Abstract
The current study aimed to explore the relationship between maternal exposure to various types of trauma and child anxiety outcomes, and to investigate maternal depression and parenting quality as potential mediators of these relationships. Aims were examined within a sample of 185 mother-child dyads who participated in a longitudinal study assessing maternal trauma history, maternal depression, and parenting quality at preschool age (ages 2.5 to 5.5 years), and for whom maternal and secondary caregiver reports of child anxiety were obtained at school age (ages 6 to 11 years). Hypotheses were that (1) maternal exposure to trauma would be positively associated with anxiety levels in offspring and that (2) parenting quality and maternal depression would mediate the relationship between maternal exposure to trauma and child anxiety. Results suggest a direct association between maternal trauma history and child anxiety, as well as indirect associations through parenting quality and maternal depression. These findings are discussed with regard to their implications for the prevention of child anxiety, as well as their implications for the advancement of the literature on intergenerational effects of trauma.
Keywords: maternal trauma, parenting, maternal depression, child anxiety, trauma, anxiety
There is increasing scientific interest in the intergenerational effects of trauma, as well as the social, psychological, and biological channels through which trauma exposure may influence offspring outcomes (Buss et al., 2017; Bosquet Enlow, Englund, & Egeland, 2016). Studies in this area have historically focused on large-scale traumatic events such as the Holocaust and World War II, but have recently begun to focus on more common domains of trauma, such as childhood abuse. These more recent studies have found associations between maternal childhood trauma and offspring internalizing and externalizing symptomology (Min et al., 2013; Miranda, de la Osa, Granero & Ezpeleta, 2011; Morrel, Dubowitz, Kerr & Black, 2003; Myhre, Dyb, Wentzel-Larsen, Grøgaard, & Thoresen, 2014). Of note, very few of these intergenerational trauma studies have focused on the outcome of childhood anxiety. This is surprising, because trauma-related fear and anxiety tendencies would be expected to be primary contenders for intergenerational transmission via both modeling and genetic processes. Moreover, childhood anxiety symptoms are predictive of a myriad of developmental cascades, with potential long-term negative impacts on mental health (Vasey, Bosmans, & Ollendick, 2014). This gap in the literature likely reflects a general trend in the field of developmental psychopathology where studies of child anxiety have lagged behind those of other psychological problems (e.g., childhood depression, conduct problems, Muris & Broeren, 2009). Therefore, the primary aim of the current study was to examine maternal exposure to trauma as a risk factor for offspring anxiety outcomes, and to focus attention on this previously neglected research question.
Only two published studies to date have examined the relationship between maternal childhood trauma and offspring anxiety. In the first study, Smith and colleagues (2009) found that maternal exposure to sexual abuse in childhood was associated with higher levels of emotional and anxiety-related problems in offspring. In the second study, Jovanovic and colleagues (2011) demonstrated that offspring dark-enhanced startle response – a physiological marker of anxiety – was greater among mothers with histories of childhood physical abuse. These initial studies suggest that maternal exposure to both childhood physical and sexual abuse may influence anxiety-related outcomes in offspring. However, there is a need for replication and extension of these findings. In particular, empirical studies should examine the long-term emotional and behavioral manifestations of these intergenerational risks among children of mothers with histories of trauma and to elucidate the potential mechanisms involved in these intergenerational effects of trauma exposure.
Parenting is considered a primary pathway by which a mother’s exposure to trauma may influence her children’s behavior problems. Previous studies have found that women who have a history of sexual and/or physical abuse demonstrate higher rates of hostile parenting behaviors, hyper-criticism, flattened emotional response, and parenting stress, and lower rates of parental sensitivity and offspring autonomy-granting; Juul et al., 2016; Newcomb & Locke, 2001; Sprang et al., 2013; van Ee, Kleber, & Mooren, 2012; Zvara, Mills-Koonce, Carmody, Cox, & Family Life Project Key Investigators, 2015). While negative parenting behaviors, including hostility and harsh discipline, have been found to mediate the relationship between maternal trauma history and offspring behavior problems (Collishaw et al., 2007; Rijlaarsdam et al., 2014; Thompson, 2007), less is known about the role of positive parenting qualities and their potential role in intergenerational impacts of trauma. These positive parenting qualities, which include behaviors such as praising or rewarding a child, demonstrating warmth, and providing adequate emotional support, have been found to have significant impact on the development of behavioral and emotional problems in childhood. Researchers from our group, for example, in a study examining the relationship between maternal and child personality traits, have previously found that maternal antisocial traits predicted child psychopathic traits, but only when positive parenting practices were lacking (Robinson, Azores-Gococo, Lilienfeld, & Brennan, 2016). This finding suggests that positive parenting may serve as a buffer between maternal risk factors and offspring development. Van der Sluis, van Steensel, & Bögels have presented a more complex picture, namely that some positive parenting practices (e.g., parental modeling, reassurance) are associated with lower rates of offspring anxiety (van der Sluis, van Steensel, & Bögels, 2015a), whereas other positive parenting practices (e.g., positive reinforcement) are more common among parents of clinically anxious children in comparison to parents of healthy controls (van der Sluis, van Steensel, & Bögels, 2015b). Others have found that the nature of the relationship between parenting practices and child anxiety may depend on a number of factors, including the gender of the child (Suveg, Sood, Barmish, Tiwari, Hudson, & Kendall, 2008) and the particular circumstances or context in which the parenting behaviors are exhibited (e.g., the emotions being displayed by the child, Hudson, Comer, Kendall, 2008). Overall, these studies suggest that the relationship between positive parenting practices and children’s emotional development may be more nuanced than formerly assumed and that more research is needed on the role that these parenting qualities may play in influencing children’s emotional development, especially in the context of the intergenerational transmission of trauma.
The current study aims to advance the literature on the potential role of parenting practices in the intergenerational transmission of trauma by examining observable parenting behaviors exhibited by mothers toward their children, rather than relying upon self-report measures of parenting practices. For quite some time, researchers have argued that parenting should be operationalized behaviorally, rather than assessed via self-report questionnaires to minimize self-report biases and provide a more valid assessment of parenting (Rapee, 1997). Parents’ self-perceptions and reports of parenting behaviors may be particularly susceptible to bias when they have experienced traumatic events in their lifetime (Bailey et al., 2012; Fitzgerald et al., 2005). Given that much of the existing literature has focused primarily on self-reports of parenting, the current study aims to utilize a less subjective measure involving laboratory observations of interactions between mother and child. By doing so, we hope to provide an important contribution to the existing literature in this area and a greater understanding of the role of parenting in the intergenerational transmission of trauma-related outcomes.
