Abstract
Hydrocephalus is a very common brain disorder affecting both children and adult populations. Its global burden has been well documented in the literature, and its management is not without challenges and complications, especially in low-income countries. This study aims at reviewing the management of hydrocephalus in a tertiary hospital in Nigeria and illustrating two cases managed with peculiar challenges. This study is a retrospective clinical review of 170 patients with hydrocephalus amenable to ventriculoperitoneal shunting as primary treatment. Two cases of hydrocephalus with peculiar management challenges were illustrated. The first case was that of an abandoned infant with hydrocephalus. The second case was that of a 5-year-old boy with post-meningitic hydrocephalus with delays in having cerebrospinal fluid (CSF) shunting. Majority of the patients with hydrocephalus were infants (71.2%), and the top two most common etiologies were aqueductal stenosis (64.7%) and post-meningitic hydrocephalus (11.2%), respectively. Shunt infection was the most common complication (9.4%), which was within the lower limit of rates reported in the literature (8.6%–50%). Approximately 84% of shunting had no complication. In conclusion, ventriculoperitoneal shunting is the preferred treatment option for hydrocephalus in low-income countries, and it is not without management challenges that are peculiar to these climes. Shunt infection appeared to be the most common complication.
Keywords: Challenges, hydrocephalus, low-income country, ventriculoperitoneal shunt
Introduction
Hydrocephalus is a common brain disorder of childhood and is one of the most common conditions treated by neurosurgeons worldwide. It is seen in both pediatric and adult populations. Treatment of uncomplicated hydrocephalus consists of cerebrospinal fluid (CSF) diversion by means of a shunt or endoscopic third ventriculostomy.[1]
The first shunt surgery was performed over a century ago, and since then, ventriculoperitoneal (VP) shunt has remained a mainstream treatment method for hydrocephalus.[2] Although there has been increasing interest in performing an endoscopic third ventriculostomy for selected cases of hydrocephalus, VP shunt appears to be a preferred treatment option in low-income countries.[2,3]
In low-income countries, limitations with appropriate radiological investigations have been reported to contribute to the burden of hydrocephalus management.[1] Other associated challenges may include delayed prenatal diagnosis, perinatal and maternal morbidity, shunt complications, child neglect, malnutrition and abandonment, economic burden, and sociocultural beliefs. These add to the disease burden and possible complications of treatment. Children with VP shunts, when compared with children admitted to other hospital services, require a disproportionately higher share of health resources for acute and longitudinal management. Delayed access to neurosurgical care has also been implicated with more shunt complications and increased mortality.[4]
Late presentation and delayed shunting have also been reported to be responsible for poorer outcomes, as early features of hydrocephalus are being ignored or misunderstood. Late presentation has also been attributed to social taboos and socioeconomic conditions.[5,6] Better outcomes have been reported in patients who were shunted earlier than those who underwent late shunt surgery.[7,8,9]
The paucity of neurosurgeon trainers, limited accredited training centers, and high rate of brain-drain of neurosurgery trainees and trainers to developed countries has also limited neurosurgical care.[10]
Knowing the scope of these challenges is essential to any systematic, multi-regional, or public health initiative, aimed at ameliorating these challenges in hydrocephalus.
Patients and Methods
A retrospective study of patients of cases with hydrocephalus managed in our neurosurgery service between July 2000 to June 2021. Patients with other intracranial pathologies associated with hydrocephalus, requiring major cranial surgeries other than internal CSF diversion, were excluded from the cases reviewed. The clinical data of the patients were retrieved from the hospital’s medical records department, the unit’s, and operating theatre registers. The data were analyzed and reported in a frequency table and pie chart. We also illustrated two variety of cases of hydrocephalus managed, highlighting some peculiarities and management challenges encountered.
