Abstract
Context
Clinicians use brain magnetic resonance imaging (MRI) to discuss neurodevelopmental prognosis with parents of neonates with hypoxic-ischemic encephalopathy (HIE) treated with therapeutic hypothermia (TH).
Purpose
To investigate how clinicians and parents discuss these MRI results in the context of HIE and TH and how these discussions could be facilitated and more meaningful for parents.
Procedures
Mixed-methods surveys with open-ended and closed-ended questions were completed by two independent groups. (1) Clinicians responded to clinical vignettes of neonates with HIE treated with TH with various types of clinical features, evolution and extent of brain injury and questions about how they discuss brain MRI results in this context. (2) Parents of children with HIE treated with TH responded to questions about the discussion of MRI that they had while still in the neonatal intensive care unit and were asked to place it in perspective with the outcomes of their child when he/she reached at least 2 years of age. Open-ended responses were analyzed using a thematic analysis approach. Closed-ended responses are presented descriptively.
Results
Clinicians reported uncertainty, lack of confidence, and limitations when discussing brain MRI results in the context of HIE and TH. Brain MRI results were “usually” (53%) used in the prognostication discussion. When dealing with day-2 brain MRIs performed during TH, most clinicians (40%) assumed that the results of these early MRIs were only “sometimes” accurate and only used them “sometimes” (33%) to discuss prognosis; a majority of them (66%) would “always” repeat imaging at a later time-point to discuss prognosis. Parents also struggled with this uncertainty, but did not discuss limitations of MRI as often. Parents raised the importance of the setting where the discussion took place and the importance to inform them as quickly as possible. Clinicians identified strategies to improve these discussions, including interdisciplinary approach, formal training, and standardized approach to report brain MRI. Parents highlighted the importance of communication skills, the stress, the hope surrounding their situation, and the need to receive answers as soon as possible. The importance of showing the pictures or making representative drawing of the injury, but also highlighting the not-injured brain, was also highlighted by parents.
Conclusions
Discussing brain MRI results for neonates with HIE treated with TH are challenging tasks for clinicians and daunting moments for parents.
Keywords: Birth asphyxia, Brain, Clinician, Magnetic resonance imaging, Neonate, Parents, Neonatal encephalopathy, Hypothermia
Abbreviations: MRI, magnetic resonance imaging; HIE, hypoxic-ischemic encephalopathy; NICU, neonatal intensive care unit; TH, therapeutic hypothermia
Highlights
-
•
Discussing brain MRI results for neonates with HIE are challenging tasks for clinicians and daunting moments for parents.
-
•
Clinicians reported uncertainty, lack of confidence, and limitations, when discussing brain MRI results in the context of HIE and TH.
-
•
For parents, most important themes were communication skills, stress, hope, and pressing need to receive answers.
-
•
There is an urgent need to develop a systemic and interdisciplinary approach to prognostication.
-
•
There is an urgent need to standardize reporting of brain MRI results.
-
•
There is an urgent need to further train clinicians how to properly discuss these MRI results with parents.
-
•
These solutions may help facilitate difficult decision-making discussions and make these discussions more meaningful for parents.
1. Introduction
Neonates surviving hypoxic-ischemic encephalopathy (HIE) treated with therapeutic hypothermia (TH) remain at significant, but uncertain risk of long-term neurodevelopmental sequelae. Historically, prognostication of long-term outcomes has been based largely on clinical history and on evolution of neurological assessment during the first week of life [1]. Over the last two decades, advances in magnetic resonance imaging (MRI) techniques have allowed the visualization of the extent of brain injury and research has been ongoing to correlate MRI findings in the postnatal period with long-term outcomes in neonates with HIE treated with TH [[1], [2], [3], [4]]. However, prognostication remains difficult [5]. Prognostic uncertainty arises from the plasticity of the developing infant's brain and the potential of early therapeutic interventions such as TH [1,6]. Knowledge, training, professional and personal experience have also been shown to influence prognostication [7,8]. This prognostic uncertainty may result in a lack of consistency between clinicians [9].
MRI and prognosis are key topics in discussions with parents of neonates with HIE treated with TH [4]. Typically, a formal meeting is arranged between clinicians and parents to discuss the results of brain MRIs performed on days 4–10 of life and the possible prognosis of their neonate. Little is known about how this given prognosis or its timing impact parents' views about their neonate. Moreover, recent research has indicated that day-2 brain MRIs performed during TH in the first days of life can already accurately identify the presence and the extent of brain injury [[10], [11], [12], [13], [14], [15]], even if there remains concerns that the full extent of injuries may not yet be well visualized at that timing [16], especially in centers not used to interpreting these early imaging in the context of HIE and TH. These results may warrant earlier discussion of MRI results with parents. Earlier prognostication with MRI may also accelerate decision-making processes regarding goals of care in the most severe cases before such decisional options (i.e., elective extubation) are no longer available or acceptable [17]. This study included a subgroup of parent respondents whose neonates received an early brain MRI on day-2 of life during TH, in addition to the standard of care MRI performed after completion of TH around day 10 of life at our institution.
Due to the challenges of prognostication in the postnatal period, it is important to explore clinicians' actual use of brain MRI in the context of HIE and TH and parents' evaluation of it. We hypothesized that clinicians may often not be at ease with discussing brain MRI results for neonates with HIE treated with TH and that parents' expectations and preferences in the context of this overwhelming situation may often not be met. Receiving MRI results early in the course of the disease may help parents adjust more easily to the situation rather than waiting for 4–10 days as it is currently the standard of care. This study was thus designed to investigate the challenges met by clinicians in the discussion of brain MRI results for neonates with HIE treated with TH and the parents' perspective on the topic.
2. Materials and methods
We used mixed-methods surveys given to (1) clinicians who discuss brain MRI results of neonates with HIE with parents; and (2) parents of children with HIE treated with TH, who were communicated these results. Participants were recruited from a single tertiary-level neonatal intensive care unit, which is a referral centre for TH. The research protocol was approved by the local institutional ethics review board, and we obtained informed consent for all survey respondents.
2.1. Data collection
We sent all clinicians who discuss brain MRI results with parents at the institution an electronic survey with anonymized answers via SurveyMonkey® [18]. The survey prompted respondents to consider four clinical vignettes (Supplemental material), which described anonymized clinical history and brain MRI results of neonates with HIE treated with TH who presented with various types of clinical features, evolution and extent of brain injury. In addition, respondents were asked to give their opinion on how they would discuss these brain MRI results with parents and to answer general questions about their practice. The potential prognosis was placed in the perspective of the evolution of these children at or beyond 3 years of age. In addition, the survey asked the clinicians general questions about their practices.
