Abstract
Objectives
The purpose of this paper is to describe a university program, Spartan Caregiver Support, that provided free on-demand telehealth services to caregivers of people with autism during the State of Michigan’s 2020 Stay-at-Home order.
Method
Participants (n = 17) were caregivers of people with autism residing within the State of Michigan. Participants engaged with program members over video-conference technology, where participants received specific advice to support social and behavioral needs.
Results
We found that caregivers reported a variety of social and behavioral concerns, including concerns related to problem behavior, social/play skills, school/academics, and daily living.
Conclusions
This program description provides a framework for how to deliver on-demand telehealth support to caregivers of people with autism, especially during moments of crisis or emergency.
Supplementary Information
The online version contains supplementary material available at 10.1007/s41252-022-00281-7.
Keywords: Autism, Caregiver, COVID-19, Telehealth, Technology, Qualitative research
In response to the outbreak of COVID-19, Michigan Governor Gretchen Witmer signed the “Stay Home, Stay Safe” Executive Order (stay-at-home order) on March 23, 2020 until June 1, 2020, directing residents in the State of Michigan to stay in their homes unless they were an essential worker, engaged in outdoor activity (e.g., jogging), or were performing tasks that were essential to sustain life (e.g., going to the grocery store) (State of Michigan, 2020). The stay-at-home order also resulted in the closure of Michigan schools (Manning et al., 2020), leading to the immediate loss of access to the primary sources of behavioral services for individuals with autism (Boyd et al., 2018; Kasari & Smith, 2013; Stenhoff et al., 2020). While the State of Michigan did deem some private behavioral services essential, a majority of service providers complied with the stay-at-home order and suspended in-person services in an effort to slow the spread of COVID-19 (Cox et al., 2020; Manning et al., 2020).
The closure of schools and in-person autism services resulted in massive disruptions of daily life for many individuals with autism and their families (Cahapay, 2022; Di Renzo et al., 2020; Garcia et al., 2020; Manning et al., 2020). Huge life disruptions for people with autism and their caregivers, such as the sudden loss of behavioral services, have the potential to increase challenging behaviors, disrupt sleep and routines, and decrease social skills and language development (degli Espinosa et al., 2020; Di Renzo et al., 2020; Garcia et al., 2020; Stenhoff et al., 2020). Furthermore, temporary suspension of services for individuals with autism who require intensive behavioral support may place the individual or others at risk of serious harm such as self-injury or hurting family members (Cox et al., 2020).
Individuals with autism were greatly impacted by the stay-at-home orders during the COVID-19 pandemic (Garcia et al., 2020). For example, children with autism showed an increase in repetitive behaviors, a worsening in sleep regulation, and an increase in agitation (Di Renzo et al., 2020). In addition, adolescents with autism engaged in a fewer number of days with physical activity and increased their amount of screen time (Garcia et al., 2020). Further, current research examining the impact of COVID-19 on children’s mental health status reveals that children as young as 3-years-old who experienced quarantine are more likely to experience anxiety and depression (Loades et al., 2020).
Family members of individuals with autism reported that the COVID-19 crisis resulted in high levels of stress and disruption to daily living (degli Espinosa et al., 2020; Manning et al., 2020). Families reported that the greatest areas of stress included isolation, illness, and financial struggles. Moreover, the severity of autism symptoms seemed to impact family stressors: families of individuals with autism who displayed more severe autism-like symptoms (e.g., higher engagement in problem behavior and less communication skills) correlated to a higher degree of familial stress (Manning et al., 2020). The increase in level of stress for families of individuals with autism is concerning because parental stress and functioning is closely related to child outcomes (Russell et al., 2020; Russell et al., 2021).
Given the increase in behavioral concerns for individuals with autism and the stress and toll this would take on caregivers, many disciplines “pivoted” to providing support through technology (Stenhoff et al., 2020). Telehealth then became an essential modality in which caregivers of individuals with autism could receive the help they need to support them during disruptions to healthcare services (Stark et al., 2020; Wagner et al., 2020). Professionals providing behavioral services were no exception, rapidly adopting telehealth to help support caregivers and individuals with autism affected by the COVID-19 pandemic (Wagner et al., 2020).
The adoption of telehealth technology was not without merit. In fact, a recent review of telehealth research found caregiver implementation of evidence-based supports resulted in positive improvements for 100% of child participants (Unholz-Bowden et al., 2020). In addition, telehealth has been found to be socially acceptable (Bice-Urbach & Kratochwill, 2016; Fischer et al., 2017; Neely et al., 2019; Tomlinson et al., 2018). Of note, Lindgren et al. (2016) reported that caregivers of children with autism found telehealth training of behavioral-based interventions as acceptable as in-person training. Additionally, training through telehealth was more cost effective than in-person training (Lindgren et al., 2016).
