Abstract
Objective
The purpose of this study was to evaluate the best placement of calcar screws in proximal humerus fracture surgeries.
Methods
This retrospective cohort study included clinical and radiographic outcomes of 98 patients treated with proximal humerus fracture surgeries between January 2017 and June 2020. Demographic data of patients were obtained from medical records. The surgical and radiographic results were also collected: operation time, blood loss, time to surgery, fibular allograft, disruption of medial region hinge, Neer classification, and recovery of medial support. Patients were allocated into two groups: the locking plate group (n = 65) and the intramedullary nail group (n = 33). In this study, we proposed new predictive indicators, named horizontal ratio (HR) and vertical ratio (VR), to quantify the placement of calcar screws in these two groups. A receiver operating characteristic (ROC) analysis was conducted to display the accuracy of these indicators. Shoulder activity, visual scale analog (VAS) score, and Constant score were performed to evaluate postoperative clinical outcomes at 1 year follow‐up.
Results
In the multivariate logistic regression analysis, only time to surgery and effective medial support were considered statistically significant factors of postoperative complications (p < 0.05). Significant differences were observed between medial support and postoperative complications both in the locking plate group and the intramedullary nail group (p < 0.05). Only the vertical ratio of locking plate (VRLP) was a statistically significant predictor of postoperative complications (p < 0.05). The area under curve was calculated to assess the predictive value of VRLP, which came to 0.84. In addition, a ROC analysis found quantifiable thresholds of the VR was 0.1713 as measures to avoid postoperative complications in the locking plate fixation.
Conclusion
In locking plate fixation, the incidence of postoperative complications increased significantly when the VR of calcar screws greater than 0.1713, which was beneficial to surgeons to place calcar screws.
Keywords: Calcar screw, Medial support, Postoperative complication, Predictive indicator, Proximal humerus fracture
In this study, time to surgery and medial support were significantly correlated with postoperative complications in proximal humerus fracture. New indicators of calcar screws were proposed to explore best placement to avoid complications after surgery.

Introduction
Proximal humerus fractures account for 4%–10% of all adult fractures, which often happened to elderly patients after a low energy fall. 1 In spite of the fact that acceptable results can be achieved with non‐operative treatment in 80% of proximal humerus fractures, surgical treatment is generally performed in unstable fractures, especially in displaced and osteoporotic cases. On the other hand, conservative treatment for proximal humerus fractures often results in shoulder disability, which owes to subacromial impingement and limitations of abduction and external rotation. Benefited from significant improvements in surgical instruments and techniques, a broader indication for surgical treatment is considered an option for surgeons. The purpose of surgical treatment is to achieve stable fixation which provides early rehabilitation training and obtains the recovery of joint function. Therefore, surgical treatments nowadays are increasingly considered as the most common option. 2
A recent study showed that complications in proximal humerus fractures after internal fixation remain high. 3 Avascular necrosis (AVN) of humerus head brings out a delayed pain and deficiency in range of motion. Non‐union often acquires a revision surgery. 4 , 5 Other complications, such as screw loosing and plating breakage, also cause trouble for both surgeons and patients.
It is known that anatomic reduction is associated with great clinical outcomes in proximal humerus fractures. Gardener firstly stressed the importance of medial support in avoiding reduction loss. In addition, he proposed the concept of the calcar screw: an inclined locking screw pointing upwards, precisely placed in the inferior medial region of humerus head, aiming to achieve stable medial support and reliable maintenance of reduction. 6 However, a quantifiable distance from the calcar screws of internal fixations to the medial region has not been clearly defined. In addition, he found that an additional allograft fibula could provide a better support in the medial region. 7 Nevertheless, Hinds et al. believed that allograft fibula did not significantly improve clinical outcomes in osteoporosis cases and increased the cost of surgery. 8 Then, calcar screws were applied to intramedullary nail technology, which showed great prospects in surgical neck fracture with medial region destruction. In subsequent clinical studies, Zhang et al. and Jung et al. proved that medial support could decrease the postoperative complication rate impressively. 9 , 10
A clinical report shows additional calcar screws are associated with many postoperative complications, such as AVN, non‐union, screw penetration, screw loosening, and varus deformity. 11 As far as we know, many studies emphasized the importance of calcar screws in maintaining reduction, but the exact location of calcar screw remained controversial either in plate or intramedullary nail fixation. In this study, we came up with some indicators to quantify the placement of calcar screws in locking plate and intramedullary nail fixation. Therefore, we did a retrospective study of two cohorts of patients treated with either intramedullary nail and locking plates for proximal humerus fracture from January 2017 to June 2020. We hope to achieve the following: (i) to explore significant factors associated with postoperative complications in proximal humerus fracture; (ii) to evaluate the position of calcar screws quantitatively; (iii) to provide an ideal clinical option of calcar screw placement to prevent postoperative complications.
Methods
Study Design
A retrospective cohort study was approved by the Ethics Committee of Beijing Chaoyang Hospital to analyze the clinical and radiographic outcomes of patients receiving surgical treatments for proximal humerus fractures between January 2017 and June 2020 (approval no. 2021‐ke‐441). The Committee waived the requirement for written informed consent because the study was retrospective, it did not have any adverse effect on patients' health, and it reported anonymized patient data.
To explore the risk factors associated with complications, clinical and radiographic data were analyzed in our research. Therefore, cases were grouped according to the presence or absence of postoperative complications.
Following results included predictive indicators and postoperative functional scores. To evaluate the clinical effect of the new predictive indicators in different surgical methods, we additionally divided the cases into two groups: the locking plate group and the intramedullary nail group. Finally, this study also concentrated on postoperative functional evaluation, which included a clinical comparison of with and without effective medial support.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (i) 16 years old or older; (ii) a proximal humerus fracture with clinical and radiography evidence; (iii) receiving locking plates (PHILOS, Synthes, Paoli, PA, USA) or intramedullary nails (The MultiLoc Nails, DePuy Synthes, Raynham, MA, USA) internal fixation; (iv) followed up for at least 12‐month postoperatively. Exclusion criteria were previous tumor history of injured limb, nerves injury, open fractures, rotator cuff injury, shoulder arthroplasty, or non‐surgical treatment. Patients with inadequate preoperative or postoperative radiograph and incomplete clinical variables were also excluded.