We also surveyed parents of neonates with HIE treated with TH who expressed interest to participate in the study to a member of the local Infant Follow-up Clinic. Parents were selected when their infants reached at least 2 years of age, and not directly after the neonatal intensive care unit (NICU) stay, so that they could put into perspective what they were told in the NICU about MRI results and compare with how their child was doing at the time of the survey. A subgroup of these neonates was enrolled in an imaging study that included the early brain MRI on day 2–3 of life during TH, in addition to the standard of care MRI performed around day 10 of life. Parents of neonates with HIE treated with TH were categorized in four groups: (1) no brain injury and only one post-cooling MRI; (2) no brain injury and two MRIs (1 day-2 MRI during TH and one after TH); (3) brain injury and only one MRI after TH; and (4) brain injury and two MRIs (one day-2 MRI during TH and one after TH). A general letter about the study was first sent to these parents. Then, a member of the local Infant Follow-up Clinic – the multidisciplinary clinic that follows the neurodevelopment of all these neonates with HIE up to the age of 3 years – contacted the parents to discuss the study and see if they agreed to be contacted by the research team. If they agreed, a member of the research team contacted them to obtain consent and discussed how they preferred to answer the questionnaire focused on the use of brain MRI. Parents were invited to answer a semi-structured questionnaire focused on the use of brain MRI either via an online survey (SurveyMonkey® [18]), a paper survey (with open and closed questions), or an in-person interview. One or both parents together could participate in the survey.
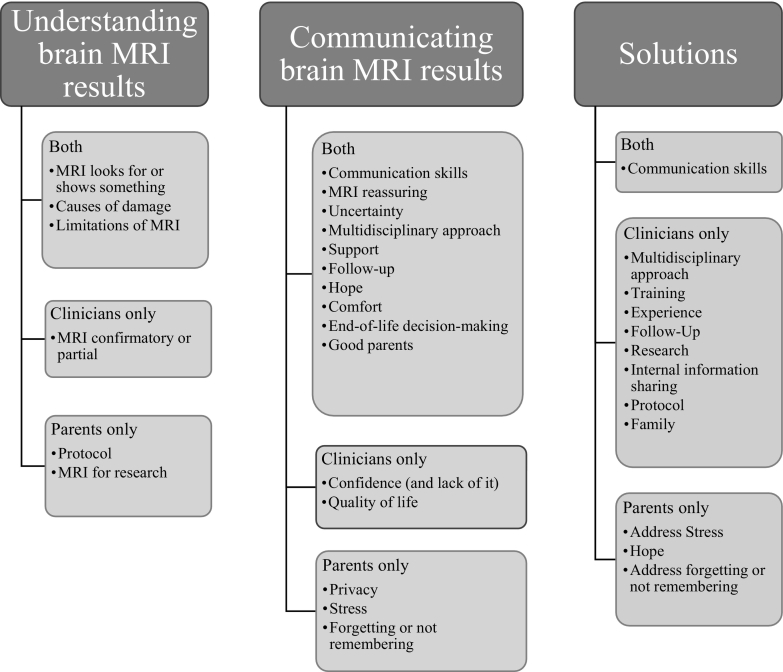
2.2. Data analysis
Answers to closed questions from clinicians and parents were presented using descriptive statistics. Categorical data were reported as frequencies and percentages. Answers to open-ended questions from clinicians and parents were analyzed using a thematic analysis approach. The analysis team consisted of 1 neonatologist and clinician-scientist (AF) and 2 non-physician scholars (AC and ER) who specialize in mixed-methods empirical investigations related to ethics issues, as well as 1 neonatologist and clinician-scientist specialized in birth asphyxia (PW). The research team identified key concepts and themes [19,20]. First, one team member (AC) coded a subset of responses from both respondent groups, using open coding [21]. Two team members (AC and AF) discussed those codes and developed an initial list of emerging themes to use as a codebook. AC then recoded the initial subset and a new subset using the new codebook. AF then coded 20% of that coding to validate coding consistency and identify potential new themes. Four research team members (AC, AF, ER, PW) met to discuss the draft codebook at this stage. This meeting resulted in a near-final codebook. AC used this codebook to code the complete dataset, and AF reviewed and validated a subset (20%) of the coding to ensure consistency. The coders identified a few new themes when coding the complete dataset and added them to the final codebook until the coders were satisfied that thematic saturation had been reached (they identified no new themes) [23]. The entire dataset was then reviewed to identify any previous instances of these themes. Qualitative analysis software (NVivo Version 12 [22]) was used to assist with coding and analysis. Throughout the analysis process, the team met to discuss the relationship between themes and develop a conceptual framework (Fig. 1). Through this discussion, the team classified themes as relating to (1) perceptions of MRI, (2) discussing MRI, and (3) proposed solutions. Some themes fell into multiple categories. The conceptual model divides these themes into those discussed by parents and medical team members, those discussed by parents only, and those discussed by the medical team only, to highlight commonalities and differences. [19].
Fig. 1.
Conceptual framework.
3. Results
3.1. Participants
3.1.1. Clinicians
Sixteen clinicians completed the case vignettes and the online survey, including six neonatologists, two neonatal nurse practitioners, two fellows in neonatology, four neurologists, and two pediatricians from the Infant Follow-up Clinic. Most (46%) of the respondent clinicians had 10–20 years of experience.
3.1.2. Parents
Twenty-eight parents (or pairs of parents) answered the semi-structured questionnaire focused on the use of brain MRI; 26 answered the survey online, one answered on the paper version, and one answered through in-person interview. Twelve parents belonged to the group with brain injury (six only had one MRI after TH, and six had two MRIs) and thirteen parents belonged to the group without brain injury (13 only had one MRI after TH, and three had two MRIs). The survey was answered by mother only (43%), father only (43%), or both parents (14%). Mean age of their children at survey time was 3 years and 2 months. Highest level of parent education was university (68%), CÉGEP college (24%) and secondary (8%). Most parents (64%) understood what was explained to them and most (80%) found that the doctor used words easy to understand. When asked if the prognosis received during the NICU stay corresponded to how their child is doing today, 56% of parents answered that the description was somewhat accurate, but 32% that the description was not accurate and 12% that the description was wrong.
3.2. How do different respondents understand brain MRI results?
3.2.1. Clinicians
When asked which elements they used to discuss prognosis with parents of neonates with HIE treated with TH, clinicians mentioned that they rely on the clinical exam of the neonate (93%), the brain MRI report (93%), the results of the other ancillary tests (93%), the review of the MRI images (80%), the pediatric neurologist's opinion (73%), previous experience (67%), previous training (67%), and literature review (40%).