Even though Michigan’s stay-at-home order required most educational and medical providers of autism services to switch to providing services via telehealth (Manning et al., 2020), access to telehealth was not widely available for all Michigan families. Many educational providers (e.g., teachers) may not have been well equipped with the technological resources to provide telehealth services. Even then, providing support to caregivers of children receiving special education services (e.g., under IDEA) likely does not entail caregiver training. That is, educational providers that did have access to technological resources likely did not provide caregiver training to the families of individuals with autism because caregiver training is not required by law. For individuals with autism receiving services in the form of “medically necessary” autism treatment, such as in in-patient or in-home autism services, access to telehealth services (e.g., caregiver training) during the stay-at-home order was only available to families who had been receiving services prior to the COVID-19 pandemic. Put another way, behavioral services via telehealth were likely not available to families on waitlists to receive in-home or in-patient services, or who were not actively pursuing telehealth services prior to the pandemic. In addition to the inaccessibility of telehealth services, access to autism services and qualified providers in Michigan, in general, were extremely limited to begin with (see Drahota et al., 2020 and Yingling et al., 2021).
In this article, we describe the program we developed and deployed, Spartan Caregiver Support (SCS), that leveraged technology to provide telehealth services to caregivers of individuals with autism during the State of Michigan’s stay-at-home order. This program description documents our efforts taken during the COVID-19 pandemic to make caregiver support more accessible to all families and offers a framework for future responses to local, state, federal, and global emergencies. We also describe the primary concerns reported by caregivers of individuals with autism in the State of Michigan during Michigan’s stay-at-home order. Finally, we provide implications for future research.
Method
Participants
Figure 1 depicts how SCS recruited and retained caregivers to participate in its program. First, caregivers were directed to a Web site (https://mtb.msu.domains/spartan-caregiver-support/) through Facebook posts (see Supplementary Materials Figure S1) or e-mail distributions where they could learn about SCS and sign up for a listserv. The Web-based program, WordPress, was used to create the SCS Web site, which was hosted by Michigan State University. The Web-based service, ConstantContact, was used to host and manage the listserv (see Supplementary Materials Figure S2 for a sample Listserv e-mail). Every Thursday at 8 pm EST, caregivers subscribed to the listserv would receive an e-mail with instructions on how to sign up for a free 15-min meeting with a team member the following week. It is important to note that while SCS marketed 15-min meetings, most meetings lasted longer than 15 min. Each e-mail also included a “Caregiver Resource of the Week” which featured curated resources that were directly aimed to support families during COVID-19. Examples of curated resources included the following: how to establish routines in the home; strategies for wearing masks in public; and tips and tricks for toilet training.
Fig. 1.
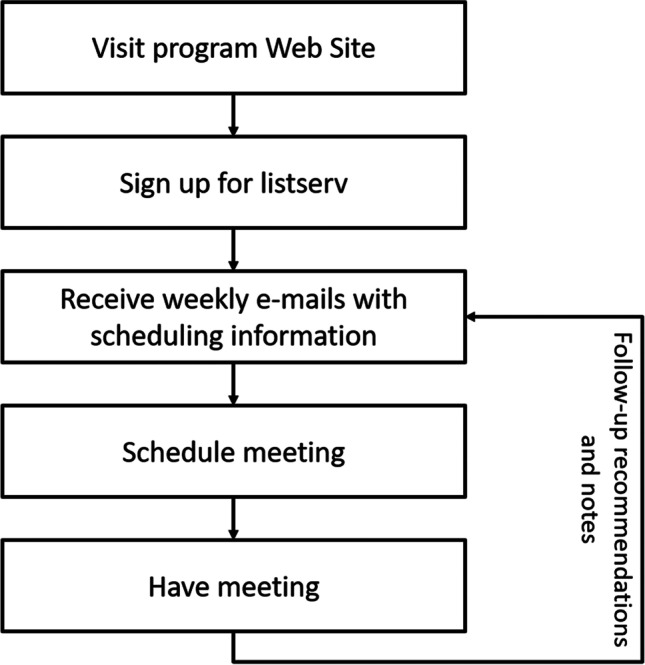
Recruitment and engagement process for caregivers who received services from spartan caregiver support
Participants (n = 17) consisted of caregivers of individuals with autism that lived in the State of Michigan. Recruitment was limited to Michigan to understand the effects of the strict stay-at-home order, and because the authors’ institutional IRB prohibited research involving participants outside the State of Michigan. Because we reported that participants resided in Michigan, additional participant characteristics (e.g., gender, age of child with autism, socio-economic status) will not be reported in order to protect confidentiality. Participants must have lived in the State of Michigan, been a caregiver of an individual with autism, and been 18 years old or older.
Procedures
Spartan Caregiver Support Program Description
Spartan Caregiver Support is a free support service for caregivers of individuals with autism and began providing services to caregivers in the State of Michigan in early April 2020.The mission of SCS was as follows: to provide quality behavioral and social support that meets the needs of caregivers of people with autism within the State of Michigan in a cost-effective way. Through SCS, we assisted caregivers by addressing social or behavioral challenges exhibited by their dependent with autism through video-chat technology. For example, we addressed concerns related to challenging behavior, communication difficulties, rule following, and fostering relationships. Specific examples of the types of supports SCS provided, and did not provide, are depicted in Table 1. Further, to fulfill the SCS’s mission to provide supports in a cost-effective way, SCS offered its services free of charge. To provide services free of charge, the SCS team volunteered any of their extra free-time (e.g., time previously devoted to in-person activities) to the program.
Table 1.
