Abstract
Objectives
Lupus nephritis (LN) is a frequent complication of systemic lupus erythematosus (SLE). Severe (proliferative) forms of LN are treated with induction immunosuppressive therapy (IST), followed by maintenance IST, to target remission and avoid relapses. The optimal duration of maintenance IST is unknown. The WIN-Lupus trial tested whether IST discontinuation after 2‒3 years was non-inferior to IST continuation for two more years in proliferative LN.
Methods
WIN-Lupus was an investigator-initiated multicentre randomised controlled trial. Patients receiving maintenance IST with azathioprine or mycophenolate mofetil for 2–3 years, and hydroxychloroquine, were randomised (1:1) into two groups: (1) IST continuation and (2) IST discontinuation. The primary endpoint was the relapse rate of proliferative LN at 24 months. Main secondary endpoints were the rate of severe SLE flares, survival without renal relapse or severe flare, adverse events.
Results
Between 2011 and 2016, 96 patients (out of 200 planned) were randomised in WIN-Lupus: IST continuation group (n=48), IST discontinuation group (n=48). Relapse of proliferative LN occurred in 5/40 (12.5%) patients with IST continuation and in 12/44 (27.3%) patients with IST discontinuation (difference 14.8% (95% CI −1.9 to 31.5)). Non-inferiority was not demonstrated for relapse rate; time to relapse did not differ between the groups. Severe SLE flares (renal or extrarenal) were less frequent in patients with IST continuation (5/40 vs 14/44 patients; p=0.035). Adverse events did not differ between the groups.
Conclusions
Non-inferiority of maintenance IST discontinuation after 2‒3 years was not demonstrated for renal relapse. IST discontinuation was associated with a higher risk of severe SLE flares.
Trial registration number
Keywords: Lupus Nephritis; Hydroxychloroquine; Glucocorticoids; Lupus Erythematosus, Systemic; Outcome Assessment, Health Care
WHAT IS ALREADY KNOWN ON THIS TOPIC
Proliferative lupus nephritis (LN) can lead to renal failure. In patients with LN, after the induction phase of immunosuppressive therapy (IST), maintenance IST aims to prevent LN relapses. The optimal duration of maintenance IST, to reduce the risk of relapse while minimising treatment-related adverse events, is unknown.
WHAT THIS STUDY ADDS
WIN-Lupus is the first randomised controlled trial comparing maintenance IST discontinuation versus maintenance IST continuation in proliferative LN. WIN-Lupus tested the non-inferiority of maintenance IST discontinuation after 2‒3 years, compared with its continuation for two more years, in proliferative LN. Non-inferiority was not demonstrated and patients who discontinued IST had a higher risk of severe flares of lupus. However, the majority of patients who discontinued IST did not experience a flare.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE AND/OR POLICY
Instead of prolonging maintenance IST for all patients with proliferative LN, our results call for the development of tailored strategies, possibly involving repeat biopsy, to identify patients who can be safely weaned off maintenance IST.
Introduction
Lupus nephritis (LN) is a frequent and severe manifestation of systemic lupus erythematosus (SLE).1 Although the prognosis of LN has improved, substantial morbidity, partly related to treatment, is still observed.2–5 The therapeutic strategy relies on pathological classification of renal lesions.6 7 In patients with proliferative LN (class III or IV with active lesions, with or without associated class V, according to the ISN/RPS 2003),7 the treatment relies on two consecutive phases: (1) induction phase and (2) maintenance phase. The aim of induction therapy is to control renal inflammation and ideally achieve renal remission; the aim of maintenance treatment is to complete renal remission and prevent renal relapses. Gold-standard maintenance therapy is either mycophenolate mofetil or azathioprine, and progressive discontinuation of low-dose corticosteroids.6 The addition or continuation of an antimalarial drug is also required.6 Renal relapses nevertheless occur in 15‒43% of patients after 3 years,8–10 and 10%–20% of patients reach end-stage kidney disease (ESKD) after 10 years.9–11 The optimal duration of immunosuppressive therapy (IST) in proliferative LN is unknown and the possibility of discontinuing IST in patients in remission is still open to debate.3 4 12–14 While IST reduction or discontinuation before 18 months appears to be associated with a high risk of relapse,15 with subsequent organ damage, long-term continuation of IST could be associated with higher rates of adverse events such as cardiovascular events, infections and malignancy.2
No randomised controlled trial (RCT) to date has prospectively assessed the possibility of maintenance IST withdrawal in proliferative LN. The hypothesis of the WIN-Lupus trial was that discontinuation of maintenance IST after 2‒3 years in patients with proliferative LN who had been in remission for at least 1 year, and who were taking hydroxychloroquine, would be non-inferior to IST continuation for two more years in terms of renal relapse. The primary objective was to demonstrate non-inferiority of IST discontinuation in terms of renal relapse at 24 months. The main secondary objectives were to identify the risk factors for renal relapse and to demonstrate non-inferiority of IST discontinuation in terms of severe SLE flares (renal or extrarenal).
Methods
Study design and participants
WIN-Lupus was a multicentre, two parallel-arms, randomised, non-inferiority trial conducted between February 2011 and December 2018, in 28 centres in France. The study design is described in online supplemental figure 1.
annrheumdis-2022-222435supp001.pdf (1.3MB, pdf)
The following inclusion criteria were required: age ≥18 years, meeting at least 4/11 SLE classification criteria of the American College of Rheumatology (ACR),16 first flare or relapse of biopsy-proven proliferative LN (ISN/RPS 2003),7 induction treatment with high-dose corticosteroids and intravenous cyclophosphamide or mycophenolate mofetil, current maintenance IST with either azathioprine (≥50 mg/day) or mycophenolate mofetil (≥1000 mg/day or mycophenolate sodium ≥720 mg/day) for at least 2 years and a maximum of 3 years, patient in complete (proteinuria ≤0.2 g/day) or partial (proteinuria ≤0.5 g/day, or stable and considered to be related to chronic damage) renal remission, with inactive urinary sediment and normal (>90 mL/min/1.73 m²) or stable (no decrease >10%) estimated glomerular filtration rate (eGFR), as defined in the 2009 European consensus criteria,17 for the past 12 months, current treatment with hydroxychloroquine for ≥2 months, current prednisone daily dose ≤10 mg/day, effective contraception in women of childbearing age.
