Abstract
Background
The concept of mobile health has attracted considerable attention across the globe, as it provides both healthcare professionals and patients with a distinct means of information and resources.
Aim
This study was conducted with the aim of utilising mobile health (mHealth) applications by nurses and presenting a scenario of how and why they are utilised.
Methods
This study was a scoping review. Data collection was carried out by searching the related keywords in Google Scholar, Scopus, Cochrane, EMBASE, Ovid, and PubMed databases from January 2000 to March 2019.
Results
Regarding the reasons for using mobile applications by nurses, five objectives were identified, including learning and knowledge enhancement, treatment and improvement of the patient care process, diagnostic process, data and patient management, and health promotion. Effective factors in the nurses’ use of mobile applications were categorised into eight themes: ease of use, usefulness, security and confidentiality, feasibility and functionality, design and use—interface, effectiveness, infrastructure, versatility, and social norms.
Conclusions
Mobile health applications have considerable potential in enhancing nurses’ professional activities. This study contributes to both nursing and health policy by providing a scenario of how and why nurses use mobile health applications.
Keywords: application, mobile, mobile health applications, nurse
Introduction
With the advent of commercialised phones in the year 1983, cell phone technology has spread with unprecedented speed (DeGusta, 2012). Miniaturisation along with advances in sensors, batteries, and computational technologies has resulted in the release of the first collection of smart-phones in 2007 and tablets 1 year later. Both devices are able to independently run software programs known as applications. This issue has changed the role of these devices to beyond simple telephone communication (Johnston et al., 2015). Like any other computer, a mobile has a variety of different software applications. In the mobile application market, the term “application” or App, for short, is more common than the term software and this expression has the same meaning as software application, which is known as the mobile application or mobile software. One of the common methods used today to obtain health information are through the use of mobile applications (Mobasheri et al., 2015).
These technologies have created a revolution in people’s lives and led to a great interest in their utilisation in the healthcare industry. In healthcare, mHealth is defined as providing health services by using transportable communication devices (Whittaker, 2012). By using mHealth, the majority of these programs are made available to users, indirectly, and result in improving a healthy lifestyle or empowering patients to manage conditions of their disease. Nevertheless, a growing number of applications has been designed which are specifically for professional healthcare use in the clinical environment in order to increase efficiency regarding design-related tasks (Mobasheri et al., 2015).
Mobile phones’ distinctiveness, portability, and ability to connect to healthcare specialists help them to access health-related content at practically any time or place (Ozdalga et al., 2012). A reliable healthcare institute, such as the National Institute for Health and Care Excellence in England has provided access to most of its regulations for physicians in the form of applications in order to facilitate decision-making. Regardless of the enthusiasm towards digital health, errors exist, and numerous studies have shown the potential of some applications in creating injury for patients (Haffey et al., 2013; Mobasheri et al., 2014; Wolf et al., 2013). In addition, the use of mobile phones in the clinical domain has created specific safety and privacy concerns, which should be considered to overcome risks of violations in the patients’ highly sensitive diagnostic and personal data (Hagbaghery et al., 2004; Martínez-Pérez et al., 2015).
Among the medical staff, nurses have a direct responsibility in maintaining the health of individuals and are in close contact with their patients. With this in mind, nurses have numerous important roles that include providing clinical care, consultation, follow-up of accurate treatment and teaching disease prevention methods (Hagbaghery et al., 2004). Nurses make up the largest group of health care providers and play a significant role in the continuity of healthcare, improving, and maintaining health at various levels of the healthcare system (Hagbaghery et al., 2004). On the other hand, as one of the key components in the healthcare system, nurses have a valuable role in educating patients because they have better access to the patients and their families and spend a great amount of time caring for them (Marcum et al., 2002; Sullivan and Decker, 1998). Continuous scientific advances along with the patients changing condition requires nurses to diagnose patients’ problems by integrating their technical skills and professional knowledge, and taking a step towards reducing errors and increasing the quality of healthcare by designing, implementing and evaluating the program. During the past few years, it has been found that nurses who based their services on reliable health information were able to make better decisions and provide higher quality healthcare services (Rahimi and AhmadianMajin, 2017).
