Abstract
Introduction
Performing total knee arthroplasty (TKA) without the use of tourniquet is gaining popularity. However, performing a “tourniquetless TKA” has a variety of meanings regarding the timing and application of a tourniquet and associated techniques. The purpose of this systematic review was to evaluate the literature and more accurately define “tourniquetless TKA.”
Methods
A systematic review following PRISMA guidelines was performed of the PubMed, Web of Science, and Cochrane databases for articles published from 2016 to 2021. Inclusion criteria included papers that used “tourniquetless” or a similar term to describe their TKA procedure, original clinical studies, English language, and full-text studies.
Results
A total of 1,096 studies were identified, of which 84 full text studies with 9,349 total patients were included. Overall, 17 (20.2%) of the studies performing tourniquetless TKA never applied a tourniquet, 17 (20.2%) applied a tourniquet but kept it deflated throughout the entire procedure, 2 (2.4%) applied a tourniquet and inflated during cementation only, and 48 (57.1%) did not specify. Ultimately, of the studies that did specify tourniquet use, only 17 studies (47.2%) truly never applied a tourniquet throughout the procedure. A review of 7 recommended techniques to control blood loss in tourniquetless TKA found that no one technique was performed in more than 10.6% of patients.
Conclusion
Variation in the definition of tourniquetless TKA and the utilization of augmented techniques to control blood loss remains. We propose the terms “tourniquetless” for no tourniquet application, “tourniquet-available” for tourniquet applied but kept deflated throughout surgery, and “tourniquet-assisted” for tourniquet inflation during cementation only. These terms can help better differentiate the literature, guide surgeons as they transition to tourniquetless TKA, and assist in the development of more definitive protocols for tourniquetless TKA.
Keywords: Tourniquetless, Tourniquet, TKA, Total knee arthroplasty, Hemostasis, Blood loss, Systematic review
Abbreviations: TKA, Total Knee Arthroplasty
Highlights
-
•
There is inconsistency in the definition of tourniquetless TKA in the current literature.
-
•
This review reveals poor uptake in recommended techniques for blood control in tourniquetless TKA.
-
•
We propose novel terms to more precisely define methods in tourniquetless TKA.
1. Introduction
The use of a pneumatic tourniquet has historically been common practice in total knee arthroplasty (TKA). As recently as 2011, over 90% of surgeons in the US and Europe routinely used tourniquets for TKA.1, 2, 3 Typically, a tourniquet is applied at high pressure around the upper leg for all or part of the procedure. Reduced intraoperative blood loss, decreased operative time, improved visualization, and better cement fixation were all considered advantages to tourniquet use.4, 5, 6
However, the clinical evidence has not supported these benefits and highlighted important risks. Tourniquet use can introduce venous stasis and ischemia and has been associated with increased pain, compartment syndrome, venous thromboembolisms, rhabdomyolysis, nerve damage, and infection.7, 8, 9 A 2021 Cochrane review of 41 randomized control trials found while tourniquet use did significantly reduce mean operative time, it had no significant impact on blood loss and was associated with increased risk for serious adverse events, increased pain scores, and longer length of hospital stays.10 Alternative methods have been developed that create many of the benefits of tourniquet use without the risks. Techniques such as anemia screening, controlled hypotension, knee flexion through surgery, placement of a bone plug in the femoral canal, pulse lavage, swab packing, CO2 gas application, and computer navigation have all contributed to the safe performance of tourniquetless TKA.9
As the performance of tourniquetless TKA becomes more common, so does the diversity in tourniquetless surgery protocols. Tourniquet inflation from the start of cementation to the completion of the procedure, inflation during cementation only, deflation throughout the procedure but applied as an emergency measure, and tourniquet never applied have all been reported in the literature as alternatives to full tourniquet use in TKA.11, 12, 13, 14 The term “tourniquetless” in the context of TKA can thus be associated with a wide variety of meanings regarding the use of tourniquet and associated adjunct techniques during the procedure. By surveying the available literature, our purpose was to more accurately define “tourniquetless” TKA by exact timing and application of tourniquet. Our hypothesis is that there is large inconsistency in the use of the term tourniquetless that requires the proposal of novel terms to more precisely represent tourniquet use in TKA.