Subjects were excluded from the study if they had any of the following exclusion criteria: eGFR, estimated by the Modification of Diet in Renal Disease study equation, <30 mL/min/1.73 m², pregnancy, lactation, patient wishing to become pregnant in the next 2 years, recent extrarenal flare of SLE (in the past 6 months) that required an increase in corticosteroids to >20 mg/day for at least 7 days.
The trial was conducted in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonisation Guidelines for Good Clinical Practice, addendum E6. All patients gave their written informed consent before any study-related procedure. The study, which was funded by the French Ministry of Health (PHRC 2010), was registered with the Clinical Trials identifier NCT01284725.
Groups
The patients were divided into two groups: (1) IST continuation: maintenance IST was continued over the study period and (2) IST discontinuation: maintenance IST was tapered and discontinued over a 3-month period.
In both groups, hydroxychloroquine was continued and baseline low-dose corticosteroids (prednisone ≤10 mg/day) could be prescribed. Patients were followed up at 1 month (M1), 3 months (M3) and every 3 months thereafter until M24 postrandomisation, unless they were excluded earlier due to renal relapse, severe SLE flare or a severe adverse event.
Randomisation
Eligible patients were randomly assigned (1:1) to the IST continuation or IST discontinuation group. The method used for randomisation was permuted block randomisation. Randomisation was stratified on a single factor: ‘zone’. Three zones were defined: zone 1 including centres in the south of France, zone 2 including centres in the North of France, zone 3 including centres in the Paris region and the French West Indies. The study was not blinded to participants, investigators or data managers.
Outcomes
The primary efficacy outcome was the percentage of patients with relapse of proliferative LN between randomisation and M24. Renal relapse was suspected in the case of confirmed proteinuria >0.5 g/24 hours, or urinary protein/creatinine ratio (UPCR) >0.5 g/g or doubling of pre-existing proteinuria, and/or recurrence of microscopic hematuria, and/or 25% increase in serum creatinine after elimination of a functional, obstructive or toxic cause. Suspected renal relapse involved a kidney biopsy to confirm (class III or class IV LN with active lesions, with or without associated class V LN) or eliminate relapse of proliferative LN.
The key secondary efficacy outcome was the percentage of patients with a severe SLE flare (renal or extrarenal), defined by the need for induction IST (high-dose steroids≥0.5 mg/kg/day and/or induction IST), between randomisation and M24.
Additional secondary outcomes included: overall patient survival, survival without renal relapse, survival without severe SLE flare, adverse events at M24 (comprising renal adverse events defined by an elevation in serum creatinine >20%, >50%, or ESKD), extrarenal SLE activity between M0 and M24 evaluated by the SLE Disease Activity Index (SELENA-SLEDAI),18 overall exposure to corticosteroids (mean daily dose at each visit) between M0 and M24, hydroxychloroquine blood levels, health-related quality of life (QoL) (The Short Form 36 Health Survey, SF-36) and medicoeconomic impact.
Statistical analysis
WIN-Lupus was designed as a non-inferiority trial. Non-inferiority of IST discontinuation versus continuation would be concluded if the lower limit of the 95% CI for the between-group difference was <15% for the primary outcome. At a 5% significance level, 80% statistical power and a 10% lost to follow-up or exclusion, 100 patients per group were needed (total: 200). No interim analysis was planned.
Statistical significance was defined as p<0.05. The methodology was based on the extension of Consolidated Standards of Reporting Trials Statement for reporting of non-inferiority RCTs.19
For the primary outcome, the main analysis was performed on the per-protocol (PP) population and in the intention-to-treat (ITT) population.20 21 Non-inferiority would be concluded if the lower limit of the 95% CI for the between-group difference (discontinuation minus continuation) was <15% renal relapses (primary analysis) in the two sets. In the case of non-significance, superiority would be tested. Renal relapse was expressed as number and percentage for each group, and as the difference D (discontinuation minus continuation) and 95% CI. For the primary outcome, survival estimates were calculated according to the Kaplan-Meier method and compared using the log-rank test.
The secondary outcomes were compared between the two groups using the χ2 test or Fisher’s exact test for binary variables, and the Student’s t-test for continuous variables. Evolution of the SLEDAI, exposure to corticosteroids, QoL, serum creatinine and blood hydroxychloroquine levels were compared between the two groups over the 2-year follow-up period. Risk factors for relapse were assessed by univariate analysis.
A cost analysis was also performed in which total costs were estimated and compared between the two groups. Healthcare costs related to SLE and LN management were assessed: (1) maintenance IST from inclusion to the end of follow-up; (2) hydroxychloroquine and corticosteroids; and (3) inpatient care for the management of adverse events, disease progression, disease surveillance, LN relapse or severe SLE flare. Inpatient care costs were valued based on diagnosis-related groups codes (Classification Internationale des Maladies CIM-10 coding system), and using 2018 hospital activity and associated costs from the French National Reference Costs. Indirect costs (using time lost for work activity) were also investigated.
Analysis was performed using SPSS software V.20.0.
Role of the funding source
WIN-Lupus was an academic trial, designed by the scientific committee of the Groupe Coopératif sur le Lupus Rénal (GCLR) and funded by the French Ministry of Health (PHRC 2010). Data were collected by site investigators, compiled by the Clinical Research Department from the Assistance Publique-Hôpitaux de Marseille, and analysed by the department of Public Health from Aix-Marseille University. The scientific committee of the GCLR interpreted the data. All authors had access to the data and were responsible for the decision to submit the manuscript.