Results
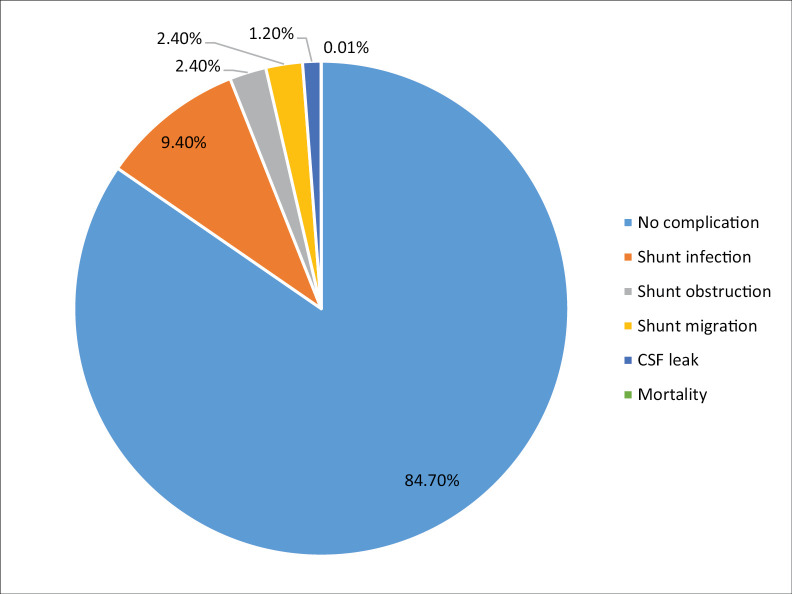
Within the study period (July 2000 to June 2021), a total of 170 patients with hydrocephalus, who had VP shunts, were managed in our neurosurgical service. There were 81 males and 89 females (male:female of 1:1.1). This study only included patients with hydrocephalus, who presented to our neurosurgical unit, and eventually had VP shunting. The age range of the patients was 14 days to 62 years, and infantile hydrocephalus consisted of 121 patients (71.2%). Aqueductal stenosis and post-meningitis hydrocephalus were the top two most common etiologies, with frequencies of 64.7% and 11.4%, respectively. Shunt infection was the most common complication, with a frequency of 9.4%, whereas CSF leak was encountered in 2 patients (1.2%) [Figure 1]. Most of the patients had no complication (85.2%), whereas the overall complication rate was 14.8%, in a 6-month follow-up period.
Figure 1.
Shunt complication rates
Case Illustrations
Case 1
Baby X, an estimated 6–8-month-old male infant [Figure 2], was found abandoned along the corridor of the neonatal unit by patrolling security officers at approximately 4.30 AM. The child was subsequently taken to the children’s emergency ward for a proper evaluation. Clinical history could not be ascertained as there was no caregiver or eyewitness report.
Figure 2.

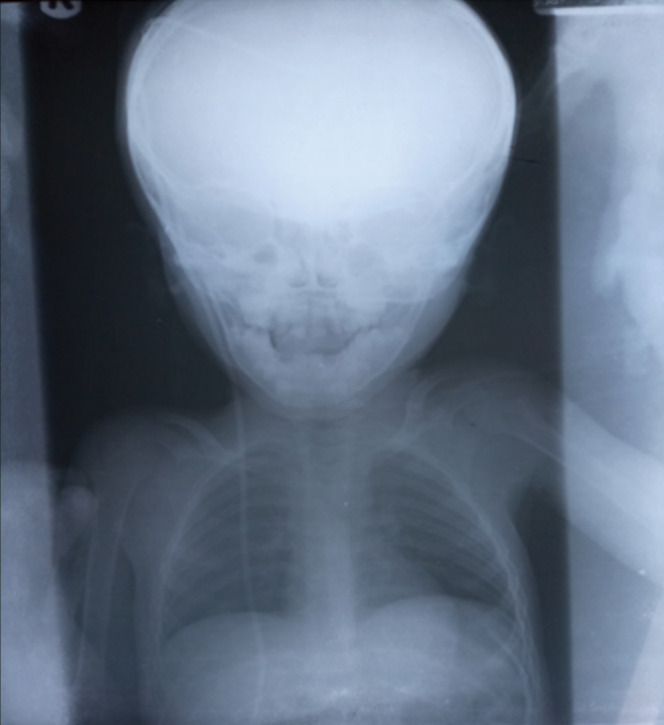
Cranio facial disproportion: prominent scalp veins
On examination, he was listless, febrile, pale, dehydrated, macrocephalic (occipitofrontal circumference of 65 cm), and with marked craniofacial disproportion and prominent scalp veins. The anterior fontanelle was patent, bulging, tense, and with marked sutural diastasis. There was also a sun-setting appearance of the eyes, absent light tracking, and global hypertonia and hyperreflexia. On examination of the back, there was a 10 cm × 10 cm × 8 cm mass in the lumbosacral region. The findings of the other regional examinations were unremarkable.