2. Methods
This review was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.15 A review protocol was completed and published on the PROSPERO database (323,025). A literature search was preformed of the PubMed, Web of Science, and Cochrane Library databases in October 2021. Search criteria was “((tourniquetless) OR (tourniquet-less) OR (tourniquet)) AND (arthroplasty)) AND (knee).” To ensure the most updated data was used, only articles published from 2016 to 2021 were included. Only English language and full-text studies were included. Inclusion criteria was all clinical studies discussing primary TKA that indicated they performed the surgery without the use of a tourniquet through terms such as “tourniquetless,” “tourniquet-less,” “without tourniquet,” “no tourniquet,” “tourniquet free,” “absence of tourniquet,” and “tourniquet use obsolete.” Risk of bias assessment was performed at the individual study level across outcomes. Exclusion criteria included studies with Level V evidence or below, systematic reviews and meta-analyses, and studies that did not indicate they performed surgery without the use of a tourniquet.
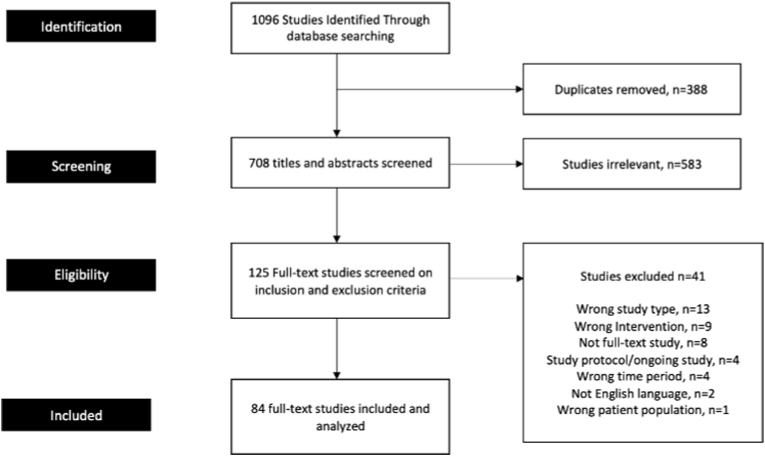
The literature search resulted in a total of 1096 studies. After the removal of duplicates, the 708 studies remaining studies were then reviewed by title and abstract. Finally, the full text of each of the remaining studies was screened by inclusion and exclusion criteria. Any differences in reviews were verbally sorted and resolved by consensus. Each study included in the final analysis was assessed to determine how they defined “tourniquetless.” From this analysis, the team categorized definitions of tourniquetless into four groups: no tourniquet applied ever, tourniquet applied but deflated throughout surgery, tourniquet inflated only during cementation, and not specified.
Using a standardized data collection form, we evaluated the type of study, category of “tourniquetless,” number of patients, the use of recommended techniques to control blood loss, and use of cemented or Press Fit implants. The performance of 7 augmented methods that have been cited in the literature to control blood loss and improve visualization in tourniquetless TKA were collected in this study: controlled hypotension, knee flexion throughout surgery, autologous bone plug placed in the femoral canal, pulse lavage, swab packing, CO2 gas use, and use of computer navigation.9 The use of other methods of blood control, such as tranexamic acid and electrocautery, were considered standard of care and not collected. The data was synthesized into 3 tables and presented as total number and percentages of included studies and patients. Covidence online software was used to facilitate citation tracking, screening of abstracts and full-text articles, and extraction of data.
3. Results
Of a total of 125 full text studies screened for eligibility, 41 were excluded for failing to meet our inclusion criteria (Fig. 1). A total of 9349 patients participated in the 84 studies included in the analysis (Supplemental Appendix). In all, 47 of the studies were randomized control trials (56.0%), 27 were retrospective reviews (32.1%), 6 were prospective cohort studies (7.1%), 3 were prospective case series (3.6%), and 1 was a case-control study (1.2%). Risk of bias assessment resulted in the exclusion of 13 articles for containing Level V evidence or below.