Results
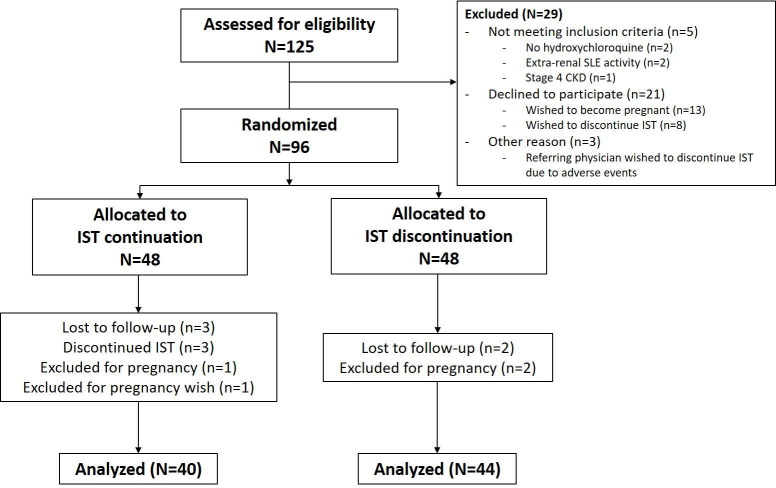
A total of 125 patients were screened (figure 1) and 96 were enrolled in the trial (intention-to-treat population): 48 in the IST continuation group and 48 in the IST discontinuation group. Inclusions were interrupted after 5 years and the expected number of inclusions was not reached. As depicted in figure 1, 12 randomised patients were excluded from the study; 84 patients completed the study protocol (per-protocol population). The baseline characteristics of these 84 patients are shown in table 1. Most patients were female (84.5%), Caucasian (63.1%), and had suffered a first flare of proliferative LN (76.2%). Most patients had received low-dose intravenous cyclophosphamide as induction therapy (59.5%) and were receiving mycophenolate mofetil as maintenance IST (78.6%). The baseline characteristics of the 96 randomised patients (intent-to-treat population) are shown in online supplemental table 1.
Figure 1.
Flow diagram of the study population. CKD, chronic kidney disease; IST, immunosuppressive therapy; SLE, systemic lupus erythematosus.
Table 1.
Baseline characteristics of the patients in the per-protocol population
| Characteristics | IST continuation (N=40) |
IST discontinuation (N=44) |
| Mean (SD) N (%) |
Mean (SD) N (%) |
|
| Age, years | 37.5 (14.0) | 36.7 (13.2) |
| Sex, female | 33 (82.5) | 38 (86.4) |
| Ethnicity | ||
| Caucasian | 27 (67.5) | 26 (59.1) |
| Black | 9 (22.5) | 14 (31.8) |
| Asian | 4 (10.0) | 4 (9.1) |
| SLE disease duration, years | 9.7 (10.2) | 7.6 (6.2) |
| Antiphospholipid syndrome | 5 (12.5) | 6 (13.6) |
| Menopause | 6/31 (19.4) | 10/38 (26.3) |
| Obesity (body mass index ≥30 kg/m2) | 5 (12.5) | 6 (13.6) |
| Systolic blood pressure, mm Hg | 121 (13) | 116 (14) |
| Diastolic blood pressure, mm Hg | 73 (11) | 73 (10) |
| First flare of proliferative LN | 32 (80.0) | 32 (72.7) |
| Induction therapy | ||
| Low-dose intravenous cyclophosphamide | 26 (65.0) | 24 (54.5) |
| Mycophenolate mofetil | 14 (35.0) | 20 (45.5) |
| Maintenance IST | ||
| Duration, years | 2.8 (0.9) | 2.8 (0.8) |
| Mycophenolate mofetil | 30 (75.0) | 36 (81.8) |
| Azathioprine | 10 (25.0) | 8 (18.2) |
| Doses prescribed (mg/day) | ||
| Mycophenolate mofetil | 1633 (571) | 1364 (684) |
| Azathioprine | 82.5 (29) | 81.2 (39) |
| Corticosteroids | 4.3 (2.8) | 4.3 (2.8) |
| Hydroxychloroquine | 365 (89) | 334 (131) |
| Hydroxychloroquine serum level, ng/L | 861 (714) | 644 (428) |
| Serum creatinine, µmol/L | 67.7 (14.7) | 72.7 (17.2) |
| Estimated GFR, mL/min/1.73 m² | 101.6 (28.0) | 94.9 (25.8) |
| Urinary protein/creatinine ratio, g/g | 0.28 (0.38) | 0.21 (0.28) |
| Urinary protein/creatinine ratio ≤0.2 g/g | 26 (65.0) | 29 (65.9) |
| Urinary protein/creatinine ratio ≤0.5 g/g | 34 (85.0) | 42 (95.5) |
| Urinary protein/creatinine ratio ≤0.7 g/g | 35 (87.5) | 43 (97.7) |
| Serum albumin, g/dL | 4.2 (0.5) | 4.2 (0.5) |
| Haemoglobin, g/L | 1.30 (0.18) | 1.29 (0.13) |
| Leucocytes, G/L | 5.71 (1.7) | 5.58 (2.4) |
| Lymphocytes, G/L | 1.5 (0.7) | 1.39 (0.6) |
| Platelets, G/L | 255 (89) | 240 (79) |
| Low C3 | 5/38 (13.2) | 5/42 (11.9) |
| Low C4 | 4/38 (10.5) | 4/42 (9.5) |
| Positive anti-dsDNA | 24/38 (63.2) | 24/44 (54.5) |
| SLEDAI score | 2.2 (1.7) | 1.6 (1.8) |
Data are expressed as mean (SD), number (%) or number/number available (%).
GFR, glomerular filtration rate; IST, immunosuppressive therapy; LN, lupus nephritis; SLE, systemic lupus erythematosus; SLEDAI, SLE Disease Activity Index.
Primary outcome
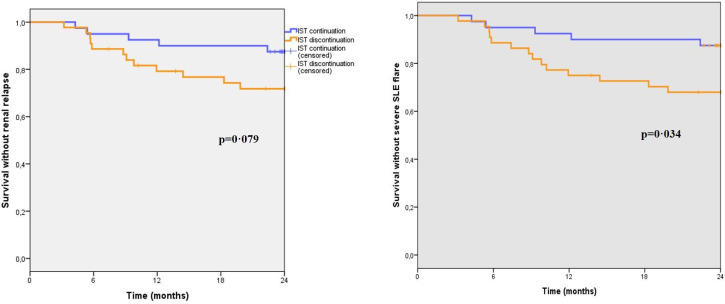
Relapse of proliferative LN occurred in 5/40 (12.5%) patients from the IST continuation group and in 12/44 (27.3%) patients from the IST discontinuation group (p=0.710, D (95% CI): 14.8 (−1.9 to 31.5)) in the PP set and the ITT set. Non-inferiority of IST discontinuation was not demonstrated. IST continuation was not significantly superior to discontinuation in terms of relapse of proliferative LN (p=0.092). Relapses occurred after a median of 9 months (IQR: 5‒17) in patients with IST continuation and 9 months (IQR: 7‒14) in patients with IST discontinuation. Time to renal flare, compared by Kaplan-Meier survival curves (log rank test), did not differ between the groups (p=0.079) (figure 2A). The baseline individual characteristics of the 17 patients who relapsed, as well as renal presentation and pathology at the time of LN relapse, are presented in online supplemental table 2.