A comprehensive list of supports that could be and could not be provided by spartan caregiver support
| Supports program could provide | Supports program could not provide |
|---|---|
| Behavioral concerns, such as tantrums and meltdowns | Respite care, on-site consultation, or medical, academic (we do not provide online academic instruction), and diagnostic support |
| Communication difficulties, such as difficulty expressing wants and needs | Caregivers who reside outside the State of Michigan |
| Daily schedules and routines, such as completing a list of chores and brushing one’s teeth | Any areas other than what is listed as a support we can provide |
| Sleep concerns, if those concerns have a behavioral (and not medical) cause | |
| Getting along with family members, such as siblings and cousins | |
| Following rules and expectations, such as following a caregiver’s instructions | |
| Toileting concerns, such as learning to void on the toilet |
SCS was situated within Michigan State University’s College of Education’s Special Education Program. The SCS team consisted of the Program Director (a faculty member within the tenure stream system), as well as MA and PhD students. All team members had extensive experience providing behavior analytic supports to individuals with autism in community-based settings as well as supporting families with behavioral challenges. All team members were mandated reporters and had undergone trainings concerning mandated reporting.
All team members underwent initial training by either the Program Director or an advanced team member. Each team member was observed using a program-generated fidelity checklist (see Supplementary Materials). After the team member was observed, they were provided with descriptive feedback based on their performance. Team members were allowed to independently conduct meetings once they demonstrated that they could complete every step on the fidelity checklist on their own.
After a caregiver signed up for a meeting, that caregiver was assigned to a team member. Once a meeting was scheduled, the team sent an email with a Zoom link to meet with their assigned team member along with an IRB fact sheet. The meeting was then subsequently held via video-chat (i.e., Zoom) while caregivers and researchers were in their respective homes. To ensure caregiver privacy, we used the “waiting room” feature on Zoom so that only caregivers scheduled at that specific time would be able to join the video-chat. All SCS team members were familiar with the technology used during service provision.
To start the initial meeting, the team member began by confirming the caregiver’s name, email address, and phone number to ensure confidentiality. In addition, the team member began to build rapport by saying statements or asking questions such as, “thank you for calling in today,” and “how is your day going.” Next, the caregiver was provided with a brief description of the team member (e.g., “Hello, my name is [name], and I am a doctoral student at [university]”), the objectives of SCS (e.g., SCS was created to support families of individuals with autism), and was read a series of disclaimers (e.g., team members are mandated reporters). Upon agreeing to the disclaimers (e.g., “Do you acknowledge that I am a mandated reporter?”), the team member began to inquire about the individual with autism (e.g., tell me about [your child with autism]). As the caregiver described their dependent, the team member typed notes into the survey program Qualtrics (Qualtrics, Provo, UT, 2019). Throughout the conversation, the team member prompted additional information by asking questions regarding the behavioral challenges or concerns experienced by the person with autism and their family. Specifically, caregivers were asked questions such as, “what concerns do you have about your child,” and “how can I help you and your family?”.
The team member responded to reported behavioral challenges by providing specific advice for how to respond to the behavior. For example, team members provided support in managing behavioral instances (e.g., minimize attention during tantrums; keep hair up to avoid hair pulls), suggested environmental arrangements and supports (e.g., incorporating a visual schedule; maintaining daily routines; minimize distractions during online instruction), and provided recommendations for specific behavioral interventions (e.g., functional communication training; toilet training; discrete trail training). It is important to note that the context in which the beforementioned activities occurred was incredibly unique, given the stay-at-home order. Caregivers were juggling multiple responsibilities (e.g., working from home while providing childcare), and most of the behavioral services that were once available prior to the pandemic were on-hold. Though we were unable to train caregivers to implement the beforementioned interventions at high levels of fidelity (or even measure fidelity of implementation), we believed it was ethically justifiable to provide recommendations in light of those limitations, given the dearth of services and support that were available during the stay-at-home order, as well as the challenges caregivers were experiencing. Further, often the team did not expect that caregivers could implement, for example, functional communication training, with high fidelity. Instead, the team explained to caregivers how to implement specific aspects of behavioral interventions (e.g., trained caregivers in how to prompt their dependent to exchange a picture card to access a preferred item). In addition, team members provided training on how caregivers could incorporate recommendations into their home and emailed materials that would assist caregivers in implementing recommendations. For example, team members trained caregivers on how to implement a visual schedule across an entire day and send sample visual schedules and photos to assist caregivers in creating their own visual schedule. Further, during each meeting, the team member ensured their advice and support for the caregiver fit within their own scope of competence as a consultant (see Brodhead et al., 2018).
At the end of the initial meeting, the team member asked the caregiver if they would like to schedule a follow-up meeting. Then, an e-mail that provided a clear and concise summary of the SCS’s recommendations was sent to the caregiver no later than 24 h after the meeting concluded. If the caregiver requested a follow-up meeting, the follow-up meeting information was also included in the email (see Figure S3 in Supplementary Materials for a sample of a follow up e-mail). This e-mail was constructed by the graduate student who conducted the meeting and sent to the Program Director for revision (if required) and approval, prior to the e-mail being sent to the caregiver. This process ensured the Program Director maintained oversight of all outward communication/recommendations to caregivers and also provided an opportunity for providing feedback and coaching to team members.