Fig. 1.
Prisma flow diagram.
Only 17 studies (20.2%) including 2799 patients (29.9%) indicated that a tourniquet was never applied at any point during surgery (Table 1). In 17 studies (20.2%) a tourniquet was applied but kept deflated throughout the entire procedure and in 2 studies (2.4%) a tourniquet was applied and inflated during cementation only. The greatest number of studies, 48 (57.1%), did not specify what they meant by tourniquetless surgery. Ultimately, of the studies that did specify tourniquet use, only 17 studies (47.2%) truly never applied a tourniquet throughout the procedure.
Table 1.
Classification of definitions of tourniquetless TKA.
| Classification | Studies (%) | Patients (%) |
|---|---|---|
| Never applied | 17 (20.2%) | 2799 (29.9%) |
| Applied but deflated throughout entire procedure | 17 (20.2%) | 1910 (20.4%) |
| Applied and inflated during cementation | 2 (2.4%) | 104 (1.1%) |
| Not specified | 48 (57.1%) | 4536 (48.5%) |
| Total | 84 | 9349 |
For augmented techniques to control blood loss, only controlled hypotension (10.5%) and autologous bone plug placement in the femoral canal (10.6%) were performed in greater than 10% of all patients (Table 2). The techniques most cited in studies were controlled hypotension (13, 15.5%) and pulse lavage (17, 20.2%). CO2 gas (2, 2.4%), swab packing (3, 3.6%), and computer navigation (3, 3.6%) were the techniques reported in the least number of studies. Only two studies reported using 4 of the recommended techniques tracked for this study. No study reported using more than 4 of the of the 7 augmented techniques to control blood loss. 47 studies (56.0%) did not specify using any of the recommended techniques to control blood loss. Press Fit implants were used in a total of 6 studies (7.1%) or 615 patients (6.6%) (Table 3). The remainder of the studies used cemented implants (92.9%).
Table 2.
Number of patients for whom augmented techniques to control blood loss were utilized.
| Classification | Controlled hypotension | Knee flexion throughout surgery | Bone plug in femoral canal | Pulse Lavage | Swab Packing | CO2 gas | Computer Navigation |
|---|---|---|---|---|---|---|---|
| Never applied | 195 (6.7%) | 130 (4.6%) | 96 (3.4%) | 368 (13.1%) | 0 (0%) | 79 (2.8%) | 79 (2.8%) |
| Applied but deflated throughout entire procedure | 72 (3.8%) | 72 (3.8%) | 31 (1.6%) | 179 (9.4%) | 51 (2.7%) | 0 (0%) | 20 (1.0%) |
| Applied and inflated during cementation | 0 (0%) | 104 (100%) | 54 (51.9%) | 54 (52.0%) | 54 (51.9%) | 0 (0%) | 0 (0%) |
| Unspecified | 716 (15.8%) | 86 (1.9%) | 809 (17.8%) | 285 (6.3%) | 29 (5.4%) | 91 (2.0%) | 91 (2.0%) |
| Total | 983 (10.5%) | 392 (4.2%) | 990 (10.6%) | 886 (9.5%) | 134 (6.6% | 170 (1.8%) | 190 (2.0%) |
Table 3.
Tourniquet use by Press Fit and Cemented Implant Type.
| Classification | Press Fit TKA implants | Cemented Implants |
|---|---|---|
| Never applied | 173 (6.2%) | 2626 (93.8%) |
| Applied but deflated throughout entire procedure | 196 (10.3%) | 1714 (89.7%) |
| Applied and inflated during cementation | 0 (0%) | 104 (100%) |
| Unspecified | 246 (5.4%) | 4290 (94.6%) |
| Total | 615 (6.6%) | 8734 (93.4%) |
4. Discussion
Many studies exist reporting on the performance of tourniquetless TKA. However, the lack of consistency in the definition of “tourniquetless” makes it difficult to reliably compare surgical procedures and draw conclusions from the outcomes. In the current TKA literature, a majority of studies (57.1%) did not specify on how they defined the term “tourniquetless” in TKA. In different studies that did specify, no tourniquet ever applied, tourniquet applied but kept deflated, and tourniquet inflated only during cementation were all defined as tourniquetless. These findings highlight the diversity in protocols that are all considered tourniquetless in the current literature.
