilitate fracture reduction while minimizing surgical injury. 4 The surgical approaches for acetabular fractures generally include the anterior approach, posterior approach and combined approach. As a classical anterior approach, the ilioinguinal (IL) approach has been widely used for pelvic ring and acetabular fractures. 5 , 6 Simple anterior acetabular fractures and some complex acetabular fractures with anterior column displacement may be treated with this approach. 7 , 8 Although it allows direct visualization of the anterior column to the symphysis pubis, it also has a “blind spot” in terms of exposure. For example, when the quadrilateral surface is exposed by the IL approach, it can only be done by palpation of the endopelvic finger. In addition, the incision of this approach is long and often requires three or four windows for exposure. Due to the complexity of local anatomy, nerves and blood vessels are easily damaged during surgery.
Since most acetabular fractures involve the quadrilateral surface, intraoperative exposure of the quadrilateral surface facilitates fracture reduction and fixation. Therefore, it is necessary to choose other surgical approaches to overcome the deficiency of IL in exposing the quadrilateral surface. The famous French hernia surgeon Stoppa invented a method of repairing inguinal hernia in 1969, which was also known as the Stoppa approach. Later, Hirvensalo et al. applied the Stoppa approach to the treatment of pelvic fracture for the first time. 9 The modified Stoppa (mS) approach as an intrapelvic approach has been increasingly favored by trauma orthopedic surgeons. 10 , 11 , 12 It has obvious advantages in exposing the quadrilateral surface. Some scholars even believe that acetabular fractures that can be solved by IL approach can also be treated by the mS approach. 13 , 14 Compared with the IL approach, the mS approach is easier to operate and has a relatively flat learning curve. Furthermore, this approach does not require exposure of the external iliac vascular bundle, iliopsoas muscle and femoral nerve. Of course, it does not solve all acetabular fractures and has limitations in terms of surgical exposure. For example, it cannot expose the iliac wing. For some complex acetabular fractures involving the iliac wing, the mS approach combined with the lateral window (the iliac fossa approach) of the IL approach is required to manage such fractures. 15 , 16
The iliac fossa (IF) approach is not simply an additional incision, it can be used as an auxiliary window for the mS approach. The addition of the IF approach not only facilitates intraoperative fracture reduction and fixation, but also expands the scope of application of the mS approach. For more than 10 years, our team has used the modified Stoppa combined with Iliac Fossa (mS + IF) approach to treat complex acetabular fractures. Therefore, the aims of this study were: (i) to investigate the medium‐ and long‐term efficacy of the mS + IF approach in the treatment of complex acetabular fractures; and (ii) to make a recommendation on choosing a single approach for complex acetabular fractures.
Materials and Methods
Subjects
From January 2009 to January 2016, we retrospectively studied 71 patients with complex acetabular fractures. The inclusion criteria included: (i) complex acetabular fracture according to Judet–Letournel classification; 17 (ii) time from injury to surgery ≤3 weeks; (iii) treated by the mS + IF approach; and (iv) age over 18 years. Exclusion criteria included: (i) severe osteoporosis, pathological fracture, or pre‐existing hip diseases; (ii) lost to follow‐up or follow‐up of less than 5 years; (iii) open fracture; (iv) conservative treatment; and (v) previous bladder, uterus or prostate surgery. A total of 57 patients were enrolled based on inclusion and exclusion criteria. The ethics committee of the hospital approved the study (HX‐IRB‐AF‐04‐V3.0). All patients signed the ethical informed consent after admission.