Any requested follow-up meetings were similar to the initial meetings, beginning with the team member reading the same series of disclaimers. Follow-up meetings often began with the team member asking questions such as, “how was your week,” or “do you have any updates you would like to share?” Follow-up meetings then followed the same format as initial meetings—team members asked questions regarding any behavioral challenges and provided support where needed.
Data Analyses
Our analysis is rooted in phenomenography. Phenomenography is an empirically based methodology that seeks to understand by analyzing descriptions of participant experiences (Bazeley, 2013). For the current study, we recorded exploratory case study field notes (i.e., meeting notes) (Bazeley, 2013). Our analysis involved scheduling planned interviews (i.e., caregiver meetings) and recording caregiver reported behavioral problems.
First Cycle Coding
Our analytic process involved pencil-and-paper descriptive coding (Bazeley, 2013; Saldaña, 2016). To begin, we read through all meeting notes and created a list of initial data codes that described our data. Our initial codes included: problem behavior, schedule/routine, social/play skills, communication, daily living, school/academics, toileting, eating, sleep, and current issues. We then read through all meeting notes a second time and indexed (Bazeley, 2013) the data in order to assign codes to each meeting note. To do this, we first created an index card for each code. We then read the notes from each caregiver meeting and recorded their caregiver meeting identification (e.g., 016) to respective codes. For example, in meeting 1 with caregiver 016, we recorded problems with “hitting, scratching, and punching [parent] and [sibling],” and “problem expressing wants and needs.” These behavior problems were coded as “problem behavior” and “communication” respectively. In order to record these codes, we wrote 016 on the “problem behavior” and “communication” index cards. We continued this process for all 17 clients.
Second Cycle Coding
After conducting first cycle coding, we engaged in focused coding (Saldaña, 2016) in order to reanalyze the data collected though our descriptive coding. During the focused coding process, we again read through all meeting notes and assigned codes to our data. Through the focused coding process, we finalized our list of 12 codes (see Table 2 for a code list). We kept the 10 codes identified from first cycle coding and added the codes “technology” and “mental health” to our final list of codes based on our focused coding.
Table 2.
Coding categories of reported problems, examples of reported problems, and coding categories of reported problems organized into themes
| Code | Examples | Themes | ||
|---|---|---|---|---|
| Decreasing inappropriate behavior | Acquiring new skills | Maintaining current levels of performance | ||
| Problem behavior | Aggression; disruption; self-injury; inappropriate language; elopement | X | ||
| Social/play skills | No socialization with peers; virtual etiquette; internet safety; inappropriate play with toys; creating sibling relationships | X | X | |
| School/academics | Resistance/avoids work; lack of focus; how to teach at home | X | X | X |
| Daily living | How to teach toothbrushing; refusal to leave home; lack of personal hygiene; clothing selectivity | X | ||
| Schedule/routine | How to create a home routine; routine rigidity | X | X | |
| Technology | Asks for iPad all day; how to decrease screen time | X | ||
| Eating | Food refusal; food selectivity | X | X | |
| Toileting | Not toilet trained; increase in accidents | X | ||
| Sleep | Will not fall asleep; wakes up in the middle of the night | X | ||
| Communication | Cannot express wants and needs | X | ||
| Current issues | How to explain COVID-19; how to explain the Black Lives Matter protests | X | ||
| Mental health | Anxiety | X | ||
Post-Coding
In order to conclude our analysis, we engaged in the trinity focusing strategy (Saldaña, 2016). Through the trinity strategy, we identified three main themes: caregivers of individuals with autism needed support: (1) decreasing inappropriate behavior, (2) acquiring new skills, and (3) maintaining current levels of performance. We then organized our 12 codes into the three main themes (Table 2).
As a measure of social validity (Schwartz & Baer, 1991), we also collected data on the ongoing participation in SCS follow-up meetings. During the 8-week period, 13 of the 17 participants attended at least one follow-up meeting (range, 0–6 follow-up meetings).
Results
Figure 2 displays the number of caregivers who subscribed to the listserv (top panel) and the cumulative number of caregiver meetings (bottom panel) held over the course of the stay-at-home order. Over an 8-week period, the program received 74 individual caregiver subscriptions to the listserv and held 48 meetings with 17 caregivers via Zoom.
Fig. 2.