Figure 2.
Survival analyses. (A) Survival without renal relapse. (B) Survival without severe SLE flare (online supplemental material). IST, immunosuppressive therapy; SLE, systemic lupus erythematosus.
Secondary outcomes
There were significantly more severe SLE flares in patients in the IST discontinuation group compared with the IST continuation group (14/44 (31.8%) vs 5/40 (12.5%) patients, p=0.035, D (95% CI) 19.3% (CI 1.3% to 35.7%)), and time to severe SLE flares was shorter in patients in the IST discontinuation group (log rank test, p=0.034) (figure 2B).
The adverse events in the 96 randomised patients are shown in table 2. There was no significant difference between the groups.
Table 2.
Adverse events
| IST continuation (N=48) |
IST discontinuation (N=48) |
All patients (N=96) |
||
| Death | 0 | 0 | 0 | |
| Renal adverse events | 14 | 18 | 32 | |
| Serum creatinine +20% | 14 | 16 | 30 | |
| Serum creatinine +50% | 0 | 2 | 2 | |
| End-stage kidney disease | 0 | 0 | 0 | |
| Infections | 19 | 14 | 33 | |
| Severe | 1 | 3 | 4 | |
| Appendicitis | 0 | 1 | 1 | |
| Malaria | 0 | 1 | 1 | |
| Zoster | 1 | 1 | 2 | |
| Other | 18 | 11 | 29 | |
| Lower urinary tract | 6 | 4 | 10 | |
| Upper respiratory tract | 4 | 4 | 8 | |
| Ear, nose, and throat | 2 | 1 | 3 | |
| Erysipelas | 1 | 1 | 2 | |
| Dermatomycosis | 2 | 0 | 2 | |
| Cervical human papillomavirus | 2 | 1 | 3 | |
| Warts | 1 | 0 | 1 | |
| Haematological | 41 | 48 | 89 | |
| Myelodysplastic syndrome | 1 | 0 | 1 | |
| Hypereosinophilia | 1 | 0 | 1 | |
| Haematoma | 0 | 1 | 1 | |
| Anaemia with Hb <10 g/dL | 5 | 2 | 7 | |
| Anaemia with Hb <8 g/dL | 1 | 0 | 1 | |
| Leucopenia <4 G/L | 16 | 17 | 33 | |
| Leucopenia <3 G/L | 0 | 4 | 4 | |
| Neutropenia <1.5 G/L | 3 | 7 | 10 | |
| Neutropenia <1 G/L | 0 | 1 | 1 | |
| Lymphopenia <1 G/L | 12 | 16 | 28 | |
| Lymphopenia <0.5 G/L | 1 | 0 | 1 | |
| Thrombopenia <100 G/L | 1 | 0 | 1 | |
| Other | 3 | 6 | 9 | |
| Cataract | 1 | 1 | 2 | |
| Alopecia | 0 | 2 | 2 | |
| Rash unrelated to SLE | 1 | 0 | 1 | |
| New-onset hypertension | 1 | 0 | 1 | |
| Obstructive sleep apnoea | 0 | 1 | 1 | |
| Unexplained chest pain | 0 | 1 | 1 | |
| Unexplained transient dyspnoea | 0 | 1 | 1 | |
Hb, haemoglobin; IST, immunosuppressive therapy; SLE, systemic lupus erythematosus.
The evolution over time of several clinical (SLEDAI, dose of corticosteroids, SF-36 mental and physical component summaries) and biological (UPCR, serum creatinine, blood hydroxychloroquine levels) parameters through the study period are shown in online supplemental figure 2. Extrarenal SLE activity, evaluated by the SLEDAI and exposure to corticosteroids, did not differ between the two groups.
IST discontinuation was less costly than IST continuation in terms of maintenance therapy (−83%; p<0.001), but more costly in terms of inpatient care (+61%, p=0.027) (online supplemental table 3). No difference was found in indirect costs. Overall, patients from the IST discontinuation group had lower costs compared with the IST continuation group (−40%; p=0.001).
Risk factors for proliferative ln relapse
The risk factors for proliferative LN relapse (univariate analysis) are shown in table 3. Antiphospholipid syndrome, higher UPCR at baseline, low C3 and higher SLEDAI at inclusion were associated with LN relapse. Higher eGFR, lower serum albumin, lower haemoglobin level and lower leucocyte, lymphocyte, and eosinophil counts were also associated with LN relapse.
Table 3.