This inconsistency extends to the reporting of adjunct procedures recommended to augment blood control in tourniquetless TKA. Of the 7 recommend techniques to augment blood control in tourniquetless TKA, no method was reported as being utilized in more than 10.6% of patients included in this study. No single study reported utilizing more than 4 of the 7 recommended techniques tracked in this analysis. Additionally, a Press Fit implant was utilized in small percentage of patients (6.6%), suggesting clinicians are still comfortable with implant cementation without the use of a tourniquet. These findings reflect a broad variety of augmented surgical protocols employed in tourniquetless TKA and a slow uptake of techniques recommended to improve blood control and maintain proper visualization.
There is a growing body of literature supporting TKA with no tourniquet. Benefits include reduced pain and severe adverse events while not compromising blood control or cement penetration.7,9,10,16 While the use of tourniquet in TKA still remains common practice, this trend is changing. A poll conducted by the American Association of Hip and Knee Surgeons found that 88% of respondents in 2019 used tourniquet in TKA, down from 100% in 2010.3 As TKA without tourniquet grows in popularity, more clarity is needed in defining its terminology. The differences in technique all reported in this study as “tourniquetless” could create key clinical differences.
Multiple studies have analyzed the use of tourniquet only during cementation and found it to result in decreased pain, shorter functional recovery time, and a reduction in inflammatory markers compared to full tourniquet use.13,17 However, studies comparing tourniquet only during cementation to no tourniquet groups found no tourniquet to lead to lower inflammatory factor levels, shorter length of hospital stay, better range of motion, and lower postoperative pain.18,19 Additionally, multiple authors who defined tourniquetless as applying a tourniquet but keeping it deflated stated that the tourniquet acted as a safety device in the event of uncontrollable bleeding.11,20 However, awareness should be raised that this method can lead to a venous tourniquet causing increased congestion and surgical field bleeding.9 Rather, it is recommended to keep a tourniquet readily available in the operating room but not applied. This previous literature demonstrates the importance of distinguishing the three methods all considered “tourniquetless” in the studies included in this analysis.
We propose the definition of three terms to differentiate these methods. We propose the term “tourniquetless” only for cases where a tourniquet was never applied during TKA. We propose the term “tourniquet available” for all cases where a tourniquet is applied but kept deflated throughout surgery. Finally, we propose the term “tourniquet assisted” for all cases where a tourniquet is inflated during cementation only. We believe this more precise terminology offers a clear benefit in differentiating these often-conflated techniques. When describing “tourniquet assisted” surgery, it is additionally important the clinician describes the duration of tourniquet inflation and which part of the procedure is performed under the assistance of a tourniquet. In the future, this terminology could allow researchers and clinicians to better evaluate the distinct methods and draw more precise conclusions on their benefit.
We acknowledge several limitations of this study. Two large studies included in this analysis had exceptionally large sample sizes, comprising 24.2% of all patients included in the analysis.21,22 These outliers may have an undue impact on the analysis. An additional limitation of this analysis was the high number of studies not specifying how they defined tourniquetless or their methods employed to control blood loss. However, despite the high rate of studies not specifying, we believe this study still captured the entirety of methods considered tourniquetless and the rates and which recommended adjunct techniques are being employed. This study also assumed the use of tranexamic acid as a standard of care in TKA. While the use of tranexamic acid has become increasingly common, there are still variations in its use, dosing, and route of administration that should be explored in future research on tourniquetless TKA. Additional future research should better elucidate the utility of tourniquet assisted, such as inflation during cementation only, versus completely tourniquetless surgery. Finally, more research should be performed on the utility of definitive protocols for tourniquetless TKA using the recommended techniques to control blood loss. More uniformity in the use of these adjunct techniques may help maintain bloodless fields, decrease blood loss, and improve outcomes.