Mobile health applications have a considerable potential in enhancing nurses’ professional activities and are mostly used by nurses for various reasons. However, as it was mentioned above, all of these applications have not been successful and worries still exist, such as compatibility with the nurses’ job and privacy and safety concerns. Until now, a number of studies have been carried out regarding the reasons for nurses’ use of mobile health applications and effective factors in their behaviour when using these applications. In this study, we evaluate issues such as the objective of these studies, the type of study, study population, use of mobile applications, explanations of mobile applications, effective factors in nurses’ use of these mobile applications, criteria reported for the assessment and evaluation of mobile health applications, and the results obtained from these studies.
Methodology
Search Strategy
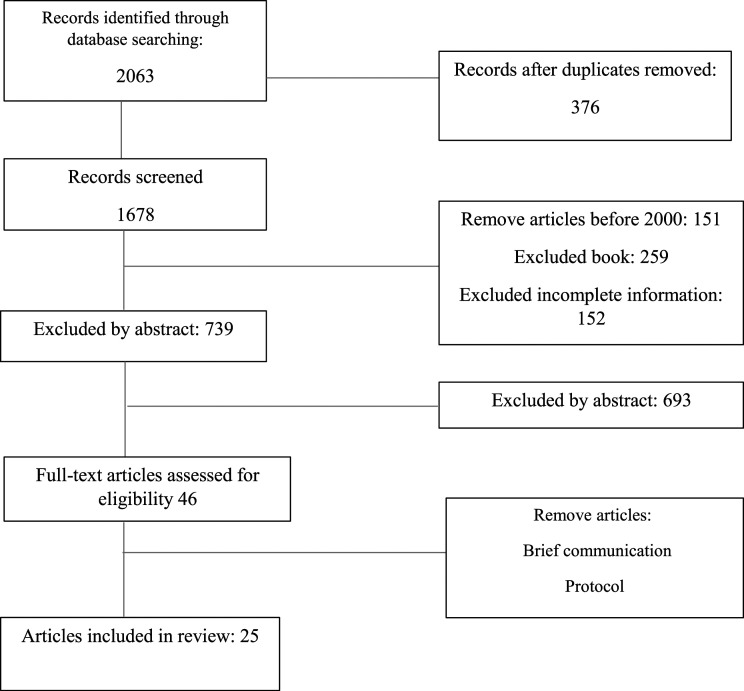
The study was a scoping review and is presented using the PRISMA-ScR checklist (Tricco et al., 2018). The search was conducted in Google Scholar, Scopus, Cochrane, EMBASE, Ovid, and PubMed databases, without any limitation during the search. However, after retaining the articles, we considered a limit for date of publication between 2000 and 2019 and articles that were in this range were included in the study. The search was conducted based on the following keywords: “electronic, application, apps, app, clinical staff, nurse, nurses, smart-phone, smart phone, smart phone, cell phone, cellphone, tablet, mobile, device, mobile applications software.” A total of 2063 articles were retained. Three hundred and seventy-six articles were eliminated due to duplication among databases. Among the 1678 remaining articles, 151 articles published before the year 2000 were eliminated. Two hundred and fifty-nine items were excluded because they were books and another 152 articles were excluded due to incomplete information. Finally, 739 articles remained for which the initial evaluation was done based on article title. After this evaluation based on the abstracts, 693 irrelevant articles were excluded, leaving a number of 46 articles. 21 of these articles were eliminated from the study due to the type of articles including brief communication, protocol, commentary, and feature. Ultimately, the 25 remaining articles were included in the study. The search and inclusion process are provided in Figure 1 (Tricco et al., 2018).
Figure 1.
Search and inclusion process of the study (07/21/2020).
Inclusion and Exclusion Criteria
The inclusion criteria are as follows: (1) articles introducing the application programs (2) articles that studied nurses working in hospitals (3) articles in which mobile health applications were in line with nurses’ responsibilities (4) articles that provided access to the full text.
The exclusion criteria are as follows: (1) articles related to teaching mobile applications (2) articles related to nursing care at home and (3) articles that did not provide access to full text, were all excluded from the study.
Results
After evaluating and eliminating duplicates and excluding articles based on inclusion and exclusion criteria, 25 articles finally remained and were used for evaluation.
In this study, the following two research questions are put forth
1. For what reasons and purposes do nurses use mobile health applications?
2. What are the effective factors in nurses’ use of health mobile applications?
The Process of Publishing Articles
The article publication process is related to the year 2000 onwards, and the number of studies carried out has increased after 2017, with most studies conducted in 2018 (eight studies). Figure 2 shows the trend of publication during these years.