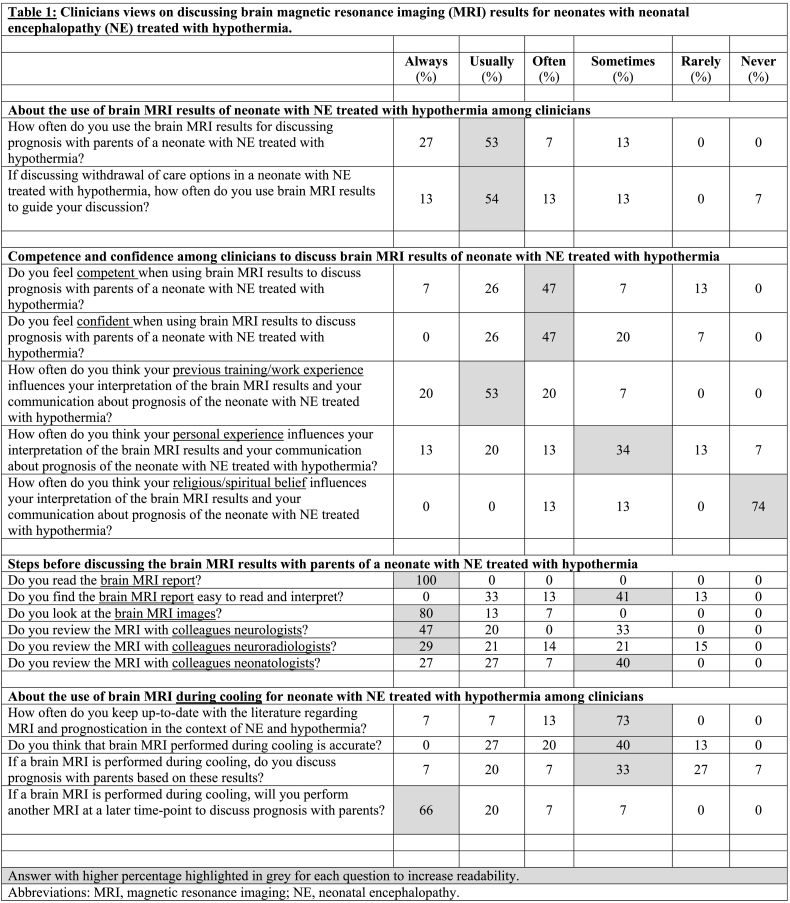
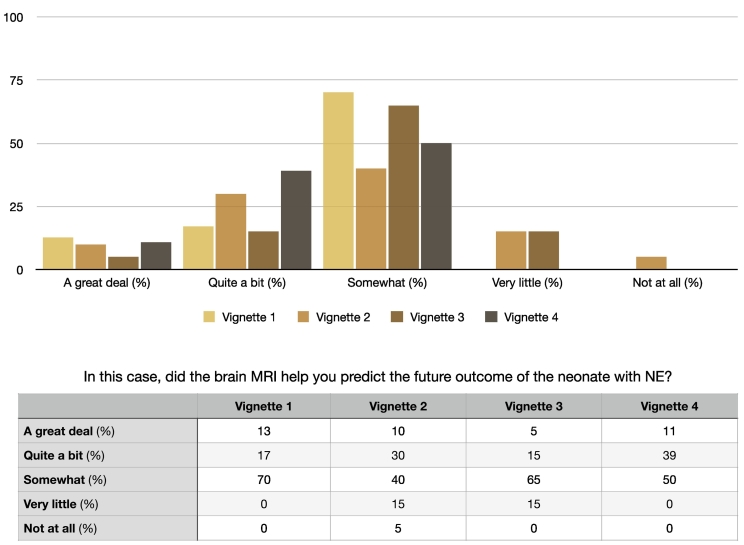
Brain MRI results were thus most often “usually” (53%) used in the prognostication discussion (Table 1), but were most often only “somewhat” helpful in that discussion as highlighted in the answers to the vignettes (Fig. 2). Most clinicians (73%) highlighted that they could only “sometimes” remain up to date with the current literature about prognostication in the context of HIE and TH (Table 1). When dealing with day-2 brain MRIs performed during TH, most clinicians (40%) assumed that the results of these early MRIs were only “sometimes” accurate and most of them (33%) only used “sometimes” these results to discuss prognosis (Table 1). A majority of them (66%) would “always” repeat imaging at a later time-point to discuss prognosis (Table 1).
Table 1.
Clinicians views on discussing brain magnetic resonance imaging (MRI) results for neonates with neonatal encephalopathy (NE) treated with hypothermia.
Fig. 2.
Usefulness of brain MRI results for clinicians to predict future outcome of the neonates with NE treated with TH described in the different vignettes.
The most common comments from the clinicians stressed the view that MRI was confirmatory, e.g., “re inforces [sic] what we know from the clinical examination and evolution to date.” Clinicians also commonly described uncertainty when discussing brain MRI results, noting that it is often difficult or impossible to predict or prognosticate what the future exactly entails: e.g., “the full range of possibilities is still possible.” When faced with results of day-2 MRIs, several clinicians expressed that it was “too early” or that they needed “more time” to develop a prognosis. However, a few clinicians did assert that the day-2 MRI may help mitigate uncertainty in some cases: e.g., “In case of considering early withdrawal of care and there [is] some uncertainty, MRI earlier on might be helpful – if catastrophic, [it] might help family to make decisions.” Clinicians acknowledged the co-existence of certainty and uncertainty: e.g., “Even though we can be fairly certain that the infant will have sequelae, there remains uncertainty about the severity of these sequelae.” They also stressed the importance of long-term follow up to “see the impact that this injury will have” and “to specify the outcome between mild and severe disability.”
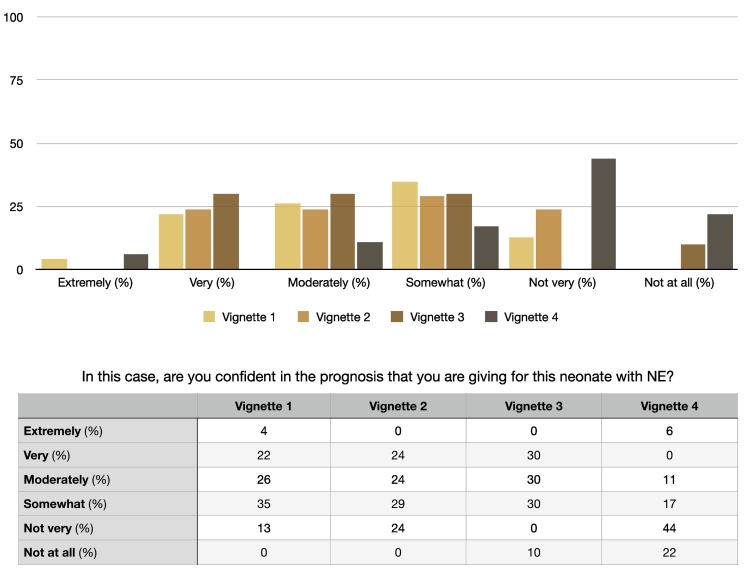
Limited confidence among clinicians was highlighted in the answers to the vignettes (Fig. 3), in the closed questions (Table 1) and in many comments. Many described a lack of confidence in their discussion of the brain MRI results and formulation of prognosis, e.g., “I am never confident with predicting outcome completely unless the baby presents extreme and MRI is clearly catastrophic.” Clinicians also highlighted limitations of MRI in prognostication: e.g., “an image that [,] unless it is completely abnormal [,] can only give you a suggestion – infants have a certain plasticity to their brain that can help/not help in their recovery. [A] return to normal exam or mild at the time of discharge is much more encouraging than a picture.”
Fig. 3.
Level of confidence among clinicians to predict future outcome of the neonates with NE treated with TH described in the different vignettes.
Clinicians also explained what helped alleviate the challenges of MRI discussion. In both closed questions (Table 1) and comments, most clinicians focused on the role of a interdisciplinary approach, i.e., consulting or working together with other clinicians, including neurologists, neuroradiologists and other neonatologists. As one respondent explained: “I do not personally know the exact significance of the above MRI findings, and therefore I would feel much more comfortable consulting one or more of the following: another neonatologist, radiologist, neurologist, neonatal follow-up [clinicians,] prior to counseling the family. This allows for a better understanding of the FULL picture and obtain [a] consensus.”