Clinical and Radiographic Data
Clinical and radiographic data were collected including gender, age, history of alcohol and tobacco use, injury type (high‐energy and low‐energy), comorbidities (hypertension, hyperlipidemia, and diabetes mellitus), shoulder joint activity (preoperative), operation time, blood loss, time to surgery, fibular allograft, disruption of medial region hinge, the condition of postoperative medial support, postoperative complications, and the Neer classification. 12
The primary outcomes included failure of internal fixation (screw loosening and plate breakage) and varus deformity. The secondary outcomes were non‐union and AVN of humerus head.
The classification of proximal humerus fractures and the condition of medial support were determined by preoperative X‐ray and three‐dimensional computed tomography. All fractures were classified by the Neer classification. Clinical findings and radiographs including anteroposterior and axillary views were jointly reviewed by the primary and senior surgeons after 1, 6, and 12 months postoperatively.
At the last follow‐up, patients received a detailed shoulder motion examination and an assessment of shoulder function score assessment. In order to achieve a comprehensive comparison, both healthy contralateral and injured limbs were included.
Surgical Process
Anesthesia and Position
Both locking plate and intramedullary nail groups were performed under general anesthesia, in a “beach chair” position.
Locking Plate Group
The injured upper limb of patient was routinely disinfected and covered. The surgery used a deltopectoral approach to enter between the deltoid and ectopectoralis to expose the fracture line. The greater and smaller tuberosity of humerus were prepositioned with sutures. The fracture segment was reduced by using Kirschner wire as a temporary measure. A locking plate and several screws were fixed. A calcar screw providing stability for medial region of proximal humerus was applied while visible presence of medial region defect existed. Then greater and smaller tuberosity of humerus were sutured and knotted with preset sutures. The entire wound was sutured and a drainage tube was placed after satisfied passive shoulder joint motion and immediate postoperatively radiographies obtained.
Intramedullary Nail Group
With the assistance of C‐arm radiography, the proximal humerus fracture was reduced by traction and a routine disinfection was performed subsequently. Anterolateral acromion incision was performed to split deltoid. After dissecting rotator cuff and the joint capsule, a round needle entered into the interior joint surface and an optional guide pin was placed to insert the distal medullary cavity. The intramedullary nail was inserted to stabilize the fracture segment with the appropriate position of proximal and distal screws. Depending on medial region condition, the screw was placed into the inferomedial quadrant of the proximal humeral head. After obtaining immediate postoperatively radiographs including fracture reduction and placement of internal fixation, the rotator cuff and deltoid muscle was repaired and the entire wound was sutured.
Definition of Observation Indicators
Non‐union and AVN
Non‐union was defined as a fracture without radiographic signs of complete healing 9 months after humeral head fracture or progressing union for more than 3 months on postoperative X‐rays. AVN of the humerus head conformed to the identification criteria of AVN. 13
Varus Collapse
Varus collapse was measured as the change of neck‐shaft angle more than 20° on the anteroposterior view of postoperative radiograph, using the healthy limb as a reference. 14
Internal Fixation Failure
The internal fixation failure was observed as plate breakage or dislocation of screws for at least 5 mm on the postoperative X‐rays. 15
Condition of Medial Region Supports
According to the theory of Hertel, the medial region hinge of proximal humerus was considered disrupted if there was a displacement of the shaft in any direction greater than 2 mm. 16
The presence of medial support was defined if (i) the medial pillar of the proximal humerus was not comminuted and anatomically reduced successfully; (ii) the shaft was medialized and impacted into the head fragment; or (iii) an oblique locking screw was placed directly into the inferomedial quadrant of the proximal humeral head fragment. 6
Predictive Indicators for Calcar Screws
In order to describe the placement of calcar screws in locking plates or intramedullary nails fixation, new predictive indicators were proposed: horizontal ratio (HR) and vertical ratio (VR). The distance from the tip of calcar screws to the medial hinge was recorded as a1 or a3 (along the direction in which the screw was inserted). The total length of the humerus head along the same direction was recorded as b1 or b3. HR of the locking plate (HRLP) or intramedullary nail (HRIN) was defined as a1/b1 or a3/b3.
Similarly, the distance from inferior of calcar screws to junction of humerus head and stem were recorded as a2 or a4. The distance from junction of humerus head and stem to the other side of the humeral head were recorded as b2 or b4 (along the same direction of a2 or a4). VR of locking plate (VRLP) or intramedullary nail (VRIN) was defined as a2/b2 or a4/b4. (Figure 1).
Fig. 1.