A full blood count revealed anemia (packed cell volume of 26%), leukocytosis (white cell count of 19,800/mm3). Serum electrolytes showed mild hypokalemia (3.2 mmol/L) and hyponatremia (127 mmol/L). Blood films for malaria parasite were positive for moderate Plasmodium falciparum parasitemia (++). Blood culture samples were taken and culture yielded growth of Haemophilus spp., sensitive to ceftriaxone.
A cranial computed tomography done showed tri-ventriculomegaly with relative sparing of the fourth ventricle, marked thinning of the cortical mantle [Figures 3 and 4]. A diagnosis of severe hydrocephalus with lumbosacral myelomeningocele, anemia, septicemia, electrolyte derangement in an abandoned male infant, was made.
Figure 3.
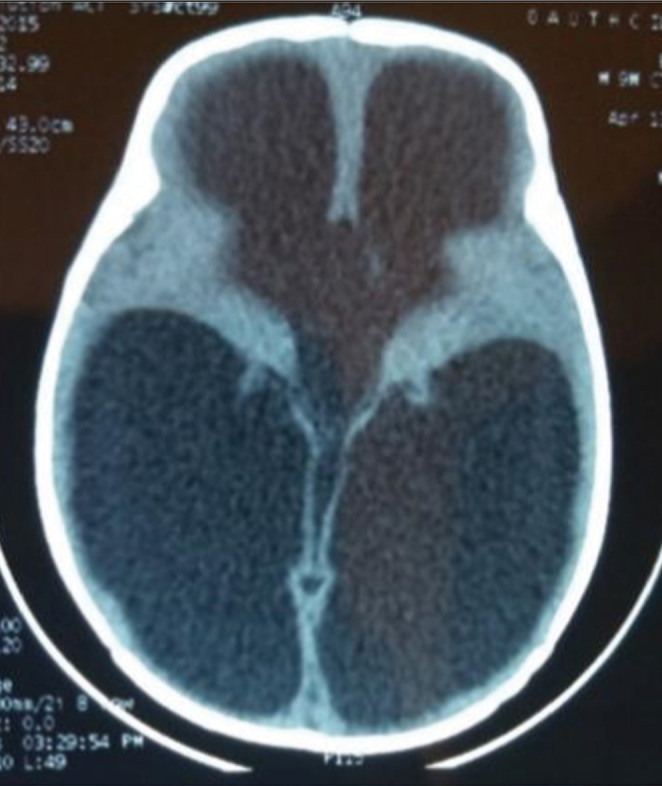
Cranial CT scan: triventriculomegaly
Figure 4.