3.2.2. Parents
When asked to select reasons why a brain MRI was performed for their neonate (Table 2), parents chose the following options: to evaluate brain damage (88%), to predict the future development of the infant (46%), to predict the future complications and the possible recovery (42%), to establish a diagnosis (38%), to predict the quality of life of the infant (31%) and to understand the cause of the brain damage (12%). In contrast to clinicians, parents never described the MRI as confirmatory. They did describe that the MRI would show not only the damage to the brain from birth, but also the effect of the TH treatment: e.g., “to check the brain after treatment”. Some parents mentioned that the imaging was part of the clinical protocol: e.g., “Someone told me that MRI was part of a protocol of tests to be done after the cooling.” A few parents mentioned that the MRI of their child was done for research: e.g., “My baby was part of a study group and they wanted to see the behavior of the damage to the brain.”
Table 2.
Summary of parent comments.
| Theme | Example of comments |
|---|---|
| Understanding brain MRI results | |
| MRI looks for or shows something | “To see if there was brain damage.” “If there are black or dark shadows, this implies that this part of the brain is dead. We do not want to see dark zones on the brain.” |
| Causes of damage | “To verify the after effects of hypoxia to the brain following delivery” “It was to verify that he did not have any necrosis following a possible lack of oxygen” |
| Limitations of MRI | “One was done after he was born and another one needed to be done after 10 days to get more [clear] image” |
| Protocol | “Someone told me that MRI was part of a protocol of tests to be done after the cooling.” |
| MRI for research | “My baby was part of a study group and they wanted to see the behavior of the damage to the brain.” |
| Communicating brain MRI results | |
| Communication skills | “Again, eliminate all possible delays and inform the parents as quickly as possible.” “To have access to the images (MRI)” “I believe that it is very important to not go too far, only that which is certain must be discussed.” “To offer parents to be accompanied during the discussion because of the emotional implications.” “Maybe discussing it in a place other than the critical care unit would be good. With all the noise from the incubators and machines in the room, it was not so easy.” “Be sure to have empathy and that the parent is capable, emotionally and physically, of understanding what you are explaining to them.” |
| MRI reassuring | “Reassuring” “It said that it was very positive, so we could be optimistic.” |
| Uncertainty | “There was no damage, therefore it was reassuring, but I was told that nothing could be predicted in advance for sure. There was too much uncertainty.” |
| Multidisciplinary | “A meeting with the two parents, the doctor and the neurologist, with concrete explanations and the supporting images” |
| Privacy | “We were the two parents and it was our moment. This did not concern anyone, but us.” |
| Support | “Have face-to-face meeting with the MRI images and a social worker or someone else to support us.” “Always meet face-to-face with the family, do not underestimate the impact that these results have on parents, offer psychological support.” |
| Follow-up | “The pediatrician who did my baby's follow-up responded to many of my questions that remained unanswered following my baby's hospitalization.” |
| Hope | “Do not make too grave a diagnosis too quickly. Put a little more stress on what we can do to help our baby progress.” |
| Comfort | “The pediatrician's call brought us a little relief and decreased the stress we endured all across the hospitalization.” |
| End-of-life decision-making | “As [NAME] was likely not to breathe or eat on his own, we had to decide what we would do in the following days. We experienced immense anger, sadness, and incomprehension about the precarious situation that he was in.” “We started to talk about funerals and getting him baptized in the event that he dies.” |
| Good parents | “I remember that they told us that she could have a developmental delay. It tore me apart, and we worked with the little one to provide the most encouragements and provide her with every possible chance. It went super well and she is very intelligent.” |
| Solutions | |
| Communication skills | “Teach bedside manner. The doctor was extremely rude. The doctor with her looked annoyed that I was here and asked who I was and what I was doing there. Needless to say, I was in tears.” “A better attitude in the face of the potential barriers that await us.” |
| Hope | “After the first MRI, we had a big hope that the baby will be fine and will grow up normally. [It was still a] stress but comforting to know what to expect.” |
| Address stress | “It was an unbelievable stress for about two months. My son was in critical care for 30 days. I lost my beard hair, my convictions and my illusions” |
| Address forgetting or not remembering | “I am personally questioning my own memory. I remember that they talked to me, but I do not remember who, when, or where, I am sorry. I think that my husband might have been there, still not sure [….] it is definitely necessary to be accompanied by someone such as a partner and to repeat, because I asked my husband and it is unclear to him too. Maybe because the results were neither negative nor positive.” |
3.3. How do different respondents communicate brain MRI results?
3.3.1. Clinicians
Clinicians discussed specific items that they would communicate to parents about brain MRI results. Some clinicians focused on communicating what clinical cause could explain the brain damage seen on MRI, e.g., “their child's brain sustained injury from lack of oxygen.” Others mentioned more clearly the visual components and specified that they would show the MRI images to parents. Several clinicians explained how they would describe the MRI as reassuring: e.g., “Considering [his] traumatic birth history and turbulent neonatal course, the MRI is somewhat reassuring. However, [he] remains at risk for neurodevelopmental sequelae and will require close follow-up to monitor his progress.” Indeed, when they found the MRI reassuring or not, many clinicians also highlighted that they would communicate the need for future follow-up: e.g., “mention that MRI does show some areas of “scar[r]ing“ that is consistent with the story and that this does increase the possibility of long term development challenges that will be followed by development specialists.”
Clinicians also mentioned that they needed to communicate the risk, uncertainty, and limitations of the brain MRI. As one clinician explained, “I am always careful about giving a very ‘black [or] white’ prognosis. I tend to discuss in terms of ‘risks.’” Another noted “that there remains (and will remain for several months) some uncertainty with respect to his development.” When dealing with day-2 brain MRIs performed during TH, some clinicians reiterated that they would mention to parents the limitations of these early brain MRIs: e.g., “I would also mention that, at this stage, we may not see all the damages”.
Clinicians discussed how they would communicate with parents. Many clinicians stressed the importance of answering parents' questions and needs. They talked about the importance of when and where these conversations with parents should take place, mentioning that: “We should not discuss everything at the meeting where we explain the MRI results. This type of situation requires more meetings over several days”. Some clinicians stressed joint decision-making, even going so far as noting that the vignettes “don't indicate the views of the parents. So I find these cases very hypothetical as the recommendation is based on a two-way street [of] understanding and communication.” Clinicians noted the importance of communicating hope, stressing that “it is important to encourage and give hope to parents” and that they “would be optimistic with parents.” Others highlighted being consistent and non-judgmental: e.g., “In order to give a consistent response, I would meet the family with neurology [….] I would not put judgment on mild or moderate disability as mild disability can be devastating for some parents.” Again, clinicians stressed a interdisciplinary approach in these communications: e.g., “Preferably I would ask the consultants to accompany me to discuss with parents.”
3.3.2. Parents
Parents' responses provided insight into parents' communication preferences (Table 2). Seventy percent of parents would have liked the MRI earlier if it was possible. Of the parents of neonates with HIE who participated in the research study with day-2 MRIs during TH, 87% mentioned that knowing earlier was useful. Comments from parents urged to “eliminate all possible delays and inform the parents as quickly as possible.” Only 24% of parents reported that the doctors showed them the actual imaging; 80% of them found that very useful. Among parents who did not see the actual imaging, 76% thought that it could have been useful. In comments, parents did express interest in seeing the imaging and mentioned that “access to the images” helped them better understand.