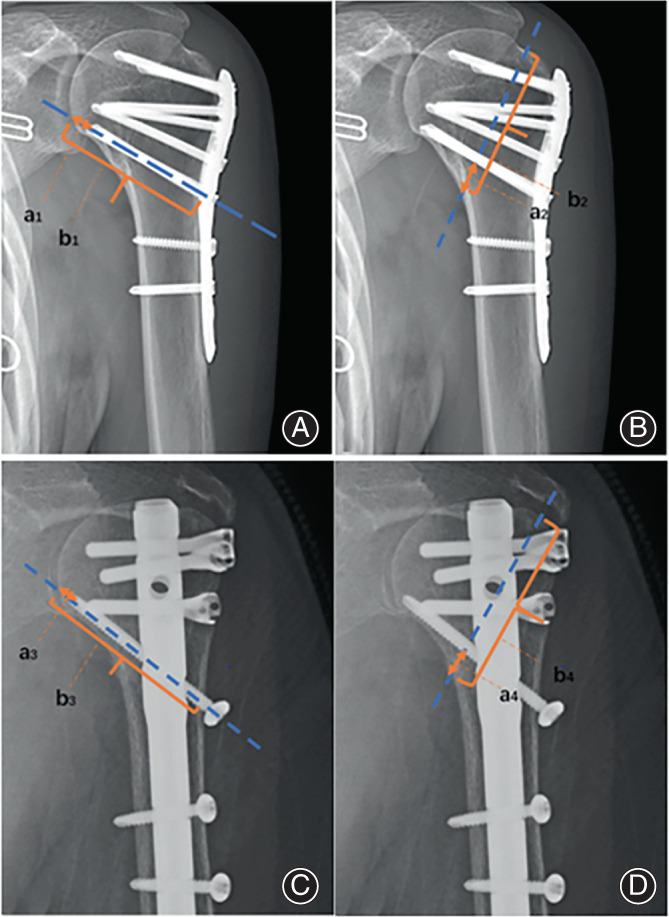
(A, B) The horizontal and vertical ratio of locking plate are equal to the ratio of a1 to b1 and a2 to b2; (C, D) The horizontal and vertical ratio of intramedullary nail are equal to the ratio of a3 to b3 and a4 to b4
Two independent and blinded orthopaedic surgeons assessed pre‐ and postoperative radiographs and their measurements were averaged.
Shoulder Activity and Function Scores Assessment
Shoulder Motion Examination
The shoulder motion examination included flexion, abduction, external rotation, and internal rotation while patients stood and breathed peacefully without any assistant.
Constant Score
The Constant score was used to evaluate shoulder function, consisting of four categories, including pain (15 points), activity level (20 points), total range of motion (40 points), and muscle strength grade (25 points). The total score is the sum of these four items, and the higher scores indicate greater function. A score of 100 points is defined as normal, 90–100 as excellent, 80–89 as good, 70–79 as fair, and 0–69 as poor.
Visual Analog Scale (VAS) Score
The VAS score was performed to assess patient pain level, ranging from no pain to worst pain possible. 17 The total score is from 0 to 10, and the higher scores indicate worse pain. A score of 0 points is defined as normal, 1–3 as mild pain, 4–6 as moderate pain, 7–9 as severe pain, and 10 as worst pain possible.
Statistical Analysis
Statistical analyses were performed using the SPSS version 21.0 (IBM, Armonk, New York, USA). All continuous variables were expressed as the mean ± standard deviation. All counting data were expressed in frequency and percentage. Data were analyzed using independent two‐sample t‐test and chi‐square test for continuous and counting variables, respectively. To identify the statistically significant clinical factors responsible for postoperative complications, multivariate logistic regression analysis with combinations of two independent variables (the presence of medial support and time to surgery) was performed. p values <0.05 were considered statistically significant. A ROC curve was generated to identify a threshold predictive. The area under the curve was calculated to assess the predictive value of these variables. The Youden index was calculated and reported as a reference of the threshold optimizing accuracy.
Results
Clinical and Radiographic Results
Presented in Table 1, there was no significant difference between with and without complication groups in gender ratio (four men to 10 women vs 20 men to 64 women, p = 0.70) and mean age (59.9 years vs 63.0 years, p = 0.58). The clinical data also showed no statically significant difference in history of alcohol and tobacco use, injury type, comorbidities (including hypertension, diabetes, and hyperlipidemia), shoulder mobility, operation time, and blood loss in these two groups (p > 0.05). The average time of surgery to the complication group was significantly longer than the group without complication (8.4 days vs 5.3 days, OR = 1.28, p = 0.004).
TABLE 1.
Demographic statistics according to the presence of postoperative complication
| Overall | With complication | Without complication | p value | ||
|---|---|---|---|---|---|
| Gender | Male | 24 | 4 | 20 | 0.7 |
| Female | 74 | 10 | 64 | ||
| Age (years) | 62.5 ± 17.0 | 59.9 ± 14.9 | 63.0 ± 16.8 | 0.58 | |
| History of tobacco and alcohol use | Yes | 9 | 1 | 8 | 0.78 |
| No | 89 | 13 | 76 | ||
| Injury type | High‐energy violence | 13 | 2 | 11 | 0.9 |
| Low‐energy violence | 85 | 12 | 73 | ||
| Comorbidities | Yes | 55 | 7 | 48 | 0.62 |
| No | 43 | 7 | 36 | ||
| Shoulder mobility | Bad | 1 | 1 | 0 | 1 |
| Good | 97 | 13 | 84 | ||
| Operation time (min) | 120.0 ± 55.0 | 138.6 ± 50.9 | 120.0 ± 45.0 | 0.08 | |
| Blood loss (ml) | 125.0 ± 100.0 | 200.0 ± 150.0 | 100.0 ± 100.0 | 0.05 | |
| Time to surgery (day) | 5.0 ± 3.0 | 8.4 ± 4.7 | 5.0 ± 3.0 | 0.004 | |
| Fibular allograft | Yes | 22 | 5 | 17 | 0.21 |
| No | 76 | 9 | 67 | ||
| Disruption of medial region hinge | Yes | 61 | 11 | 50 | 0.18 |
| No | 37 | 3 | 34 | ||
| Neer classification | Two‐part | 32 | 3 | 29 | 0.54 |
| Three‐part | 60 | 11 | 49 | ||
| Four‐part | 6 | 0 | 6 | ||
| Recovery of MS | Yes | 73 | 5 | 68 | 0.001 |
| No | 25 | 9 | 16 |
Values are presented as the mean ± SD.
Abbreviations: CI, confidence intervals; MS, medial support.
By reviewing the radiographic data, there was no significant difference in fibular allograft, disruption of medial region hinges, and Neer classification (p > 0.05). However, a significant difference was found between the two groups in recovery of medial support (five of 14 vs 68 of 84, OR = 0.13, p = 0.001).
