Abstract
Background
Closed flexor pulley injuries are a clinical entity of great interest in hand surgery, and these lesions could be observed mainly in rock-climbing athletes.
Objective
An extensive literature search of PubMed, SCOPUS, Cochrane Library, and Web of Sciences databases on closed finger pulley rupture, related treatments, and outcomes were performed. All relevant information was used in this literature review.
Conclusions
Many athletes are potentially exposed to these uncommon injuries. Therefore, these lesions require careful examination and a high index of suspicion to confirm the diagnosis and identify the degree of soft tissue injury, particularly in patients not involved in sporting activities. The data summarized in this literature review demonstrated that according to Schöffl's classification, conservative treatment should be indicated for low-grade injuries (grade 1 or 2), whereas surgical treatment should be performed in patients with more severe acute injuries (grade 4). Grade 3 flexor pulley injuries lie in a grey area where conservative and surgical treatment may give good clinical and return-to-sport patient results.
Keywords: Pulley injury, Pulley rupture, Flexor tendon, Rock climbing, Bowstringing, Finger injury
1. Introduction
Finger flexor pulleys prevent the flexor tendons from deviating from their anatomical position during hand activities.1 These injuries are uncommon but sometimes may be found in some sports categories, such as rock-climbing, bouldering, and martial arts athletes.2,3 Flexor tendon pulley lesions are mainly observed in athletes who are out of shape or undergo overtraining. Additional risk factors are the absence of a proper warm-up before training and the lack of stretching and cooling of the body's muscles at the end of the workout.3 This lesion occurs mainly in a specific anatomical-functional hand position defined as a “crimp grip”. This condition results in an attitude of the proximal interphalangeal joint (PIPJ) in 90–100° flexion and hyperextension of the distal interphalangeal joint (DIPJ). In this situation, the flexor tendons exert very intense forces on the corresponding pulleys.4 Pulley ruptures should result in tendon flexor bowstringing, leading to functional deficits. The diagnosis may be made clinically if tendon bowstringing is observable; otherwise, diagnostic accuracy is enhanced with ultrasound (US) or magnetic resonance imaging (MRI).5 The scientific literature on closed-finger flexor pulley injuries has increased recently. Nevertheless, few published studies analyze clinical and diagnostic management strategies and treatment outcomes.
This review examines flexor tendon pulley injuries by analyzing their anatomy and biomechanical characteristics and aiming to provide a methodical diagnostic and therapeutic approach to assist orthopedics in appropriately managing this rare hand injury.
2. Methodology
This review evaluated current evidence of closed finger pulley rupture treatments and outcomes. A literature search was done in the following databases: PubMed, SCOPUS, Cochrane Library, and Web of Sciences. All information relevant to the review was considered. We used the following inclusion criteria: articles published in English, French and Italian languages, the full text of the articles should be available, human studies only. Biochemical and in vitro studies, editorials, technical notes, preclinical studies, and studies with a methodology lack or level of evidence (LoE) 5 were excluded from the search.
3. Anatomic considerations
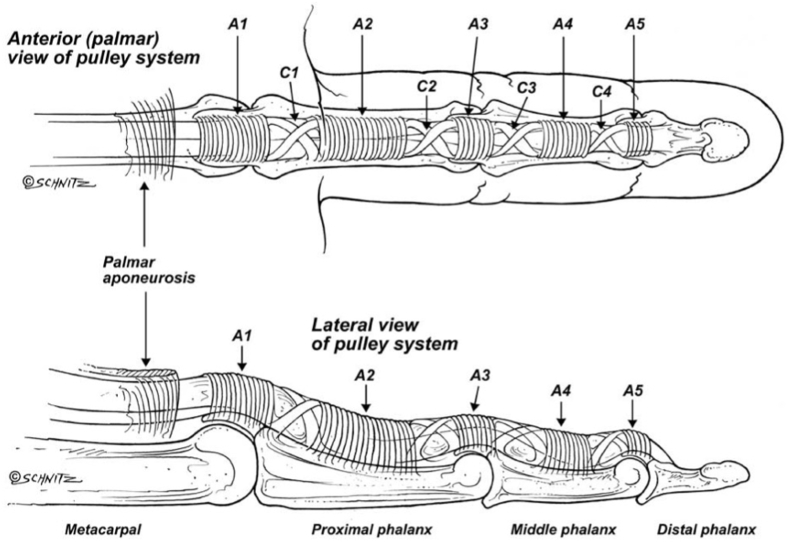
The long fingers' pulley system comprises eight pulleys through which the flexor tendons slide: five annular (A) pulleys defined A1-5 and three cruciate (C) pulleys defined C1-3 (Fig. 1).