The reports of this review support our hypothesis that there is large diversity in the techniques considered “tourniquetless” in TKA. As tourniquetless TKA becomes more popular, greater attention needs to be paid to defining these methods and other adjunct techniques utilized. We propose the terms “tourniquetless,” “tourniquet available,” and “tourniquet assisted” to define these methods moving more precisely forward. These terms will aid appropriate analysis of studies in the literature and help guide surgeons as they transition to tourniquetless TKA and the uptake of associated techniques.
5. Conclusion
The performance of TKA without a tourniquet is gaining popularity; however, wide variation in the definition of “tourniquetless” TKA and utilization of augmented techniques to control blood loss remains. In this study, we found that “tourniquetless” had been used to define procedures where no tourniquet was applied, a tourniquet was applied but kept deflated, and a tourniquet was inflated only during cementation. Due to key clinical differences between these techniques, we propose the terms “tourniquetless,” “tourniquet available,” and “tourniquet assisted” to define these methods more precisely moving forward. The duration of tourniquet use and stage of surgery in which it was used are additional key descriptors in tourniquet assisted surgery. These terms can help better differentiate the literature, guide surgeons as they transition to tourniquetless TKA, and assist in the development of more definitive protocols for the use of adjunct techniques to control blood loss during tourniquetless TKA.
Funding/sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
DC: conceptualization, methodology, investigation, project administration, writing – review & editing WP: conceptualization, methodology, formal analysis, investigation, data curation, writing- original draft, writing – review & editing, project administration SS: conceptualization, writing – review & editing DVB: conceptualization, investigation, writing – review & editing JG: conceptualization, investigation, writing – review & editing VH: conceptualization, writing – review & editing, supervision.
Declaration of competing interest
Senior author VH declares paid consultation for Stryker, Pfizer, and Consensus, as well as roles as a voting member of the AAHKS International Committee and Editor of JBJS CME. No other authors have any financial disclosures nor declare any conflicts of interest.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2022.09.003.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Zhang W., Li N., Chen S., Tan Y., Al-Aidaros M., Chen L. The effects of a tourniquet used in total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2014 Dec 6;9(1):13. doi: 10.1186/1749-799X-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.No authors listed . 2012. Swedish Knee Arthroplasty Register Annual Report 2012. Lund, Sweden. [Google Scholar]
- 3.Abdel M.P., Berry D.J. Current practice trends in primary Hip and knee arthroplasties among members of the American association of Hip and knee surgeons: a long-term update. J Arthroplasty. 2019 Jul;34(7):S24–S27. doi: 10.1016/j.arth.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Pfitzner T., von Roth P., Voerkelius N., Mayr H., Perka C., Hube R. Influence of the tourniquet on tibial cement mantle thickness in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016 Jan 25;24(1):96–101. doi: 10.1007/s00167-014-3341-6. [DOI] [PubMed] [Google Scholar]
- 5.Alcelik I., Pollock R.D., Sukeik M., Bettany-Saltikov J., Armstrong P.M., Fismer P. A comparison of outcomes with and without a tourniquet in total knee arthroplasty. J Arthroplasty. 2012 Mar;27(3):331–340. doi: 10.1016/j.arth.2011.04.046. [DOI] [PubMed] [Google Scholar]