Independent Factors Predicting Complications
Multivariate logistic regression analysis with combinations of two independent variables (time to surgery and effective medial support) in the univariate analysis was performed, which showed both time to surgery (OR = 1.34, p = 0.002) and effective medial support (OR = 0.08, p = 0.001) were considered as independent predictors of avoiding postoperative complications (Table 2). Obviously, medial support was a protective independent predictor than time to surgery (OR 0.08 vs 1.34).
TABLE 2.
Multivariate logistic regression analyses with postoperative complication as outcome
| All cases | With complication | Without complication | p value | Odds ratio (95% CI) | |
|---|---|---|---|---|---|
| Time to surgery (day) | 5.0 ± 3.0 | 8.4 ± 4.7 | 5.0 ± 3.0 | 0.002 | 1.34 (1.11–1.62) |
| Medial support | 0.001 | 0.08 (0.02–0.35) | |||
| (+) | 73 | 5 | 68 | ||
| (−) | 25 | 9 | 16 | ||
Values are presented as the mean ± SD.
Abbreviation: CI, confidence intervals.
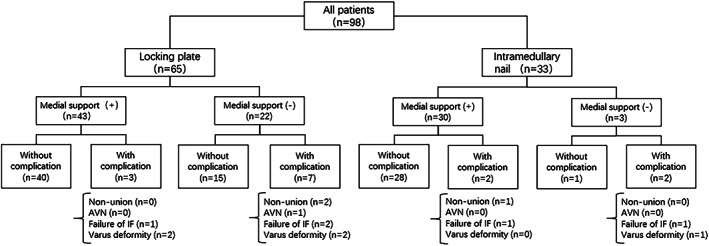
Then, all the patients were allocated into the locking plate group (n = 65) and the intramedullary nail group (n = 33). The medial support was proved as a statistical significance in two groups (the locking plate group, OR = 0.35, p = 0.015; intramedullary nail group, OR = 0.29, p = 0.02) (Figure 2). In addition, we found that only in the locking plate group, time to surgery was a significant predictor (OR = 1.41, p = 0.004).
Fig. 2.
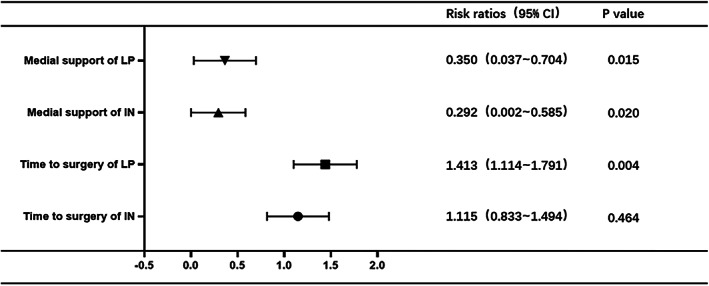
The forest plot illustrating the relationship between two risk factors (time to surgery and medial support) and with/without postoperative complications in locking plate and intramedullary nail fixation
Predictive Indicators (HR and VR)
There were four new indicators (horizontal ratio of locking plate, vertical ratio of locking plate, horizonal ratio of intramedullary nail, and vertical ratio of intramedullary nail) assessed and observed. Only the VRLP (p = 0.002) was considered a statistically significant predictor of postoperative complications (Figure 3).
Fig. 3.
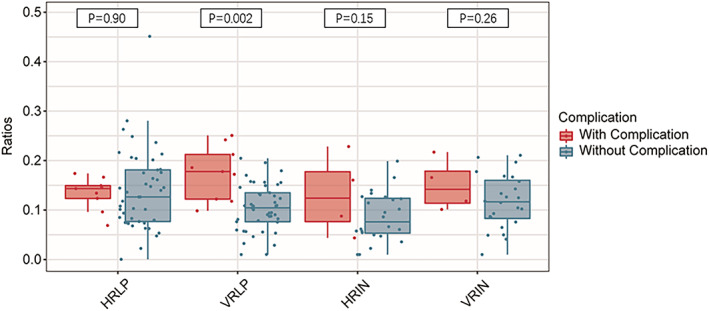
Relationship between new indicators proposed in this study and postoperative complications. In these four indicators (horizontal ratio of locking plate (HRLP), vertical ratio of locking plate (VRLP), horizonal ratio of intramedullary nail (HRIN), and vertical ratio of intramedullary nail (VRIN)), only a low VRLP significantly decreased the incidence of postoperative complications
A ROC curve was generated for VRLP to identify a threshold predictive of avoiding postoperative complications. The area under curve was calculated to assess the predictive value of VRLP, which came to 0.84. The optimal threshold to avoid postoperative complications was 0.1713 or less, of which the Youden index was 0.6. In addition, the sensitivity and specificity were 66.7% and 99.3%, respectively. The picture of ROC curve was shown in Figure 4, demonstrating that VRLP was very useful in the diagnosis of postoperative complications. The rate of postoperative complications increased significantly once the VRLP was more than 0.1713.
Fig. 4.
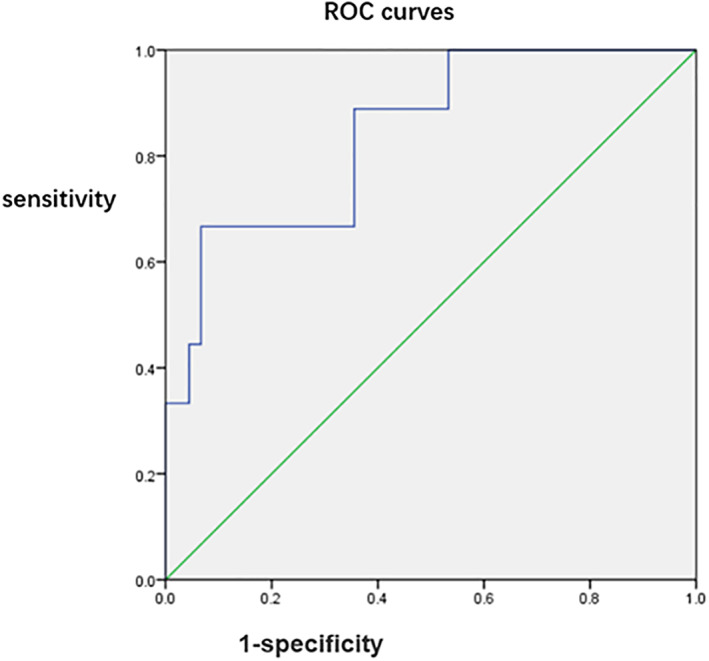
An AUC of receiver operating characteristic curve demonstrating the relationship between VRLP and postoperative complications
Postoperative Complications Results
No postoperative axillary nerve injury was found in locking plate group and in intramedullary nail group (Figure 5). All patients with non‐union or AVN received a secondary surgery. Failure of internal fixation (screw loosing and internal fixation breakage) was found in five of 98 patients in these two groups, which were treated with internal fixation removal (five of five) or replacement (two of five). Four of five patients with varus deformity preferred a conservative treatment and showed a satisfied result and the remaining one underwent an internal fixation removal which restricted his injured limb motion extremely at 8 months postoperatively.