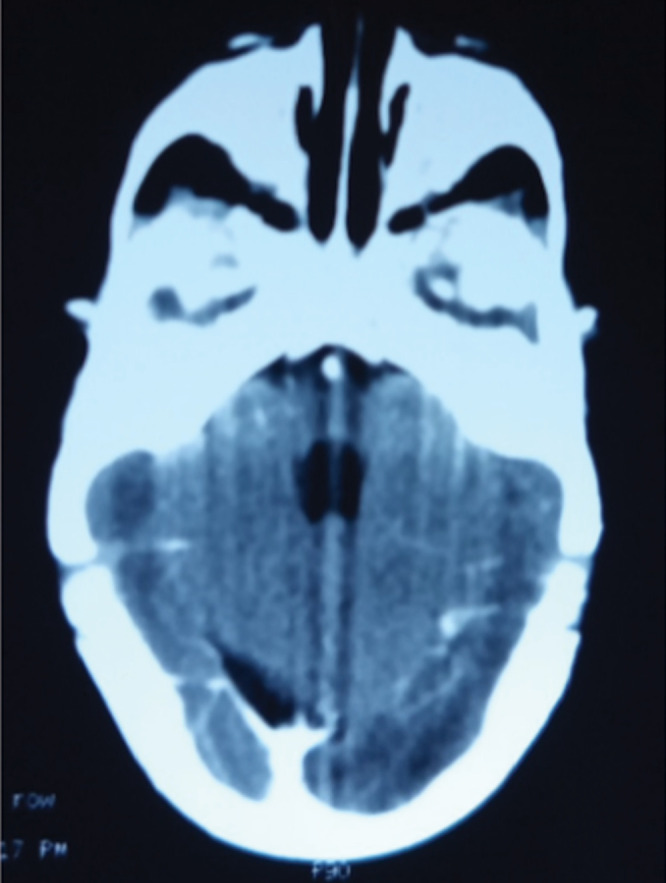
Cranial CT scan: spared fourth ventricle
Child’s management was multidisciplinary, involving the pediatrician, pediatric intensivist, and neurosurgeon, pediatric nursing staff, nutritionist, medical social workers, and the hospital management. Child was transfused with packed red cells, had correction of electrolyte derangement, nutritional rehabilitation, and empirical parenteral antibiotics and was prepped for CSF diversion. Optimization was over a 48-h period after the child was rescued; however, the child died a few days later from severe sepsis and failure to thrive.
Case 2
Master AA, a 5-year-old boy, presented on referral from an affiliated tertiary hospital, on account of progressively increasing head size of 2 months, recurring seizures of 1 month, fever, and altered consciousness of 10 days. The child had been on self-prescribed over-the-counter antibiotics prior to presentation. He had a past medical history of an arrested congenital hydrocephalus in infancy.
On examination, he was febrile, dehydrated, macrocephalic (occipitofrontal circumference of 64 cm), and with craniofacial disproportion, prominent scalp veins, and sun-setting appearance of both eyes. He had a Glasgow coma scale score of 10, positive Kernig’s sign, and global hypertonia and hyperreflexia. A brain magnetic resonance imaging (MRI) was requested; however, it was done after 2 weeks (the delay was due to financial constraint) and showed tri-ventriculmegaly with sparing of the fourth ventricle [Figures 5 and 6]. A full blood count showed leukocytosis (14,000/mm3) and ventricular tap CSF analysis yielded no bacterial growth; however, it was suggestive of bacterial ventriculitis. A diagnosis of post-meningitic hydrocephalus was made. Empirical intravenous antibiotics and anticonvulsants were started; however, irregular as caregivers could not sustain the pay-out-of-pocket expenses. The medical social workers were invited in patient’s management. Child subsequently had three negative ventricular tap CSF analysis and was scheduled for a VP shunt [Figure 7]. The procedure was performed after 3 weeks; the delay was due to further financial limitations with shunt procurement. He was discharged on postoperative day 3 and has been seen at the outpatients with improved seizure control.
Figure 5.