Empirical evidence suggests that exposure to trauma during childhood increases the risk of depression in women (Nanni, Uher & Danese, 2012). Maternal depression also has substantial links to offspring anxiety (Lewis et al., 2011), which suggests it may be a mechanism of intergenerational risk. Indeed, previous studies have found that maternal depression acts as a mediator between childhood trauma and offspring internalizing and externalizing behavioral problems (Collishaw et al., 2007; Koverola et al., 2005; Miranda et al., 2011). In one such study, maternal depression served as a mediator only when examining maternal reports of child behavior, suggesting that multiple informants of child outcome should be considered when examining intergenerational impacts of maternal trauma (Min et al., 2013). The present study adds to this literature by including both maternal and alternate caregiver reports of child anxiety.
The current study aimed to fill existing gaps in the literature by examining associations between maternal trauma exposure and child anxiety. We used data from a prospective study of 185 children to examine two potential mechanisms (parenting and maternal depression) that might explain the intergenerational effects of trauma exposure. We hypothesized that children of mothers who have been exposed to trauma would have greater rates of anxiety symptoms than children of non-exposed mothers. We also hypothesized that parenting quality and maternal depression would mediate the relationship between maternal trauma exposure and child anxiety. Finally, throughout our analyses, we explored the relative contributions of lifetime experiences of trauma and early childhood physical and sexual abuse on offspring anxiety outcomes.
Method
Participants
The current study is based on a sample of 185 mother-child dyads who participated in a study of preschool and school age child development. The majority (82%) of participants were recruited and assessed through Emory’s Women’s Mental Health Program (WMHP)—a referral center housed within the Department of Psychiatry at the Emory University School of Medicine that specializes in the provision of mental healthcare during pregnancy and in the postpartum period. Consequently, all mothers recruited from this center had some history of psychiatric illness and had received treatment within the WMHP in the postnatal period. Mothers were recruited from the WMHP for participation in a broader study examining the course of maternal psychiatric symptoms and the effects of prenatal psychotropic exposure on offspring outcomes. Mothers included in this study were not recruited on the basis of prior exposure to trauma. Despite being recruited from a treatment center, mothers were not required to receive treatment to participate in the study. Nonetheless, 59.4% of mothers were currently undergoing mental health treatment (psychological or psychiatric treatment) at the time of study enrollment.
The remaining mothers in the sample were community controls recruited from the Emory Child Study Center database, a database of mothers recruited at local events for participation in various Emory-affiliated research studies. This separate sampling strategy was necessary to recruit a control group of mothers without prenatal exposure to psychotropic medications given the broader study’s objectives. Mothers were recruited from this database for the current study with the inclusion criteria that they were not medicated or treated for a psychological disorder when pregnant with the target child.
Participants recruited from the WMHP and controls did not differ on any demographics relevant to the current study (i.e., mother age, child age, mother/child ethnicity, mother marital status, maternal education level, number of hours mother worked per week, number of adults in the household) with the exception of number of children in the home (p = 0.046), with controls having more children in the household than participants recruited from the WMHP. Participants recruited from the WMHP and controls also did not differ on rates of maternal trauma exposure (all ps >.13). Given that the WMHP sample is a high risk clinical sample, mothers recruited from this center had a higher prevalence of psychiatric diagnosis (including diagnosis of PTSD) at the time of the preschool visit compared to controls (p=0.018).
The mother-child dyads who participated in the school age follow up (N=185) represent approximately 85% of the participants who were initially recruited for the preschool phase of the study. The mothers lost to follow-up differed significantly from retained participants with regard to mothers’ educational levels (lost: M=5.88 years of post-secondary education (graduated from a 4-year college), SD=1.64; retained: M=6.56 years of post-secondary education (part-graduate or –professional school), SD=1.45). Children included in the final sample did not differ from those lost to follow-up on measures of preschool ratings of anxiety, child gender, maternal age, maternal depression ratings, or race/ethnicity.
Mothers in the final sample were primarily Caucasian (83%), highly educated (median bachelor’s degree), and married (83%). Children's ages ranged from 2.5 to 5.5 years old (M=3.73; SD=0.89) at the preschool phase of this study and from 6 to 11 years old (M=7.16; SD=1.19) at the time of the online school-age follow-up. Approximately half (48.6 %) of the children were male, and half (51.4%) were female. Mothers’ ages ranged from 21 to 49 years old (M=37.12; SD=4.78) during the preschool phase and from 24 to 53 years old (M=40.85; SD=4.87) at follow-up.
Procedure
During the preschool phase of this study, participants completed a 3-hour lab visit at Emory University during which a structured clinical interview was administered to mothers, several behavioral and self-report measures were administered to both mother and child, and a parent-child interaction was recorded. In the online follow-up study, data were collected via REDCap—a secure online database used by research institutions for confidential data collection (Harris et al., 2009). Recruitment for the school-aged follow-up was conducted by contacting participants from the original study via email and/or phone. Participants were emailed an embedded hyperlink, which led them to the REDCap server where they were provided consent information and guided through a series of online questionnaires if they agreed to all stated study details. To supplement our mother-report measures, data were also gathered from an alternate caregiver identified by mothers in our sample as someone who knows their child well and with whom the child has regular contact (e.g., father, grandparent, teacher). These alternate caregivers were then contacted using the secure online REDCap procedures outlined above. Alternate caregivers in our sample included fathers/father figures (78.3%), grandparents, (10.9%), teachers (6.5%), nannies/babysitters (2.9%), and other caregivers (e.g., aunt; 1.4%).
Measures
Maternal history of trauma.
Maternal trauma was assessed during the preschool phase of this study using a self-report questionnaire – the Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998) – and a clinical interview – the Structured Clinical Interview for DSMIV Axis I Disorders (SCID-I). In order to maintain consistency with the current literature (e.g., Brand et al., 2010; DiLillo et al., 2006), two subscales from the CTQ were used to evaluate childhood trauma exposure: Physical Abuse and Sexual Abuse. The Physical Abuse subscale includes items assessing whether an individual has experienced being hit hard enough to see a doctor, being hit hard enough to leave bruises, or being hit badly enough to be noticed, among other items. The Sexual Abuse subscale within this measure includes items assessing whether an individual was touched sexually, was hurt if she did not do something sexual, or was made to do sexual things, among other items. Items are rated on a 5-point Likert scale with response options ranging from “Never True” to “Very Often True.” Consistent with previous literature, individuals who scored a 6 or above on the Sexual Abuse scale (N=39) or an 8 or above on the Physical Abuse scale (N=38) were considered to have experienced sexual or physical abuse in childhood (DiLillo et al., 2006). Separate variables were coded dichotomously for presence (1) or absence (0) of either physical or sexual abuse in childhood. Based on this coding scheme, 13.0% of our sample (n = 24) experienced physical abuse only, 14.1% (n = 26) experienced sexual abuse only, and 7.0% (n = 13) experienced both types of trauma in childhood as measured by the CTQ.