Preoperative Planning
Acetabular fracture was often associated with head, chest, or abdominal injuries, so a comprehensive physical examination was important to rule out life‐threatening injuries. In addition, it was also necessary to assess the peripelvic soft tissue. All patients underwent fracture examinations, including X‐ray, CT scans and 3D reconstruction on admission or when their condition permitted. In addition to fluid resuscitation, advanced analgesia and management of associated injuries, the treatment after admission also required temporary fixation of the fracture by traction of the affected limb. Emergency reduction of the hip was required when hip dislocation occurred. At the same time, we should also pay attention to the prevention and risk screening of lower limb thrombosis. If there were no obvious bleeding contraindications, anticoagulant therapy with low molecular weight heparin sodium was used, and was stopped 24 h before surgery. Patients were encouraged to do plantarflexion and dorsiflexion exercises of the ankle. Those patients bed‐ridden for more than 3 days were screened for deep vein thrombosis (DVT) every 3 days. Surgical fixation of the acetabular fracture was considered as soon as the patient was hemodynamically stable. Surgical indications included a fracture displaced by more than 2 mm, or hip instability and incongruence. 18
Surgical Technique
Position
All patients were administered antibiotics prophylactically with a second‐generation cephalosporin 30 min before skin incision. The patients were placed in the supine position and were administered general anesthesia.
Approach and Exposure
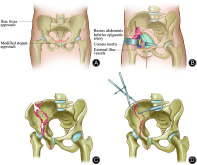
A transverse incision was made at the two transverse fingers above the pubic symphysis to expose the anterior sheath of the rectus abdominis (mS approach in Fig. 1A). The deep fascia layer in front of the muscle was bluntly separated, and the abdominal linea alba was found. The incision was longitudinally split into the pelvic cavity from the linea alba to protect the bladder. The pubic symphysis and the superior ramus of the pubis can be exposed by retracting the rectus abdominis. The rectus abdominis and neurovascular bundle were retracted laterally to protect them. If corona mortis was encountered, ligation was performed immediately (Fig. 1B). The iliopubic fascia and obturator fascia were incisively dissected to expose the true pelvic rim, the quadrilateral surface, and the posterior column of the acetabulum. This could be achieved by stripping the psoas muscle to better expose the ischial support band and the back of the pelvic rim.
Fig. 1.
Schematic diagram illustrating some key surgical steps and techniques. (A) The red line represented the incision of the mS + IF approach. (B) This diagram showed the anatomical location of the corona mortis. As soon as the corona mortis was encountered, it was ligated immediately. (C) The numbers 1, 2, and 3 represented the three main fragments, with 1 being the first to be reduced, followed by 2, and finally 3. (D) The manipulation of the critical fragments was accomplished by a number of reduction devices, such as a ball‐spiked pusher, acetabular reduction forceps
When certain fractures involved the iliac wing or the fracture line crossed the iliopectineal line, the mS approach alone could not fully expose and reduce the fractures. In this case, the IF approach as an additional incision could be adopted to solve the problem. It began at the middle of the iliac crest to the anterior superior iliac spine (IF approach in the Fig. 1A). The iliac wing could be exposed by retracting the iliac muscle and iliac vessels. And surgical exposure could be ameliorated by intraoperative movement of the affected hip, such as flexion, rotation, adduction, and abduction.
Fracture Reduction and Fixation
For critical free fragments involving or around the articular surface, screw fixation of these main fragments facilitated the restoration of anatomic markers. (i) Reduction was usually ordered from the periphery toward the center of the acetabulum, especially in the cases with iliac crest or anterior pelvic ring fractures (Fig. 1C); (ii) Reduction was carried out by means of a ball‐spiked pusher pushing, acetabular reduction forceps compressing and temporarily fixing, Kirschner wires prying, femoral traction, or the use of traction bed for longitudinal traction, etc. (Fig. 1D); (iii) The combination of the two approaches was beneficial for accurate reduction of acetabular fracture. After careful reduction with emphasis on correcting the rotational displacement of the fracture fragments, satisfactory reduction of the posterior column could be achieved; (iv) When fracture reduction was satisfactory, the main fragments were temporarily fixed with Kirschner wires, followed by intraoperative fluoroscopy to determine fracture reduction. Lastly, the pelvic reconstruction plates and cortical bone screws were used to fix the fracture.
Postoperative Management
A drainage tube was placed in the local cavity before the incision was closed. Low molecular weight heparin sodium was restarted 6 h after surgery. If there was no evidence of local or systemic infection, antibiotic use should be discontinued 48 h after surgery. If the daily drainage was less than 50 ml, the drainage tube was removed. On the first postoperative day, the patients began physical therapy with isometric quadriceps and abductor strengthening exercises. Passive mobilization of the hip began at 2 days postoperatively. A limitation in weight bearing was maintained for the first 8 weeks postoperatively, after which progressive weight bearing as tolerated was encouraged. Regular follow‐up was performed at 1, 2, 3, 6 and 12 months postoperatively. Thereafter, patients were examined at 1‐year intervals.