Figure 2.
Trend of publication from 2000 to 2019 (07/21/2020).
Countries that Conducted the Studies
Articles were published in 15 countries including the USA (four articles), Switzerland (three articles), India (three articles), Korea (two articles), Brazil, Spain, Taiwan, Ghana, New Zealand, Canada, Australia, the Netherlands, Italy, South Korea, and Sweden (each with one article). Based on the latest classification of the World Trade Bank in 2019/2020, 18 studies were conducted in high-income countries, one study was conducted in an average-to-high-income country, and four studies were conducted in average-to-low-income countries. Among these statistics, it is concluded that in high-income countries, nurses have a greater tendency of using mobile health applications.
Evaluation Objectives in the Studies
Considering the reasons for nurses’ use of mobile health applications, these reasons are categorised into five main themes of “learning and knowledge enhancement”, “treatment and improvement of the patient care process”, “improvement of the diagnostic process”, “data and patient management”, and “health promotion”, and 52 subthemes have been identified as presented in Table 1.
Table 1.
Objectives of using mHealth applications.
| Theme | Subtheme |
|---|---|
| 1. Learning and knowledge enhancement | • Anticoagulation knowledge |
| • Ensuring current evidence-based findings are disseminated to targeted end-users in a timely manner | |
| • Equipped with features based on the educational goals and practicum course | |
| • Evidence-based clinical decision support (CDS) | |
| • Improve nurses’ atrial fibrillation | |
| • Support nursing students | |
| • Support tool for inexperienced case managers/district nurses | |
| • Supporting an in-depth problem assessment | |
| 2. Treatment and improvement of the patient care process | • Assess the personal health status of patients |
| • Automated short-messaging service to reinforce compliance to drug intake | |
| • Avoid medical errors | |
| • Increase medication safety | |
| • Decrease medication errors | |
| • Reduce medication errors and time to drug delivery | |
| • Search for chemotherapy drugs | |
| • Developed to facilitate brief conversations between patients and clinicians as part of clinical care | |
| • Follow-up visit | |
| • Grounded in Krishnamacharya–Desikachar yoga therapy | |
| • Helps users to assess pain intensity | |
| • Improve cardiovascular disease (CVD) detection | |
| • Improve the quality of care | |
| • Medical order check | |
| • Monitor patients bio-features | |
| • Nursing care plan | |
| • Self-monitoring of the disease progression | |
| 3. Improve the diagnostic process | • Assist the early diagnosis |
| • Provide a broader/better overview of possible solutions | |
| • Provide a guideline/checklist for problem assessment and advice on solutions | |
| • Provide up-to-date information | |
| 4. Data and patient management | • Support nurses in their daily workflow |
| • Birth data tracking and analysis | |
| • Data entry | |
| • Data recording is made at the bedside | |
| • Documentation practices | |
| • Effective manner | |
| • Hospital electronic health record (EHR) | |
| • Facilitate documentation at the bedside | |
| • Frequency in communicating the need to use the bathroom and the need to get something | |
| • Integrate management of chronic conditions | |
| • Longitudinal health data | |
| • Manage data for the care of mothers, infants and children | |
| • Mobile electronic medical record | |
| • Modified to solve problems in the PC based EMR application | |
| • Nursing recording | |
| • Patient information management | |
| • Personalisation | |
| • Provide easy input interface and various outputs for nursing records | |
| • Support documentation of nurses at bedside using a user-centred approach | |
| 5. Health promotion | • Guided approach for promoting health and healing |
| • Health indicators for patients to track physical activity, diet, and sleep | |
| • Primary health care settings |
Effective factors in nurses’ use of mobile health applications were classified into eight themes including “ease of use”, “usefulness”, “security and confidentiality”, “feasibility and functionality”, “design and use – interface”, “effectiveness”, “infrastructure” and “social norms and versatility”, and 66 subthemes.
Discussion
By conducting the search strategy in the databases, 2063 articles were retrieved and after evaluation and exclusion of duplications and eliminating articles based on the exclusion criteria, 25 articles were finally considered for the study.
The results indicate that nurses use mobile health applications with the aim of learning and improving knowledge (Table 1). Nurses use these applications in order to access evidence-based scientific knowledge (Ferguson et al., 2019), support evidence-based decision-making (Jindal et al., 2018), enhance performance skills (Choi et al., 2018), train nursing students (Thoma-Lürken et al., 2019), and for problem-based methods of teaching (Johansson et al., 2013).