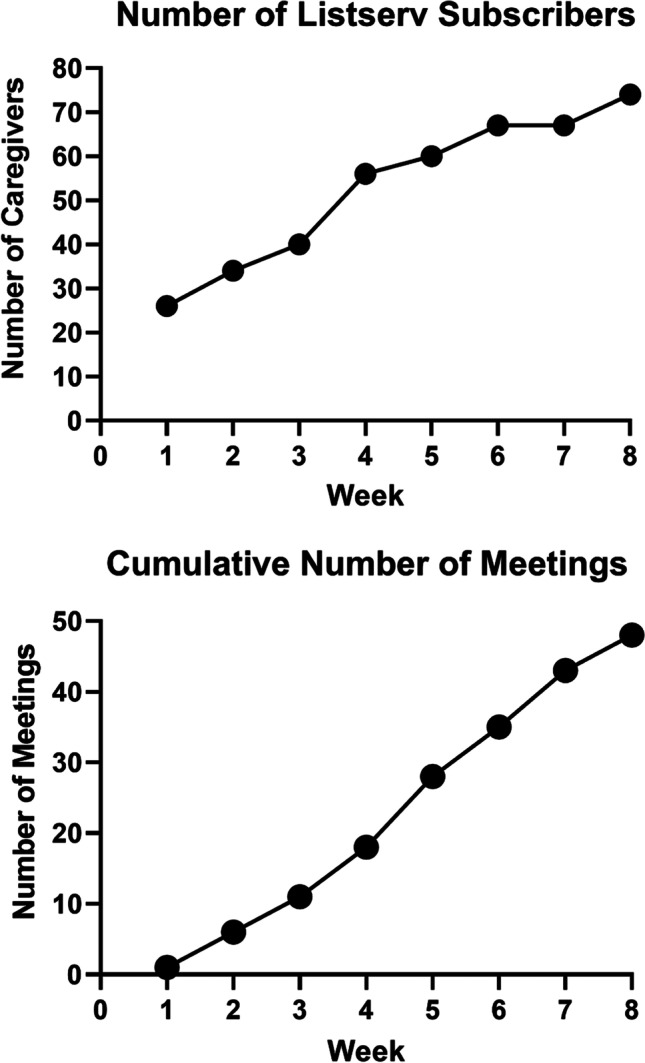
Number of program listserv subscribers and cumulative number of meetings held during the stay-at-home order
Challenges reported by caregivers are displayed in Fig. 3. Ninety-four percent (n = 16) of caregivers reported that their dependent engaging in problem behavior was an issue at home during the stay-at-home order, and all 16 of these caregivers requested assistance decreasing their dependent’s problem behavior. Commonly reported problem behaviors by caregivers included aggression, property disruption, elopement, self-injury, and inappropriate language.
Fig. 3.
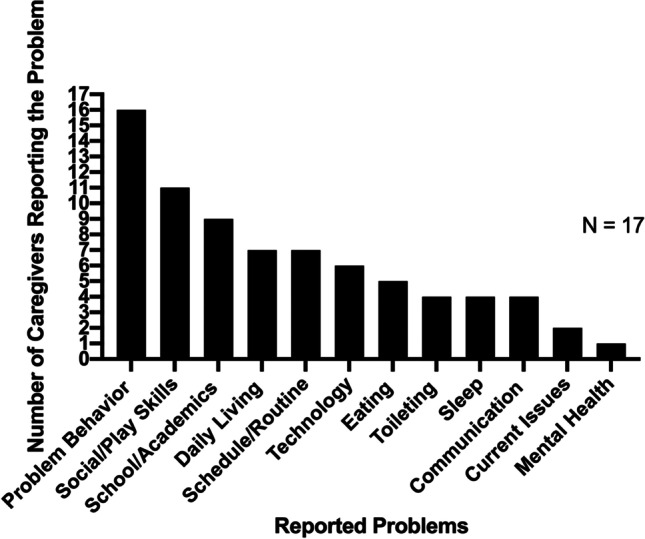
Number of caregiver reported problems during stay-at-home order
Sixty-five percent (n = 11) of the caregivers reported that their dependents’ lack of appropriate social and play skills was an issue at home during Michigan’s stay-at-home order. For example, participant 011 reported that their child struggled with sharing toys at home with their siblings, and participant 005 reported that their child struggled to appropriately play with their friends at the pool. Additionally, some caregivers expressed concerns maintaining the social skills that were targeted while at school (e.g., having conversations with same-aged peers).
Fifty-three percent (n = 9) of the caregivers reported that facilitating and maintaining school and/or academics in the home was an issue during the stay-at-home order. Caregivers frequently reported that their child often resisted work, remained off task while attending online instruction, and many caregivers requested assistance setting up an academic environment for their child.
Forty-one percent (n = 7) of the caregivers reported that teaching and/or maintaining daily living was an issue at home during Michigan’s stay-at-home order. For example, participant 019 reported that they needed help teaching their child to complete chores and to maintain personal hygiene skills (e.g., remembering to wear deodorant). Additionally, forty-one percent (n = 7) of the caregivers reported that facilitating or teaching their dependent to follow a schedule and/or routines was an issue at home during the stay-at-home order. For example, participant 004 reported that their child struggled to follow through with tasks and reported that their child was very rigid with their routines.
Thirty-five percent (n = 6) of the caregivers reported that decreasing the amount of time on technology was an issue at home during Michigan’s stay-at-home order. All six of these caregivers reported that their child used technology (e.g., iPad) for long periods of time during the day. For example, participant 003 reported that their child asked for an iPad throughout the day and asked for suggestion on how to decrease their child’s amount of screen time.
Twenty-nine percent (n = 5) of the caregivers reported that their dependent’s eating habits were an issue at home during Michigan’s stay-at-home order. Caregivers reported limited food preferences, overeating, and resistance to solid foods. For example, participant 010 reported that their child only wanted to eat pizza and [fast food restaurant] for lunch and dinner and often refused other food items during mealtimes.