Outcome Measures
Primary outcome measures included quality of reduction and clinical outcomes. Secondary outcome measures, including time from injury to surgery, surgical time, intraoperative blood loss, blood transfusion and complications, were also recorded.
Quality of Reduction
Anteroposterior pelvic radiographs, Judet radiographs, and pelvic CT scans were obtained routinely. According to the scoring system published by Matta, 19 a displacement of greater than 3 mm on any plain radiographic view indicated a poor reduction. A displacement of 3 mm or less was defined as an imperfect reduction, with an anatomic reduction of less than 1 mm.
Clinical Outcomes
Clinical outcomes at 1 year postoperatively and the last follow‐up were scored according to the system published by Merle D'Aubigne and Postel, 20 with four grades possible: excellent (18 points), good (15–17 points), fair (12–14 points), and poor (3–11 points). At each visit, hip motion and neurovascular status were examined.
Statistical Analysis
SPSS version 25.0 statistical software (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Student's t test was used for quantitative variables. Categorical variables were analyzed by Pearson's chi‐square test or Fisher's exact test where appropriate. A value less than 0.05 was considered statistically significant.
Results
Follow‐up Data
Follow‐up was performed at 1, 2, 3, and 6 months and 1 year after surgery and yearly thereafter. The average follow up was 7.7 years (range, 5–12 years). The follow‐up period was still ongoing (Figs 2 and 3).
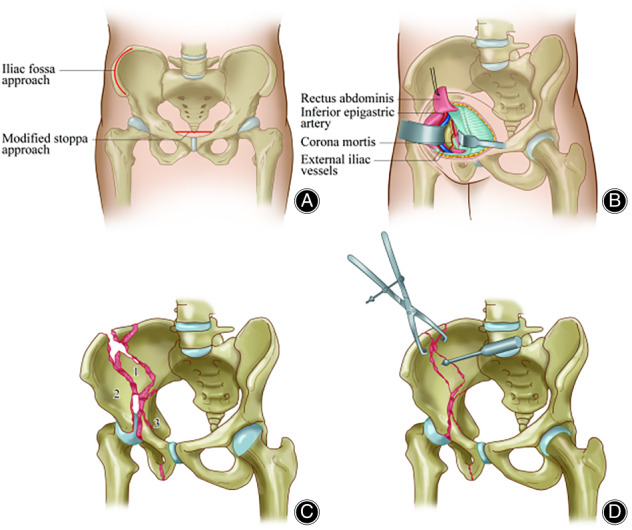
Fig. 2.
(A–E) A 44‐year‐old male patient sustained a road‐traffic accident. Preoperative radiographs and three‐dimensional reconstructions showed a both‐column fracture. (F–H) Immediate postoperative radiographs showed satisfactory reduction was obtained by the mS + IF approach. (I–L) Gross appearance and postoperative radiographs at 8 years of follow‐up showed the patient had a good functional hip outcome
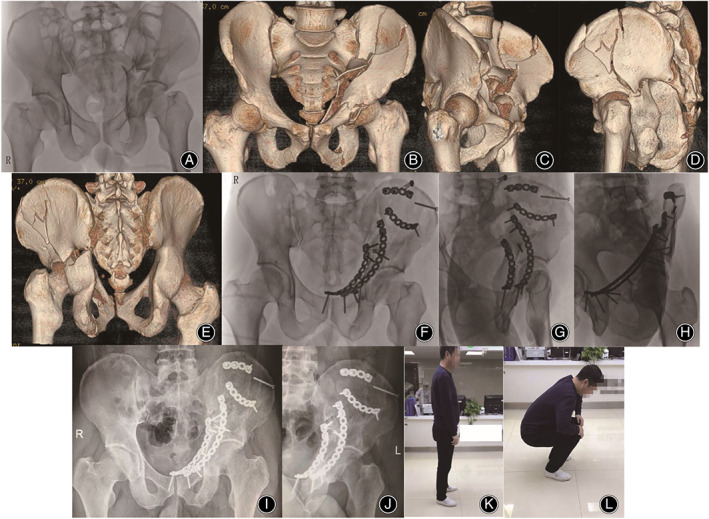
Fig. 3.