Fig. 5.
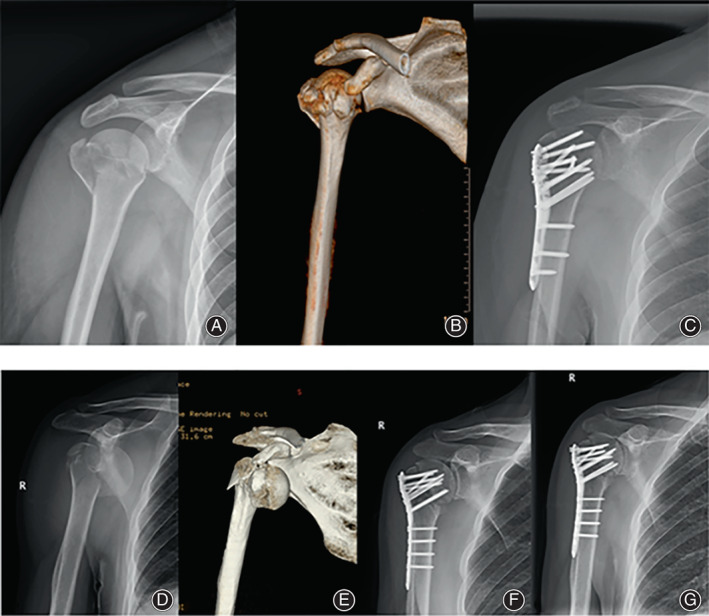
Two representative cases: (A–C) a 59‐year‐old female patient with a low VRLP achieved a better motion activity and clinical score; (D–G) a 60‐year‐old male suffered from a bone nonunion when VRLP exceeds the boundary values we provide in this article
Motion Outcomes and Score Evaluation Results
All cases were then subdivided into one of two groups according to the presence or absence of medial support, which showed no significant difference obtaining from healthy contralateral shoulder in shoulder motion activity, VAS score, and Constant score (p > 0.05) (Table 3). Furthermore, observed with injured limbs, patients with an effective medial support showed a significantly higher Constant score (p = 0.04) and superior performance on internal rotation (p = 0.04) (Table 4). However, no significant difference was found in VAS scores of both the healthy and the injured limbs (p > 0.05).
TABLE 3.
Mean shoulder activity, Constant score, and VAS score of healthy shoulder
| With MS | Without MS | p value | t value | |
|---|---|---|---|---|
| Flexion | 171.4 ± 6.9 | 170.9 ± 6.4 | 0.76 | −0.30 |
| Abduction | 144.2 ± 10.4 | 145.1 ± 8.2 | 0.7 | 0.38 |
| External rotation | 69.3 ± 9.5 | 69.4 ± 7.5 | 0.94 | 0.07 |
| Internal rotation | 76.4 ± 8.0 | 77.9 ± 5.9 | 0.39 | 0.86 |
| Constant score | 79.8 ± 6.9 | 80.5 ± 5.9 | 0.68 | 0.41 |
| VAS score | 0.4 ± 0.6 | 0.3 ± 0.6 | 0.72 | −0.36 |
Values are presented as the mean ± SD.
Abbreviations: MS, medial support; VAS, visual analog scale.
TABLE 4.
Mean shoulder activity, constant score, and VAS score of injured shoulder
| With MS | Without MS | p value | t value | |
|---|---|---|---|---|
| Flexion | 135.5 ± 19.6 | 136.6 ± 21.6 | 0.63 | 0.47 |
| Abduction | 122.7 ± 23.6 | 116.7 ± 21.6 | 0.06 | −1.93 |
| External rotation | 60.3 ± 19.6 | 56.4 ± 23.4 | 0.31 | 0.92 |
| Internal rotation | 70.3 ± 18.0 | 63.2 ± 18.9 | 0.04 | −2.20 |
| Constant score | 70.9 ± 15.9 | 67.2 ± 20.5 | 0.04 | −2.20 |
| VAS score | 1.8 ± 1.6 | 1.8 ± 1.1 | 0.96 | 0.06 |
Values are presented as the mean ± SD.
Abbreviations: MS, medial support; VAS, visual analog scale.
Representative Cases
To illustrate the importance of calcar screw placement in locking plate fixation, two typical cases were presented in Figure 6. A patient with a low VRLP achieved a great clinical outcome (Figure 6A–C). Conversely, one patient suffered from a bone nonunion attributing to a high VRLP (Figure 6D–G).
Fig. 6.
A demographic tree shows the cohort breakdown of patients in which internal fixation was used. Cohorts are further subdivided into whether the medial support was achieved. These additionally were subclassified as with or without complications
Of note, another case was more representative, of which one patient with a medial region disruption and anterior dislocation of shoulder received a locking plate fixation (Figure 7A,B). It was found that the humerus stem and head had poor concord at 3 months postoperatively (Figure 7C). Benefiting from accurate calcar screw placement and active rehabilitation exercises, she achieved a satisfied clinical outcome without secondary surgery (Figure 7D).