Other findings indicate that treatment and improvement of the patient care process is another one of the main reasons for nurses’ use of mobile health applications (Table 1). Nurses use these applications in order to monitor patients’ health status, reduce medical errors, increase patient safety while prescribing medication, follow-up on patients, observe the vital signs of patients, and plan for patient care (Supplemental Table 1).
The diagnostic process is another one of the main bases of using mobile health applications by nurses. Nurses use these applications in order to provide a better overview of possible solutions, assist the early diagnosis, provide a guideline/checklist for problem assessment, give advice on solutions, and to provide up-to-date information (Sobrinho et al., 2018; Thoma-Lürken et al., 2019).
Other findings show that one of the other uses of these applications is patient and data management (Table 1). Nurses use these programs to support their daily workflow, data entry, birth data tracking and analysis, documentation practices, for the hospital Electronic Health Record, to facilitate documentation at the bedside, for integrated management of chronic conditions, for longitudinal health data, to manage data for the care of mothers, patient information management, personalisation, to provide an easy input interface and various outputs for nursing records, and support documentation at the bedside by means of a user-centred approach (Supplemental Table 1) (Crowley et al., 2017; Choi et al., 2004, 2018; Ferguson et al., 2019; Lehto et al., 2018; Rothstein et al., 2016).
Health promotion is another one of the reasons for nurses’ use of mobile health applications (Table 1). They use these programs to track patients’ health indicators such as physical activity, diet and sleep and as a guided approach for promoting health and healing in primary health care settings (Holtz et al., 2019; Jindal et al., 2018; Lehto et al., 2018).
The second aim of the current research was to identify effective factors in using mobile health applications by nurses. Ease of use was identified as the first effective theme in nurses’ use of mobile health applications (Table 2). Factors such as perceived ease of use, facilitating conditions, perceived convenience, simplicity, and perceived patient barriers were classified as subthemes of “ease of use” as effective factors in nurses’ use of mobile health applications (Supplemental Table 1) (Choi et al., 2018; Day and Song, 2017; De La Vega et al., 2014; Ehrler et al., 2018b; Giraldo et al., 2018; Holtz et al., 2019; Lee and Kim, 2018; Lehto et al., 2018; Siebert et al., 2019; Sobrinho et al., 2018; Rothstein et al., 2016). Thus, “ease of use” is a very important factor and if mobile health applications did not have this factor, they were not worthy of attention by nurses.
Table 2.
Factors affecting the use of mHealth applications.
| Theme | Subtheme |
|---|---|
| 1. Ease of use | • Convenience |
| • Facilitating conditions | |
| • application’s ease of use | |
| • Perceived ease of use | |
| • Perceived patient barriers | |
| • Simplicity | |
| • Perceived stress | |
| 2. Usefulness | • Helpfulness |
| • Perceived benefits | |
| • Perceived usefulness | |
| • application’s usefulness | |
| 3. Security and confidentiality | • Confidentiality |
| • Privacy | |
| • Safety, security, and liability | |
| • Trustworthiness | |
| 4. Feasibility and functionality | • Credibility |
| • Easily portable | |
| • Easy to learn | |
| • Easy to understand | |
| • application’s feasibility | |
| • Practicability | |
| • Functionalities of the tool | |
| • Functionality of the app and input device | |
| • Suitability | |
| • Usability and suitability | |
| • Acceptability | |
| 5. Design and use-interface | • Customisation |
| • Design | |
| • Familiarity | |
| • Fun feature | |
| • Interaction design of the app | |
| • Lack of clarity of some icons | |
| • Layout | |
| • Conducive menu | |
| • Easy-to-use interface | |
| • Guided instruction | |
| • Having guided tour | |
| • Navigation | |
| • User interface, user satisfaction | |
| 6. Effectiveness | • Effectiveness |
| • Efficiency | |
| • Effort expectancy | |
| • Impact on the workflow | |
| • Increased confidence | |
| • Patient safety | |
| • Perceiving an increase of productivity | |
| • Performance efficiency | |
| • Performance | |
| • Productivity of work processes | |
| • Quality of care | |
| • Reduced my workload | |
| • Time savings, time | |
| • Workflow | |
| • Satisfaction | |
| 7. Infrastructure (content hardware/software) | • High quality |
| • Low-cost | |
| • Poor network connectivity | |
| • Quality of information | |
| • Supportive technology | |
| • Update content | |
| • Managerial support | |
| 8. Social norms and versatility | • Easily integrated into routine care |
| • Social influence dimension | |
| • Social norm | |
| • Versatility |
Other findings indicated that perceived usefulness, perceived benefits, and helpfulness, were factors that had a significant effect on nurses’ use of mobile health applications and were all classified under the subtheme of usefulness (Table 2) (Choi et al., 2004, 2018; Day and Song, 2017; Giraldo et al., 2018; Holtz et al., 2019; Johansson et al., 2013; Lehto et al., 2018; Spindler et al., 2018). Therefore, nurses will use an application that is useful for them, one that is not cumbersome and is compatible with their workflow.