(A–E) A 41‐year‐old female patient sustained a road‐traffic accident. Preoperative images suggested a both‐column fracture. (F–H) Immediate postoperative radiographs showed satisfactory reduction by the mS + IF approach. (I‐K) No complications such as traumatic osteoarthritis and necrosis of femoral head were found in 5 years follow‐up
General Results
The study included a total of 57 patients with an average age of 43.3 years. There were 46 males and 11 females. There were 32 cases on left side and 25 cases on right side. The mechanism of injury was a high‐energy violence in all cases. Pulmonary contusion occurred in more than one in six patients. Both‐column fractures accounted for nearly half of all included acetabular fractures (Table 1). These patients were treated with open reduction and internal fixation via the mS + IF approach. The average time from injury to surgery was 7.3 days. The average surgical time was 156.8 min (range, 90–240 min). The average intraoperative blood loss was 750.9 ml (range, 300–1600 ml). The average blood transfusion was 564.3 ml (range, 200–1000 ml) (Table 2). All fractures healed within 6 months after surgery.
TABLE 1.
The demographics of subjects
| Variable | Value | Percent |
|---|---|---|
| Mean age, years (range) | 43.3 (18–80) | ‐ |
| Gender | ||
| Male | 46 | 80.7 |
| Female | 11 | 19.3 |
| Side of injury | ||
| Right | 25 | 43.9 |
| Left | 32 | 56.1 |
| Bilateral | 0 | 0 |
| Mechanism of injury | ||
| Road traffic accident | 31 | 54.4 |
| Fall from height | 20 | 35.1 |
| Others | 6 | 10.5 |
| Associated injuries | ||
| Limb fracture | 6 | 10.5 |
| Hip dislocation | 4 | 7.0 |
| Sciatic nerve injury | 3 | 5.3 |
| Pulmonary contusion | 10 | 17.5 |
| Traumatic brain injury | 3 | 5.3 |
| Fracture pattern | ||
| Both‐column | 27 | 47.4 |
| Anterior column with posterior hemitransverse | 16 | 28.1 |
| T‐type | 14 | 24.5 |
TABLE 2.
Surgery‐related variables
| Variable | Value | Percent |
|---|---|---|
| Mean time to surgery, days | 7.3 (3–16) | ‐ |
| Surgical time, min | 156.8 (90–240) | ‐ |
| Blood loss, mL | 750.9 (300–1600) | ‐ |
| Blood transfusion, mL | 564.3 (200–1000) | ‐ |
| Quality of reduction | ||
| Anatomic | 23 | 40.3 |
| Imperfect | 22 | 38.6 |
| Poor | 12 | 21.1 |
Radiographic Evaluation
Quality of reduction was graded as anatomic in 23 patients, imperfect in 22 patients, and poor in 12 patients (Table 2).
Merle d’ Aubigne and Postel Score System for Functional Evaluation
Excellent and good outcomes were mostly found in anatomic reduction of fractures. The relationship between quality of reduction and clinical outcomes was statistically significant (P < 0.05). Clinical outcomes at 1 year follow‐up were excellent in 17 patients, good in 25 patients, fair in four patients, and poor in 11 patients. The overall excellent and good rate was 73.7%, which was higher than that of the last follow‐up (χ2 = 1.076, P = 0.783) (Table 3).
TABLE 3.