Twenty-four percent (n = 4) of the caregivers reported that toileting (e.g., increased accidents) or toilet training was an issue at home during Michigan’s stay-at-home order. For example, participant 002 reported that their child was not toilet trained and requested assistance teaching their child to void in the toilet. Twenty-four percent (n = 4) of the caregivers also reported that their dependent’s lack of healthy sleeping habits was an issue at home during Michigan’s stay-at-home order. For example, participant 006 reported that their child often refused to fall asleep at night and refused to wake up in the morning Additionally, twenty-four percent (n = 4) of the caregivers reported that their dependent’s communication was an issue at home during Michigan’s stay-at-home order. These caregivers reported that their child had limited communication skills and requested assistance increasing their child’s ability to express wants and needs. For example, participant 002 reported that their child did not engage in any spontaneous vocal communication.
Further, 12% (n = 2) of the caregivers reported that explaining current events (e.g., COVID-19, quarantine, and Black Lives Matter movement) was a problem at home during Michigan’s stay-at-home order. For example, participant 001 reported that their child was “stressed about COVID-19” and requested additional information to share with their child. Further, participant 019 reported that their child was seeking information regarding the Black Lives Matter movement; the caregiver requested adolescent appropriate information to share with their child.
Lastly, 5% (n = 1) of the caregivers reported that mental health was an issue at home during Michigan’s stay-at-home order. Participant 019 reported an increase in their child’s anxiety since being required to stay at home.
Discussion
Overall, we found that caregivers of individuals with autism in the State of Michigan reported problems in three main thematic areas: (1) decreasing inappropriate behavior, (2) acquiring new skills, and (3) maintaining current levels of performance. Specifically, the majority (> 50%) of caregivers reported that they needed help decreasing problem behavior, increasing social or play skills, and facilitating appropriate school/academic behaviors. In the present paper, we were solely focused on caregiver reported problems during the Michigan stay-at-home order and only reported the problems and concerns expressed by caregivers of individuals with autism to the SCS team.
Our program findings align with those found by recent research (Cahapay, 2022; degli Espinosa et al., 2020; Garcia et al., 2020; Manning et al., 2020) on the impact of COVID-19 on individuals with autism and their caregivers. Our findings further affirm that caregivers of individuals with autism experienced an increase in inappropriate behaviors (e.g., aggression, resistance to demands) and struggled to support appropriate behaviors (e.g., functional communication, daily living skills). Additionally, the COVID-19 crisis caused drastic changes in the established routines for individuals with autism and their families. As a result, caregivers were forced to learn how to educate their child at home, find new activities to keep their child busy, and balance the needs of round-the-clock care for their children with autism (Cahapay, 2022; degli Espinosa et al., 2020; Garcia et al., 2020). Even though we did not ask caregivers to report on their own personal battles, it is interesting that many caregivers did share their own problems at home. For example, some caregivers disclosed marital problems, mental health struggles, and employment/financial struggles caused by Michigan’s stay-at-home order. These reports are consistent with other studies about the impact of COVID-19 (Manning et al., 2020).
Similar to our findings, degli Espinosa et al. (2020) reported that individuals with autism in Italy engaged in increased levels of problem behavior (e.g., aggression), stereotypic behavior, and noncompliance. The authors hypothesize that the increase in inappropriate behaviors may be due in part to changes in reinforcement systems. That is, the reinforcement system at community-based or clinic-based programs may not have generalized to the home setting. Along those lines, typical home reinforcers such as eating at restaurants or attending leisure actives (e.g., cinemas) were no longer available. Caregivers who received telehealth services from our program emphasize the notion that disruptions in reinforcement systems may have impacted problem behaviors. For example, one participant reported that denied access to restaurants did result in bouts of problem behavior. Additionally, degli Espinosa reported that individuals with autism may have requested higher levels of attention, and those requests for attention could have been denied due to caregivers’ need to attend other activities (e.g., work, household chores, attention to siblings).
Limitations and Future Research
Because Michigan did enact a strict stay-at-home order, the results of our program may not generalize to areas that did not enact strict quarantine guidelines (e.g., the State of Georgia). Second, the program did not record meetings with caregivers which may have resulted in undocumented reported problems or important meeting notes. Future telehealth research studies may consider recording meetings on a HIPAA compliant platform for the purposes of further analysis (e.g., discourse analysis). Third, team members did not ask caregivers to report on previous/ongoing service delivery nor did team members record demographic data from participants. Lastly, we did not collect data on client outcomes or procedural fidelity of recommended supports. Due to the immediate need of services caused by the COVID-19 pandemic, SCS was rapidly developed, and the team provided services in less than 1 month after project conception. Here, we believed the ethical course of action was to make services available as soon as possible without getting caught-up in the time-consuming process of designing a controlled research study. But clearly, the need to provide services immediately and the limited time the SCS team with caregivers resulted in obstacles related to data collection (e.g., lack of baseline data). In addition, we did not record procedural fidelity of parent implemented recommendations or supports because we did not want to impose any additional demands on the family system. That is, we were concerned that placing data collection demands on caregivers would result in additional caregiver stress. Because we did not record fidelity of implementation, we also did not collect outcome data for the dependent with autism. These limitations should be taken into consideration when evaluating our program description and its initial findings.