The issue of security and confidentiality of mobile health applications is also a serious issue for nurses, and based on the literature, this issue had a significant effect on their use of these applications. Confidentiality, privacy, safety, security and liability, and trustworthiness are all among factors classified under security and confidentiality as mentioned in the literature (Supplemental Table 1) (Giraldo et al., 2018; Holtz et al., 2019; Lee and Kim, 2018; Sobrinho et al., 2018). Thus, it can be stated that security and confidentiality are one of the nurses’ concerns in using mobile health applications and should be considered in their design.
The feasibility and functionality of mobile health applications is also among effective factors in nurses’ use of these applications (Table 2). The literature has referred to issues such as easy to learn, easily portable, credibility, functionalities of the tool, practicability, feasibility, easy to understand, usability and suitability, functionality of the app and input device, and acceptability (Ankem et al., 2019; Choi et al., 2004; Ehrler et al., 2018b; Ferguson et al., 2019; Giraldo et al., 2018; Grossi et al., 2014; Jindal et al., 2018; Lee and Kim, 2018; Lehto et al., 2018; Motulsky et al., 2017; Rothstein et al., 2016; Sobrinho et al., 2018; Vossebeld et al., 2019; Yeh, 2016). Therefore, feasibility and functionality are among crucial factors and if the application does not have these features, it will not be successful.
Factors such as familiarity, fun feature customisation, interaction design of the app, lack of clarity of some icons, layout, conducive menu, easy-to-use interface, guided instruction, having a guided tour, navigation, and user interface and user satisfaction are also mentioned in the literature as factors that nurses consider when working with mobile health applications, (Ankem et al., 2019; Choi et al., 2004, 2018; De La Vega et al., 2014; Ehrler et al., 2018a; Jindal et al., 2018; Lee and Kim, 2018; Lehto et al., 2018; Praveen et al., 2014; Thoma-Lürken et al., 2019) which we classified in the design and use—interface group. Thus, it can be stated that an appropriate and alluring design and an easy-to-use interface are one of the effective factors in nurses’ selection of mobile health applications.
Other findings indicated that effectiveness is also one the effective factors in nurses’ use of mobile health applications (Table 2). The evaluated studies indicated that factors such as efficiency, effectiveness, patient safety, effort expectancy, impact on workflow, increased confidence, increased productivity, performance efficiency, productivity of the work processes, quality of care, reduction in workload, time savings, time workflow, and satisfaction were greatly considered by nurses when using mobile health applications and are all classified in the group “effectiveness” (Choi et al., 2004; Ehrler et al., 2018b; Giraldo et al., 2018; Johansson et al., 2013; Motulsky et al., 2017; Thoma-Lürken et al., 2019; Vossebeld et al., 2019; Yeh, 2016). Thus, mobile health applications are rendered successful if they are effective for nurses.
Infrastructure (hardware/software content) is the next effective factor in nurses’ use of mobile health applications. The studies indicate that factors such as poor network, low-cost, high quality, managerial support, up-to-date content, supportive technology, quality of information, and connectivity are effective in the use of mobile health applications from the nurses’ viewpoint (Day and Song, 2017; Ferguson et al., 2019; Motulsky et al., 2017; Thoma-Lürken et al., 2019; Vossebeld et al., 2019). Thus, the existence of appropriate hardware and software infrastructures is necessary for the acceptability and popularity of an application.
The final items considered were social norms and versatility. With analyses and evaluation carried out in the literature, social norms, social influence dimension, being easily integrated into routine care, and versatility were classified in this group (Day and Song, 2017; De La Vega et al., 2014; Ehrler et al., 2018b; Rothstein et al., 2016). That is, when working with mobile health applications, nurses consider social norms and their versatility in society and select the mobile health applications based on these social norms.