Some parents described the MRI as reassuring, though much less often than the medical team; parents typically used this specific word when their neonates did not display brain injury on MRI. However, other parents, especially but not only parents of neonates with brain injury, reported the uncertainty and the limitations in prognostication transmitted by the clinicians: e.g., “There was no damage, therefore it was reassuring, but I was told that nothing could be predicted in advance for sure. There was too much uncertainty.” Several parents would have liked to know more information, and especially more concrete information. However, at least one parent was willing to trade off the amount of given information for the certainty of information: “I believe that it is very important to not go too far, only that which is certain must be discussed.”
Parent described waiting for the meeting with the doctors with “concrete” explanations. They identified that the neonatologist and the pediatric neurologist of their baby were the persons most often giving these results. Parents had varying opinions on who should be present for the conversation. A majority (64%) reported not being able to choose who was present with them during the discussion. Comments revealed a range of specific preferences, from statements such as “We were the two parents and it was our moment. This did not concern anyone, but us” to requests “to offer parents to be accompanied during the discussion because of the emotional implications.” Others specifically requested a social worker or chaplain be present.
Parents most often reported conversations taking place at the bedside (32%), during a formal meeting in a conference room (20%), or through a phone call (20%). In comments, they raised the importance of privacy and other concerns about the setting, such as noise, suggesting “Maybe discussing it in a place other than the critical care unit would be good. With all the noise from the incubators and machines in the room, it was not so easy.” Parents also commented about how they wanted to receive news from the clinicians. Like the clinicians, they highlighted the importance of answering questions: e.g., praising a pediatrician who “responded to many of my questions that remained unanswered following my baby's hospitalization.” Parents requested that the news be delivered with care and empathy: e.g., “Be sure to have empathy and that the parent is capable, emotionally and physically, of understanding what you are explaining to them.” They stressed the importance of hope in communication: e.g., “Do not make too grave a diagnosis too quickly. Put a little more stress on what we can do to help our baby progress.”
3.4. What are the solutions to improve discussion of MRI results?
3.4.1. Clinicians
Clinicians formulated the following potential solutions to the challenges of discussing brain MRI results. Clinicians suggested enhancing the interdisciplinary approach through “more regular and formal interaction with consultants and experts,” and “the inclusion of colleagues during the communication of results, i.e., neurologist, neonatologist, neonatal follow-up pediatrician, social worker, and bedside nurse.”
Some clinicians highlighted their lack of formal training in discussing brain MRI data: 73% reported not to have received formal training for understanding reports and images of brain MRI, and 93% reported not to have received formal training for communicating brain MRI results. All clinicians answered that they could improve their skills in discussing brain MRI results (20% a great deal, 40% quite a bit, and 40% somewhat). Comments also expressed interest in further training, suggesting possibilities like “courses on how to understand the reports and the images and how to look at them”, “conferences on the subject,” and “lectures on prognostication by interdisciplinary team (neonatology, neurology, neuroradiology, EEG/evoked response).” In addition, a few clinicians proposed that getting more information about the follow-up of these neonates would help: e.g., “Receiving regular feedback from the follow-up team reporting patient outcomes in comparison to their neonatal history and brain MRI results.” Some clinicians highlighted the potential usefulness of additional research (“larger and more extensive outcome studies”) and experience (“experience in neonatal follow-up.”)
Many clinicians noted that better internal information-sharing systems would help them in discussing brain MRI results. Proposed solutions included “Having written documentation that reports what type of lesion (location, severity) […]. Having reports that are easier to read and interpret.”
Clinicians discussed specific skills that would help when communicating with parents of neonates with HIE, such as using laymen's terms, having “clarity, compassion, accepting and communicating uncertainty” and using “more precise words, more similar to those of my colleagues, to avoid confusing parents.” Some clinicians highlighted how families can be an important source of improving clinician's communication skills, by expressing “their input on what is significant and meaningful information for them.” Some clinicians proposed that specific protocols and guidelines be developed to enhance communication skills in cases of neonatal brain injury: e.g., “Standardized institutional guidelines [would] improve homogeneity of the perception between colleagues and of information given to the families.”
3.4.2. Parents
Parents emphasized several themes around communication (Table 2). They identified poor communication skills. One respondent stressed: “Teach bedside manner. The doctor was extremely rude. The doctor with her looked annoyed that I was here and asked who I was and what I was doing there. Needless to say, I was in tears” and another requested “a better attitude in the face of the potential barriers that await us.” They often mentioned the stress surrounding their situation: e.g., “It was an unbelievable stress for about two months. My son was in critical care for 30 days. I lost my beard hair, my convictions and my illusions”. Stress interacted with hope, e.g., “After the first MRI, we had a big hope that the baby will be fine and will grow up normally. [It was still a] stress but comforting to know what to expect.” They also highlighted the issue of forgetting or not remembering: e.g., “I am personally questioning my own memory. I remember that they talked to me, but I do not remember who, when, or where, I am sorry. I think that my husband might have been there, still not sure [….] it is definitely necessary to be accompanied by someone such as a partner and to repeat, because I asked my husband and it is unclear to him too. Maybe because the results were neither negative nor positive.”
4. Discussion
Prognosis has been part of medicine ever since its inception, with patients and parents often coming to clinicians looking for decisive answers. Advanced technologies such as MRI would seem to help establishing clear prognoses, but they do not eliminate uncertainty for several reasons. First, prognosis is seldom taught and is researched to a lesser degree compared to diagnoses or treatments [24,25]. This was also reflected in the answers given by our participants. Second, the future is inherently unpredictable and therefore at odds with the more ascertained ability to talk about past and current medical events [26,27]. Third, these issues are exacerbated in neonates with HIE treated with TH. Prognosis in these neonates is extremely unpredictable as many factors such as the plasticity of the brain in development and the impact of the environment modulate the long-term outcomes and their impact on quality of life [28,29]. The care of neonates with HIE has drastically changed over the last few years, with the advent of TH [[28], [29], [30]], and there are limited long-term outcome data for neonates treated with TH. Fourth, MRI is no panacea: despite its alleged abilities, it remains a tool in process of being refined, especially in terms of its ability to inform prognostication [31,32]. Fifth, prognosis was historically avoided in order to shield patients and parents from the distress of bad news [33] and it continues to be an uneasy and uncomfortable aspect of medical practice as reported in our study and others [9,[34], [35], [36]]. It is therefore unsurprising that clinicians in this study often struggle with uncertainty and reported a lack of confidence in discussing MRI findings, consistent with some emerging literature [9,34,35].
Parents also struggled with uncertainty related to the brain MRI results, but did not discuss the limitations of brain MRI as much as clinicians. They mentioned that the outcome of their child did not always correspond to what was discussed in the postnatal period. They expressed an expectation of “concrete” knowledge, but also highlighted their needs for time to emotionally process the information received, for their questions to be addressed (even if there is not always an answer), and for empowerment to take care of their infant with brain injury.
Parents unanimously requested to receive information more quickly in the context of HIE and TH. However, several clinicians mentioned that they would not feel comfortable using the MRIs during TH for prognostic purposes, because they felt it was too early. Several studies have now shown that MRIs during TH show the same injuries as later MRIs for neonates with HIE treated with TH [[10], [11], [12], [13], [14], [15]]. This example illustrates how it is challenging for clinicians to remain attuned to emerging research literature and to apply these new research findings.