While similar outcomes are reported by many caregivers in the State of Michigan and across the world, it is important to note that each family unit is different, each with unique needs (degli Espinosa et al., 2020). Even though Michigan’s stay-at-home order has been lifted, it is important to understand how individuals with autism and their families were impacted by the COVID-19 crisis. Our program’s findings shed light on such impact, and the stories told by caregivers of individuals with autism during the COVID-19 crisis may inspire additional research and service mechanisms that address strategies to respond to disruptions in service delivery. Though COVID-19 affected lives on a global scale, natural disasters, political unrest, and unforeseen world events will likely continue to disrupt ongoing care for individuals with autism. By establishing, researching, and disseminating innovative technologies to respond to family needs under such circumstances, we can ensure that individuals with autism continue to receive support from trained and compassionate professionals.
Professionals responded to the urgent need of its consumers during the COVID-19 pandemic; however, it is unfortunate that it took a pandemic to establish a broad and overarching infrastructure to provide remote services via technology. Now that we have responded to the consumers receiving services prior to the pandemic (by providing them with remote support via technology), it is long overdue that we consider those who are currently beyond our geographical reach. We encourage researchers and practitioners to employ the use of technology to support families in need, with focused behavioral interventions, while those families are on a waitlist to receive more comprehensive behavioral services. Processes for intake, handling client needs, oversight and supervision, and identifying and building upon key competencies will all be necessary components to evaluate in research, but may further expand the infrastructure available to provide autism services through technology.
An additional area of future research is for scholars to evaluate the effects of on-demand support for children and families who require focused treatment in addressing specific challenges. These children and families may not otherwise require, or pursue, comprehensive services, but may receive focused interventions via telehealth. Relatedly, an on-demand treatment model may allow for the opportunity to identify individuals who may require more intensive or comprehensive interventions. By standardizing operating procedures, the professional may instead recommend an in-home or center-based consultation to better support the person with autism and their family, if remote delivery of behavioral interventions does not meet the client’s needs.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This paper is dedicated to the caregivers and families in the State of Michigan who participated in this project.
Author Contribution
ANW assisted with designing the caregiver program, served as a team member, conducted the data analysis, and wrote the first draft of the paper, and completed a majority of the writing of subsequent paper revisions. MTB created the caregiver program, was responsible for the administration and oversight of the program, wrote the program’s IRB application oversaw human subjects protection and IRB and University compliance, served as a team member, and supervised the writing and revision of the paper. ESS-T assisted with designing the caregiver program, served as a team member, developed training and implementation fidelity materials, and collaborated with writing and editing the paper. DRGM assisted with creating materials and collaborated with writing and editing the paper. HML served as a team member and collaborated with writing and editing the paper. MHF assisted with project conception and writing this paper.
Funding
Financial support for the first author was provided by the Bosco Family Fellowship in Autism and Michigan State University’s College of Education. Financial support for the third and fifth authors was provided by Michigan State University’s College of Education. Financial support for the fourth author was provided by Michigan State University’s Early Learning Institute.
Declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Michigan State University’s Institutional Review Board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Bazeley, P. (2013). Qualitative data analysis: Practical strategies. SAGE.
- Boyd BA, Watson LR, Reszka SS, Sideris J, Alessandri M, Baranek GT, Belardi K. Efficacy of the ASAP intervention for preschoolers with ASD: A cluster randomized controlled trial. Journal of Autism and Developmental Disorders. 2018;48:3144–3162. doi: 10.1007/s10803-018-3584-z. [DOI] [PubMed] [Google Scholar]
- Bice-Urbach BJ, Kratochwill TR. Teleconsultation: The use of technology to improve evidence-based practices in rural communities. Journal of School Psychology. 2016;56:27–43. doi: 10.1016/j.jsp.2016.02.001. [DOI] [PubMed] [Google Scholar]
- Brodhead MT, Quigley SP, Wilczynski SM. A call for discussion about scope of competence in behavior analysis. Behavior Analysis in Practice. 2018;11:424–435. doi: 10.1007/s40617-018-00303-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahapay, M. B. (2022). How Filipino parents educate their children with autism during the covid-19 period. International Journal of Developmental Disabilities, 68(3), 95–398. 10.1080/20473869.2020.1780554 [DOI] [PMC free article] [PubMed]
