ABSTRACT - BACKGROUND:
The use of Appendicitis Inflammatory Response clinical score in patients with suspected acute appendicitis makes the diagnosis more objective and accurate.
AIMS:
The aim of this study was to prospectively compare two groups with suspected acute appendicitis, analyzing the number of imaging tests requested, waiting time in the emergency department, until definition of conduct, as well as the sensitivity and specificity of this diagnostic method.
METHODS:
This is a prospective randomized study comparing 55 patients submitted to clinical-radiological diagnosis according to the routine of the service (control group), with another 55 patients submitted to the Appendicitis Inflammatory Response score flowchart (intervention group).
RESULTS:
Waiting time for defining the intervention group’s conduct was 1.5 h shorter than the control group (p=0.02). Computed tomography was performed in 42 patients in the control group, compared with 25 in the intervention group (p=0.001). The impact of the flowchart based on the Appendicitis Inflammatory Response score of the cases compared to the control group was the reduction of appendectomies with a normal-appearing appendix from 5 to 1 and an increase in the exclusion of appendicitis diagnoses. The use of the Appendicitis Inflammatory Response score resulted in a diagnostic specificity of 92%, compared to 29% in the control group.
CONCLUSIONS:
The use of the Appendicitis Inflammatory Response score reduced the waiting time for the diagnosis of acute appendicitis, decreased the number of imaging tests, and increased diagnostic specificity of the disease.
HEADINGS: Appendicitis, Clinical Diagnosis, Tomography
RESUMO - RACIONAL:
A utilização do escore clínico Appendicitis Inflammatory Response em pacientes com suspeita de apendicite aguda torna o diagnóstico mais objetivo e preciso.
OBJETIVOS:
Comparar prospectivamente dois grupos com suspeita de apendicite aguda, analisando o número de exames de imagem solicitados, o tempo de espera no Pronto-Socorro, até a definição da conduta, bem como a sensibilidade e especificidade desse método diagnóstico.
MÉTODOS:
Estudo prospectivo randomizado comparando 55 pacientes submetidos ao diagnóstico clínico-radiológico de acordo com a rotina do Serviço (grupo controle), com outros 55 pacientes submetidos ao fluxograma do escore Appendicitis Inflammatory Response (grupo intervenção).
RESULTADOS:
O tempo de espera para definir a conduta do grupo intervenção foi 1,5 hora menor do que o grupo controle (p=0,02). A tomografia computadorizada foi realizada em 42 pacientes do grupo controle, em comparação com 25 do grupo intervenção (p=0,001). O impacto do fluxograma baseado no escore Appendicitis Inflammatory Response dos casos em relação ao grupo controle foi a redução de apendicectomias com apêndice de aparência normal de 5 para 1 e um aumento na exclusão de diagnósticos de apendicite. O uso do escore Appendicitis Inflammatory Response resultou em especificidade diagnóstica de 92%, comparado a 29% no grupo controle.
CONCLUSÕES:
A utilização do escore Appendicitis Inflammatory Response reduziu o tempo de espera para o diagnóstico de apendicite aguda, diminuiu o número de exames de imagem e aumentou a especificidade diagnóstica da doença.
DESCRITORES: Apendicite, Diagnóstico Clínico, Tomografia
INTRODUCTION
Acute appendicitis (AA) is a common cause of abdominal pain at all ages, with a lifetime prevalence of one case in seven people 15 . In the initial phase, the symptoms can be vague and nonspecific, especially in women 15 . The final diagnosis is usually based on clinical history, physical examination, and related laboratory and imaging tests 6 , 17 .
Early diagnosis of AA is essential for reducing morbidity and mortality associated with advanced stages of the disease. Therefore, imaging tests such as ultrasound (US) and tomography are often used to clarify the diagnosis of AA 2 , 3 . However, performing routine imaging tests for patients with abdominal pain can mean an increase in hospital costs and the length of stay of patients in the emergency care units, until the definitive conduct 13 , 14 .
Consequently, several diagnostic scores have been developed to aid in the diagnosis of AA, derived from systematic clinical analyses 5 , 7 , 12 . These scores aim to reduce uncertainty by standardizing the collection and interpretation of clinical and laboratory data 8 . Risk stratification using clinical scores has the potential to improve the diagnosis of AA and the management of hospital resources 6 , 18 .
Among the clinical scores described, the Appendicitis Inflammatory Response (AIR) was superior to the Alvarado score, most used in clinical studies, with superior accuracy in the evaluation of patients with suspected AA, reducing the need for imaging tests and the number of hospital admissions for low-risk patients without compromising investigation safety 1 , 9 .
Some studies have evaluated the use of scores to aid decision-making in suspected cases of AA, providing agility in follow-up or surgical indication, in cases with low-risk or high-risk scores, respectively 4 , 10 . However, the use of the flowchart suggested by the consensus of AA is still not a reality among emergency physicians.