Discussing brain MRI results and potential for disability requires that a lot of information is conveyed at one time to parents, who may already feel stressed and overwhelmed by the situation. Several models support a clinically meaningful and ethical practice of prognostication [[37], [38], [39]]. Common features of proposed approaches were described as ouR-HOPE approach (Reflection – Humility – Open-mindedness – Partnership – Engagement) [36] and included: (1) transparency in what is known and not known [40]; (2) recognizing and communicating the limits of medicine; (3) maintaining a stance of humility toward parents; (4) being open to reevaluation of current knowledge and to learning through challenging and unexpected cases; (5) supporting parents who need to make decisions upon uncertain medical information. Clinicians and parents also proposed several actionable solutions to improve the discussion of brain MRI findings. Some studies have demonstrated that the real outcome of neonates is often less somber than what healthcare professionals depicted in the postnatal period [[41], [42], [43]] and that this issue has also been raised to in the context of HIE and TH [44]. As suggested by the clinicians in this study, an interdisciplinary and integrative approach, where MRI is only one of the elements used for prognosis, and an increased knowledge in follow-up could help mitigate the uncertainty and the lack of confidence of the clinicians, address the needs of the parents and foster their engagement in long-term follow up care [36].
Many clinicians highlighted that they were missing formal training in discussing brain MRI results for neonates with HIE and more generally for neonates with brain injury. To palliate to the difficulty of training all clinicians to these tasks, some centers have developed an expertise in neonatal neurology (neuro-NICU) [45], with a small group of clinicians trained in neonatal neurology. Alternatively, if feasible, a more inclusive approach would be to train all clinicians taking care of these neonates and discussing with parents. Organizing regular interdisciplinary teaching rounds where cases and their follow-up can be reviewed would expose all clinicians to the range of possible outcomes and refine their prognostication skills. In addition, communication guidelines for breaking bad news are widely described in adult medicine [46,47], as well as in pediatrics [48]. They are still emerging in neonatology [49,50], even though the NICU can be an emotional environment where difficult decisions often need to be made. Similar guidelines and trainings are urgently needed in this particular setting. Participation of families of neonates with HIE treated with TH in the development of these training are of utmost importance to ensure that they are meaningful and respond to their expectations and wishes. In our study, parents had actionable insights on what they wanted to know, from whom, where, when, and how during these complex and often difficult discussions. Many parents' suggestions for good communication matched the communication strategies described by clinicians, and can therefore reinforce clinicians' approaches. The importance of showing the pictures or making representative drawing of the injury, but also highlighting the not-injured brain appeared to help parents better understand the medical information and gave them hope.
Finally, standardizing the reporting of brain MRI results are reported and including only relevant information for clinicians seems to be an interesting option to pursue, considering that most clinicians rely only on reports to discuss the MRI results with parents. Making them simpler and to the point by highlighting the location and the extent of the injury, as well as using common terminology would help clinicians, who may have difficulties with the subtleties of radiological language (i.e., the significance of signal changes according to different MRI sequences). A systemic scoring system that has been shown to predict neurodevelopmental outcome may be another solution to improve reporting of the injury extent [2,[49], [50], [51], [52]].
A strength of the study was surveying both those giving prognosis and those receiving prognosis to better understand both points of view and better highlight the variability in such discussions. Among the limitations of the study, our clinicians' samples size was small and did not offer the possibility to stratify and analyze responses based on specialties and levels of training, but reflected the diversity of age and experience of clinicians discussing such results with parents at our institution. Clinicians typically have fear of judgment. Even though it was clear that answers were anonymized, some of the narrative comments evoked this concern. It is common for clinicians to profoundly dislike being placed in a situation where they do not know and to consider uncertainty a taboo topic [53,54]. Another limitation was that our parents' sample size was also small and it was not possible to stratify and analyze responses based on nature/extent of injury. Waiting that their infants reached 3 years of age or beyond to survey parents may also be a limitation and have introduced recall bias, but it would also open this unique perspective to assess what they remembered from these discussions and how it influenced their view of their child. Parents' sample included a similar number of parents of neonates with and without brain injury. In addition, the age range of children with HIE within each group of parents were similar, giving them a homogenous time perspective to reflect on what was said in the NICU and compare with how their child was doing at time of survey. Finally, discussion of results and prognosis may vary by institution, including who discusses these brain MRI results with parents and when they are discussed. Only clinicians and parents from a single center were surveyed in our study, so an additional multi-institutional study with a larger sample size of clinicians and parents is needed to confirm generalizability of our results, to continue to raise awareness for these difficult conversations, and to find constructive solutions for clinicians and parents to these challenges. It may also be interesting to survey parents immediately after the NICU stay and later on, to compare the evolution of their perspectives over time.
5. Conclusion
This study provided the opportunity to highlight that discussing brain MRI results for neonates with HIE are challenging tasks for clinicians and daunting moments for parents. There is an urgent need to develop a systemic and interdisciplinary approach to prognostication, to standardize reporting of brain MRI results and to further train clinicians in their discussion. These solutions may help facilitate difficult decision-making discussions and make them more meaningful for parents. Similar interventions may be applied more generally to other critically ill neonates with brain injury and their parents in order to empower them in the care of their infants.
Credit authors statement
All the authors fulfill the authorship credit requirements. Ariel Cascio and Amaryllis Ferrand were postdoctoral fellows at the time of the study. Cascio coded the transcript, developed the conceptual framework that organizes concepts into clusters, and drafted the first version of the manuscript. Amaryllis Ferrand reviewed and validates a subset of coding, participated to the development of the conceptual framework that organizes concepts into clusters, read, added suggestions and approved the manuscript. Eric Racine supervised Ariel Cascio and Amaryllis Ferrand, participated to the design of the study and the development of the conceptual framework that organizes concepts into clusters, read, added suggestions and approved the manuscript. Marie St-Hilaire was a fellow in neonatology at the time of the study and participated to the design of the study, helped to prepare the survey and the vignettes collected the data and the transcripts, read and approved the manuscript. Priscille-Nice Sanon collected the data and the transcripts, read, and approved the manuscript. Andreea Gorgos participated to the design of the study, read, added suggestions and approved the manuscript. Pia Wintermark designed the study, prepared the survey and the vignettes, supervised Marie St-Hilaire and Priscille-Nice Sanon for the data collection, participated to the development of the conceptual framework that organizes concepts into clusters, read, added suggestions and finalized the manuscript.
Declaration of Competing Interest
The authors have stated that they had no interests, which might be perceived as posing a conflict or bias. No conflict of interest exists. The authors have no financial relationships relevant to this article to disclose. The study sponsors had no involvement in the study design; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the paper for publication.
Acknowledgments
Pia Wintermark is supported by FRSQ Clinical Research Scholar Career Award Senior and a Canadian Institutes of Health Research (CIHR) Project Grant. Eric Racine is supported by a FRQS Researcher Emeritus Award.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ensci.2022.100424.