Risk factors for renal relapse at inclusion (per-protocol population)
| Relapse (N=17) |
No relapse (N=67) |
P value | |
| Mean (SD) N (%) |
Mean (SD) N (%) |
||
| Age, years | 32.4 (11.7) | 38.3 (13.8) | 0.111 |
| Sex, female | 17 (100.0) | 54 (80.6) | 0.061 |
| Ethnicity | 0.395 | ||
| Caucasian | 9 (52.9) | 44 (65.7) | – |
| Black | 5 (29.4) | 18 (26.9) | – |
| Asian | 3 (17.6) | 5 (7.5) | – |
| SLE disease duration, years | 8.1 (5.9) | 8.7 (8.9) | 0.764 |
| Antiphospholipid syndrome | 5 (29.4) | 6 (9.0) | 0.041 |
| Menopause | 1 (5.9) | 15/52 (28.8) | 0.094 |
| Obesity | 2 (11.8) | 9 (13.4) | 1.00 |
| First flare of proliferative LN | 12 (70.6) | 52 (77.6) | 0.537 |
| Induction therapy with: | 0.947 | ||
| Intravenous cyclophosphamide | 10 (58.8) | 40 (59.7) | |
| Mycophenolate mofetil | 7 (41.2) | 27 (40.3) | |
| Maintenance IST duration at M0, years | 2.6 (1.0) | 2.9 (0.7) | 0.231 |
| Maintenance IST | 0.753 | ||
| Mycophenolate mofetil | 13 (76.5) | 53 (79.1) | – |
| Azathioprine | 4 (23.5) | 14 (20.9) | – |
| Doses prescribed at M0, mg/day | |||
| Mycophenolate mofetil | 1500.0 (277.3) | 1510.2 (639.3) | 0.956 |
| Azathioprine | 75.0 (28.9) | 82.7 (35.9) | 0.676 |
| Corticosteroids | 4.8 (3.3) | 4.1 (2.6) | 0.436 |
| Hydroxychloroquine | 332 (142) | 354 (105) | 0.455 |
| Serum hydroxychloroquine level, ng/L | 787 (494) | 722 (598) | 0.464 |
| Serum hydroxychloroquine level <200 ng/L | 2/15 (13.3) | 12/53 (22.6) | 0.719 |
| Serum creatinine, µmol/L | 63.8 (10.4) | 71.9 (17.0) | 0.052 |
| Estimated GFR, mL/min/1.73 m² | 107.2 (24.0) | 95.8 (27.3) | 0.046 |
| Chronic kidney disease stage | 0.134 | ||
| Stage 1 | 14 (82.4) | 38 (56.7) | – |
| Stage 2 | 2 (11.8) | 24 (35.8) | – |
| Stage 3 | 1 (5.9) | 5 (7.5) | – |
| Urinary protein/creatinine ratio, g/g | 0.548 (0.550) | 0.169 (0.187) | 0.001 |
| Urinary protein/creatinine ratio ≤0.2 g/g | 5 (29.4%) | 50 (74.6%) | <0.001 |
| Urinary protein/creatinine ratio ≤0.5 g/g | 12 (70.6) | 64 (95.5) | 0.007 |
| Urinary protein/creatinine ratio ≤0.7 g/g | 12 (70.6) | 66 (98.5) | 0.001 |
| Serum albumin, g/dL | 3.9 (0.4) | 4.3 (0.4) | 0.004 |
| Haemoglobin level, g/L | 1.19 (0.14) | 1.32 (0.14) | 0.003 |
| Leucocyte count, g/L | 4.8 (2.4) | 5.8 (1.9) | 0.011 |
| Neutrophil count, g/L | 3.3 (2.4) | 3.8 (1.9) | 0.204 |
| Lymphocyte count, g/L | 1.0 (0.4) | 1.5 (0.6) | 0.003 |
| Basophil count, g/L | 0.01 (0.01) | 0.02 (0.02) | 0.128 |
| Eosinophil count, g/L | 0.04 (0.04) | 0.10 (0.14) | 0.049 |
| Platelet count, g/L | 289 (130) | 237 (65) | 0.109 |
| Low C3 | 6/16 (37.5) | 4/64 (6.3) | 0.003 |
| Low C4 | 3/16 (18.8) | 4/64 (7.8) | 0.194 |
| Positive anti-dsDNA | 13 (76.5) | 36 (53.8) | 0.092 |
| SLEDAI score | 3.1 (2.6) | 1.6 (1.4) | 0.025 |
Data are expressed as % or mean (SD). In the case of missing data, the number/number available (%) is indicated.
GFR, glomerular filtration rate; IST, immunosuppressive therapy; LN, lupus nephritis; SLE, systemic lupus erythematosus; SLEDAI, SLE Disease Activity Index.
The risk factors for severe SLE flares (univariate analysis) are shown in online supplemental table 4.
The risk factors for LN relapse among patients in the IST discontinuation group are shown in online supplemental table 5. The risk factors for severe SLE flares among patients in the IST discontinuation group are shown in online supplemental table 6.
Discussion
In this multicentre RCT, non-inferiority of IST discontinuation after 2‒3 years was not demonstrated, although IST continuation was not significantly superior regarding LN relapse. IST discontinuation was associated with a higher risk of severe SLE flares (renal or extrarenal) requiring induction IST. No patient developed kidney failure and only two patients, with IST discontinuation, experienced an increase in serum creatinine ≥50%. Health-related costs were lower in the IST discontinuation group. Exposure to corticosteroids and adverse events did not differ between the groups.
In patients with proliferative LN, the possibility of discontinuation of maintenance IST, and the optimal timing for this discontinuation, is poorly defined. In a national survey conducted in France in 2012 among LN specialists,22 40% stated that they continued maintenance IST for 2 years in patients who were stable in remission, 25% continued for 3 years, 25% for 4‒5 years and 9% for >5 years. Different expert recommendations on the treatment of proliferative LN were published in 2012.23 While the European Alliance of Associations for Rheumatology (EULAR)/ERA-EDTA24 recommended to continue maintenance IST for at least 3 years after induction therapy, the Kidney Disease Improving Global Outcome (KDIGO)25 proposed to continue maintenance IST for at least 1 year after clinical remission before considering tapering, and the ACR26 highlighted the need for evidence-based data to determine the optimal duration of maintenance IST. A recent update of the EULAR/ERA-EDTA recommendations proposed the gradual withdrawal of treatment (corticosteroids first, then immunosuppressive drugs) after at least 3‒5 years in patients with a complete clinical response (grade 2b/C recommendation).6 Similarly, the KDIGO 2021 update proposed a minimum of 3 years of IST.27
Moroni et al 28 tested the discontinuation of IST and corticosteroids in 73 patients with LN who had achieved a stable clinical remission. A flare requiring treatment reinforcement was observed in 21 (29%) patients during treatment tapering, which is consistent with the 25% rate of renal relapse (and 32% of overall severe relapse) observed here in patients with IST discontinuation. Zen et al recently reported the outcomes of 83 patients in remission after LN, for whom IST was discontinued after a mean of 3.8 years.29 After a mean follow-up of 9.7 years, 8 (10%) patients had an LN relapse and 19 (23%) patients experienced a flare of SLE. Younger age at IST discontinuation and the absence of HCQ prescription were associated with LN flares. This risk of relapse should be considered against the high proportion of patients who were weaned from IST without relapse.