In addition to the CTQ, the SCID-I was administered to mothers in our sample by Master’s-level trained clinicians to assess mothers’ mental health histories across the lifespan. Within this clinical interview, mothers were asked whether they had experienced an event that was extremely upsetting or life threatening and were given several examples of such events (e.g., major disaster, fire, combat, serious car accident, sexual abuse, physical abuse) as outlined in the SCID-I interview. Mothers’ responses were dichotomously coded as yes (1) or no (0) for the purposes of data analysis. This coding procedure is considered to be an accurate and cost-effective method of measuring trauma exposure in healthy (Elhai et al., 2008) and mentally ill samples (Franklin et al., 2002). Interrater reliability for maternal reports of lifetime trauma was high (κ =0.98). A total of 63 mothers (35%) reported lifetime trauma. The full PTSD module was administered to determine whether mothers met criteria for PTSD at present and/or across their lifetime. 13.3% of mothers in our sample met criteria for PTSD at some point in their lifetime, while only 3.2% met criteria for a current diagnosis of PTSD at the time of the preschool visit.
The use of both CTQ and SCID trauma measures allowed us to examine impacts of both childhood trauma exposure and trauma across the lifespan. The correlations between CTQ and SCID measures of trauma were significant and modest in strength (see Table 2).
Table 2.
Zero-Order Correlations Between Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Maternal Lifetime Trauma | --- | .36** | .29** | .10 | .17* | .20* | .26** | −.20** | .17* | −.03 |
| 2.Maternal Childhood Sexual Abuse | --- | .17* | .03 | .01 | .05 | .24** | −.10 | .09 | −.01 | |
| 3. Maternal Childhood Physical Abuse | --- | .03 | .05 | .15 | .25** | −.22** | .25** | −.16* | ||
| 4. PROMIS-Anx (Mother Report) | --- | .63** | .43** | .41** | −.08 | .12 | −.03 | |||
| 5. CBCL-Anx (Mother Report) | --- | .47** | .28** | −.16* | .16* | −.001 | ||||
| 6. CBCL-Anx (Alt.Cgv. Report) | --- | .15 | −.03 | −.03 | .09 | |||||
| 7. Maternal Depression | --- | −.19** | .22** | −.03 | ||||||
| 8. Positive Engagement | --- | −.82** | −.03 | |||||||
| 9. Negative Engagement | --- | −.38* | ||||||||
| 10. Positive Reinforcement | --- |
p<.05.
p<.01.
Note. PROMIS=Patient Reported Outcomes Measurement Information System; Anx=Anxiety; CBCL=Cluld Behavior Checklist; Alt.Cgv.= Alternate Caregiver.
Parenting quality.
Parenting quality was assessed during the preschool visit using the Dyadic Parent-Child Interaction Coding System (DPICS; Eyberg & Robinson, 1981). Trained research assistants coded two ten-minute segments (structured and unstructured) of play by identifying and recording the frequency of mother and child behaviors across three categories: verbalization, vocalization, and physical behavior. Ten maternal DPICs behaviors were coded by these raters, and interrater reliability was found to be good to excellent (kappas >.70).
As in our previous work (Schechter et al., 2017), we used three composite parenting variables derived from Principle Components Analysis (PCA): (1) Positive Engagement (comprised of maternal use of reflective statements, neutral talk, indirect commands, information questions, and descriptive questions); (2): Negative Engagement (comprised of maternal use of negative talk and direct commands); and (3) Positive Reinforcement (comprised of maternal use of labeled praise, unlabeled praise, and behavioral descriptions; see Table 1 for descriptions of coded parenting behaviors). The parenting variables used for analysis were residuals resulting from regressing the total number of maternal verbalizations onto the composite scores of positive engagement, negative engagement, and positive reinforcement; this approach controlled for any variation in parenting behaviors that may reflect differences in the amount of speech produced during parent-child interactions, rather than the more qualitative differences in parenting behaviors in which we were interested.
Table 1.
Descriptions of coded parenting behaviors
| Factor | Description |
|---|---|
| Positive Engagement | |
| Reflective Statement | Statement that reflects upon and has the same meaning as previous verbalizations made by the child. For example, in response to a child saying, “this game is fun,” a reflective statement might be “you like playing this game!” |
| Neutral Talk | A statement made to the child that is non-descriptive and non-evaluative of the child or the child’s actions (e.g., “I want to draw with you.”) |
| Indirect Command | Parent suggests that their child perform a particular vocal or motor behavior; suggestion can be made in the form of a question or statement (e.g., “I’d like you to finish the picture,” “Will you tell me what color this is?”) |
| Information Question | Parent asks a question to which they expect an informative response (e.g., “What time is it?”) |
| Descriptive Question | A descriptive statement expressed in question form with the expectation that the child give a brief (often yes/no) response (e.g., “That was fun, wasn’t it?”) |
| Negative Engagement | |
| Negative Talk | Parent expresses disapproval of the child or the child’s activities and choices (e.g., “I think you are being careless.) |
| Direct Command | Declarative statement made by the parent that orders or directs the child to engage in certain behaviors (e.g., “hurry up,” “put these away”) |
| Positive Reinforcement | |
| Labeled Praise | Positive evaluation of the child or the child’s behaviors and activities (e.g., “you are a good builder,” “your picture is pretty”) |
| Unlabeled Praise | Parent expresses non-specific approval of the child or child’s behavior (e.g., “good job,” “I like that”) |
| Behavioral Description | Declarative statement made about the child’s actions (e.g., “you are singing a song,” “you and I are playing”) |
Maternal depression.
During the preschool phase of the study, mothers also reported their current depressive symptoms on the Beck Depression Inventory (BDI; Beck, Steer & Carbin, 1988). The BDI is a 21-item questionnaire with established reliability and validity that queries about depressive symptoms experienced over the course of the past two weeks. Items within this questionnaire are rated on a four-point scale (0-3) and yield total scores ranging from 0 to 63 where higher scores are indicative of more severe depressive symptoms. In this sample, the average maternal BDI score was 6.01 (SD=7.38). Mothers’ responses on the BDI revealed high internal consistency (α=.921).
Child anxiety.
Mothers and alternate caregivers completed the Child Behavior Checklist (CBCL; Achenbach, 1991) during the online school-age follow-up. The 6-item DSM oriented Anxiety Problems subscale of the CBCL (Achenbach, Dumenci & Rescorla, 2003) was used to assess child anxiety levels. Items within the CBCL Anxiety Problems subscale are rated on a 3-point Likert scale (0 = Not True, 1 = Somewhat or Sometimes True, 2 = Very True or Often True). Total scores range from 0 to 12 with higher scores indicating higher levels of anxiety (mother CBCL α=.80, M=1.82, SD=2.41; alternate caregiver CBCL α=.79, M=1.72, SD=2.23).
In addition, mothers completed the Pediatric Anxiety form of the Patient-Reported Outcomes Measurement Information System (PROMIS; Irwin et al., 2012). The pediatric proxy report of anxiety consists of 10 items assessing fear, worry, and nervousness. Items are rated on a 5-point Likert scale (1 = Never, 2 = Almost never, 3 = Sometimes, 4 = Often, 5 = Almost Always) and yield total scores of 10 to 50 with higher scores reflecting higher levels of anxiety. Mothers’ responses on this measure revealed high internal consistency (α=.94, M=9.34, SD=9.43). Maternal PROMIS, maternal CBCL, and secondary caregiver CBCL anxiety measures served as observed variables that were used to create a latent factor of school-age child anxiety. The use of multiple reporters allowed us to reduce biases that might result from relying solely on mothers’ reports (De Los Reyes & Kazdin, 2005).