Appendix A. Supplementary data
Supplementary material 1
Supplementary material 2
Supplementary material 3
Supplementary material 4
References
- 1.Wilkinson D. MRI and withdrawal of life support from newborn infants with hypoxic-ischemic encephalopathy. Pediatrics. 2010;126(2):e451–e458. doi: 10.1542/peds.2009-3067. [DOI] [PubMed] [Google Scholar]
- 2.Al Amrani F., Marcovitz J., Sanon P.-N., Khairy M., Saint-Martin C., Shevell M., et al. Prediction of outcome in asphyxiated newborns treated with hypothermia: is a MRI scoring system described before the cooling era still useful? Eur. J. Paediatr. Neurol. 2018;22(3):387–395. doi: 10.1016/j.ejpn.2018.01.017. [DOI] [PubMed] [Google Scholar]
- 3.Cheong J.L.Y., Coleman L., Hunt R.W., Lee K.J., Doyle L.W., Inder T.E., et al. Prognostic utility of magnetic resonance imaging in neonatal hypoxic-ischemic encephalopathy: substudy of a randomized trial. Arch. Pediatr. Adolesc. Med. 2012;166(7):634–640. doi: 10.1001/archpediatrics.2012.284. [DOI] [PubMed] [Google Scholar]
- 4.Sanchez Fernandez I., Morales-Quezada J.L., Law S., Kim P. Prognostic value of brain magnetic resonance imaging in neonatal hypoxic-ischemic encephalopathy: a meta-analysis. J. Child Neurol. 2017;32(13):1065–1073. doi: 10.1177/0883073817726681. [DOI] [PubMed] [Google Scholar]
- 5.Saigal S., Tyson J. Measurement of quality of life of survivors of neonatal intensive care: critique and implications. Semin. Perinatol. 2008;32(1):59–66. doi: 10.1053/j.semperi.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 6.Shevell M.I., Majnemer A., Miller S.P. Neonatal neurologic prognostication: the asphyxiated term newborn. Pediatr. Neurol. 1999;21(5):776–784. doi: 10.1016/s0887-8994(99)00102-2. [DOI] [PubMed] [Google Scholar]
- 7.Parker M., Shemie S.D. Pro/con ethics debate: should mechanical ventilation be continued to allow for progression to brain death so that organs can be donated? Crit. Care. 2002;6(5):399–402. doi: 10.1186/cc1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andrews P., Azoulay E., Antonelli M., Brochard L., Brun-Buisson C., Dobb G., et al. Year in review in intensive care medicine, 2004. III. Outcome, ICU organisation, scoring, quality of life, ethics, psychological problems and communication in the ICU, immunity and hemodynamics during sepsis, pediatric and neonatal critical care, experimental studies. Intensive Care Med. 2005;31:356–372. doi: 10.1007/s00134-005-2573-9. [DOI] [PubMed] [Google Scholar]
- 9.Bell E., Rasmussen L.A., Mazer B., Shevell M., Miller S.P., Synnes A., et al. Magnetic resonance imaging (MRI) and prognostication in neonatal hypoxic-ischemic injury: a vignette-based study of Canadian specialty physicians. J. Child Neurol. 2015;30(2):174–181. doi: 10.1177/0883073814531821. [DOI] [PubMed] [Google Scholar]
- 10.Agut T., León M., Rebollo M., Muchart J., Arca G., Garcia-Alix A. Early identification of brain injury in infants with hypoxic ischemic encephalopathy at high risk for severe impairments: accuracy of MRI performed in the first days of life. BMC Pediatr. 2014;14(1):1–7. doi: 10.1186/1471-2431-14-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boudes E., Tan X., Saint-Martin C., Shevell M., Wintermark P. MRI obtained during versus after hypothermia in asphyxiated newborns. Arch Dis Child-Fetal. 2015;100(3):F42–F238. doi: 10.1136/archdischild-2014-306550. [DOI] [PubMed] [Google Scholar]
- 12.Chakkarapani E., Poskitt K.J., Miller S.P., Zwicker J.G., Xu Q., Wong D.S.T., et al. Reliability of early magnetic resonance imaging (MRI) and necessity of repeating MRI in noncooled and cooled infants with neonatal encephalopathy. J. Child Neurol. 2016;31(5):553–559. doi: 10.1177/0883073815600865. [DOI] [PubMed] [Google Scholar]
- 13.Charon V., Proisy M., Ferré J.-C., Bruneau B., Tréguier C., Beuchée A., et al. Comparison of early and late MRI in neonatal hypoxic–ischemic encephalopathy using three assessment methods. Pediatr. Radiol. 2015;45(13):1988–2000. doi: 10.1007/s00247-015-3419-4. [DOI] [PubMed] [Google Scholar]
- 14.O’Kane A., Vezina G., Chang T., Bendush N., Ridore M., Gai J., et al. Early versus late brain magnetic resonance imaging after neonatal hypoxic ischemic encephalopathy treated with therapeutic hypothermia. J. Pediatr. 2021;232:73–79. doi: 10.1016/j.jpeds.2021.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wintermark P., Hansen A., Soul J., Labrecque M., Robertson R.L., Warfield S.K. Early versus late MRI in asphyxiated newborns treated with hypothermia. Arch Dis Child-Fetal. 2011;96(1):F36–F44. doi: 10.1136/adc.2010.184291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wisnowski J.L., Wintermark P., Bonifacio S.L., Smyser C.D., Barkovich A.J., Edwards A.D., de Vries L.S., Inder T.E., Chau V., Newborn Brain Society Guidelines and Publications Committee Neuroimaging in the term newborn with neonatal encephalopathy. Semin. Fetal Neonatal Med. 2021;26(5):101304. doi: 10.1016/j.siny.2021.101304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilkinson D. The window of opportunity for treatment withdrawal. Arch. Pediatr. Adolesc. Med. 2011;165(3):211–215. doi: 10.1001/archpediatrics.2011.4. [DOI] [PubMed] [Google Scholar]
- 18.Momentive Inc . Momentive Inc.; San Mateo, California, USA: 1999-2021. SurveyMonkey.www.momentive.ai [Google Scholar]
- 19.Hsieh H.-F., Shannon S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 20.Creswell J.W. Sage Publications; Thousand Oaks, Calif: 1998. Qualitative Inquiry and Research Design: Choosing among Five Traditions / John W. Creswell. [Google Scholar]
- 21.Nicholls D. Qualitative research: part one–philosophies. Int J Ther Rehab. 2009;16(10):526–533. [Google Scholar]
- 22.QSR Internioantal Pty Ltd NVivo (Version 12) 2018. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- 23.Saunders B., Sim J., Kingstone T., Baker S., Waterfield J., Bartlam B., et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual. Quant. 2018;52(4):1893–1907. doi: 10.1007/s11135-017-0574-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Christakis N.A. The ellipsis of prognosis in modern medical thought. Soc. Sci. Med. 1997;44(3):301–315. doi: 10.1016/s0277-9536(96)00100-1. [DOI] [PubMed] [Google Scholar]
- 25.Sisk B.A., Kang T.I., Mack J.W. Prognostic disclosures over time: parental preferences and physician practices. Cancer. 2017;123(20):4031–4038. doi: 10.1002/cncr.30716. [DOI] [PubMed] [Google Scholar]
- 26.Mack J.W., Joffe S. Communicating about prognosis: ethical responsibilities of pediatricians and parents. Pediatrics. 2014;133(Supplement 1):S24–S30. doi: 10.1542/peds.2013-3608E. [DOI] [PubMed] [Google Scholar]