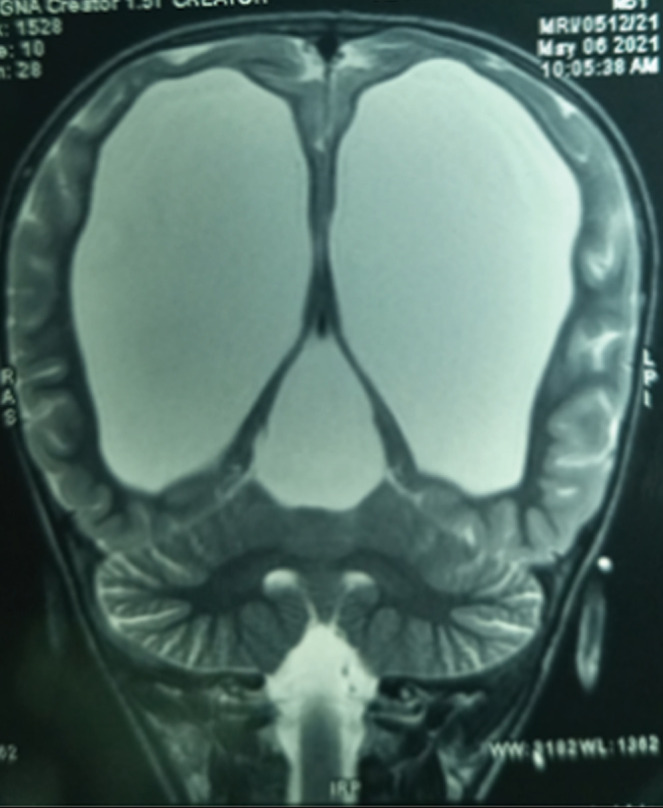
Brain MRI. T2W. Coronal section. Triventriculomegaly
Figure 6.
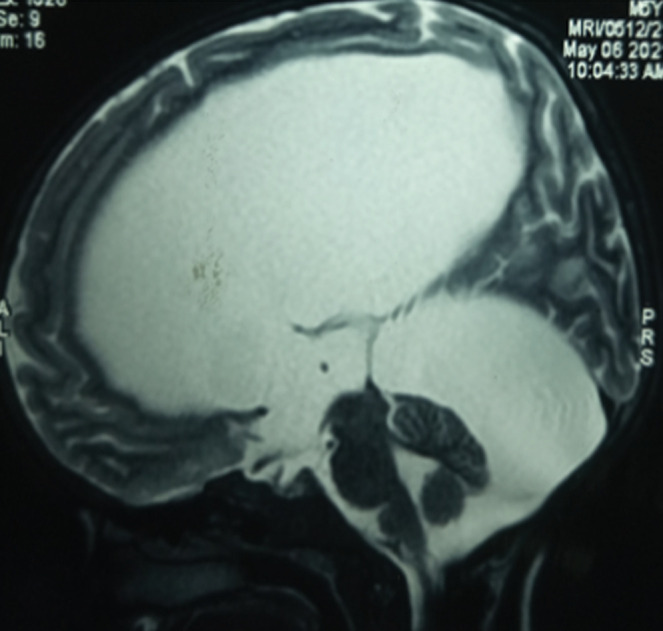
Brain MRI. T2W. Sagittal section. Triventriculomegaly
Figure 7.
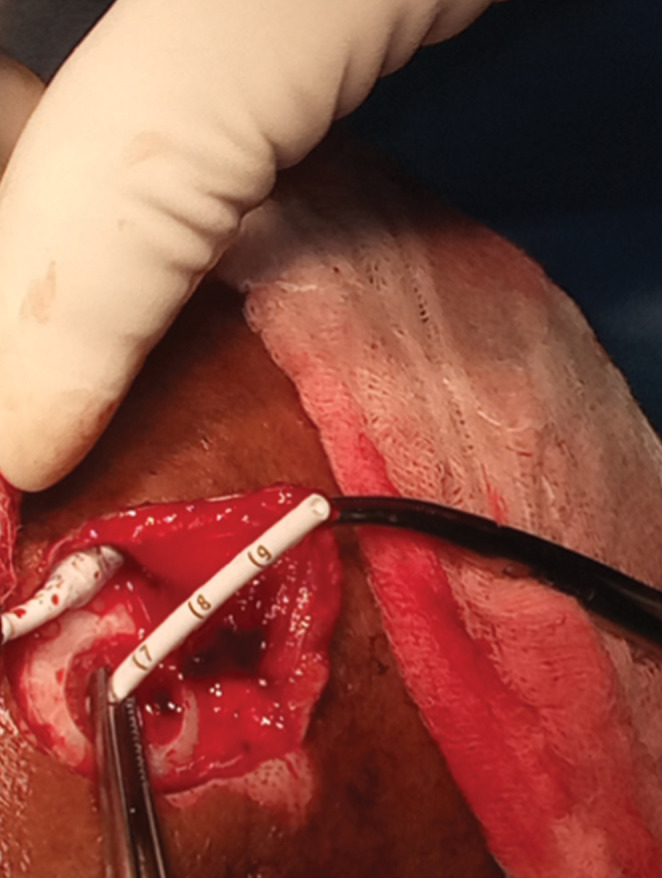
Ventricular catheter placement
Discussion
VP shunt insertion is the mainstay of hydrocephalus treatment in resource-limited countries.[11,12] This treatment modality is effective, although is not without complications with the potential for several revisions over a lifetime.[11] In this series, 167 patients (98.2%) had VP shunt insertion, whereas only 3 patients (1.8%) had endoscopic third ventriculostomy (ETV). The etiological profile in this study were as follows: aqueductal stenosis (64.7%), post-meningitis (11.2%), Dandy–Walker malformation (9.4%), Chiari malformation (10.6%), normal pressure hydrocephalus (3.5%), and porencephalic cyst (0.58%) [Table 1]. The recommended treatment for aqueductal stenosis is an ETV; however, this procedure could not be sustained due to lack of neuroendoscopy setup in this center. The Chabbra VP shunt system is currently the most commonly used system our center due to its relatively wide availability and lower cost. This shunt system has also been reported not to have any significant difference in outcomes or complications when compared with the Codman–Hakim Micro Precision shunt systems.[13]
Table 1.
Etiological profile of hydrocephalus patients
| Etiology | Number of cases | Frequency (%) |
|---|---|---|
| Aqueductal stenosis | 110 | 64.7 |
| Post-meningitis | 19 | 11.2 |
| Dandy–Walker malformation | 16 | 9.4 |
| Chiari malformation | 18 | 10.6 |
| Normal pressure hydrocephalus | 6 | 3.5 |
| Porencephalic cyst | 1 | 0.58 |
| Total | 170 |