Covariates.
Mothers provided information concerning child age, sex, and ethnicity, as well as their own age and education level on self-report questionnaires at the preschool and school-age follow up. In addition, maternal prenatal psychotropic medication exposure was available from prospectively collected clinic records and was calculated by multiplying the number of drugs in each major classification of psychotropic medications (antipsychotics, antiepileptics, selective serotonin reuptake inhibitors (SSRIs)) by the number of weeks taken, standardized to a 40-week pregnancy. This is a common procedure used to examine the effects of varying “doses” of prenatal medication exposure (i.e., the amount of time a fetus was exposed to psychotropic medications in utero) over the course of a 40-week pregnancy (e.g., Johnson, Smith, Stowe, Newport, & Brennan, 2016; Smith et al., 2012).
Statistical Approach
SPSS AMOS 23 was used to test all hypotheses, with the dependent measure being the latent factor of child anxiety as described above. Potential confounds (e.g., demographics, maternal medication use) were included in the model if they significantly predicted child anxiety. To test for relative impacts and reduce the number of statistical tests, all maternal trauma variables were examined together as predictors of child anxiety. This constituted our primary structural equation model (SEM) to test for main effects of maternal trauma exposure. Next, potential mediators were individually added to this model to assess indirect effects. Four potential mediators were examined: three measures of observed parenting quality and self-reported maternal depression.
Model fit was assessed using the χ2 index, comparative fit index (CFI), and root-mean-square of approximation (RMSEA). The χ2 index tests discrepancies between the population covariance and the covariance predicted by the model, where a non-significant χ2 indicates a good, non-discrepant fit (Hooper, Coughlan, & Mullen, 2008). The CFI compares the model of interest with the independence model while taking the sample size into account. CFI values range from 0-1 with those over 0.90 indicating adequate fit and those over 0.95 indicating good fit (Hu & Bentler, 1999). RMSEA measures how well the model estimates fit the population covariance matrix (Browne, Cudeck, Bollen, & Long, 1993), where values less than 0.06 indicate a good fit (Hu & Bentler, 1999; Kline, 2010). To test for mediation, bootstrapping methods (Hayes, 2013) were used in AMOS to calculate the significance of the path from the predictor variable (e.g., maternal trauma) through the mediator (e.g., maternal depression) to the outcome (child anxiety).
Results
Preliminary Analyses
Bivariate correlations between study variables can be found in Table 2. Notably, child anxiety variables were significantly and positively correlated with one another, providing justification for our latent factor approach.
Demographic factors including child age, child sex, child ethnicity, maternal education, and maternal age at child’s birth were assessed as potential confounds in separate SEM analyses. Because the majority of the women in the sample were recruited from a psychiatric treatment center, we also assessed maternal medication use during pregnancy as a potential confound. Although no sociodemographic factors significantly predicted child anxiety, maternal SSRI use in pregnancy (but not antipsychotic or antiepileptic use during pregnancy) was significantly associated with the latent variable of child anxiety (β =.267; p =.003), and was therefore controlled for in subsequent SEM analyses.
Main Effects of Maternal Trauma Exposure
It was hypothesized that maternal trauma exposure would predict higher levels of anxiety in school-aged offspring. SEM was used to examine maternal experiences of physical abuse in childhood, sexual abuse in childhood, and trauma across the lifetime as independent variables in the prediction of a latent measure of offspring anxiety (as described in the Methods section). The overall model demonstrated good fit (χ2(N=185)=6.88, df=11, p=.81, CFI=1.0, RMSEA=0.00). Maternal lifetime exposure to trauma was found to significantly and positively predict offspring anxiety. Neither maternal childhood sexual abuse, nor maternal childhood physical abuse, were related to offspring anxiety (see Figure 1).
Figure 1:
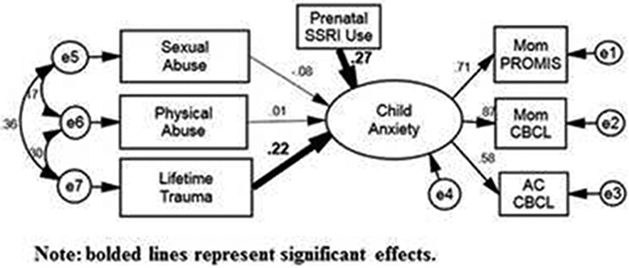
Overall estimated SEM model investigating prospective relationships among maternal trauma exposure and a latent measure of offspring anxiety (as measured by mothers and alternate caregivers). The overall model demonstrated good fit (χ2(N = 185) = 6.88, df = 11, p = .81, CFI = 1.0, RMSEA = .00). Maternal lifetime exposure to trauma was found to significantly and positively predict offspring anxiety. Neither maternal childhood sexual abuse, nor maternal childhood physical abuse, were related to offspring anxiety. Note: Bolded lines represent significant direct and indirect effects. Latent variables are depicted using circles, whereas measured variables are depicted using rectangular boxes
Potential Mediators
It was hypothesized that parenting quality and maternal depression would mediate the association between maternal trauma and offspring anxiety. Parenting quality was represented by observations of positive reinforcement, positive engagement, and negative engagement as described in Methods. Each potential mediator was separately entered into the primary SEM model, and indirect effects were estimated for each hypothesized mediational pathway.
Parenting quality.
The model that included maternal positive engagement with the child (see Figure 2a) demonstrated excellent fit (χ2(N=185)=10.71, df=14, p=0.71, CFI=1.00, RMSEA=0.00). In this model, maternal history of childhood physical abuse negatively predicted maternal use of positive engagement, such that mothers who were physically abused during childhood showed lower rates of positive engagement during the mother-child interaction (β=−.18, p=0.02). There was also a significant indirect effect of maternal experiences of childhood physical abuse on offspring anxiety via maternal positive engagement (see Table 3). Neither maternal experiences of childhood sexual abuse (β=−.01, p=0.89) nor lifetime trauma (β=−.13, p=0.13) were significantly associated with maternal positive engagement.