The objective of this study was to evaluate the effectiveness of the use of the AIR score against a suspicion of AA in a referral hospital for the care of these patients and to analyze the use of imaging tests and the length of stay of the patient in the emergency unit.
METHODS
This is a prospective randomized study comparing patients admitted to the emergency department of São José Hospital Municipal from Joinville, with suspected AA. Patients were randomly divided into two groups: control or intervention, according to a computerized list generated by the Random Allocation Software program 11 .
The control group included patients managed according to the routines and procedures currently used in the emergency surgery service, for the investigation of suspected cases of AA.
The intervention group followed the flowchart (Figure 1) adapted from Saverio et al. 4 . Patients under 40 years of age, classified as low risk, were followed up and were instructed to return to the emergency department at any time or routinely for reassessment at the Hospital’s General Surgery Outpatient Clinic.
Figure 1 -. Flowchart used in the research.
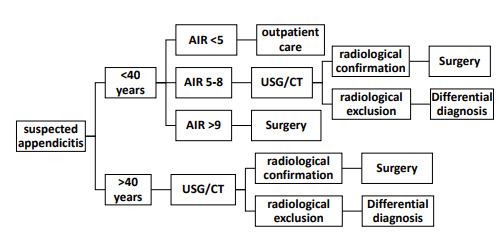
AIR: Appendicitis Inflammatory Response; USG: Ultrasonography/CT: computed tomography.
The AIR score on signs and symptoms found in patients with clinical suspicion of AA is described in Table 1.
Table 1 -. Score used in patients with clinical suspicion of acute appendicitis to determine the Appendicitis Inflammatory Response score.
| Symptoms, signs, and laboratory tests | Score | |
|---|---|---|
| Vomiting | 1 | |
| Pain in the right iliac region | 1 | |
| Tenderness and rigidity in the right iliac region | Light | 1 |
| Moderate | 2 | |
| severe | 3 | |
| Temperature >38.5°C | 1 | |
| Moderate-severe | 4 | |
| Leukocytes (x109) | ≥10 and <15 | 1 |
| ≥15 | 2 | |
| Neutrophils % | ≥70 and <85 | 1 |
| ≥85 | 2 | |
The expected sample for the study was 100 patients, based on a retrospective analysis of appendectomies in the past 3 years of the Service. Data collection took place between April and September 2021, totaling 110 cases.
Inclusion criteria were patients, over 16 years old, seen at the hospital emergency department with suspicious clinical symptoms or a definite diagnosis of AA. Exclusion criteria were younger than 15 years.
Data collected include age, sex, comorbidities, information on imaging test results (computed tomography CT scans and ultrasonography - USG), length of stay of the patient in the emergency department (beginning of care until discharge or admission), and macroscopic and histopathological analysis of the appendix of the cases submitted to surgical treatment.
For statistics, analysis of variance or nonparametric Kruskal-Wallis test was used to compare quantitative variables, and the association between qualitative variables was evaluated using the chi-square test.
This research was approved by the Research Ethics Committee of São José Municipal Hospital, Joinville-SC, under number 5362, with informed consent.
RESULTS
The flowchart used in this research is shown in Figure 1.
Most patients were young adults between 16 and 40 years (71%), with a mean age of 26.3 years. There was a slight predominance of males (51.8%), without statistical significance (p=0.7).
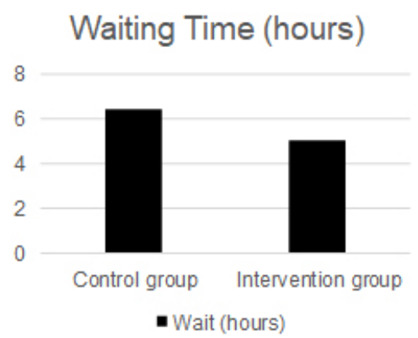
The patient’s waiting time in the emergency department, until being admitted for surgery or being discharged for outpatient return, was on average 6.4 h in the control group and 5 h in the intervention group with statistical significance (p=0.03) (Figure 2).
Figure 2 -. Waiting time in hours of the patient in the emergency department, in the control group and intervention group.
A greater number of imaging tests were performed in patients in the control group. US was performed in 23 patients in the control group compared to 22 indications in the intervention group, without statistical significance (p=0.2) (Table 2). CT was performed in 42 patients in the control group compared to 25 indications in the intervention group, with statistical significance (p=0.001) (Table 3).
Table 2 -. Abdominal ultrasound performed or not in patients in the control and intervention groups (p=0.2).
| USG | CONTROL GROUP | INTERVENTION GROUP |
|---|---|---|
| Did not perform | 32 | 33 |
| Perform | 23 | 22 |
USG: Ultrasonography.