Challenges in infantile hydrocephalus management may be first encountered during the preoperative period. These include a late presentation from child neglect and abandonment as was seen in the first case illustration. Other reported causes of late presentation include social taboos, low socioeconomic status, ignorance, and misunderstanding of the early symptoms of hydrocephalus.[5,7,8,9] Shunt-related complications and poor outcomes are more common in patients with delayed shunt insertion, and this is a common occurrence in developing countries. The risk factors for these include co-morbidities like anemia and malnutrition, advanced presentation, and lack/delay of adequate diagnostic imaging.[12] The first case illustrated suffered anemia, malnutrition, malaria, electrolyte derangement, and sepsis, among other problems resulting from neglect and abandonment. Unfortunately, these premorbid factors largely contributed to his demise before CSF shunting was performed.
The second case illustrated presented with progressively increasing head size and recurring seizures in childhood. The early features of raised intracranial pressure from hydrocephalus were probably misunderstood or ignored by his caregivers and had a 2-month delay in presentation. He also had a 2-week delay in getting a brain MRI done and a further 2-week delay in having a VP shunt insertion. These were largely due to financial limitations. The estimated cost for a brain MRI and VP shunting procedure are approximately 80,000 naira (160 USD) and 200,000 naira (400 USD), respectively. These figures are estimated to be approximately 266% and 666% of the monthly minimum wage, respectively.
The Chabbra shunt system is being used in our hospital due to its wider availability and affordability.
Globally, the complication rates of VP shunts are reported to be between 1% and 40% [Figure 8], with developing countries bearing the greater burden. VP shunt infections are the most common complication, and the incidence ranges from 2%–9% and 8.6%–50% in developing and developed countries, respectively.[14,15,16,17,18,19] In this study VP shunt infection rate was (9.4%) and overall complication rate was (14.8%).