Figure 2:
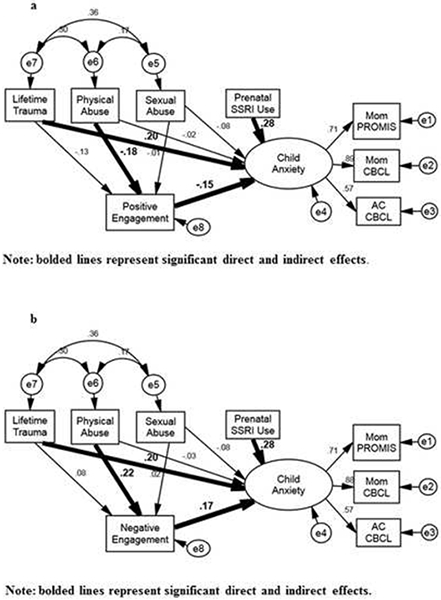
Overall estimated SEM model investigating the prospective role of parenting quality as a mediator in the association between maternal trauma exposure and offspring anxiety. The model including maternal positive engagement as a mediator (a) demonstrated excellent fit (χ2(N = 185)=10.71, df = 14, p = .71, CFI =1.00, RMSEA = .00), as did the model including maternal negative engagement (b) (χ2(N = 185) = 10.76, df= 14, p = .71,CFI = 1.00, RMSEA = .00). Maternal history of childhood physical abuse (but not childhood sexual abuse or lifetime trauma) predicted lower rates of positive engagement and higher rates of negative engagement, both of which predicted higher rates of offspring anxiety. Note: Bolded lines represent significant direct and indirect effects. Latent variables are depicted using circles, whereas measured variables are depicted using rectangular boxes
Table 3.
Indirect Effects Analyses Predicting Child Anxiety
| Indirect Effects Pathway | Effect | p | Lower Limit CI | Upper Limit CI |
|---|---|---|---|---|
| Positive Reinforcement | ||||
| Maternal lifetime trauma | .016 | .477 | −.057 | .285 |
| Maternal physical abuse | −.076 | .575 | −.570 | .231 |
| Maternal sexual abuse | −.001 | .830 | −.211 | .115 |
| Positive Engagement | ||||
| Maternal lifetime trauma | .292 | .072 | .017 | .982 |
| Maternal physical abuse | .491 | .039 | .084 | 1.33 |
| Maternal sexual abuse | .028 | .697 | −.208 | .470 |
| Negative Engagement | ||||
| Maternal lifetime trauma | .211 | .181 | −.029 | .841 |
| Maternal physical abuse | .623 | .031 | .143 | 1.603 |
| Maternal sexual abuse | .050 | .592 | −.200 | .546 |
| Maternal Depression | ||||
| Maternal lifetime trauma | .878 | .007 | .284 | 1.931 |
| Maternal physical abuse | 1.08 | .018 | .296 | 2.549 |
| Maternal sexual abuse | .952 | .032 | .193 | 2.483 |
Note: CI=Confidence Interval.
Similarly, the model that included maternal negative engagement with the child (see Figure 2b) also demonstrated excellent fit (χ2(N=185)=10.76, df=14, p=0.71, CFI=1.00, RMSEA=0.00). Maternal history of childhood physical abuse (β=.22, p<.01), but not history of childhood sexual abuse (β=.02, p=0.83) or lifetime trauma (β=.08, p=0.30), predicted maternal use of negative engagement such that mothers who were physically abused during childhood utilized more negative engagement during the parent-child interaction. There was a significant indirect effect of maternal childhood physical abuse on offspring anxiety via maternal use of negative engagement (see Table 3).
The model that included maternal positive reinforcement of the child as a potential mediator demonstrated excellent fit (χ2(N=185)=8.95, df=14, p=0.84, CFI=1.00, RMSEA=0.00). In this model, maternal childhood physical abuse (β=−.18, p=0.02), but not childhood sexual abuse (β=−.003, p=0.97) or lifetime trauma (β=.05, p=0.59), negatively predicted maternal use of positive reinforcement during the parent-child interaction such that mothers who experienced physical abuse used less positive reinforcement overall. However, there were no significant indirect effects of maternal trauma on child anxiety via positive reinforcement (see Table 3).
Maternal depression.
The model that included maternal depression as a potential mediator demonstrated good fit (χ2(N=185)=22.05, df=14, p=0.08, CFI=0.96, RMSEA=0.06). In this model, significant indirect effects were noted for each type of maternal trauma (see Table 3). In addition, maternal lifetime trauma no longer directly predicted child anxiety once the indirect effect of maternal depression was accounted for (see Figure 3).
Figure 3:
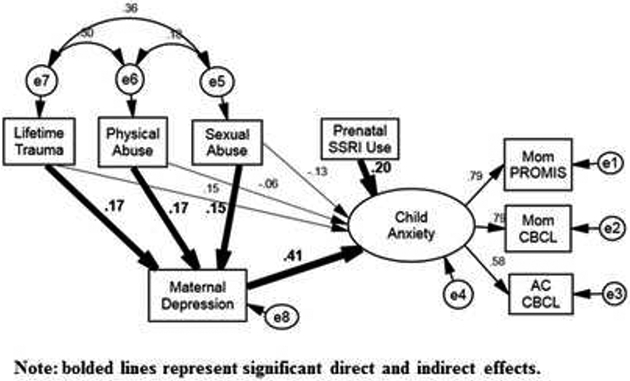
Overall estimated SEM model investigating the prospective role of maternal depression in the association between maternal trauma exposure and offspring anxiety. The model demonstrated good fit (χ2(N = 185) =22.05, df = 14, p = .08, CFI = .96, RMSEA = .06). Significant indirect effects were found for each type of maternal trauma, and maternal lifetime trauma no longer directly predicted child anxiety once the indirect effect of maternal depression was accounted for. Note: Bolded lines represent significant direct and indirect effects. Latent variables are depicted using circles, whereas measured variables are depicted using rectangular boxes
Discussion
Findings from this study both replicate and extend previous results in the area of intergenerational effects of maternal trauma. All types of maternal trauma that were examined (childhood physical abuse, childhood sexual abuse, and lifetime trauma) predicted directly or indirectly to child anxiety outcomes. Additionally, given that our study design measured variables of interest across multiple observers (mothers, alternate caregivers, and observational data collected by researchers in a controlled lab setting), the findings presented in this study advance the existing body of literature by utilizing multiple forms of measurement.
Results of this study suggest that several different types of maternal trauma are relevant predictors of offspring anxiety. Although only maternal lifetime trauma exposure was directly associated with anxiety, all three forms of trauma exposure were indirectly associated with increased offspring anxiety through increases in maternal depression. These results are consistent with previous research suggesting that the type or timing of maternal trauma may not differentially predict offspring outcomes (Dubowitz et al., 2001). It remains possible that the cumulative impact of multiple maternal traumas may lead to differential offspring outcomes compared to singular exposures; however, sample size limitations precluded our examination of this question in the current study.
Maternal depression most strongly and consistently linked maternal trauma history and offspring anxiety. Of note, the measure of maternal depression used in the current study was collected when the children were in preschool, and was predictive of child anxiety disorders during the school age period. These results replicate and extend similar findings noted for offspring internalizing and externalizing problems in general (Koverola et al., 2005; Miranda et al., 2011), and underline the predictive power of maternal depression on later child outcomes.