Table 3 -. Abdominal computed tomography performed or not in patients in the control and intervention groups (p=0.001).
| CT | CONTROL GROUP | INTERVENTION GROUP |
|---|---|---|
| Did not perform | 13 | 30 |
| Perform | 42 | 25 |
CT: computed tomography.
Surgical treatment was not indicated in 20% of patients in the intervention group versus 3% in the control group. None of the patients in whom surgery was contraindicated were readmitted to the emergency department for investigation or treatment of AA.
The number of appendectomies without histopathological changes was higher in the control group compared to that in the intervention group (9 vs. 1.5%). The diagnostic sensitivity of both the groups was 100%, with specificity being 29% in the control group and 92% in the intervention group (Tables 4 and 5).
Table 4 -. Sensitivity and specificity of the clinical diagnosis of acute appendicitis in the control group (sensitivity 100%; specificity 29%).
| CONTROL GROUP | APPENDICITIS | NORMAL APPENDIX |
|---|---|---|
| Positive clinical diagnosis | 48 | 5 |
| Negative clinical diagnosis | 0 | 2 |
Table 5 -. Sensitivity and specificity of the Appendicitis Inflammatory Response score in the diagnosis of acute appendicitis in the intervention group (sensitivity 100%; specificity 92%).
| INTERVENTION GROUP | APPENDICITIS | NORMAL APPENDIX |
|---|---|---|
| Positive AIR flowchart | 42 | 1 |
| Negative AIR flowchart | 0 | 12 |
AIR: Appendicitis Inflammatory Response.
Patients who scored low on the AIR score or had differential diagnoses such as urolithiasis, pelvic inflammatory disease, and gastroenteritis were followed up on an outpatient basis with treatment aimed at these etiologies (Table 6).
Table 6 -. Differential diagnosis of three patients treated with suspected acute appendicitis.
| Differential diagnosis | Number of cases |
|---|---|
| Urinary lithiasis | 1 |
| Acute cholecystitis | 1 |
| Right colon tumor | 1 |
DISCUSSION
CT was the most accurate examination, diagnosing AA in 77.6% of patients, compared to 51% of those who underwent US in both groups. CT was necessary to diagnose AA in 13 patients who underwent US with inconclusive results 16 .
All patients in the intervention group who received high risk according to the AIR underwent surgical treatment without performing additional tests, with a histopathological diagnosis of AA. In the control group, all patients at high risk according to the AIR underwent CT before appendectomy and no appendices without histopathological changes were observed in patients at high risk. Therefore, the AIR score flowchart proved to be safe in indicating surgical treatment without performing imaging tests for these patients.
A critical analysis regarding the AIR score, observed during data collection, was the subjectivity in the abdominal defense criterion. The original article describing AIR does not set out objective criteria for scoring. This item receives a score from 1 to 3, according to the examiner’s assessment. However, a definition in the final conduct was noticed by the weight of this score. A more objective criterion would facilitate the application of the score.
It was possible to determine a difference in the waiting time of patients in the emergency department until the definition of the AA diagnosis. Patients in the control group waited 1.4 h longer than patients in the intervention group. Therefore, the flowchart applied decreased by more than 1 h, until the final conduct, hospital discharge, or surgical treatment.
As for the final outcome of the cases, there were no false-negative results in the diagnosis of AA in the control group, as in the flowchart based on the AIR score of the intervention group, therefore giving a sensitivity of 100%. Regarding specificity, there was a difference between the group (29 control vs. 92% intervention), demonstrating the effectiveness of the flowchart based on the AIR score to safely rule out the diagnosis of appendicitis, reducing the frequency of appendectomies with the appendix showing a normal appearance.
CONCLUSION
The flowchart used in this study proved to be effective in reducing the patient’s waiting time in the emergency department and also in reducing complementary examinations for the diagnosis of abdominal pain suspected of AA. The reduction in the number of requested imaging tests observed in the intervention group implies lower hospital costs.
How to cite this article: Deboni VS, Rosa MI, Lima AC, Graciano AJ, Garcia CE. The Appendicitis Inflammatory Response score for acute appendicitis: is it important for early diagnosis? ABCD Arq Bras Cir Dig. 2022;35:e1686. https://doi.org/10.1590/0102-672020220002e1686
Financial source: None
Central Message
Early diagnosis of acute appendicitis is essential for reducing morbidity and mortality associated with advanced stages of the disease. Therefore, imaging tests such as ultrasound and tomography are often used to clarify the diagnosis of acute appendicitis [2, 3]. However, performing routine imaging tests for patients with abdominal pain can mean an increase in hospital costs and the length of stay of patients in the emergency care units, until the definitive conduct.
Perspectives
The use of Appendicitis Inflammatory Response (AIR) score reduced the waiting time for the diagnosis of acute appendicitis, decreased the number of imaging tests, and increased diagnostic specificity of the disease.