Rather than generalising long-term continuation of maintenance IST to prevent relapses, the challenge consists of identifying patients who can safely be weaned from IST. Here, SLEDAI at inclusion, C3 consumption and lower lymphocyte count were predictive of renal relapse and of severe SLE flare. Other biological parameters, possibly associated with residual inflammation (lower serum albumin, lower haemoglobin), were also predictive of relapse and severe SLE flares. Higher eGFR was also a risk factor for relapse, which is of interest as SLE disease activity may decrease as kidney function declines.30 Different thresholds (0.2, 0.5 or 0.7 g/g), routinely used in clinical trials to define LN complete remission or response, were predictive of risk of relapse. Proteinuria in patients with a previous flare of LN can result from persistent active lesions, or from chronic glomerular damage. No repeat kidney biopsy was warranted in WIN-Lupus to ascertain histological remission, and patients with higher initial UPCR may have presented ongoing histological activity. Of note, histological activity can be observed even in patients with complete clinical remission,31 32 and the performance of a repeat kidney biopsy to confirm histological remission before IST weaning could become a new standard.
de Rosa et al 31 suggested that repeat biopsy could allow the selection of patients with pathological remission for IST discontinuation. Malvar et al 33 proposed a kidney biopsy-based management of maintenance IST for proliferative LN. Among 69 patients with histological remission and IST discontinuation, only 7 (10%) experienced a renal relapse.
The main motivation for IST discontinuation is to limit the burden of adverse events related to immunosuppression. Here, we evaluated the discontinuation of maintenance IST (mycophenolate mofetil or azathioprine), but all patients were on hydroxychloroquine, and low-dose corticosteroids could be prescribed. The reason we permitted the continuation of low-dose corticosteroids in this trial was to allow flexibility in controlling the extrarenal manifestations of lupus. Indeed, in a national survey,22 55% of physicians managing patients with LN reported continuing low-dose corticosteroids in maintenance. WIN-Lupus was not a trial of complete treatment withdrawal, as reported in recent cohort studies.4 One of the possible reasons for clinicians to maintain IST is to prevent the need for corticosteroid use or increase,34 which is itself associated with significant damage.35 36 Here, the overall exposure to corticosteroids did not differ between the groups, indicating that IST discontinuation did not lead to a compensatory increase in corticosteroid dose for lupus containment. Blood levels of hydroxychloroquine were not associated with renal relapses or severe flares in this cohort, but only a minority of patients had low blood levels of hydroxychloroquine. In the present trial, the absence of a difference in adverse events between the groups could be related to the relatively short follow-up, which does not allow us to conclude on the absence of benefit of treatment withdrawal long term.
From an economic perspective, IST discontinuation was associated with cost savings due to lower maintenance therapy costs, while inpatient costs increased due to relapse care.
This study has several limitations. First, we did not reach the 200 inclusions that were expected, and the scientific committee decided to end patient recruitment after 5 years due to the slow inclusion rate (mainly related to the strict inclusion criteria, and to the exclusion of patients wishing to become pregnant within 2 years). The trial is thus underpowered, and superiority of treatment continuation could have been demonstrated with more patients. Second, block randomisation was applied to limit allocation bias, but only randomisation zone was used for stratification. Other clinically relevant factors could have been taken into account, such as induction and maintenance therapies, or initial doses of corticosteroids. Yet, these factors were well balanced between groups. Third, it was an open label and not double-blinded trial, due to budget constraints. Yet, the primary endpoint was strictly defined and documented by kidney biopsy. Fourth, we did not select patients with appropriate adherence to treatment, but rather chose real-life patients, who were prescribed an antimalarial and mycophenolate mofetil or azathioprine, which they declared they were taking. In addition, low-dose corticosteroids was defined as a daily dose of ≤10 mg/day and not as a daily dose of <7.5 mg/day. Moreover, LN relapses can occur several years after IST discontinuation28 and late relapses were not captured by this study. A 2-year follow-up may also have been too short to determine the impact of IST continuation or discontinuation on long-term kidney function. Finally, selection bias is possible, as investigators may have refrained from including patients who had previously relapsed (small proportion of patients with a previous history of relapse), or those who were in complete remission and were willing to discontinue IST.
This study also has strengths. WIN-Lupus is the first RCT to compare maintenance IST continuation with IST discontinuation in patients with proliferative LN. The patients included were homogeneous in terms of organ involvement (biopsy-proven proliferative LN), duration of maintenance IST (2‒3 years), duration of remission (≥1 year) and all patients were prescribed hydroxychloroquine. Second, although patients were included over several years, the gold-standard therapeutic strategy for proliferative LN remained the same during the study period.
To conclude, non-inferiority of maintenance IST discontinuation after 2‒3 years was not demonstrated for renal relapses in patients with proliferative LN. IST discontinuation was associated with a higher risk of severe SLE flares. Nonetheless, a majority of patients did not relapse at 2 years after IST discontinuation. The most important challenge remains the identification and selection of patients who can be safely weaned from IST.
Acknowledgments
We thank all members of the Groupe Coopératif sur le Lupus Rénal (GCLR) who participated in the conception of the study, in particular Professor Jacques Pourrat and Professor Bruno Moulin. We are grateful to Elisabeth Castanier, Sophie Tardoski and Julien Faraut for their help in the conduct of this research and data acquisition. We thank the Direction de la Recherche Santé from AP-HM, especially Patrick Sudour for his help in the conception and conduct of this trial, and Richard Malkoun for data management. The authors thank Newmed Publishing Ltd. for providing English editing services.
Footnotes
Handling editor: Josef S Smolen
Twitter: @NJourde, @michelinepha
Contributors: NJ-C, KB, ZA and ED designed the study. NC-C, LB, SB, VC, LCh, LCo, CD, BD, SF, PG, GG, AHua, AHum, EK, AK, ML, VLG, LL, HM-L, FM, MP, VQ, PR, FS-R, DV, EH, ZA and ED included patients in the trial, revised the manuscript, and provided additional data for the revised version of the manuscript. LD supervised interpretation of kidney biopsy results. NJ-C, KB, AL and SL analysed the data, KB and AL performed the statistical analyses, SL did the medicoeconomic analyses. NJ-C wrote the draft of the manuscript. NJ-C, NC-C, KB, EH and ED revised the manuscript. All authors read the final manuscript and gave their consent for publication. Non-author contribution: Professor Jacques Pourrat and Professor Bruno Moulin participated in the initial phase of study design. Elisabeth Castanier, Sophie Tardoski and Julien Faraut collected data. Patrick Sudour supervised the conduct of the study and monitored data collection. Richard Malkoun was the data manager of the study. NJ-C is responsible for the overall content as guarantor. She accepts full responsibility for the finished work and the conduct of the study, had access to the data and controlled the decision to publish.