Clinical outcomes
| Time | Clinical grading system according to Merle d’ Aubigne and Postel | |||
|---|---|---|---|---|
| Excellent | Good | Fair | Poor | |
| One‐year follow‐up | 17 | 25 | 4 | 11 |
| The last follow‐up | 15 | 22 | 6 | 14 |
Complications
Intraoperative complications included one case with obturator artery injury and one case with the corona mortis injury, both of which were caused by careless dissection. No major intraoperative blood loss occurred by packing and ligating. Four patients had the obturator nerve injury due to possible excessive traction or careless dissection. At the last follow‐up, three patients recovered remarkably, whereas the remaining one patient only recovered slightly, with partial loss of hip adductor strength. One patient had delayed healing of the incision caused by infection, but he recovered within 3 weeks by prolonged antibiotic administration. Two patients developed DVT in the lower limbs, but they were dissolved after aggressive antithrombotic treatment, and no cases of pulmonary embolism occurred during the entire follow‐up. Three patients presented with asymptomatic heterotopic ossification. There were five cases of hip osteoarthritis, including three mild cases and two moderate cases. After the corresponding symptomatic treatment, the symptoms of arthritis were relieved in different degrees. Two patients had avascular necrosis of the femoral head, one underwent hip replacement and the other refused further surgical treatment (Table 4).
TABLE 4.
Complications
| Complications | Value | Percent |
|---|---|---|
| Intraoperative | ||
| Vascular injury | 2 | 3.5 |
| Nerve injury | 4 | 7.0 |
| Early | ||
| Delayed healing | 1 | 1.8 |
| DVT | 2 | 3.5 |
| Late | ||
| Heterotopic ossification | 3 | 5.3 |
| Post‐traumatic arthritis | 5 | 8.8 |
| Avascular necrosis | 2 | 3.5 |
Discussion
Surgical Approach
In the treatment of acetabular fractures, surgical approach is a key factor. 21 In the study, we chose the mS + IF approach for the treatment of complex acetabular fractures based on the following points: (i) compared with the classical IL approach, this approach has obvious advantages in the exposure of the quadrilateral surface and has a relatively flat learning curve; (ii) compared with the combined approach, this approach, as a simple anterior approach, has less surgical trauma, shorter operative time, and less risk of vascular and nerve injury and infection; and (iii) in more than 10 years of clinical practice, we have accumulated some experience in the application of this approach. The results of this study showed that this approach achieved satisfactory reduction quality and no serious bleeding or embolic disease occurred during the perioperative period. In addition, most patients achieved satisfactory hip function during the follow‐up period.
It should be noted that the selection of the surgical approach requires consideration of various factors, such as fracture characteristics, soft tissue condition, timing of surgery and the preference of the surgeon. Preoperatively, we fully evaluated these factors and tried to manage complex acetabular fractures through a single surgical approach without compromising the reduction quality. In fact, in some cases of acetabular fractures involving both columns, satisfactory reduction of the posterior column fracture can be achieved indirectly after reduction and fixation of the anterior column. Of course, we were not overly pursuing in a single surgical approach. If satisfactory reduction of the posterior column fracture cannot be achieved, anterograde lag screws or an additional posterior approach may be considered.
Comparison of the Other Approaches and mS + IF Approach
A prospective comparative study showed no significant differences in the reduction quality, clinical outcomes, and complications between the mS approach and the IL approach for the treatment of acetabular fractures. However, compared with the IL approach, the mS approach had obvious advantages in some aspects, such as less operative time, blood loss and blood transfusion. 22 In a retrospective study, 88% of patients treated with the mS approach achieved satisfactory hip function over a 10‐year period. 12 The results of another 10‐year retrospective study showed that only the mS approach or in combination with iliac wing approach resulted in better hip function than the IL approach. 23 Zou et al. compared the efficacy of the IL approach and the pararectus approach in the treatment of acetabular fractures. 24 Satisfactory hip function was achieved in 83% of patients treated by the pararectus approach, which was similar to that (77%) of patients treated by the IL approach.
In these studies, satisfactory hip function was achieved with both MS and IL approaches. In our study, the excellent and good clinical outcomes at 1 year follow‐up were rated at 73.7%. Although the rate of satisfactory outcomes decreased at the last follow‐up, there was no statistically significant difference. Moreover, the satisfactory outcomes reported in our study were slightly lower than those presented in the aforementioned literature. This may be related to the following factors: first, the cases included in our study were complex acetabular fractures, and nearly half of them were both‐column fractures, which were difficult to treat. Second, it may be related to factors such as the technique of the surgeon and the heterogeneity of the cases. Future studies will focus on the efficacy of this approach compared with other approaches in the treatment of complex acetabular fractures.