Overall, it can be stated that mobile health applications are effective tools for nurses in learning and enhancement of knowledge, diagnosis and treatment of disease, and improving patients’ quality of care. Effective factors in nurses’ use of these applications include a wide range of factors including usefulness and ease of use, functionality, effectiveness and compatibility and social versatility. Policy makers, planners, and designers of mobile health applications should consider the factors obtained in these review studies when designing applications with great accuracy. As it was previously mentioned, these applications, especially in the cloud computing platform (Asadi et al., 2020), have considerable potential in education, the professional excellence of nurses, and improving quality of care for patients.
Conclusion
The concept of mobile health has attracted considerable attention across the globe, as it provides both healthcare professionals and patients with a distinct means of information and resources. As a result, it is deemed to be a promising tool for the support and advancement of healthcare. The findings from this scoping review provide a well-established understanding of the effective factors in nurses’ use of mobile health applications, unravelling the challenges and opportunities associated with mHealth utilisation by nurses. mHealth applications are effective tools for nurses in the fields of learning and knowledge enhancement, diagnosis and treatment of disease, and improving the patient care process. Effective factors in nurses’ behaviour when using these applications encompass a wide range such as usefulness and ease of use, feasibility and functionality, effectiveness, versatility and social norms. Regardless of the barriers and facilitators for mHealth adoption as a source of information communication technology, this study has enabled us to identify effective factors that should be taken into consideration in the nursing profession.
Key points for policy, practice and/or research
Mobile health applications are promising tools for the support and advancement of healthcare.
We provided a well-established understanding of the effective factors in nurses’ use of Mobile Apps.
We addressed the challenges and opportunities associated with mHealth utilisation by nurses.
Ease of use and usefulness are the main factors affecting nurses’ intention to adopt Mobile Apps.
Security and confidentiality should be considered in mobile health application designs.
Social norms and versatility are determinant factors that affect adopting mobile applications.
Supplemental Material
Supplemental Material, sj-pdf-1-jrn-10.1177_17449871221077080 for Adopting mobile health applications by nurses: a scoping review by Soghra nezamdoust, Mohammadhiwa Abdekhoda, Fatemeh Ranjbaran, and Saber Azami-Aghdash in Journal of Research in Nursing
Biography
Soghra Nezamdoust MSc, Student of Medical Library and Information Sciences, School of Health Management and Medical Informatics, Tabriz University of Medical Sciences, Tabriz, Iran. She received her bachelor degree in Medical Librarianship. Her research interests include: health information technology, nursing informatics and health information management.
Mohammadhiwa Abdekhoda, PhD, Associate Professor in Health Information Management. Department of Medical Library and Information Sciences. School of Health Management and Medical Informatics. Tabriz University of Medical Sciences. Tabriz, Iran. He received a PhD degree in Health Information Sciences from Iran University of Medical Sciences. Also, he received his MSc degree in Medical Library and Information Sciences from Tehran University of Medical Sciences. His research interests include: health information systems, information systems adoption, scientometric, medical library and information sciences.
Fatemeh Ranjbaran, PhD in Forging Language, Department English Language Center, University of Technology and Applied Sciences, Nizwa, Oman. She received her MSc and bachelor degree in Forging Language. Her research interest include: health information technology, and nursing informatics.
Saber Azami-Aghdash, PhD, Assistance Professor in Health Policy. Department of Health Services Management. School of Health Management and Medical Informatics. Tabriz University of Medical Sciences. Tabriz, Iran. His research interests include: health services management.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: Different ethical aspects of the present research were approved by the Ethics Council of Tabriz University of Medical Sciences (IR.TBZMED.REC.1397. 1058).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article: This study was funded by Tabriz University of Medical Sciences (Grant Number: 62124).
Supplemental material: Supplemental material for this article is available online.