Funding: The trial was funded by the French Ministry of Health (PHRC 2010-24-13).
Competing interests: NJ-C reports receiving non-financial support from Sanofi-Genzyme and Vifor; speaking and consulting fees from Vifor and Otsuka; research grant from Fresenius Medical Care; outside the submitted work. NC-C reports research grant from Roche; outside the submitted work. LB reports speaking fees from GSK, Novartis, Biocryst, Takeda, Behring and Blueprint; research grants from Takeda, GSK, Sanofi, Biocryst, Novartis; outside the submitted work. LCh reports speaking fees from BMS and non-financial support from AstraZeneca; outside the submitted work. LCo reports speaking fees from Astellas, Chiesi, Novartis, Sandoz, Otsuka, GSK, Biotest; consultancy fees from Biotest, Hansa, Novartis; research grants from Novartis, Astellas; travel funding from Astellas, Chiesi, Novartis, Sandoz, Vifor; outside the submitted work. LD reports speaking fees from AstraZeneca and Janssen. BD reports speaking fees from Genzyme and Novonordisk; consultancy fees from Amicus; research grant from Shire; outside the submitted work. SF reports speaking fees from Asahi, Vifor and Sanofi; consultancy fees from Abyonyx Pharma; outside the submitted work. GG reports speaking fees from Genzyme, Pfizer and Novartis; non-financial support from Novartis, Amgen, Addmedicca, Lilly, Abbvie, Amicus therapeutics, Shire, Pfizer and LFB medicaments; outside the submitted work. AH reports speaking fees from Janssen and Pfizer; outside the submitted work. AK reports speaking fees from Vifor, GSK, AstraZeneca, Roche; consultancy fees from Novartis, GSK, Bohringer-Ingelheim; non-financial support from Vifor, Sanofi and Alexion; outside the submitted work. ML reports speaking fees from Chugai-Roche, Bayer, Pfizer, Leopharma; grant from Chugai-Roche; outside the submitted work. VQ reports consultancy fees from Boehringer Ingelheim and GSK; outside the submitted work. EH reports consulting fees from Johnson&Johnson, Boehringer Ingelheim, Bayer, GSK, Roche-Chugai, Sanofi-Genzyme; speaking fees from Johnson&Johnson, GSK, Roche-Chugai; research grants from CSL Behring, Johnson&Johnson, GSK, Roche-Chugai; outside the submitted work. ZA reports speaking and consultancy fees from GSK. ED reports speaking fees from GSK, Amgen, AstraZeneca; consultancy fees from GSK, AstraZeneca, Amgen; research grant from Roche; outside the submitted work.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Comite de Protection des Personnes Sud-Mediterranee IID-RCB 2010-022859-30. Participants gave informed consent to participate in the study before taking part.
References
- 1. Cameron JS. Lupus nephritis. J Am Soc Nephrol 1999;10:413–24. 10.1681/ASN.V102413 [DOI] [PubMed] [Google Scholar]
- 2. Arnaud L, Tektonidou MG. Long-Term outcomes in systemic lupus erythematosus: trends over time and major contributors. Rheumatology 2020;59:v29–38. 10.1093/rheumatology/keaa382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dörner T, Furie R. Novel paradigms in systemic lupus erythematosus. Lancet 2019;393:2344–58. 10.1016/S0140-6736(19)30546-X [DOI] [PubMed] [Google Scholar]
- 4. Moroni G, Frontini G, Ponticelli C. When and how is it possible to stop therapy in patients with lupus nephritis? Clin J Am Soc Nephrol 2021. 10.2215/CJN.04830421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lightstone L, Doria A, Wilson H, et al. Can we manage lupus nephritis without chronic corticosteroids administration? Autoimmun Rev 2018;17:4–10. 10.1016/j.autrev.2017.11.002 [DOI] [PubMed] [Google Scholar]
- 6. Fanouriakis A, Kostopoulou M, Cheema K, et al. 2019 update of the joint European League against rheumatism and European renal Association-European dialysis and transplant association (EULAR/ERA-EDTA) recommendations for the management of lupus nephritis. Ann Rheum Dis 2020;79:713–23. 10.1136/annrheumdis-2020-216924 [DOI] [PubMed] [Google Scholar]
- 7. Weening JJ, D'Agati VD, Schwartz MM, et al. The classification of glomerulonephritis in systemic lupus erythematosus revisited. Kidney Int 2004;65:521–30. 10.1111/j.1523-1755.2004.00443.x [DOI] [PubMed] [Google Scholar]
- 8. Houssiau FA, Vasconcelos C, D'Cruz D, et al. Immunosuppressive therapy in lupus nephritis: the Euro-Lupus nephritis trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum 2002;46:2121–31. 10.1002/art.10461 [DOI] [PubMed] [Google Scholar]
- 9. Houssiau FA, D'Cruz D, Sangle S, et al. Azathioprine versus mycophenolate mofetil for long-term immunosuppression in lupus nephritis: results from the maintain nephritis trial. Ann Rheum Dis 2010;69:2083–9. 10.1136/ard.2010.131995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dooley MA, Jayne D, Ginzler EM, et al. Mycophenolate versus azathioprine as maintenance therapy for lupus nephritis. N Engl J Med 2011;365:1886–95. 10.1056/NEJMoa1014460 [DOI] [PubMed] [Google Scholar]
- 11. Hanly JG, O'Keeffe AG, Su L, et al. The frequency and outcome of lupus nephritis: results from an international inception cohort study. Rheumatology 2016;55:252–62. 10.1093/rheumatology/kev311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moroni G, Gatto M, Raffiotta F, et al. Can we withdraw immunosuppressants in patients with lupus nephritis in remission? an expert debate. Autoimmun Rev 2018;17:11–18. 10.1016/j.autrev.2017.11.003 [DOI] [PubMed] [Google Scholar]
- 13. Grootscholten C, Berden JHM. Discontinuation of immunosuppression in proliferative lupus nephritis: is it possible? Nephrol Dial Transplant 2006;21:1465–9. 10.1093/ndt/gfl208 [DOI] [PubMed] [Google Scholar]