Complications
Complications of acetabular fractures can be caused by a variety of factors, including infection, vascular nerve injury, heterotopic ossification, traumatic osteoarthritis, abdominal hernia, and so on. The occurrence of these complications is related to the anatomical characteristics of acetabular fractures on the one hand and the choice of surgical approach on the other hand. Liu et al. 25 believed that the incidence of postoperative complications of the mS approach was significantly lower than that of the IL approach, especially for the complications in the inguinal region.
In our study, four cases of obturator nerve injury were observed. Through postoperative analysis, they may be caused by excessive intraoperative traction. Therefore, intraoperative attention should be paid to the tension of blood vessels and nerve tracts between the two incisions to avoid excessive traction. One patient had the incision infection. But it is not clear whether there is a direct link between incision infection and surgical approach. One of the two patients with vascular injury had corona mortis injury. For the management of such cases, our recommendation is to ligate immediately once the corona mortis is encountered. The mS approach can directly view and treat the important structure of the corona mortis, greatly reducing intraoperative bleeding. In addition, two patients developed avascular necrosis of femoral head, which was associated with preoperative dislocation of the hip. One patient had to undergo reoperation. Therefore, in the event of acetabular fractures with hip dislocation, it is best to treat such injuries within 6 h. 26
Limitations
This study was subject to several limitations. First, this study was a single‐center study with a small sample size. Second, this study was a retrospective analysis without a randomized controlled study. Finally, the lack of a control group was a major weakness of the study, which might weaken the strength of the study to draw the conclusion. In the future, prospective, randomized, controlled studies are warranted to verify the validity and reliability of the mS + IF approach for complex acetabular fractures.
Conclusions
Our experience shows that the mS + IF approach can obtain satisfactory radiological and clinical outcomes in complex acetabular fractures. This approach can effectively manage complex acetabular fractures and might be a valuable alternative to the ilioinguinal approach for the surgical treatment of such injuries.
Author Contributions
Yun Yang and Ting‐ting Tang wrote the draft of the manuscript and were major contributors to study design and revision. Chang Zou was involved in data collection. Yue Fang critically reviewed and revised the manuscript for important intellectual content. All authors approved the final manuscript and agreed to be accountable for all aspects of the work.
Acknowledgments
We sincerely thank all the patients and medical stuff who participated in this study.
References
- 1. Kelly J, Ladurner A, Rickman M. Surgical management of acetabular fractures—a contemporary literature review. Injury. 2020;51(10):2267–77. [DOI] [PubMed] [Google Scholar]
- 2. Cimerman M, Kristan A, Jug M, Tomaževič M. Fractures of the acetabulum: from yesterday to tomorrow. Int Orthop. 2021;45(4):1057–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta‐analysis. J Bone Jt Surg, Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 4. Kacra BK, Arazi M, Cicekcibasi AE, Büyükmumcu M, Demirci S. Modified medial Stoppa approach for acetabular fractures: an anatomic study. J Trauma. 2011;71:1340–4. [DOI] [PubMed] [Google Scholar]