The finding that maternal depression mediates the relationship between maternal trauma exposure and child anxiety is a notable extension of the literature on intergenerational effects of trauma. While the link between maternal depression and child anxiety is well established in this literature (e.g., Hammen & Brennan, 2003), the role of maternal trauma exposure in predicting maternal depression and subsequent child anxiety is less clear. These findings suggest that many of the negative effects that have been found in offspring of mothers with trauma histories may be directly related to those mothers’ subsequent experiences of depression. This may reflect a general sensitivity to trauma that is first experienced as depression by mothers and is subsequently passed down to the child (either through genetic or environmental factors) as increased risk for anxiety and other internalizing problems. By extension, this finding also implies that mothers who do not go on to develop depression as a result of their traumatic histories may not see similarly negative effects in their offspring’s anxiety development. This has important implications for prevention and clinical intervention. Identifying signs of maternal depression among mothers with histories of trauma may provide an important avenue through which child anxiety problems can be prevented. Existing literature suggests that interventions designed to treat maternal depression can have positive effects on child behavior outcomes (Weissman et al., 2006). Findings from this study suggest that these approaches could also be particularly beneficial in the prevention of child anxiety when geared specifically toward women with trauma histories.
Significant indirect effects were found for parenting (positive engagement and negative engagement) in the case of maternal childhood physical abuse. Specifically, mothers who were physically abused as children displayed lower levels of positive engagement and higher levels of negative engagement with their preschool age children. This led to an increased risk for child anxiety symptoms in school age offspring. These results are consistent with previous research (Collishaw et al., 2007; Rijlaarsdam et al., 2014) and suggest that parenting quality may be a factor worthy of attention in future interventions targeting mothers with histories of childhood physical abuse. More specifically, these findings suggest that parent training may be a useful addition to existing trauma-focused treatments among women who have experienced physical abuse as children. Currently, when adult women are treated for trauma-related problems, the focus is often on the women themselves and their overall symptomatology and functioning. The focus is rarely on their parenting practices or potential intergenerational risks to their children. These findings suggest that we should consider addressing such issues in the context of this form of treatment. Additionally, it may be useful to assess for any history of trauma in the context of prenatal care settings so that expectant mothers might be educated on the potential impact these experiences may have on their moods and parenting practices, and ultimately on their children’s development. Lastly, given that the current study provides evidence that children of these women may be at risk for higher levels of anxiety, it is also important that efforts be made to identify these children at the earliest possible stages of their development to mitigate any negative impact these risk factors may have on their emotional development.
It is interesting to consider why physical, more than sexual, abuse may be linked to the differences in parenting behaviors observed in this study. Some research suggests that a history of childhood physical abuse is specifically related to aggression in adulthood, whereas a history of childhood sexual abuse is specifically linked to adult sexual behaviors (Briere & Runtz, 1990). It is possible that aggression more directly impacts parenting behaviors that can be observed in a structured lab setting, which could explain the present results. Future research should examine mediators (e.g., aggression) linking abuse history with parenting behaviors.
Notably, the intergenerational impact of trauma symptoms likely extends to internalizing problems as a whole rather than a particular risk for anxiety. The current study focused on childhood anxiety both because it is understudied relative to childhood depression, and because of the developmental age of child participants within the study. The prevalence of childhood depression is low relative to anxiety, and anxiety in middle childhood often predicts to risk for later depression (Bittner, A., Egger, H. L., Erkanli, A., Costello, E., Foley, D. L., & Angold, A., 2007; Vasey, Bosmans, & Ollendick, 2014). Therefore, by focusing on risk for anxiety, this study contributes to the literature in a novel way and also tests the hypothesis of intergenerational transmission in a developmentally sensitive way. Still, future research should explore both specific (e.g., child anxiety) and broad (e.g., internalizing behaviors, externalizing behaviors) outcomes in relation to maternal trauma exposure.
In addition to the aforementioned contributions to the literature, the current study’s design provides an important advancement in this area of study. The results reported within this paper were derived from a longitudinal study with multiple methods of assessing maternal trauma exposure and child anxiety, as well as direct laboratory observations of parenting behaviors—a medium that enabled us to observe actual differences in parenting behaviors exhibited by mothers with histories of traumas, rather than relying on self-report measures which may be more prone to bias. As such, we hope that these findings will not only shed light on the relationships that exist in this area, but also provide some methodological considerations for how these variables might potentially be assessed in future research.
Limitations
Notably, the current study design is not sensitive to genetic influences that may be involved in the intergenerational effects of trauma. Some research, particularly in the animal literature, suggests that there might be genetic or epigenetic transmission of trauma effects across generations. For example, Kilpatrick and colleagues (2007) demonstrated that a polymorphism in the serotonin transporter gene may be related to post-traumatic symptomatology, and that this genotype can place offspring at heightened genetic risk for the development of anxiety. Others have demonstrated that intergenerational transmission of trauma-related risk can be attributed to changes in the profile of DNA methylation of several candidate genes, which are then passed on to subsequent offspring (Franklin & colleagues, 2010). Remarkably, trauma-related effects can be passed down through two or more subsequent generations via epigenetic and genetic programming (Dias & Ressler, 2014). While the current study design precludes our ability to investigate genetic or epigenetic influences, future studies should explore this potential mechanism of intergenerational transmission of trauma-related risks, as well as other biomarkers that may be implicated in this relationship.
The present study is unable to determine causality due to its correlational nature; however, the aforementioned nonhuman animal studies provide evidence that parental trauma exposure directly causes changes in offspring biology and behavior. Additionally, research conducted by Smith and colleagues (2011) on intrauterine programming lends support to the claim that maternal experience directly causes changes in offspring in utero.
The associations among maternal trauma exposure variables in this study are significant, yet modest. These modest associations are likely due to differences in measurement across these variables and the different types of maternal trauma exposure each variable represents. While the lifetime trauma variable represents the experience of any traumatic event (e.g., serious car accident, house fire) across a mother’s lifetime, the CTQ Physical Abuse and Sexual Abuse variables represent only the experience of childhood physical abuse or childhood sexual abuse, respectively. Therefore, there is significant correlation among these variables to the extent that there is overlap between them and differences among these variables where there is no overlap. Nonetheless, future studies should compare measures of trauma exposure (e.g., self-report, clinical interview) to determine whether some forms of measurement are more reliable and valid than others.
The current sample is characterized by an overrepresentation of psychopathology (particularly depression) amongst mothers as a result of the sampling strategy used. Mothers in the study also reported high rates of trauma exposure, further highlighting the clinical high-risk of the sample. Consequently, these findings may not be generalizable to non-clinical populations. Mothers enrolled in the study also tended to be Caucasian and of high socioeconomic status, further limiting generalizability to many at-risk populations. Although the present sample remains unique in many aspects, future studies should explore these relationships within populations that are socioeconomically, ethnically, and psychologically diverse to ensure greater generalizability.
