Introduction
COVID-19 is an infectious disease caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). A phenomenon of long COVID has been documented among COVID-19 patients. Long COVID syndrome can be broadly categorized into postacute COVID where symptoms last for three to 12 weeks and chronic COVID where symptoms last for more than 12 weeks.1 These “Long Haulers” continue to have symptoms after virological recovery, that is, being reverse transcription–polymerase chain reaction (RT-PCR) negative.2-4 The prevalence of these long COVID-19 varies from 35% to 87.4%.5
These persistent symptoms may range from shortness of breath, cognitive dysfunction, and fatigue. Other symptoms may include chest pain, body ache, anxiety and depression, and hair shedding.
In India, a COVID registry was started for identifying long-term effects of COVID-19.6 However as of now the literature of long COVID is scarce in India. Hence, moderate to severe cases were followed up for 24 weeks for estimating the prevalence and identifying factors associated with long COVID among discharged patients of the hospital.
Methods
The study was conducted at a makeshift Dedicated COVID Hospital in Delhi, India. Only moderate to severe cases according to Indian Council of Medical Research (ICMR) guidelines were admitted in the hospital. All the recovered patients who were discharged from the hospital from April 2021 to June 2021 were approached for the study.
The patients who consented to participate in the study were contacted telephonically at three and six months post-discharge. Patients who did not respond even after three telephonic call attempts at different duration of the day were labeled as nonresponder. Patients who refused to participate in the study during the study period, reinfected with COVID-19 in between the study period, or died in between the period of study were excluded.
Baseline data of the patients were collected from the hospital Health Management Information System (HMIS) system using case record form. Interviewers were trained to interview the participants, telephonically, with the help of the pretested questionnaire. The study was given ethical clearance from institutional ethical committee vide their letter number IEC\2021\73 dated June 13, 2021. Data were analyzed using IBM SPSS Statistics for Windows, version 20 (IBM Corp, Armonk, New York). P value of less than .05 was taken as significant.
Results
A total of 345 patients participated in the study. The mean age of the participants was 52.7 (SD = 15.1) years, median: 53 (interquartile range [IQR] = 20) years. Of the total participants, 228 (66.1%) were men. A total of 151, 43.8% (95% confidence interval [CI]: [38.5, 49.2]), of the patients had one or more co-morbidities. Diabetes mellitus was found to be the most common co-morbidity (70/151), followed by hypertension (47/151), hypothyroidism (11/151), and cardiac disease (8/151). A total of 146 and 50 patients had one and two doses of COVID-19 vaccine, respectively.
Three Months Follow-up
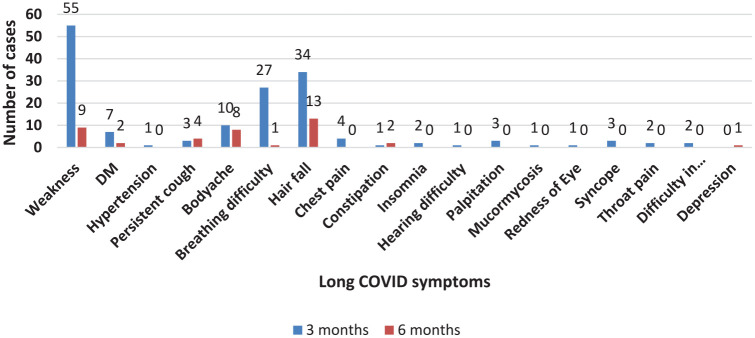
A total of 117 patients, 33.9% (95% CI: [28.9, 39.2]), gave history of long COVID. Most common symptom was weakness, contributing 55, 15.9% (95% CI: [12.2, 20.2]), followed by hairfall 34, 9.9% (95% CI: [6.9, 14.5]), and difficulty in breathing 27, 7.8% (95% CI: [5.2, 11.2]) (Figure 1).
Figure 1.
Long COVID symptoms after three and six months of discharge.
Male gender and patients with co-morbidities had 0.7 (95% CI: [0.5, 1.2]) times and 1.4 (95% CI: [0.9, 2.2]) times more risk of developing long COVID symptoms, respectively. Patients with both doses of vaccination had 0.4 (95% CI: [0.2, 0.9]) times more chance of developing long COVID symptoms (Table 1).
Table 1.