- 5. Wu H, Shang R, Cai X, Liu X, Song C, Chen Y. Single ilioinguinal approach to treat complex acetabular fractures with quadrilateral plate involvement: outcomes using a novel dynamic anterior plate‐screw system. Orthop Surg. 2020;12(2):488–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shi X, Li X, Wang A. Comparative efficacy and safety of the minimally invasive ilioinguinal approach for anterior pelvic ring fracture: a protocol for systematic review and network meta‐analysis. Medicine. 2021;100(52):e28377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tosounidis TH, Giannoudis VP, Kanakaris NK, Giannoudis PV. The Ilioinguinal approach: state of the art. JBJS Essent Surg Tech. 2018;8(2):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fensky F, Lehmann W, Ruecker A, Rueger JM. Ilioinguinal approach: indication and technique. J Orthop Trauma. 2018;32(Suppl 1):S12–3. [DOI] [PubMed] [Google Scholar]
- 9. Hirvensalo E, Lindahl J, Böstman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993;297:28–32. [PubMed] [Google Scholar]
- 10. Salama W, Hosny H, Mohamed MA, Noaman HH, Mousa S. Modified stoppa approach for the treatment of complex acetabular fractures. Orthopedics. 2021;44(3):e353–8. [DOI] [PubMed] [Google Scholar]
- 11. Al Adawy AS, Aziz AHA, El Sherief FA, Mahmoud WS, Mabrook M, Hassan YE. Modified Stoppa as an alternative surgical approach for fixation of anterior fracture acetabulum: a randomized control clinical trial. J Orthop Surg Res. 2020;15(1):154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Verbeek DO, Ponsen KJ, van Heijl M, Goslings JC. Modified Stoppa approach for operative treatment of acetabular fractures: 10‐year experience and mid‐term follow‐up. Injury. 2018;49(6):1137–40. [DOI] [PubMed] [Google Scholar]
- 13. Andersen RC, O'Toole RV, Nascone JW, Sciadini MF, Frisch HM, Turen CW. Modified Stoppa approach for acetabular fractures with anterior and posterior column displacement: quantification of radiographic reduction and analysis of interobserver variability. J Orthop Trauma. 2010;24:271–8. [DOI] [PubMed] [Google Scholar]
- 14. Sagi HC, Afsari A, Dziadosz D. The anterior intra‐pelvic (modified Rives‐Stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24:263–70. [DOI] [PubMed] [Google Scholar]
- 15. Jakob M, Droeser R, Zobrist R, Messmer P, Regazzoni P. A less invasive anterior intrapelvic approach for the treatment of acetabular fractures and pelvic ring injuries. J Trauma. 2006;60:1364–70. [DOI] [PubMed] [Google Scholar]
- 16. Wolf H, Wieland T, Pajenda G, Vecsei V, Mousavi M. Minimally invasive ilioinguinal approach to the acetabulum. Injury. 2007;38:1170–6. [DOI] [PubMed] [Google Scholar]
- 17. Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Jt Surg, Am. 1964;46:1615–46. [PubMed] [Google Scholar]
- 18. Guyton JL, Perez EA. Fractures of the acetabulum and pelvis. In: Canale ST, Beaty JH e, editors. Campbell's operative orthopaedics. 11th ed. Philadelphia. PA: Mosby; 2007. p. 3322–3. [Google Scholar]
- 19. Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Jt Surg, Am. 1996;78:1632–45. [PubMed] [Google Scholar]
- 20. Merle D'Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Jt Surg, Am. 1954;36:451–75. [PubMed] [Google Scholar]
- 21. Zha GC, Sun JY, Dong SJ. Predictors of clinical outcomes after surgical treatment of displaced acetabular fractures in the elderly. J Orthop Res. 2013;31:588–95. [DOI] [PubMed] [Google Scholar]
- 22. Ma K, Luan F, Wang X, Ao Y, Liang Y, Fang Y, et al. Randomized, controlled trial of the modified Stoppa versus the ilioinguinal approach for acetabular fractures. Orthopedics. 2013;36:e1307–15. [DOI] [PubMed] [Google Scholar]
- 23. Vikmanis A, Jakusonoka R, Jumtins A, Pavare Z. Outcome for patients with acetabular fractures treated using only modified Stoppa approach or in combination with iliac wing approach: 10‐year experience. Acta Chir Orthop Traumatol Cech. 2021;88(3):191–5. [PubMed] [Google Scholar]
- 24. Zou R, Wu M, Guan J, Xiao Y, Chen X. Clinical results of acetabular fracture via the pararectus versus ilioinguinal approach. Orthop Surg. 2021;13(4):1191–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Liu Y, Yang H, Li X, Yang SH, Lin JH. Newly modified Stoppa approach for acetabular fractures. Int Orthop. 2013;37:1347–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Phillips AM, Konchwalla A. The pathologic features and mechanism of traumatic dislocation of the hip. Clin Orthop Relat Res. 2000;377:7–10. [DOI] [PubMed] [Google Scholar]