- Cox DJ, Plavnick JB, Brodhead MT. A proposed process for risk mitigation during the covid-19 pandemic. Behavior Analysis in Practice. 2020;13:299–305. doi: 10.1007/s40617-020-00430-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- degli Espinosa, F., Metko, A., Raimondi, M., Impenna, M., & Scognamiglio, E. (2020). A model of support for families of children with autism living in the covid-19 lockdown: Lessons from Italy. Behavior Analysis in Practice, 13, 550-558.10.1007/s40617-020-00438-7 [DOI] [PMC free article] [PubMed]
- Di Renzo M, Biabchi Di Castalbianco F, Vanadia E, Petrillo M, D’Errico S, Racinaro L, Rea M. Parent-reported behavioral changes in children with autism spectrum disorder during the covid-19 lockdown in Italy. Continuity in Education. 2020;1(1):117–125. doi: 10.5334/cie.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drahota A, Sadler R, Hippensteel C, Ingersoll B, Bishop L. Service deserts and service oases: Utilizing geographic information systems to evaluate service availability for individuals with autism spectrum disorder. Autism. 2020;24:2008–2020. doi: 10.1177/1362361320931265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer AJ, Dart EH, Radley KC, Richardson D, Clark R, Wimberly J. An evaluation of the effectiveness and acceptability of teleconsultation. Journal of Educational and Psychological Consultation. 2017;27:437–458. doi: 10.1080/10474412.2016.1235978. [DOI] [Google Scholar]
- Garcia, J. M., Lawrence, S., Brazendale, K., Leahy, N. (2021). Brief report: The impact of the covid-19 pandemic on health behaviors in adolescents with autism spectrum disorder. Disability and Health Journal, 14. 10.1016/j.dhjo.2020.101021 [DOI] [PMC free article] [PubMed]
- Kasari C, Smith T. Interventions in schools for children with autism spectrum disorder: Methods and recommendations. Autism. 2013;17:254–267. doi: 10.1177/1362361312470496. [DOI] [PubMed] [Google Scholar]
- Lindgren S, Wacker D, Suess A, Schieltz K, Pelzel K, Kopelman T, Waldron D. Telehealth and autism: Treating challenging behavior at lower cost. Pediatrics. 2016;137:S167–S175. doi: 10.1542/peds.2015-2851O. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, Linney C, McManus M, Borwick C, Crawley E. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the Context of COVID-19. Journal of the American Academy of Child & Adolescent Psychiatry. 2020;59(11):1218–1239. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning J, Billian J, Matson J, Allen C, Soares N. Perceptions of families of individuals with autism spectrum disorder during the covid-19 crisis. Journal of Autism and Developmental Disorders. 2020 doi: 10.1007/s10803-020-04760-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neely L, Rispoli M, Boles M, Morin K, Gregori E, Ninci J, Hagan-Burke S. Interventionist acquisition of incidental teaching using pyramidal training via telehealth. Behavior Modification. 2019;43:711–733. doi: 10.1177/0145445518781770. [DOI] [PubMed] [Google Scholar]
- Qualtrics, Provo, UT (2019). Qualtrics software (Version October, 2020) of Qualtrics. https://www.qualtrics.com
- Russell BS, Hutchison M, Tambling R, Tomkunas AJ, Horton AL. Initial challenges of caregiving during COVID-19: Caregiver burden, mental health, and the parent–child relationship. Child Psychiatry & Human Development. 2020;51(5):671–682. doi: 10.1007/s10578-020-01037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell, B. S., Tomkunas, A. J., Hutchison, M., Tambling, R. R., & Horton, A. L. (2021). The protective role of parent resilience on mental health and the parent–child relationship during COVID-19. Child Psychiatry & Human Development, 110.1007/s10578-021-01243-1 [DOI] [PMC free article] [PubMed]
- Saldaña, J. (2016). The coding manual for qualitative researchers. SAGE.
- State of Michigan. (2020, March 23). Governor Whitmer signs “stay home, stay safe” executive order. Michigan.gov. https://www.michigan.gov/whitmer/0,9309,7-387-90499_90640-522625--,00.html#:~:text=Effective
- Schwartz IS, Baer DM. Social validity assessments: Is current practice state of the art? Journal of Applied Behavior Analysis. 1991;24:189–204. doi: 10.1901/jaba.1991.24-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark AM, White AE, Rotter NS, Basu A. Shifting from survival to supporting resilience in children and families in the COVID-19 pandemic: Lessons for informing U.S. mental health priorities. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S133–S135. doi: 10.1037/tra0000781. [DOI] [PubMed] [Google Scholar]
- Stenhoff DM, Pennington RC, Tapp MC. Distance education supports for students with autism spectrum disorder and complex needs during covid-19 and school closures. Rural Special Education Quarterly. 2020;39(4):211–219. doi: 10.1177/8756870520959658. [DOI] [Google Scholar]
- Tomlinson SR, Gore N, McGill P. Training individuals to implement applied behavior analytic procedures via telehealth: A systematic review of the literature. Journal of Behavioral Education. 2018;27:172–222. doi: 10.1007/s10864-018-9292-0. [DOI] [Google Scholar]
- Unholz-Bowden E, McComas JJ, McMaster KL, Girtler SN, Kolb RL, Shipchandler A. Caregiver training via telehealth on behavioral procedures: A systematic review. Journal of Behavioral Education. 2020;29:246–281. doi: 10.1007/s10864-020-09381-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner L, Corona LL, Weitlauf AS, Marsh KL, Berman AF, Broderick NA, Francis S, Hine J, Nicholson A, Stone C, Warren Z. Use of the tele-asd-peds for autism evaluation in response to covid-19: Preliminary outcomes and clinician acceptability. Journal of Autism and Developmental Disabilities. 2020;51(9):3063–3072. doi: 10.1007/s10803-020-04767-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yingling ME, Ruther MH, Dubuque EM, Mandell DS. County-level variation in geographic access to Board Certified Behavior Analysts among children with Autism Spectrum Disorder in the United States. Autism. 2021 doi: 10.1177/13623613211002051. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