- 14. van Vollenhoven RF, Mosca M, Bertsias G, et al. Treat-to-target in systemic lupus erythematosus: recommendations from an international Task force. Ann Rheum Dis 2014;73:958–67. 10.1136/annrheumdis-2013-205139 [DOI] [PubMed] [Google Scholar]
- 15. Laskari K, Tzioufas AG, Antoniou A, et al. Longterm followup after tapering mycophenolate mofetil during maintenance treatment for proliferative lupus nephritis. J Rheumatol 2011;38:1304–8. 10.3899/jrheum.101249 [DOI] [PubMed] [Google Scholar]
- 16. Hochberg MC. Updating the American College of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1997;40:40. 10.1002/art.1780400928 [DOI] [PubMed] [Google Scholar]
- 17. Gordon C, Jayne D, Pusey C, et al. European consensus statement on the terminology used in the management of lupus glomerulonephritis. Lupus 2009;18:257–63. 10.1177/0961203308100481 [DOI] [PubMed] [Google Scholar]
- 18. Petri M, Kim MY, Kalunian KC, et al. Combined oral contraceptives in women with systemic lupus erythematosus. N Engl J Med 2005;353:2550–8. 10.1056/NEJMoa051135 [DOI] [PubMed] [Google Scholar]
- 19. Piaggio G, Elbourne DR, Pocock SJ, et al. Reporting of noninferiority and equivalence randomized trials: extension of the CONSORT 2010 statement. JAMA 2012;308:2594–604. 10.1001/jama.2012.87802 [DOI] [PubMed] [Google Scholar]
- 20. D'Agostino RB, Massaro JM, Sullivan LM. Non-inferiority trials: design concepts and issues - the encounters of academic consultants in statistics. Stat Med 2003;22:169–86. 10.1002/sim.1425 [DOI] [PubMed] [Google Scholar]
- 21. Mo Y, Lim C, Watson JA, et al. Non-adherence in non-inferiority trials: pitfalls and recommendations. BMJ 2020;370:m2215. 10.1136/bmj.m2215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jourde-Chiche N, Chiche L, Mancini J, et al. [Proliferative lupus nephritis treatment: practice survey in nephrology and internal medicine in France]. Nephrol Ther 2014;10:170–6. 10.1016/j.nephro.2013.11.006 [DOI] [PubMed] [Google Scholar]
- 23. Wilhelmus S, Bajema IM, Bertsias GK, et al. Lupus nephritis management guidelines compared. Nephrol Dial Transplant 2016;31:904–13. 10.1093/ndt/gfv102 [DOI] [PubMed] [Google Scholar]
- 24. Bertsias GK, Tektonidou M, Amoura Z, et al. Joint European League against rheumatism and European renal Association-European dialysis and transplant association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis. Ann Rheum Dis 2012;71:1771–82. 10.1136/annrheumdis-2012-201940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group . KDIGO clinical practice guideline for glomerulonephritis. Kidney Int Suppl 2012;2:139–274. [Google Scholar]
- 26. Hahn BH, McMahon MA, Wilkinson A, et al. American College of rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res 2012;64:797–808. 10.1002/acr.21664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rovin BH, Caster DJ, Cattran DC, et al. Management and treatment of glomerular diseases (Part 2): conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Kidney Int 2019;95:281–95. 10.1016/j.kint.2018.11.008 [DOI] [PubMed] [Google Scholar]
- 28. Moroni G, Longhi S, Giglio E, et al. What happens after complete withdrawal of therapy in patients with lupus nephritis. Clin Exp Rheumatol 2013;31:S75–81. [PubMed] [Google Scholar]
- 29. Zen M, Fuzzi E, Loredo Martinez M. Immunosuppressive therapy withdrawal after remission achievement in patients with lupus nephritis. Rheumatology 2021:keab373. [DOI] [PubMed] [Google Scholar]
- 30. Nossent HC, Swaak TJ, Berden JH. Systemic lupus erythematosus: analysis of disease activity in 55 patients with end-stage renal failure treated with hemodialysis or continuous ambulatory peritoneal dialysis. Dutch Working Party on SLE. Am J Med 1990;89:169–74. 10.1016/0002-9343(90)90295-O [DOI] [PubMed] [Google Scholar]
- 31. De Rosa M, Azzato F, Toblli JE, et al. A prospective observational cohort study highlights kidney biopsy findings of lupus nephritis patients in remission who flare following withdrawal of maintenance therapy. Kidney Int 2018;94:788–94. 10.1016/j.kint.2018.05.021 [DOI] [PubMed] [Google Scholar]
- 32. Malvar A, Pirruccio P, Alberton V, et al. Histologic versus clinical remission in proliferative lupus nephritis. Nephrol Dial Transplant 2017;32:1338–44. 10.1093/ndt/gfv296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Malvar A, Alberton V, Lococo B, et al. Kidney biopsy-based management of maintenance immunosuppression is safe and may ameliorate flare rate in lupus nephritis. Kidney Int 2020;97:156–62. 10.1016/j.kint.2019.07.018 [DOI] [PubMed] [Google Scholar]
- 34. Ngamjanyaporn P, McCarthy EM, Sergeant JC, et al. Clinicians approaches to management of background treatment in patients with SLE in clinical remission: results of an international observational survey. Lupus Sci Med 2017;4:e000173. 10.1136/lupus-2016-000173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Thamer M, Hernán MA, Zhang Y, et al. Prednisone, lupus activity, and permanent organ damage. J Rheumatol 2009;36:560–4. 10.3899/jrheum.080828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Petri M, Bechtel B, Dennis G, et al. Burden of corticosteroid use in patients with systemic lupus erythematosus: results from a Delphi panel. Lupus 2014;23:1006–13. 10.1177/0961203314532699 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
annrheumdis-2022-222435supp001.pdf (1.3MB, pdf)
Data Availability Statement
Data are available on reasonable request.