Figure 8.
Shunt series
A number of international efforts have aided neurosurgical care and training. Although probably not sufficient, these include donation of VP shunts, neurosurgical equipment, and training sessions (webinars and conferences) by the World Federation of Neurosurgical Societies (WFNS) and the International Society of Paediatric Neurosurgery (ISPN).[4,20] These efforts have been undermined by the poor health-seeking behavior of the average Nigerian, which is largely due to social taboos, low average income, poverty, illiteracy, sociocultural and religious beliefs, and inadequacy of neurosurgical services and lack of an adequate national health insurance scheme.
A review in literature underemphasizes pediatric hydrocephalus as a paramount and inadequately addressed component of the global disease burden.[4] Although there has been advocacy for more investment in primary healthcare and disease prevention, evidence suggests that this burden requires more commitment in resource-limited countries.[4]
The burden of pediatric hydrocephalus is of an increasing public health concern as it is closely associated with economic and sociocultural problems, poor health education, malnutrition, communicable diseases, and maternal risk factors. Addressing these problems will help to ameliorate the preventable causes of hydrocephalus, such as post-meningitis hydrocephalus and neural tube defects. We also recommend future efforts to be geared toward community-based initiatives, providing education and support systems to parents and caregivers of hydrocephalus patients. Establishment of a sustainable and wide coverage National Health Insurance Scheme, to include brain MRI, free or subsidized shunts and essential medical bills, would improve the health-seeking behavior of the average Nigerian citizen.
The relatively small sample size of 170 was largely due to limitations with retrieval of patients’ medical records in the first decade of the study. A good number of the data was lost. During the second decade of the study, there were lesser case referrals to our neurosurgical services. This was due to the establishment of more neurosurgical centers loco-regionally.
Conclusion
VP shunting for hydrocephalus appears to be the most available or prevalent treatment modality in low-income countries, and it is not without management challenges peculiar to these climes. Understanding the scope of these problems is essential to any systematic, multiregional, public health initiative, aimed at ameliorating these challenges in hydrocephalus management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Informed consent was obtained from the patients′ caregivers, or from the hospital management as applicable. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
References
- 1.Dewan MC, Abbas R, Mekary R, Glancz L, Yunusa I, Baticulon R, et al. Global hydrocephalus epidemiology and incidence: Systematic review and met-analysis. J Neurosurg. 2018;130:1065–79. doi: 10.3171/2017.10.JNS17439. [DOI] [PubMed] [Google Scholar]
- 2.Komolafe EO, Adeolu AA, Komolafe MA. Treatment of cerebrospinal fluid shunting complications in a Nigerian neurosurgery programme: Case illustrations and review. Pediatric Neurosurg. 2008;44:36–42. doi: 10.1159/000110660. [DOI] [PubMed] [Google Scholar]
- 3.Rabiu TB, Oshola HA. Pattern of congenital craniospinal anomalies among neurosurgical patients in a tertiary hospital in Nigeria. Archives of Neurogurgery in Africa. 2020;1:4–5. [Google Scholar]
- 4.Muir RT, Wang S, Warf BC. Global surgery for pediatric hydrocephalus in the developing world: A review of the history, challenges, and future directions. Neurosurg Focus. 2016;41:E11. doi: 10.3171/2016.7.FOCUS16273. [DOI] [PubMed] [Google Scholar]