Fig. 7.
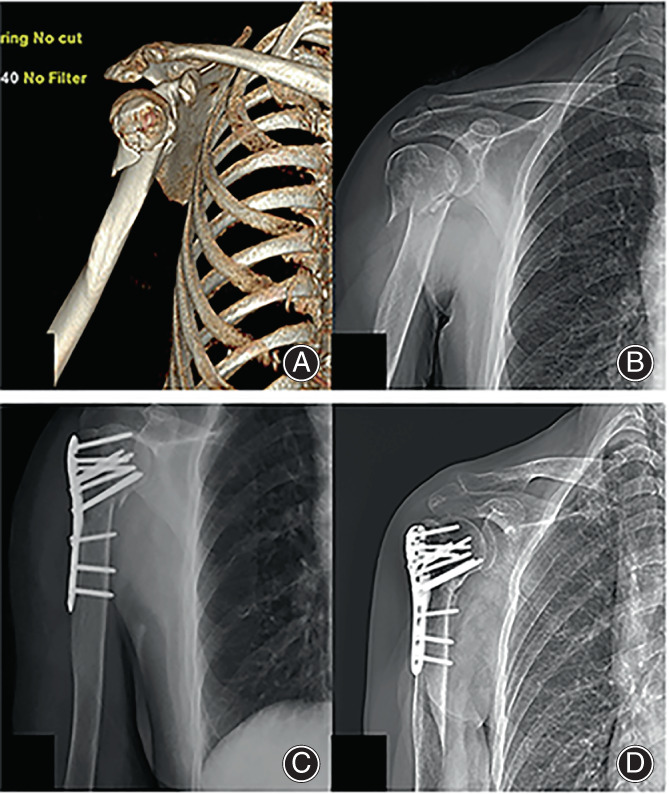
(A, B) A 73‐year‐old female patient suffered from a proximal humerus fracture with medial region hinges and anterior dislocation of shoulder. (C) A 3‐month postoperative X‐ray showed that the humerus stem was not matched up with head perfectly. (D) Eventually, she achieved a satisfied clinical outcome without secondary surgery, which benefited from accurate calcar screw placement and active rehabilitation exercises
Discussion
Importance and Methods for Recovery of Medial Support
Our study demonstrated that locked screws placed into humerus head stabilize the medial column. This idea was first proposed by Gardener, which was also reported in systematic reviews by Thanasas et al. and Oppebøen et al.. 6 , 18 , 19 Hepp et al. found that the medial region provided the sufficient trabecular density, which demonstrated that precise reduction of screws relied on fixation in the lower inner quadrant of humerus head. 20
Zhang et al. believed that the medial region supported by three calcar screws would have significant biomechanical advantages. 21 However, in complex fracture patterns, it was difficult for calcar screws to provide stability for the medial region. Kim et al. considered the medial column of the humerus was quite different from the femur. 22
Our study mentioned that patients with medial support achieved better activity on internal rotation, which required a finite element analysis or an in‐vitro experiment to verify.
There was still much controversy around calcar screws application on intramedullary nail. Katthagen et al. doubted that calcar screws in intramedullary nail contributed to the medial support. 23 However, in our study, we found that effective medial support was a protective factor to avoid postoperative complications in the intramedullary nailing group.
The clinical results of our study showed a statistically significant association between time to surgery and postoperative complications. Menendez et al. presented that delayed surgery (i.e., 3 or more days after trauma) might increase the inpatient morbidity, postoperative length of stay, and unconventional discharge. 24
Postoperative Complications without Medial Support
Our research included non‐union, AVN, failure of internal fixation (screw loosening and plate breakage), and varus deformity. Oppebøen et al. demonstrated the protective effect of the medial support on the avoidance of varus deformity. 19 Agudelo et al. further proved that application of calcar screws obtained axial loading and stiffness for humerus head to avoid varus deformity and decrease the risk of surgery failure on their retrospective studies. 25 In our study, only one patient (1%) had AVN, which showed significant absence of the humerus head in imaging findings. The fracture pattern of this patient was involved with the anatomic neck, considered to be a predictor of osteonecrosis of the humerus head presented by Hertel et al.. 16 In previous studies, however, the incidence of AVN ranged from 1.9% to 16.2%. 26 , 27 , 28 , 29 Osterhoff et al. found no statistical relationship between the absence of AVN and the medial support, which might be explained by abundant blood supply and collateral circulation of the humerus head. 30
In our study, there were three (3.1%) patients diagnosed with bone non‐union, which was in the lower range of previous articles ranging from 0% to 16% reported. 28 , 31 , 32 , 33 However, these articles reported that many factors had an influence on non‐union including fracture type, previous smoking history, osteoporosis, and premature rehabilitation.
Screw loosening and plate breakage were also included in our article. A recent series made by Ciric et al. reported that placing calcar screws closely to the subchondral bone of humerus head did not increase the risk of screw loosening. 34 In contrast, placing short calcar screws could lead to screw loosening and secondary varus deformity. In a finite element analysis of Yang et al., it pointed out that with the absence of medial support, the intense pressure near the calcar screws of the locking plate contributed to the high rate of plate breakage and iatrogenic fractures. 35 In keeping with the study by Fletcher et al., this author further proved that the arrangement of calcar screws might be of great relevance for preventing plate breakage. 36 New predictive indicators proposed in our study would be beneficial to avoid the occurrence of these postoperative complications.
Appropriate Placement of Calcar Screws in Locking Plate Fixations
A recent article has presented a clear definition on the placement of the calcar screw. 37 In this research, the authors believed that precise calcar screw positioning, such as the bottom of the calcar screw closed to the medial region and the tip of the screw closed to the subchondral bone, could avoid internal fixation failure. Alternatively, they reported that current locking‐plate technology allowed precise calcar screw placement for reduction quality. In addition, they proposed two indicators named calcar ratio and calcar distance, which were also helpful to evaluate the placement of calcar screw. Our study proposed new predictive indicators, which were obtained from both anteroposterior and lateral radiographs, to investigate the appropriate position of calcar screw either in plate or intramedullary nail fixation. In order to explore critical point, we established a relationship between calcar screws and postoperative complications.