- 6.Smith T.O., Hing C.B. Is a tourniquet beneficial in total knee replacement surgery? Knee. 2010 Mar;17(2):141–147. doi: 10.1016/j.knee.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Farhan-Alanie M.M., Dhaif F., Trompeter A., et al. The risks associated with tourniquet use in lower limb trauma surgery: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2021 Jul 1;31(5):967–979. doi: 10.1007/s00590-021-02957-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abdel-Salam A., Eyres K. Effects of tourniquet during total knee arthroplasty. A prospective randomised study. J Bone Joint Surg Br. 1995 Mar;77-B(2):250–253. [PubMed] [Google Scholar]
- 9.Stronach B.M., Jones R.E., Meneghini R.M. Tourniquetless total knee arthroplasty: history, controversies, and technique. J Am Acad Orthop Surg. 2021;29(1):17–23. doi: 10.5435/JAAOS-D-20-00321. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed I., Chawla A., Underwood M., et al. Tourniquet use for knee replacement surgery. Cochrane Database Syst Rev. 2020 Dec 8 doi: 10.1002/14651858.CD012874.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ejaz A., Laursen A.C., Jakobsen T., Rasmussen S., Nielsen P.T., Laursen M.B. Absence of a tourniquet does not affect fixation of cemented TKA: a randomized rsa study of 70 patients. J Arthroplasty. 2015 Dec;30(12):2128–2132. doi: 10.1016/j.arth.2015.05.058. [DOI] [PubMed] [Google Scholar]
- 12.Mori N., Kimura S., Onodera T., Iwasaki N., Nakagawa I., Masuda T. Use of a pneumatic tourniquet in total knee arthroplasty increases the risk of distal deep vein thrombosis: a prospective, randomized study. Knee. 2016 Oct;23(5):887–889. doi: 10.1016/j.knee.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Cao Q., Wu Q., Liu Y., et al. Effects of tourniquet application on faster recovery after surgery and ischemia-reperfusion post–total knee arthroplasty, cementation through closure versus full-course and nontourniquet group. J Knee Surg. 2021 May 15 doi: 10.1055/s-0041-1728814. [DOI] [PubMed] [Google Scholar]
- 14.Cj V., Nagarajan M. Is cement penetration in TKR reduced by not using a tourniquet during cementation? A single blinded, randomized trial. J Orthop Surg. 2017;25(1 PG-2309499016684323) doi: 10.1177/2309499016684323. [DOI] [PubMed] [Google Scholar]
- 15.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arthur J.R., Spangehl M.J. Tourniquet use in total knee arthroplasty. J Knee Surg. 2019 Aug 1;32(8):719–729. doi: 10.1055/s-0039-1681035. [DOI] [PubMed] [Google Scholar]
- 17.Ozkunt O., Sariyilmaz K., Hc G., Dikici F. The effect of tourniquet usage on cement penetration in total knee arthroplasty: a prospective randomized study of 3 methods. Med. 2018;97(4 PG-e9668) doi: 10.1097/MD.0000000000009668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rd R., Haynes J., Hellman M., Barrack T., Barrack R. Impact of tourniquet strategy on perioperative results of modern TKA. J Knee Surg. 2020;33(10 PG-987–991):987–991. doi: 10.1055/s-0039-1688919. [DOI] [PubMed] [Google Scholar]
- 19.Yi Z., Yan L., Haibo S., et al. Effects of tourniquet use on clinical outcomes and cement penetration in TKA when tranexamic acid administrated: a randomized controlled trial. BMC Muscoskel Disord. 2021;22(1 PG-126):126. doi: 10.1186/s12891-021-03968-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu H., Liu Z., Zhang Q., Guo W. Utilization of epinephrine-soaked gauzes to address bleeding from osteotomy sites in non-tourniquet total knee arthroplasty: a retrospective cohort study. BMC Muscoskel Disord. 2020;21(1 PG-578):578. doi: 10.1186/s12891-020-03595-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mm F.-A., Lee Y., Underwood M., et al. Effect of tourniquet use on the risk of revision in total knee replacement surgery: an analysis of the National Joint Registry Data Set. BMJ Open. 2021;11(6 PG-e045353) doi: 10.1136/bmjopen-2020-045353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu H., Yang J., Xie J., et al. Tourniquet use in routine primary total knee arthroplasty is associated with a higher transfusion rate and longer postoperative length of stay: a real-world study. BMC Muscoskel Disord. 2020;21(1 PG-620):620. doi: 10.1186/s12891-020-03623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.