Fig. 1.
The digital pulley system of the fingers.
The first annular pulley A1 originates from the palmar plate at the metacarpophalangeal joint level and continues to the base of the proximal phalanx. Pulley A2 includes the area between the proximal portion of the proximal phalanx (P1) and the proximal two-thirds of P1. Pulley A3 is located at the PIPJ. Pulley A4 is centered at the middle portion of the middle phalanx (P2). The A5 pulley lies on the DIPJ. The cruciate pulleys are situated between the annular pulleys, composed of oblique fibers that interdigitate with the annular pulleys ones: the C1 pulley is located distally to the A2 pulley, whereas the C2 pulley is placed between the A3 and A4 pulleys and the C3 pulley lies at the distal end of the A4 pulley.1 Their shape makes them flexible; therefore, they are secondary to digital kinematics.6
The annular pulleys can be divided into two main groups according to their peculiarities. A1, A3, and A5 pulleys are inserted on the metacarpophalangeal joint's volar plate (MCPJ), PIPJ and DIPJ; they are the most flexible ones. On the other hand, pulleys A2 and A4 are fibrous pulleys that insert on the bony surface of P1 and P2, respectively. The latter is also robust, and the pinch or grasp movements exert the main eccentric strengths.1,4
At the thumb level, there are three constant pulleys: the first is located at the MCPJ, has an annular shape, and is defined as pulley A1; the second is also an annular pulley, is called pulley A2, and corresponds to the interphalangeal joint. Between these two pulleys runs an oblique pulley which originates proximally from the radial side and inserts distally on the ulnar side of P1.7
4. Epidemiology and biomechanics
The pulleys, especially the annular ones, act like a fibrous envelope preventing the tendons from diverging from the midline axis in lateral and anteroposterior directions, minimizing the excursion of flexor tendons and allowing the conversion of the flexors' pulling action into an angular motion which causes the finger joints to bend.1,6
Pulley system injuries are not common among the population, but they are very typical rock climbers' lesions: out of all the injuries occurring in rock climbing, 33% include flexor tendons or flexor tendon pulleys injuries. Moreover, competitive climbers have an estimated 19–26% incidence of pulley ruptures.8 These lesions' peculiar distribution among these specific athletes' categories is due to the hand's position during the activity. In rock climbing, all the body weight is often exclusively supported by the distal phalanges in a kind of grip called “crimp grip”: PIPJ flexed to 90–100° and DIPJ hyper-extended.4 In this hand configuration, the flexor tendons apply very intense bowstringing forces, especially at the A2 and A4 pulleys, with 1.5–4 times the force generated at the fingertips.4,8,9 Considering a 70 kg rock climber executing the “crimp grip”, the forces usually generated on A2 and A4 pulleys are respectively 287 N and 226 N.10 However, the lesion often occurs upon a sudden and unexpected extending force acting on the fingers while already in a hanging position,11 such as a shock loading on a single finger (for instance, in case of missed foot support): forces applied on A2 rise to 450 N, exceeding the failure force of A2 pulley (400 N).8,12,13