- 5.Bakhsh A. SF shunt complications in infants: An experience from Pakistan. Pediatric Neurosurg. 2011;47:93–8. doi: 10.1159/000329628. [DOI] [PubMed] [Google Scholar]
- 6.Dakurah TK, Adam F, Iddrissu M, Wepeba G, Akoto H, Benkah P, et al. Management of hydrocephalus with ventriculoperitoneal shunt: Review of 109 cases of children. World Neurosurg. 2016;96:129–35. doi: 10.1016/j.wneu.2016.06.111. [DOI] [PubMed] [Google Scholar]
- 7.Moritake K, Nagai H, Miyazaki T, Nagasako N, Yamasaki M, Sakamoto H, et al. Analysis of a nationwide survey on treatment and outcomes of congenital hydrocephalus in japan. Neurol Med Chir (Tokyo) 2007;47:453. doi: 10.2176/nmc.47.453. [DOI] [PubMed] [Google Scholar]
- 8.Laurence KM, Coates S. The natural history of hydrocephalus. Detailed analysis of 182 unoperated cases. Arch Dis Child. 1962;37:345–62. doi: 10.1136/adc.37.194.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acakpo-Satchivi L, Shannon CN, Tubbs RS, Wellons JC, 3rd, Blount JP, Iskandar BJ, et al. Death in shunted hydrocephalic children: A follow-up study. Childs Nerv Syst. 2008;24:197–201. doi: 10.1007/s00381-007-0408-4. [DOI] [PubMed] [Google Scholar]
- 10.Warf BC. “Who is my neighbor?” global neurosurgery in a non-zero-sum world. World Neurosurg. 2015;84:1547–9. doi: 10.1016/j.wneu.2015.07.052. [DOI] [PubMed] [Google Scholar]
- 11.Drake JM, Kestle JT. Determining the best cerebrospinal fluid shunt valve design: The pediatric valve design trial. Neurosurgery. 1998;43:1259–60. doi: 10.1097/00006123-199811000-00158. [DOI] [PubMed] [Google Scholar]
- 12.Gathura E, Poenaru D, Bransford R, Albright AL. Outcomes of ventriculoperitoneal shunt insertion in Sub-Saharan Africa. J Neurosurg Pediatr. 2010;6:329–35. doi: 10.3171/2010.7.PEDS09543. [DOI] [PubMed] [Google Scholar]
- 13.Warf BC. Comparison of endoscopic third ventriculostomy alone and combined with choroid plexus cauterization in infants younger than 1 year of age: A prospective study in 550 African children. J Neurosurg. 2005;103:475–81. doi: 10.3171/ped.2005.103.6.0475. [DOI] [PubMed] [Google Scholar]
- 14.Bhuta P, Bhalodiya D, Patel U. Porencephaly: Case report and review. J Integr Health Sci. 2016;IV:52–9. [Google Scholar]
- 15.Ho SS, Kuzniecky RI, Gilliam F, Faught E, Bebin M, Morawetz R. Congenital porencephaly: MR features and relationship to hippocampal sclerosis. AJNR Am J Neuroradiol. 1998;19:135–41. [PMC free article] [PubMed] [Google Scholar]
- 16.Kinasha ADA, Kahamba JF, Semali IT. Complications of ventriculoperitoneal shunts in children in Dar es Salam. East Cent African J Surg. 2005;10:55–9. [Google Scholar]
- 17.Komolafe EO, Komolafe MA, Adeolu AA. Factors implicated for late presentations of gross congenital anomaly of the nervous system in a developing nation. Br J Neurosurg. 2008;22:764–8. doi: 10.1080/02688690802485113. [DOI] [PubMed] [Google Scholar]
- 18.Mwachaka PM, Obonyo NG, Mutiso BK, Ranketi S, Mwang’ombe N. Ventriculoperitoneal shunt complications: A three-year retrospective study in a Kenyan national teaching and referral hospital. Pediatr Neurosurg. 2010;46:1–5. doi: 10.1159/000314050. [DOI] [PubMed] [Google Scholar]
- 19.Mwang’ombe NJ, Omulo T. Ventriculoperitoneal Shunt surgery and shunt infections in children with non-tumour hydrocephalus at the Kenyatta National Hospital, Nairobi. East Afr Med J. 2000;77:386–90. doi: 10.4314/eamj.v77i7.46684. [DOI] [PubMed] [Google Scholar]
- 20.Warf BC. Educate one to save a few. Educate a few to save many. World Neurosurg. 2013;79:S15. doi: 10.1016/j.wneu.2010.09.021. [DOI] [PubMed] [Google Scholar]