Zeng et al. held the opinion that with a low‐grade medial cortical reduction, multiple and effective calcar screws were of benefit to obtain the stability of fixation and maintain the reduction of fractures. 38 Moreover, these authors attempted to build a relationship between the arrangement of calcar screws and VAS score, which was considered no statistical significance.
Recent studies indicated that imaging failure was highly collated with reoperation. 37 , 39 After determining the importance of medial region support, we attempted to establish a relationship between predictive indicators and the postoperative complications, including AVN, non‐union, plate breakage, screw loosening, and varus deformity. Unfortunately, there were no statically significant results between these indicators and complications in intramedullary nail groups. However, we found that the VRLP was statistically significant to postoperative complications. The incidence of postoperative complications increased dramatically once the VRLP was more than 17%. In locking plate fixation, once calcar screws placed in vertical positions outside of the thresholds were identified in our results, patients were at increased risk for fixation failure and secondary operation.
Limitations and Conclusions
We acknowledge that this study has several limitations, including its retrospective design. The relatively small series size limits the reliability of our study. However, the results of our study suggest that the calcar screw can be placed with quantifiable position and a low rate of postoperative complications. Future reports, including more prospective trials, will stress clinical characteristics of medial region hinge of humerus head by using finite element of biomechanics analysis.
Our study demonstrated that the time to surgery and effective medial support had a significant influence on postoperative complications of proximal humerus fractures in locking plate and intramedullary nail fixation. The precise placement of calcar screws was important to achieve anatomic reduction in locking plate internal fixation. The incidence of postoperative complications increased significantly when the VR of calcar screws exceeded the 0.1713.
AUTHORS' CONTRIBUTIONS
Hanzhou Wang designed this study. Yang Liu and Dong Wang collected and analyzed the data. Hanzhou Wang and Junlin Zhou wrote the article. Yuanming He, Peifeng Yao and Tianchao Lu revised the article. All the authors read and approved the final manuscript.
ETHICAL STATEMENT
This study was approved by the Ethics Committee of Beijing Chaoyang Hospital (approval no. 2021‐ke‐441). The Committee waived the requirement for written informed consent because the study was retrospective, it did not have any adverse effect on patients' health, and it reported anonymized patient data.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
FINANCIAL DISCLOSURE
The authors declared that this study has received no financial support.
ACKNOWLEDGMENTS
We would like to acknowledge the help provided by residents and other staff members in conducting this study.
REFERENCES
- 1. Passaretti D, Candela V, Sessa P, Gumina S. Epidemiology of proximal humeral fractures: a detailed survey of 711 patients in a metropolitan area. J Shoulder Elbow Surg. 2017;26:2117–24. [DOI] [PubMed] [Google Scholar]
- 2. Rangan A, Handoll H, Brealey S, Jefferson L, Keding A, Martin BC, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA. 2015;313:1037–47. [DOI] [PubMed] [Google Scholar]
- 3. Tamimi I, Montesa G, Collado F, González D, Carnero P, Rojas F, et al. Displaced proximal humeral fractures: when is surgery necessary? Injury. 2015;46:1921–9. [DOI] [PubMed] [Google Scholar]
- 4. Hardeman F, Bollars P, Donnelly M, Bellemans J, Nijs S. Predictive factors for functional outcome and failure in angular stable osteosynthesis of the proximal humerus. Injury. 2012;43:153–8. [DOI] [PubMed] [Google Scholar]
- 5. Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011;42:408–13. [DOI] [PubMed] [Google Scholar]
- 6. Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma. 2007;21:185–91. [DOI] [PubMed] [Google Scholar]
- 7. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma. 2008;22:195–200. [DOI] [PubMed] [Google Scholar]
- 8. Hinds RM, Garner MR, Tran WH, Lazaro LE, Dines JS, Lorich DG. Geriatric proximal humeral fracture patients show similar clinical outcomes to non‐geriatric patients after osteosynthesis with endosteal fibular strut allograft augmentation. J Shoulder Elbow Surg. 2015;24:889–96. [DOI] [PubMed] [Google Scholar]
- 9. Zhang L, Zheng J, Wang W, Lin G, Huang Y, Zheng J, et al. The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospective randomized study. Int Orthop. 2011;35:1655–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jung WB, Moon ES, Kim SK, Kovacevic D, Kim MS. Does medial support decrease major complications of unstable proximal humerus fractures treated with locking plate? BMC Musculoskelet Disord. 2013;14:102–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lin SJ, Tsai YH, Yang TY, Shen SH, Lee MS. Medial calcar support and radiographic outcomes of plate fixation for proximal humeral fractures. J Biomed Biotechnol. 2015;2015:170283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Neer C. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Jt Surg, Am Vol. 1970;52(6):1077. [PubMed] [Google Scholar]
- 13. Franceschi F, Franceschetti E, Paciotti M, Torre G, Denaro V. Surgical management of osteonecrosis of the humeral head: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;25:1–9. [DOI] [PubMed] [Google Scholar]
- 14. Ponce BA, Thompson KJ, Raghava P, Eberhardt AW, Tate JP, Volgas DA, et al. The role of medial comminution and calcar restoration in varus collapse of proximal humeral fractures treated with locking plates. J Bone Jt Surg, Am Vol. 2013;95(16):e113. [DOI] [PubMed] [Google Scholar]