REFERENCES
- 1.Andersson M, Kolodziej B, Andersson RE, STRAPPSCORE Study Group Randomized clinical trial of Appendicitis Inflammatory Response score-based management of patients with suspected appendicitis. Br J Surg. 2017;104(11):1451–1461. doi: 10.1002/bjs.10637. [DOI] [PubMed] [Google Scholar]
- 2.Brenner DJ, Hall EJ. Computed tomography-an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 3.Castro AA, Skare TL, Yamauchi FI, Tachibana A, Ribeiro SPP, Fonseca EKUN, et al. Diagnostic value of c-reactive protein and the influence of visceral fat in patients with obesity and acute appendicitis. ABCD Arq Bras Cir Dig. 2018;31(1):e1339. doi: 10.1590/0102-672020180001e1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, Boermeester M, Sartelli M, Coccolini F, Tarasconi A, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(1):27–27. doi: 10.1186/s13017-020-00306-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fleischman RJ, Devine MK, Yagapen MAN, Steichen AJ, Hansen ML, Zigman AF, et al. Evaluation of a novel pediatric appendicitis pathway using high- and low-risk scoring systems. Pediatr Emerg Care. 2013;29(10):1060–1065. doi: 10.1097/PEC.0b013e3182a5c9b6. [DOI] [PubMed] [Google Scholar]
- 6.Laupacis A, Sekar N, Stiell IG. Clinical prediction rules. A review and suggested modifications of methodological standards. JAMA. 1997;277(6):488–494. [PubMed] [Google Scholar]
- 7.Lintula H, Kokki H, Kettunen R, Eskelinen M. Appendicitis score for children with suspected appendicitis. A randomized clinical trial. Langenbecks Arch Surg. 2009;394(6):999–1004. doi: 10.1007/s00423-008-0425-0. [DOI] [PubMed] [Google Scholar]
- 8.Lintula H, Kokki H, Pulkkinen J, Kettunen R, Gröhn O, Eskelinen M. Diagnostic score in acute appendicitis. Validation of a diagnostic score (Lintula score) for adults with suspected appendicitis. Langenbecks Arch Surg. 2010;395(5):495–500. doi: 10.1007/s00423-010-0627-0. [DOI] [PubMed] [Google Scholar]
- 9.Mán E, Simonka Z, Varga A, Rárosi F, Lázár G. Impact of the Alvarado score on the diagnosis of acute appendicitis: comparing clinical judgment, Alvarado score, and a new modified score in suspected appendicitis: a prospective, randomized clinical trial. Surg Endosc. 2014;28(8):2398–2405. doi: 10.1007/s00464-014-3488-8. [DOI] [PubMed] [Google Scholar]
- 10.Ohmann C, Franke C, Yang Q. Clinical benefit of a diagnostic score for appendicitis: results of a prospective interventional study. German Study Group of Acute Abdominal Pain. Arch Surg. 1999;134(9):993–996. doi: 10.1001/archsurg.134.9.993. [DOI] [PubMed] [Google Scholar]
- 11.Random Allocation Software. http://mahmoodsaghaei.tripod.com
- 12.Sammalkorpi HE, Leppäniemi A, Lantto E, Mentula P. Performance of imaging studies in patients with suspected appendicitis after stratification with adult appendicitis score. World J Emerg Surg. 2017;12:6–6. doi: 10.1186/s13017-017-0119-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sammalkorpi HE, Mentula P, Leppäniemi A. A new adult appendicitis score improves diagnostic accuracy of acute appendicitis-a prospective study. BMC Gastroenterol. 2014;14:114–114. doi: 10.1186/1471-230X-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sammalkorpi HE, Mentula P, Savolainen H, Leppäniemi A. The introduction of adult appendicitis score reduced negative appendectomy rate. Scand J Surg. 2017;106(3):196–201. doi: 10.1177/1457496916683099. [DOI] [PubMed] [Google Scholar]
- 15.Stephens PL, Mazzucco JJ. Comparison of ultrasound and the Alvarado score for the diagnosis of acute appendicitis. Conn Med. 1999;63(3):137–140. [PubMed] [Google Scholar]
- 16.Terasawa T, Blackmore CC, Bent S, Kohlwes RJ. Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med. 2004;141(7):537–546. doi: 10.7326/0003-4819-141-7-200410050-00011. [DOI] [PubMed] [Google Scholar]
- 17.Tsze DS, Asnis LM, Merchant RC, Amanullah S, Linakis JG. Increasing computed tomography use for patients with appendicitis and discrepancies in pain management between adults and children: an analysis of the NHAMCS. Ann Emerg Med. 2012;59(5):395–403. doi: 10.1016/j.annemergmed.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 18.Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules. Applications and methodological standards. N Engl J Med. 1985;313(13):793–799. doi: 10.1056/NEJM198509263131306. [DOI] [PubMed] [Google Scholar]