The current study assessed parenting quality via laboratory observation of parenting behaviors, rather than self-reports of parenting practices, given questions that have been raised regarding the validity of and potential bias involved in self-report measures of parenting, particularly among parents with histories of trauma (Bailey et al., 2012; Fitzgerald et al., 2005; Rapee, 1997). Nonetheless, excluding such self-report measures may be a limitation of the current study given that these measures may have provided a more comprehensive understanding of the role of parenting in relation to maternal trauma exposure and child anxiety. Future work in this area should assess parenting using laboratory observations, self-report measures, and reports from other raters familiar with the parent’s practices to further the field’s understanding of how the chosen method of measurement may impact these findings.
The present study focused on maternal experiences as a risk factor for offspring anxiety, but recent research suggests that paternal traumatic experiences also play a role in offspring development (e.g., Dias & Ressler, 2014). Additional research is needed to examine individual and combined effects of both maternal and paternal trauma histories on offspring outcomes.
Conclusion
The current study suggests a relationship between maternal exposure to trauma and offspring anxiety. Such findings demonstrate that risk factors for childhood anxiety extend beyond the child’s own lifetime and experiences, and include maternal life experiences that may have occurred before the child was even conceived. Parenting quality and maternal depression were found to serve as mediators in the relationship between maternal trauma and offspring anxiety. These findings suggest that preventative interventions focused on refining parenting skills and alleviating maternal depressive symptoms may reduce offspring risk among dyads in which the mother has experienced trauma. In addition to decreasing offspring risk, such interventions may also improve the psychological wellbeing of women exposed to lifetime traumatic events and abuse during childhood.
References
- Achenbach TM (1991). Child behavior checklist/4-18. Burlington: University of Vermont. [Google Scholar]
- Achenbach TM, Dumenci L, & Rescorla LA (2003). DSM-oriented and empirically based approaches to constructing scales from the same item pools. Journal of clinical child and adolescent psychology, 32(3), 328–340. [DOI] [PubMed] [Google Scholar]
- Bailey HN, DeOliveira CA, Wolfe VV, Evans EM, & Hartwick C (2012). The impact of childhood maltreatment history on parenting: A comparison of maltreatment types and assessment methods. Child abuse & neglect, 36(3), 236–246. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Carbin MG (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical psychology review, 8(1), 77–100. [Google Scholar]
- Bernstein DP, & Fink L (1998). Childhood trauma questionnaire: A retrospective selfreport: Manual. Psychological Corporation. [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Costello E, Foley DL, & Angold A (2007). What do childhood anxiety disorders predict?. Journal of Child Psychology and Psychiatry, 48(12), 1174–1183. [DOI] [PubMed] [Google Scholar]
- Bosquet Enlow M, Englund MM, & Egeland B (2016). Maternal childhood maltreatment history and child mental health: mechanisms in intergenerational effects. Journal of Clinical Child & Adolescent Psychology, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand SR, Brennan PA, Newport DJ, Smith AK, Weiss T, & Stowe ZN (2010). The impact of maternal childhood abuse on maternal and infant HPA axis function in the postpartum period. Psychoneuroendocrinology, 35(5), 686–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buss C, Borders A, Entringer S, Culhane J, Miller G, Grobman W, … & Keenan-Devlin L (2017). 493: Maternal childhood trauma is associated with a pro-inflammatory state during pregnancy. American Journal of Obstetrics and Gynecology, 216(1), S291. [Google Scholar]
- Browne MW, Cudeck R, & Bollen KA (1993). Alternative ways of assessing model fit. Sage Focus Editions, 154, 136. [Google Scholar]
- Collishaw S, Dunn J, O'connor TG, & Golding J (2007). Maternal childhood abuse and offspring adjustment over time. Development and psychopathology, 19(02), 367–383. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, & Kazdin AE (2005). Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological bulletin, 131(4), 483. [DOI] [PubMed] [Google Scholar]
- Dias BG, & Ressler KJ (2014). Parental olfactory experience influences behavior and neural structure in subsequent generations. Nature neuroscience, 17(1), 89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiLillo D, Fortier MA, Hayes SA, Trask E, Perry AR, Messman-Moore T, Fauchier A, & Nash C (2006). Retrospective assessment of childhood sexual and physical abuse a comparison of scaled and behaviorally specific approaches. Assessment, 13(3), 297–312. [DOI] [PubMed] [Google Scholar]
- Dubowitz H, Black MM, Kerr MA, Hussey JM, Morrel TM, Everson MD, & Starr RH (2001). Type and timing of mothers' victimization: effects on mothers and children. Pediatrics, 107(4), 728–735. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Franklin CL, & Gray MJ (2008). The SCID PTSD module's trauma screen: Validity with two samples in detecting trauma history. Depression and Anxiety, 25(9), 737. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, & Robinson EA (1981). Dyadic parent-child interaction coding system. Seattle, WA: Parenting Clinic, University of Washington. [DOI] [PubMed] [Google Scholar]
- Fitzgerald MM, Shipman KL, Jackson JL, McMahon RJ, & Hanley HM (2005). Perceptions of parenting versus parent-child interactions among incest survivors. Child Abuse & Neglect, 29(6), 661–681. [DOI] [PubMed] [Google Scholar]
- Franklin CL, Sheeran T, & Zimmerman M (2002). Screening for trauma histories, posttraumatic stress disorders (PTSD) and subthreshold PTSD in psychiatric outpatients. Psychological Assessment, 14(4), 467. [DOI] [PubMed] [Google Scholar]
- Franklin TB, Russig H, Weiss IC, Gräff J, Linder N, Michalon A, Vizi S & Mansuy IM (2010). Epigenetic transmission of the impact of early stress across generations. Biological psychiatry, 68(5), 408–415. [DOI] [PubMed] [Google Scholar]
- Hammen C, & Brennan PA (2003). Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of general psychiatry, 60(3), 253–258. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde G (2009). Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press. [Google Scholar]