- 15. Sudkamp N, Bayer J, Hepp P, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg, Am. 2009;91(6):1320–8. [DOI] [PubMed] [Google Scholar]
- 16. Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13:427–33. [DOI] [PubMed] [Google Scholar]
- 17. Tashjian RZ, Hung M, Keener JD, Bowen RC, McAllister J, Chen W, et al. Determining the minimal clinically important difference for the American shoulder and elbow surgeons score, simple shoulder test, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(1):144–8. [DOI] [PubMed] [Google Scholar]
- 18. Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg. 2009;18:837–44. [DOI] [PubMed] [Google Scholar]
- 19. Oppebøen S, Wikerøy AKB, Fuglesang HFS, Dolatowski FC, Randsborg PH. Calcar screws and adequate reduction reduced the risk of fixation failure in proximal humeral fractures treated with a locking plate: 190 patients followed for a mean of 3 years. J Orthop Surg Res. 2018;13:197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hepp P, Lill H, Bail H, Korner J, Niederhagen M, Haas NP, et al. Where should implants be anchored in the humeral head? Clin Orthop Relat Res. 2003;415:139–47. [DOI] [PubMed] [Google Scholar]
- 21. Wen Z, Langqing Z, Yanjie L, et al. The mechanical benefit of medial support screws in locking plating of proximal humerus fractures. PLoS One. 2014;9:e103297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim DS, Lee DH, Chun YM, Shin SJ. Which additional augmented fixation procedure decreases surgical failure after proximal humeral fracture with medial comminution: fibular allograft or inferomedial screws? J Shoulder Elbow Surg. 2018;S1058274618302295:1852–8. [DOI] [PubMed] [Google Scholar]
- 23. Katthagen JC, Schwarze M, Bauer L, Meyer‐Kobbe J, Lill H. Is there any advantage in placing an additional calcar screw in locked nailing of proximal humeral fractures? Orthop Traumatol Surg Res. 2015;101:431–5. [DOI] [PubMed] [Google Scholar]
- 24. Menendez ME, Ring D. Does the timing of surgery for proximal humeral fracture affect inpatient outcomes? J Shoulder Elbow Surg. 2014;23:1257–62. [DOI] [PubMed] [Google Scholar]
- 25. Agudelo J, Schürmann M, Stahel P, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2015;21:676–81. [DOI] [PubMed] [Google Scholar]
- 26. Boesmueller S, Wech M, Gregori M, Domaszewski F, Albrecht C. Risk factors for humeral head necrosis and non‐union after plating in proximal humeral fractures. Injury. 2016;47:350–5. [DOI] [PubMed] [Google Scholar]
- 27. Ricchetti ET, Warrender WJ, Abboud JA. Use of locking plates in the treatment of proximal humerus fractures. J Shoulder Elbow Surg. 2010;19:66–75. [DOI] [PubMed] [Google Scholar]
- 28. Brunner F, Sommer C, Bahrs C, Heuwinkel R, Hafner C, Rillmann P, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma. 2009;23:163–72. [DOI] [PubMed] [Google Scholar]
- 29. Voigt C, Geisler A, Hepp P, Schulz AP, Lill H. Are polyaxially locked screws advantageous in the plate osteosynthesis of proximal humeral fractures in the elderly? A prospective randomized clinical observational study. J Orthop Trauma. 2011;25:596–602. [DOI] [PubMed] [Google Scholar]
- 30. Osterhoff G, Hoch A, Wanner GA, Simmen HP, Werner CML. Calcar comminution as prognostic factor of clinical outcome after locking plate fixation of proximal humeral fractures. Injury. 2012;43:1651–6. [DOI] [PubMed] [Google Scholar]
- 31. Gadea F, Favard L, Boileau P, Cuny C, d'Ollone T, Saragaglia D, et al. Fixation of 4‐part fractures of the proximal humerus: can we identify radiological criteria that support locking plates or IM nailing? Comparative, retrospective study of 107 cases. Orthop Traumatol, Surg Res. 2016;102:963–70. [DOI] [PubMed] [Google Scholar]
- 32. Konrad G, Audigé L, Lambert S, Hertel R, Südkamp NP. Similar outcomes for nail versus plate fixation of three‐part proximal humeral fractures. Clin Orthop Relat Res. 2012;470:602–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22:542–9. [DOI] [PubMed] [Google Scholar]
- 34. Ciric D, Mischler D, Qawasmi F, Wenzel L, Richards RG, Gueorguiev B, et al. Secondary perforation risk in plate osteosynthesis of unstable proximal humerus fractures: a biomechanical investigation of the effect of screw length. J Orthop Res. 2019;37:2625–33. [DOI] [PubMed] [Google Scholar]
- 35. Yang P, Zhang Y, Liu J, Xiao J, Ma LM, Zhu CR. Biomechanical effect of medial cortical support and medial screw support on locking plate fixation in proximal humeral fractures with a medial gap: a finite element analysis. Acta Orthop Traumatol Turc. 2015;49:203–9. [DOI] [PubMed] [Google Scholar]
- 36. Fletcher JWA, Windolf M, Richards RG, Gueorguiev B, Varga P. Screw configuration in proximal humerus plating has a significant impact on fixation failure risk predicted by finite element models. J Shoulder Elbow Surg. 2019;28:1816–23. [DOI] [PubMed] [Google Scholar]
- 37. Padegimas EM, Zmistowski B, Lawrence C, Palmquist A, Nicholson TA, Namdari S. Defining optimal calcar screw positioning in proximal humerus fracture fixation. J Shoulder Elbow Surg. 2017;S1058274617302549:1931–7. [DOI] [PubMed] [Google Scholar]
- 38. Zeng LQ, Zeng LL, Jiang YW, Wei HF, Zhang W, Chen YF. Influence of medial support screws on the maintenance of fracture reduction after locked plating of proximal humerus fractures. Chin Med J (Engl). 2018;131(15):1827–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Schnetzke M, Bockmeyer J, Porschke F, Studier‐Fischer S, Grutzner PA, Guehring T. Quality of reduction influences outcome after locked‐plate fixation of proximal humeral type‐C fractures. J Bone Jt Surg, Am. 2016;98:1777–85. [DOI] [PubMed] [Google Scholar]