ORCID iD
Mohammadhiwa Abdekhoda https://orcid.org/0000-0002-1797-8916
References
- Ankem K, Cho S, Simpson D. (2019) Nurses’ perceptions and problems in the usability of a medication safety app. Informatics for Health and Social Care 44: 48–69. [DOI] [PubMed] [Google Scholar]
- Asadi Z, Abdekhoda M, Nadrian H. (2020) Cloud computing services adoption among higher education faculties: development of a standardized questionnaire. Education and Information Technologies 25: 175–191. [Google Scholar]
- Choi J, Chun J, Lee K, et al. (2004) MobileNurse: hand-held information system for point of nursing care. Computer Methods and Programs in Biomedicine 74: 245–254. [DOI] [PubMed] [Google Scholar]
- Choi M, Lee H, Park JH. (2018) Effects of using mobile device-based academic electronic medical records for clinical practicum by undergraduate nursing students: a quasi-experimental study. Nurse Education Today 61: 112–119. [DOI] [PubMed] [Google Scholar]
- Crowley RA, Dumas HM, Fragala-Pinkham MA, et al. (2017) Child to nurse communication in paediatric post-acute hospital care: evaluation of the VerbalCare tablet application. Disability and Rehabilitation: Assistive Technology 12: 462–468. [DOI] [PubMed] [Google Scholar]
- Day KJ, Song N. (2017) Attitudes and concerns of doctors and nurses about using a translation application for in-hospital brief interactions with Korean patients. Journal of Innovation in Health Informatics 24: 916. [DOI] [PubMed] [Google Scholar]
- De La Vega R, Roset R, Castarlenas E, et al. (2014) Development and testing of painometer: a smartphone app to assess pain intensity. The Journal of Pain 15: 1001–1007. [DOI] [PubMed] [Google Scholar]
- DeGusta M. (2012) Are Smart Phones Spreading Faster than Any Technology in Human History. United States Massachusetts Institute of Technology Review. [Google Scholar]
- Ehrler F, Ducloux P, Wu DTY, et al. (2018. a) Acceptance of a mobile application supporting nurses workflow at patient bedside: results from a pilot study. Studies in Health Technology and Informatics 247: 506–510. [PubMed] [Google Scholar]
- Ehrler F, Weinhold T, Joe J, et al. (2018. b) A mobile App (BEDSide Mobility) to support nurses’ tasks at the patient’s bedside: usability study. JMIR mHealth and uHealth 6: e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson C, Hickman LD, Phillips J, et al. (2019) An mHealth intervention to improve nurses’ atrial fibrillation and anticoagulation knowledge and practice: the EVICOAG study. European Journal of Cardiovascular Nursing 18: 7–15. [DOI] [PubMed] [Google Scholar]
- Giraldo L, Schachner B, Luna D, et al. (2018) Exploring nurses’ perceptions and expectations toward a BCMA implementation using a mobile app and workstations as a change management strategy. Studies in Health Technology and Informatics, 250: 134–138. [PubMed] [Google Scholar]
- Grossi LM, Pisa IT, Marin HdF. (2014) Oncoaudit: desenvolvimento e avaliação de aplicativo para enfermeiros auditores. Acta Paulista De Enfermagem 27: 179–185. [Google Scholar]
- Haffey F, Brady RRW, Maxwell S. (2013) A comparison of the reliability of smartphone apps for opioid conversion. Drug Safety 36: 111–117. [DOI] [PubMed] [Google Scholar]
- Hagbaghery MA, Salsali M, Ahmadi F. (2004) A qualitative study of Iranian nurses’ understanding and experiences of professional power. Human Resources for Health 2: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtz B, Vasold K, Cotten S, et al. (2019) Health care provider perceptions of consumer-grade devices and apps for tracking health: a pilot study. JMIR mHealth and uHealth 7: e9929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jindal D, Gupta P, Jha D, et al. (2018) Development of mWellcare: an mHealth intervention for integrated management of hypertension and diabetes in low-resource settings. Global Health Action 11: 1517930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson PE, Petersson GI, Nilsson GC. (2013) Nursing students’ experience of using a personal digital assistant (PDA) in clinical practice - an intervention study. Nurse Education Today 33: 1246–1251. [DOI] [PubMed] [Google Scholar]
- Johnston MJ, King D, Arora S, et al. (2015) Smartphones let surgeons know WhatsApp: an analysis of communication in emergency surgical teams. The American Journal of Surgery 209: 45–51. [DOI] [PubMed] [Google Scholar]
- Lee J, Kim J. (2018) Method of app selection for healthcare providers based on consumer needs. CIN: Computers, Informatics, Nursing 36: 45–54. [DOI] [PubMed] [Google Scholar]
- Lehto R, Heeter C, Allbritton M, et al. (2018) Hospice and palliative care provider experiences with meditation using mobile applications. Oncology Nursing Forum 45: 380–388. [DOI] [PubMed] [Google Scholar]