A2 pulley is the most frequently damaged pulley in rock climbing activities, followed by the A4 pulley. Concomitant A3 pulley damage is possible.11,14,15 The most frequently affected fingers are the middle and ring fingers.8 In biomechanical models, the middle and the ring finger exert 60% of the total amount of fingertip force, therefore undergoing the highest tendon tensions, which cause the A2 pulley to be loaded up to close the breakpoint in normal conditions (64% at the ring finger, 90% at the middle finger).9 Repetitive strain on pulleys could lead to acute injury or overuse syndrome. Closed flexor pulley injuries represent the most diagnosed overuse syndromes in climbers. The high frequency may be explained by the biomechanics of the movement performed. The upper limbs simultaneously support a large part of the climber's weight through a few fingers. Specifically, the ‘crimp grip’ is used to maximize the contact of the fingertips on a small surface area, which leads to repetitive overloading of the pulleys, resulting in overuse injuries.16 Cases of closed pulley rupture not associated with climbing but related to carrying heavyweights on the fingertips have been documented; the mechanism of injury would appear to be very similar.4
5. Clinical presentation and diagnosis
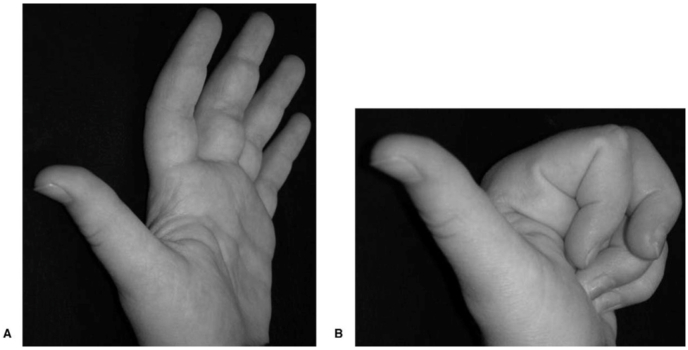
In athletes, pulleys damage could occur along with prodromic symptoms, such as pain and swelling, that usually develop two or three weeks before the rupture. However, the rupture may also occur acutely, without prodromes.14 Patients describe an acute pain onset, a “tearing” sensation, occasionally accompanied by a loud “pop” and followed by difficulty in flexion movements and decreased finger dexterity.1,4 The patients present local pain and swelling around the involved finger, tenderness and hematoma localized at the injured pulley, and pain and weakness in pinching and grasping movements.14 Bowstringing causes a deficit in tendon shortening during active flexion, resulting in loss of power and function.4 If an intact A3 pulley is present, bowstringing does not occur despite isolated rupture of the A2 or A4 pulley.8 Combined injuries of the A2-A3 and A2-A3-A4 pulleys could enhance the flexor tendons' bowstringing.6 However, these findings are not necessarily specific and, therefore, not enough to make a sure diagnosis: further imaging is usually needed14 (Fig. 2).
Fig. 2.
Clinical photograph of a patient with an acute A2-pulley rupture, middle finger, left hand. Fig. 2-A with the hand (A) open. Fig. 2-B with the hand (B) closed. Note the swelling and the active flexion deficit in the proximal interphalangeal joint one week after the trauma.
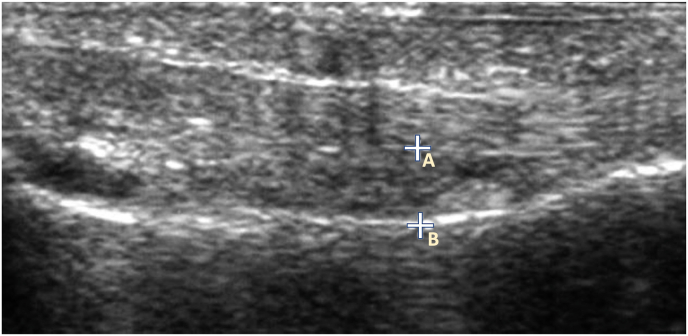
Swelling during the acute phase may render the clinical examination more complex and less accurate. Radiographs, often performed to exclude bone fractures or volar avulsions, only allow the identification of non-specific soft tissue swelling and, for these reasons, are not the diagnostic examination of first choice.17 The US, on the contrary, allows pulleys dynamic evaluation, identification of possible bone fractures, and measurement of tendon bowstringing (the distance between tendon and bone in forced flexion and extension) (Fig. 3). The US has a sensitivity of 98% and a specificity of 100%.8 When doubts persist after the US, using a high-field MRI or dedicated finger radiofrequency coil MRI of the finger could diagnose injuries that would otherwise be extremely difficult to assess and may go undiagnosed.18
Fig. 3.