Risk and Association of Various Factors With Development of Long COVID Symptoms After Three and Six Months of Discharge.
| Long COVID (three months) | OR (95% CI) | Long COVID (six months) | OR (95% CI) | |||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | |||
| Sex | ||||||
| Male | 72 | 156 | 0.738 [0.464, 1.176] |
17 | 30 | 0.425 [0.163, 1.106] |
| Female | 45 | 72 | 16 | 12 | ||
| Comorbidities | ||||||
| Yes | 58 | 93 | 1.427 [0.911, 2.235] |
14 | 10 | 2.358 [0.876, 6.348] |
| No | 59 | 135 | 19 | 32 | ||
| Both doses of vaccine | ||||||
| Yes | 10 | 40 | 0.439 [0.211, 0.914] |
27 | 36 | 0.750 [0.218, 2.583] |
| No | 107 | 188 | 6 | 6 | ||
Abbreviations: CI, confidence interval; OR, odds ratio.
Six Months Follow-up
Of 117 patients (long COVID at three months), only 75 were followed up (two patients died, 29 refused to participate, 11 could not be contacted, and 18 suffered from reinfection). There was no statistically significant difference, in age (P = .8), comorbidities (P = .7), and vaccination status (P = .3), between the nonparticipants and the participants. Of these participants, 63, 84% (95% CI: [73.7, 91.5]), had received both doses of vaccine and 24, 32% (95% CI: [21.7, 43.8]), had co-morbidities. About 50% of the participants, who had co-morbidities, had hypertension, followed by diabetes mellitus in 25% participants.
Long COVID symptoms persisted in 33, 44% (95% CI: [32.6, 55.9]) of the participants. Most common symptom was hairfall, observed in 17.3% (n = 13) participants. This was followed by weakness, 12% (n = 9); body ache, 10.6% (n = 8); and cough, 5.3% (n = 4). Patients with co-morbidities and vaccinated were at 2.4 (95% CI: [0.9, 6.5]) and 0.8 (95% CI: [0.3, 2.6]) times more risk of suffering from long COVID after six months.
Discussion
The prevalence of long COVID in our study was found to be 33.9% after three months follow-up. About 44% of the participants who had long COVID after three months continued to have symptoms after six months of follow-up. Our study is one of the very few in our country to have followed up patients up to six months for long COVID.
Chest tightness and palpitation on exertion were the most common long COVID symptoms after three months of discharge from hospital followed by dyspnea and fatigue and cough in a study conducted by Limei Liang et al.7 In contrast, in our study most common symptoms were weakness, hairfall, and dyspnea.
Fatigue and weakness were the most common symptoms after 186 days of follow-up,8 which is similar to our study. Our study revealed a significant association between two doses of COVID vaccine and its relative protection against long COVID, after three months of discharge, similar to a study conducted by Paul Kuodi et al.9 No significant association was found between both doses of vaccination and development or persistence of long COVID symptoms after six months of discharge probably due to low power.
Among moderate to severe cases of COVID-19, more than one-third have persistence of symptoms at three months; hence, from a public health point of view a large number of COVID-19 patients may require health care facility even after discharge; the need for surveillance and long-term follow-up of these patients cannot be overemphasized.
Conclusion
The present study finds that long COVID symptoms are prevalent among a significant number of hospitalized patients post-discharge. Symptoms may even persist till six months after discharge from hospital. They may vary from general symptoms like fatigue and body ache, dyspnea, and alopecia to even new onset diabetes.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Arun Kumar Yadav  https://orcid.org/0000-0001-5751-5134
https://orcid.org/0000-0001-5751-5134
References
- 1.Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute COVID-19 in primary care. BMJ. 2020;370:m3026. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 2.Crook H, Raza S, Nowell J, Young M, Edison P.Long COVID—mechanisms, risk factors, and management. BMJ. 2021;374:n1648. doi: 10.1136/bmj.n1648. [DOI] [PubMed] [Google Scholar]
- 3.Yong E. COVID-19 can last for several months. The Atlantic. Published June 4, 2020. Accessed February 26, 2022. https://www.theatlantic.com/health/archive/2020/06/covid-19-coronavirus-longterm-symptoms-months/612679/.
- 4.Garg P, Arora U, Kumar A, Wig N.The “post-COVID” syndrome: how deep is the damage. J Med Virol. 2021;93(2):673-674. doi: 10.1002/jmv.26465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(30):993-998. doi: 10.15585/mmwr.mm6930e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Clinical Registry. Accessed March 22, 2022. https://www.icmr.gov.in/tab3ob1.html.
- 7.Liang L, Yang B, Jiang N, et al. Three-month follow-up study of survivors of coronavirus disease 2019 after discharge. J Korean Med Sci. 2020;35(47):e418. doi: 10.3346/jkms.2020.35.e418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220-232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuodi P, Gorelik Y, Zayyad H, et al. Association between vaccination status and reported incidence of post-acute COVID-19 symptoms in Israel: a cross-sectional study of patients tested between March 2020 and November 2021. medRxiv, 2022. doi: 10.1101/2022.01.05.22268800. [DOI] [Google Scholar]