- Marcum J, Ridenour M, Shaff G, et al. (2002) A study of professional nurses’ perceptions of patient education. The Journal of Continuing Education in Nursing 33: 112–118. [DOI] [PubMed] [Google Scholar]
- Martínez-Pérez B, De La Torre-Díez I, López-Coronado M. (2015) Privacy and security in mobile health apps: a review and recommendations. Journal of Medical Systems 39: 181. [DOI] [PubMed] [Google Scholar]
- Mobasheri MH, Johnston M, King D, et al. (2014) Smartphone breast applications - What’s the evidence? The Breast: Official Journal of the European Society of Mastology 23: 683–689. [DOI] [PubMed] [Google Scholar]
- Mobasheri MH, King D, Johnston M, et al. (2015) The ownership and clinical use of smartphones by doctors and nurses in the UK: a multicentre survey study. BMJ Innovations 1: 174–181. [Google Scholar]
- Motulsky A, Wong J, Cordeau J-P, et al. (2017) Using mobile devices for inpatient rounding and handoffs: an innovative application developed and rapidly adopted by clinicians in a pediatric hospital. Journal of the American Medical Informatics Association 24: e69–e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozdalga E, Ozdalga A, Ahuja N. (2012) The smartphone in medicine: a review of current and potential use among physicians and students. Journal of Medical Internet Research 14: e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Praveen D, Patel A, Raghu A, et al. (2014) SMARTHealth India: development and field evaluation of a mobile clinical decision support system for cardiovascular diseases in rural India. JMIR mHealth and uHealth 2: e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahimi A, Ahmadian Majin N. (2017) Investigating health literacy level and relation to demographic factors of nurses in teaching hospitals of at west cities of Iran: 2016. Journal of Health Literacy 2: 54–61. [Google Scholar]
- Rothstein JD, Jennings L, Moorthy A, et al. (2016) Qualitative assessment of the feasibility, usability, and acceptability of a mobile client data app for community-based maternal, neonatal, and child care in rural Ghana. International Journal of Telemedicine and Applications, 2016: 2515420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siebert JN, Ehrler F, Combescure C, et al. (2019) A mobile device application to reduce medication errors and time to drug delivery during simulated paediatric cardiopulmonary resuscitation: a multicentre, randomised, controlled, crossover trial. Lancet Child Adolesc Health 3: 303–311. [DOI] [PubMed] [Google Scholar]
- Sobrinho A, da Silva LD, Perkusich A, et al. (2018) Design and evaluation of a mobile application to assist the self-monitoring of the chronic kidney disease in developing countries. BMC Medical Informatics and Decision Making 18: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spindler H, Dyer J, Bagchi K, et al. (2018) Tracking and debriefing birth data at scale: a mobile phone application to improve obstetric and neonatal care in Bihar, India. Nursing Open 5: 267–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan EJ, Decker PJ. (1998) Effective leadership and management in nursing. American Journal of Nursing 98: 16L. [Google Scholar]
- Thoma-Lürken T, Lexis MAS, Bleijlevens MHC, et al. (2019) Perceived added value of a decision support App for formal caregivers in community-based dementia care. Journal of Clinical Nursing 28: 173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, et al. (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine 169: 467–473. [DOI] [PubMed] [Google Scholar]
- Vossebeld DM, Puik ECN, Jaspers JEN, et al. (2019) Development process of a mobile electronic medical record for nurses: a single case study. BMC Medical Informatics and Decision Making 19: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittaker R. (2012) Issues in mHealth: findings from key informant interviews. Journal of Medical Internet Research 14: e129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf JA, Moreau JF, Akilov O, et al. (2013) Diagnostic inaccuracy of smartphone applications for melanoma detection. JAMA Dermatology 149: 422–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh KH. (2016) BSNCare Plus : A Robust IoT-Oriented Healthcare System with Non-repudiation Transactions. Applied Sciences-Basel, 6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-jrn-10.1177_17449871221077080 for Adopting mobile health applications by nurses: a scoping review by Soghra nezamdoust, Mohammadhiwa Abdekhoda, Fatemeh Ranjbaran, and Saber Azami-Aghdash in Journal of Research in Nursing