Ultrasound image of A2-pulley rupture. The distance between point A and point B represent the tendon-bone distance.
6. Treatment options
The treatment of closed flexor tendon pulley injuries must be regarded according to new anatomic and biomechanical concepts in recent years. Previous indications assumed that A2 and A4 pulleys were inviolable.1
In their works, Franko et al. and Mitsionis et al. demonstrated through cadaver evaluations that the A2 and A4 pulleys can be opened up to 25%, individually or in combination, without causing an increase in work or a deficit in finger flexion.19,20 For this reason, there is a threshold of pulley tolerance before functional problems arise; therefore, the indication for surgical reconstruction is not peremptory.
Schöffl et al. proposed a classification to guide the therapeutic process based on these concepts, depending on the lesion pattern5 (Table 1). According to these authors, pulley injuries can be divided into four groups. Grade 1 injuries are pulley sprain without dehiscence of the tendon from the bone (<2 mm) on MRI or US. Grade 2 injuries consist of a complete rupture of the A4 pulley or an incomplete rupture of the A2 or A3 pulleys. Grade 3 injuries are characterized by a complete pulley A2 or A3 breakage. Finally, Grade 4 injuries are the most severe and include multiple complex pulley ruptures or a single A2 or A3 pulley rupture with associated lumbrical muscle or collateral ligament injuries.4,5
Table 1.
Classification of pulley injury severity.
| Classification of pulley lesions according to Schöffl et al.5 | |
|---|---|
| Grade 1 | Stretching or slight tearing |
| Grade 2 | A2 or A3 partial rupture, A4 complete rupture |
| Grade 3 | A2 or A3 complete rupture |
| Grade 4 | Multiple complete ruptures |
A2: annular A2 pulley; A3: annular A3 pulley; A4: annular A4 pulley.
Grade 1 and 2 injuries should be treated conservatively, while grade 4 lesions may be treated surgically.5,16,21,22 There is no uniformity in the treatment of grade 3 flexor pulley injuries. Schöffl et al. proposed conservative treatment, limiting the surgical option to grade 4 lesions only.5,16 At the same time, other authors treated grade 3 and grade 4 injuries surgically.21,22 However, surgical and conservative treatment provided good clinical results and returned to the sport in patients with grade 3 flexor pulley injuries.
The most used surgical techniques are8,14:
-
-
Kleinert/Weilby Technique (Shoelace Weave): the surgeon harvests a flexor digitorum superficialis (FDS) graft, which is then passed in a shoelace fashion through holes created in the remaining pulley stumps.
-
-
Lister's Extensor Retinaculum Technique: the operator harvests a graft of extensor retinaculum, looped around the phalanx, and then sutured on itself.
-
-
Okutsu triple-loop reconstruction: a tendon graft, usually of palmaris longus, is looped subcutaneously three times around the phalanx and then sutured.
-
-
The “loop-and-a-half” technique of Widstrom: a free graft of palmaris longus is looped around the phalanx and passed through an operculum opened surgically in the thickness of the graft, then each end is sutured to either side. The last is the technique of choice for many authors in the literature.15
7. Physical therapy
The rehabilitation protocol prescribed by Schoffl et al.5 for grade 1 injuries is a functional therapy of two-four weeks, without any prescribed immobilization. Protection of the pulley by taping, linear or H-shaped, is recommended.
Grade 2 injuries are treated with ten-day immobilization, cautious functional therapy for two to four weeks, and tape to protect the damaged pulley. The treatment of injuries classified as Grade 3 involves immobilization for fourteen days, functional therapy for up to four weeks, and protection of the injured pulley with a thermoplastic ring. Grade IV injuries involve surgical treatment and a protocol of two weeks of immobilization following surgery. Functional therapy is four weeks, and pulley protection is performed with a thermoplastic ring. Various scores could assess outcomes following treatment, whether bloodless or surgical. Essential parameters in outcome assessment are interphalangeal joint flexions, extension lag, and total active motion (TAM). The Buck-Gramko score is considered these parameters, one of the most widely used evaluation scores (Table 2). A score is allocated according to the flexion of the interphalangeal joint. From 0 to 6 points are assigned for flexion between 50 and 90°, 4 points for flexion 30–49°, 2 points for flexion between 10 and 29°, and 0 if less than 10°. The extension lag, also measured in degrees, assigns a score from 1 to 3 points (an extension deficit between 0 and 10° assigns 3 points, a lag between 11 and 20° 2 points, 1 point if between 21 and 30°, and 0 if greater than 30°). TAM is the last parameter considered by this score: a TAM greater than 40° gives 6 points to the final score, 4 points if between 30 and 39°, 2 points between 20 and 29°, and 0 points if less than 20°. A final score of 14–15 points constitutes an “excellent” result, between 11 and 13 points a “good” result, between 7 and 10 “fair”, and “poor” between 0 and 6. Other essential assessment parameters are pinch strength and grip strength measured in Newtons compared to the healthy contralateral hand.