- Hooper D, Coughlan J, & Mullen M (2008). Structural equation modeling: guidelines for determining model fit. Electronic Journal of Business Research Methods, 6(1), 53–60. [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: a Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Hudson JL, Comer JS, & Kendall PC (2008). Parental responses to positive and negative emotions in anxious and nonanxious children. Journal of Clinical Child & Adolescent Psychology, 37(2), 303–313.cv [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin DE, Gross HE, Stucky BD, Thissen D, DeWitt EM, Lai JS, Amtmann D, Khastou L, Varni JW, & DeWalt DA (2012). Development of six PROMIS pediatrics proxy-report item banks. Health and quality of life outcomes 10, no. 1: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson KC, Smith AK, Stowe ZN, Newport DJ, & Brennan PA (2016). Preschool outcomes following prenatal antidepressant exposure: Differences in language and behavior, but not cognitive function. The Journal of clinical psychiatry, 77(2), e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovanovic T, Smith A, Kamkwalala A, Poole J, Samples T, Norrholm SD, Ressler KJ & Bradley B (2011). Physiological markers of anxiety are increased in children of abused mothers. Journal of child psychology and psychiatry, 52(8), 844–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juul SH, Hendrix C, Robinson B, Stowe ZN, Newport DJ, Brennan PA, & Johnson KC (2016). Maternal early-life trauma and affective parenting style: the mediating role of HPA-axis function. Archives of women's mental health, 19(1), 17–23. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Koenen KC, Ruggiero KJ, Acierno R, Galea S, Resnick HS, Roitzsch J, Boyle J & Gelernter J (2007). The serotonin transporter genotype and social support and moderation of posttraumatic stress disorder and depression in hurricane-exposed adults. The American journal of psychiatry, 164(11), 1693–1699. [DOI] [PubMed] [Google Scholar]
- Kline RB (2011). Principles and Practice of Structural Equation Modeling, Third Edition - Kline Rex B. - Google Books. [Google Scholar]
- Koverola C, Papas MA, Pitts S, Murtaugh C, Black MM, & Dubowitz H (2005). Longitudinal investigation of the relationship among maternal victimization, depressive symptoms, social support, and children’s behavior and development. Journal of Interpersonal Violence, 20(12), 1523–1546. [DOI] [PubMed] [Google Scholar]
- Lewis G, Rice F, Harold GT, Collishaw S, & Thapar A (2011). Investigating environmental links between parent depression and child depressive/anxiety symptoms using an assisted conception design. Journal of the American Academy of Child & Adolescent Psychiatry, 50(5), 451–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min MO, Minnes S, Kim H, & Singer LT (2013). Pathways linking childhood maltreatment and adult physical health. Child abuse & neglect, 37(6), 361–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda JK, de la Osa N, Granero R, & Ezpeleta L (2013). Multiple mediators of the relationships among maternal childhood abuse, intimate partner violence, and offspring psychopathology. Journal of interpersonal violence, 28(14), 2941–2965. [DOI] [PubMed] [Google Scholar]
- Morrel TM, Dubowitz H, Kerr MA, & Black MM (2003). The effect of maternal victimization on children: A cross-informant study. Journal of Family Violence, 18(1), 29–41. [Google Scholar]
- Muris P, & Broeren S (2009). Twenty-five years of research on childhood anxiety disorders: Publication trends between 1982 and 2006 and a selective review of the literature. Journal of Child and Family Studies, 18(4), 388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myhre MC, Dyb GA, Wentzel-Larsen T, Grøgaard JB, & Thoresen S (2014). Maternal childhood abuse predicts externalizing behaviour in toddlers: a prospective cohort study. Scandinavian Journal of Social Medicine, 42(3), 263–269. [DOI] [PubMed] [Google Scholar]
- Nanni V, Uher R, & Danese A (2012). Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. American Journal of Psychiatry, 169, 141–151. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, & Locke TF (2001). Intergenerational cycle of maltreatment: A popular concept obscured by methodological limitations. Child Abuse & Neglect, 25(9), 1219–1240. [DOI] [PubMed] [Google Scholar]
- Rapee RM (1997). Potential role of childrearing practices in the development of anxiety and depression. Clinical Psychology Review, 17, 47–67. [DOI] [PubMed] [Google Scholar]
- Rijlaarsdam J, Stevens GW, Jansen PW, Ringoot AP, Jaddoe VW, Hofman A, Ayer L, Verhulst FC, Hudziak JJ and Tiemeier H (2014). Maternal childhood maltreatment and offspring emotional and behavioral problems: Maternal and paternal mechanisms of risk transmission. Child maltreatment, 19(2), pp.67–78. [DOI] [PubMed] [Google Scholar]
- Robinson BA, Azores-Gococo N, Brennan PA, & Lilienfeld SO (2016). The Roles of Maternal Psychopathic Traits, Maternal Antisocial Personality Traits, and Parenting in the Development of Child Psychopathic Traits. Parenting, 16(1), 36–55. [Google Scholar]
- Schechter JC, Brennan PA, Smith AK, Stowe ZN, Newport DJ, & Johnson KC (2017). Maternal Prenatal Psychological Distress and Preschool Cognitive Functioning: the Protective Role of Positive Parental Engagement. Journal of abnormal child psychology, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AK, Brennan PA, Galanti MB, Newport DJ, Cubells JF, & Stowe ZN (2009). Evaluation of child behavioral problems in the offspring of women with early sexual abuse history: Implications of transgeneration effects. Biological Psychiatry, 64, 1S–244S. [Google Scholar]
- Smith AK, Conneely KN, Newport DJ, Kilaru V, Schroeder JW, Pennell PB, … & Brennan PA (2012). Prenatal antiepileptic exposure associates with neonatal DNA methylation differences. Epigenetics, 7(5), 458–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AK, Newport DJ, Ashe MP, Brennan PA, LaPrairie JL, Calamaras M, … Stowe ZN (2011). Predictors of neonatal hypothalamic–pituitary–adrenal axis activity at delivery. Clinical Endocrinology, 75(1), 90–95. 10.1111/j.1365-2265.2011.03998.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G, Staton-Tindall M, Gustman B, Freer B, Clark JJ, Dye H, & Sprang K (2013). The impact of trauma exposure on parenting stress in rural America. Journal of Child & Adolescent Trauma, 6(4), 287–300. [Google Scholar]
- Suveg C, Sood E, Barmish A, Tiwari S, Hudson JL, & Kendall PC (2008). " I'd rather not talk about it": Emotion parenting in families of children with an anxiety disorder. Journal of Family Psychology, 22(6), 875.c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R (2007). Mothers' violence victimization and child behavior problems: Examining the link. American journal of orthopsychiatry, 77(2), 306. [DOI] [PubMed] [Google Scholar]
- Van der Sluis CM, van Steensel FJ, & Bögels SM (2015). Parenting and children’s internalizing symptoms: How important are parents?. Journal of child and family studies, 24(12), 3652–3661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Sluis CM, van Steensel FJA, & Bögels SM (2015). Parenting clinically anxious versus healthy control children aged 4–12 years. Journal of Anxiety Disorders, 32, 1–7. [DOI] [PubMed] [Google Scholar]
- van Ee E, Kleber RJ, & Mooren TT (2012). War trauma lingers on: Associations between maternal posttraumatic stress disorder, parent-child interaction, and child development. Infant Mental Health Journal, 33(5), 459–468. [DOI] [PubMed] [Google Scholar]
- Vasey MW, Bosmans G, & Ollendick TH (2014). The developmental psychopathology of anxiety. In Handbook of developmental psychopathology (pp. 543–560). Springer US. [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, Hughes CW, Garber J, Malloy E, King CA & Cerda G (2006). Remissions in maternal depression and child psychopathology: a STAR* D-child report. Jama, 295(12), 1389–1398. [DOI] [PubMed] [Google Scholar]
- Zvara BJ, Mills-Koonce WR, Carmody KA, Cox M, & Family Life Project Key Investigators. (2015). Childhood sexual trauma and subsequent parenting beliefs and behaviors. Child abuse & neglect, 44, 87–97. [DOI] [PMC free article] [PubMed] [Google Scholar]