Table 2.
Buck-Gramcko score.
| Measurement of Index Through Ring Fingers Points | Points |
|---|---|
| Active flexion deficit,a cm/b | |
| 0–2.5/≥200 | 6 |
| 2.5–4/≥180 | 4 |
| 4–6/≥150 | 2 |
| 6/<150 | 0 |
| Extension deficit,b | |
| 0–30 | 3 |
| 31–50 | 2 |
| 51–70 | 1 |
| >70 | 0 |
| Range of motion,b | |
| ≥160 | 6 |
| ≥140 | 4 |
| ≥120 | 2 |
| <120 | 0 |
Grading was as follows: 14, 15 points: excellent; 11–13 points: good; 7–10 points: fair; 0–6 points: poor.
active flexion deficit measured as the distance from the digital tip to the distal palmar crease in active flexion.
degree(s).
A non-clinical score that could still be used for outcome assessment is the international grading system Union Internationale des Associations d'Alpinisme (UIAA). By assigning a score to each climber based on his or her sporting ability, this score may be used to assess the climber's sporting level following treatment, indirectly assessing the outcome based on his or her return to full activity.22
8. Conclusions
Closed flexor tendon pulley injuries require careful examination and a high index of suspicion, particularly in patients not involved in sports activity. Therefore, US and MRI are suggested to confirm the diagnosis and detect the grade of soft tissue injury. On this basis, the most appropriate treatment could be selected, and in most cases, positive clinical results can be achieved with either conservative or surgical therapy.
Funding
This research received no external funding.
Ethical standard
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Data availability statement
Data is contained within the article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
References
- 1.Dy C.J., Daluiski A. Flexor pulley reconstruction. Hand Clin. 2013;29(2):235–242. doi: 10.1016/j.hcl.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Lee J.H., Kim H.S., Joo S.H. Isolated A1 pulley rupture of left fourth finger in kendo players: two case reports. Ann Rehabil Med. 2015;39(5):838–843. doi: 10.5535/arm.2015.39.5.838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones G., Schöffl V., Johnson M.I. Incidence, diagnosis, and management of injury in sport climbing and bouldering: a critical review. Curr Sports Med Rep. 2018;17(11):396–401. doi: 10.1249/JSR.0000000000000534. [DOI] [PubMed] [Google Scholar]
- 4.Crowley T.P. The flexor tendon pulley system and rock climbing. J Hand Microsurg. 2012;4(1):25–29. doi: 10.1007/s12593-012-0061-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schöffl V., Hochholzer T., Winkelmann H.P., Strecker W. Pulley injuries in rock climbers. Wilderness Environ Med. 2003;14(2):94–100. doi: 10.1580/1080-6032(2003)014[0094:piirc]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 6.Martinoli C., Bianchi S., Cotten A. Imaging of rock climbing injuries. Semin Muscoskel Radiol. 2005;9(4):334–345. doi: 10.1055/s-2005-923378. [DOI] [PubMed] [Google Scholar]
- 7.Wilson S.M., Roulot E., Le Viet D. Closed rupture of the thumb flexor tendon pulleys. J Hand Surg. 2005;30(6):621–623. doi: 10.1016/j.jhsb.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 8.King E.A., Lien J.R. Flexor tendon pulley injuries in rock climbers. Hand Clin. 2017;33(1):141–148. doi: 10.1016/j.hcl.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Vigouroux L., Quaine F., Paclet F., Colloud F., Moutet F. Middle and ring fingers are more exposed to pulley rupture than index and little during sport-climbing: a biomechanical explanation. Clin Biomech. 2008;23(5):562–570. doi: 10.1016/j.clinbiomech.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 10.Schöffl I., Oppelt K., Jüngert J., Schweizer A., Neuhuber W., Schöffl V. The influence of the crimp and slope grip position on the finger pulley system. J Biomech. 2009;42(13):2183–2187. doi: 10.1016/j.jbiomech.2009.04.049. [DOI] [PubMed] [Google Scholar]
- 11.Cockenpot E., Lefebvre G., Demondion X., Chantelot C., Cotten A. Imaging of sports-related hand and wrist injuries: sports imaging series. Radiology. 2016;279(3):674–692. doi: 10.1148/radiol.2016150995. [DOI] [PubMed] [Google Scholar]
- 12.Iruretagoiena-Urbieta X., De la Fuente-Ortiz de Zarate J., Blasi M., Obradó-Carriedo F., Ormazabal-Aristegi A., Rodríguez-López E.S. Grip force measurement as a complement to high-resolution ultrasound in the diagnosis and follow-up of A2 and A4 finger pulley injuries. Diagnostics. 2020;10(4):206. doi: 10.3390/diagnostics10040206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin G.T., Amadio P.C., An K.N., Cooney W.P., Chao E.Y. Biomechanical analysis of finger flexor pulley reconstruction. J Hand Surg Br. 1989;14(3):278–282. doi: 10.1016/0266-7681_89_90081-8. [DOI] [PubMed] [Google Scholar]
- 14.Freilich A.M. Evaluation and treatment of Jersey finger and pulley injuries in athletes. Clin Sports Med. 2015;34(1):151–166. doi: 10.1016/j.csm.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Cole K.P., Uhl R.L., Rosenbaum A.J. Comprehensive review of rock climbing injuries. J Am Acad Orthop Surg. 2020;28(12):e501–e509. doi: 10.5435/JAAOS-D-19-00575. [DOI] [PubMed] [Google Scholar]
- 16.Schöffl V.R., Jüngert J. Closed flexor pulley injuries in nonclimbing activities. J Hand Surg Am. 2006;31(5):806–810. doi: 10.1016/j.jhsa.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Heiss R., Librimir A., Lutter C., et al. MRI of finger pulleys at 7T-direct characterization of pulley ruptures in an ex vivo model. Diagnostics. 2021;11(7):1206. doi: 10.3390/diagnostics11071206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krug R., Stehling C., Kelley D.A., Majumdar S., Link T.M. Imaging of the musculoskeletal system in vivo using ultra-high field magnetic resonance at 7 T. Invest Radiol. 2009;44(9):613–618. doi: 10.1097/RLI.0b013e3181b4c055. [DOI] [PubMed] [Google Scholar]
- 19.Mitsionis G., Bastidas J.A., Grewal R., Pfaeffle H.J., Fischer K.J., Tomaino M.M. Feasibility of partial A2 and A4 pulley excision: effect on finger flexor tendon biomechanics. J Hand Surg Am. 1999;24(2):310–314. doi: 10.1053/jhsu.1999.0310. [DOI] [PubMed] [Google Scholar]
- 20.Franko O.I., Lee N.M., Finneran J.J., et al. Quantification of partial or complete A4 pulley release with FDP repair in cadaveric tendons. J Hand Surg Am. 2011;36(3):439–445. doi: 10.1016/j.jhsa.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arora R., Fritz D., Zimmermann R., et al. Reconstruction of the digital flexor pulley system: a retrospective comparison of two methods of treatment. J Hand Surg Eur. 2007;32(1):60–66. doi: 10.1016/j.jhsb.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 22.Bouyer M., Forli A., Semere A., Chedal Bornu B.J., Corcella D., Moutet F. Recovery of rock climbing performance after surgical reconstruction of finger pulleys. J Hand Surg Eur. 2016 May;41(4):406–412. doi: 10.1177/1753193415623914. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is contained within the article.