- 27.Hancock K., Clayton J.M., Parker S.M., Walder S., Butow P.N., Carrick S., et al. Discrepant perceptions about end-of-life communication: a systematic review. J. Pain Symptom Manag. 2007;34(2):190–200. doi: 10.1016/j.jpainsymman.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 28.Voss W., Jungmann T., Wachtendorf M., Neubauer A.P. Long-term cognitive outcomes of extremely low birthweight infants: the influence of the maternal educational background. Acta Paediatr. 2012;101(6):569–573. doi: 10.1111/j.1651-2227.2012.02601.x. [DOI] [PubMed] [Google Scholar]
- 29.Payot A., Barrington K.J. The quality of life of young children and infants with chronic medical problems: review of the literature. Curr Prob Pediatr Ad. 2011;41(4):91–101. doi: 10.1016/j.cppeds.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 30.Jacobs S., Hunt R., Tarnow-Mordi W., Inder T., Davis P. Cooling for newborns with hypoxic ischaemic encephalopathy. Pediatr. Res. 2005;58(2):385. doi: 10.1002/14651858.CD003311.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sorokan S.T., Jefferies A.L., Miller S.P. Imaging the term neonatal brain. Paediatr. Child Health. 2018;23(5):322–328. doi: 10.1093/pch/pxx161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laptook A.R., Shankaran S., Barnes P., Rollins N., Do B.T., Parikh N.A., et al. Limitations of conventional magnetic resonance imaging as a predictor of death or disability following neonatal hypoxic–ischemic encephalopathy in the late hypothermia trial. J. Pediatr. 2021;230:106–111. doi: 10.1016/j.jpeds.2020.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sisk B.A., Bluebond-Langner M., Wiener L., Mack J., Wolfe J. Prognostic disclosures to children: a historical perspective. Pediatrics. 2016;138(3) doi: 10.1542/peds.2016-1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rasmussen L.A., Bell E., Racine E. A qualitative study of physician perspectives on prognostication in neonatal hypoxic ischemic encephalopathy. J. Child Neurol. 2016;31(11):1312–1319. doi: 10.1177/0883073816656400. [DOI] [PubMed] [Google Scholar]
- 35.Rasmussen L.A., Cascio M.A., Ferrand A., Shevell M., Racine E. The complexity of physicians’ understanding and management of prognostic uncertainty in neonatal hypoxic-ischemic encephalopathy. J. Perinatol. 2019;39(2):278–285. doi: 10.1038/s41372-018-0296-3. [DOI] [PubMed] [Google Scholar]
- 36.Racine E., Bell E., Farlow B., Miller S., Payot A., Rasmussen L.A., et al. The ‘ouR-HOPE’approach for ethics and communication about neonatal neurological injury. Dev. Med. Child Neurol. 2017;59(2):125–135. doi: 10.1111/dmcn.13343. [DOI] [PubMed] [Google Scholar]
- 37.Parvez S., Abdel-Kader K., Song M.-K., Unruh M. Conveying uncertainty in prognosis to patients with ESRD. Blood Purif. 2015;39(1–3):58–64. doi: 10.1159/000368954. [DOI] [PubMed] [Google Scholar]
- 38.Janvier A., Barrington K., Farlow B. Communication with parents concerning withholding or withdrawing of life-sustaining interventions in neonatology. Semin. Perinatol. 2014;38(1):38–46. doi: 10.1053/j.semperi.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 39.Haward M.F., Gaucher N., Payot A., Robson K., Janvier A. Personalized decision making: practical recommendations for antenatal counseling for fragile neonates. Clin. Perinatol. 2017;44(2):429–445. doi: 10.1016/j.clp.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 40.Sisk B., Frankel R., Kodish E., Isaacson J.H. The truth about truth-telling in American medicine: a brief history. Perm J. 2016;20(3) doi: 10.7812/TPP/15-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morse S.B., Haywood J.L., Goldenberg R.L., Bronstein J., Nelson K.G., Carlo W.A. Estimation of neonatal outcome and perinatal therapy use. Pediatrics. 2000;105(5):1046–1050. doi: 10.1542/peds.105.5.1046. [DOI] [PubMed] [Google Scholar]
- 42.Haywood J.L., Goldenberg R.L., Bronstein J., Nelson K.G., Carlo W.A. Comparison of perceived and actual rates of survival and freedom from handicap in premature infants. Am. J. Obstet. Gynecol. 1994;171(2):432–439. doi: 10.1016/0002-9378(94)90279-8. [DOI] [PubMed] [Google Scholar]
- 43.Chan K.L., Kean L.H., Marlow N. Staff views on the management of the extremely preterm infant. Eur J Obstet Gyn R B. 2006;128(1–2):142–147. doi: 10.1016/j.ejogrb.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 44.Brecht M., Wilkinson D.J.C. The outcome of treatment limitation discussions in newborns with brain injury. Arch Dis Child-Fetal. 2015;100(2):F60–F155. doi: 10.1136/archdischild-2014-307399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Van Meurs K.P., Yan E.S., Randall K.S., Chock V.Y., Davis A.S., Glennon C.S., et al. Development of a NeuroNICU with a broader focus on all newborns at risk of brain injury: the first 2 years. Am. J. Perinatol. 2018;35(12):1197–1205. doi: 10.1055/s-0038-1646954. [DOI] [PubMed] [Google Scholar]
- 46.Marschollek P., Bąkowska K., Bąkowski W., Marschollek K., Tarkowski R. Oncologists and breaking bad news—from the informed patients’ point of view. The evaluation of the SPIKES protocol implementation. J. Cancer Educ. 2019;34(2):375–380. doi: 10.1007/s13187-017-1315-3. [DOI] [PubMed] [Google Scholar]
- 47.Park I., Gupta A., Mandani K., Haubner L., Peckler B. Breaking bad news education for emergency medicine residents: a novel training module using simulation with the SPIKES protocol. J Emerg Trauma Shock. 2010;3(4):385–388. doi: 10.4103/0974-2700.70760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wolfe A.D., Denniston S.F., Baker J., Catrine K., Hoover-Regan M. Bad news deserves better communication: a customizable curriculum for teaching learners to share life-altering information in pediatrics. MedEdPORTAL. 2016;12:10438. doi: 10.15766/mep_2374-8265.10438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bowen R., Lally K.M., Pingitore F.R., Tucker R., McGowan E.C., Lechner B.E. A simulation based difficult conversations intervention for neonatal intensive care unit nurse practitioners: a randomized controlled trial. PLoS One. 2020;15(3) doi: 10.1371/journal.pone.0229895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fox S., Platt F.W., White M.K., Hulac P. Talking about the unthinkable: perinatal/neonatal communication issues and procedures. Clin. Perinatol. 2005;32(1):157–170. doi: 10.1016/j.clp.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 51.Weeke L.C., Groenendaal F., Mudigonda K., Blennow M., Lequin M.H., Meiners L.C., et al. A novel magnetic resonance imaging score predicts neurodevelopmental outcome after perinatal asphyxia and therapeutic hypothermia. J. Pediatr. 2018;192:33–40. doi: 10.1016/j.jpeds.2017.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shankaran S., McDonald S.A., Laptook A.R., Hintz S.R., Barnes P.D., Das A., et al. Neonatal magnetic resonance imaging pattern of brain injury as a biomarker of childhood outcomes following a trial of hypothermia for neonatal hypoxic-ischemic encephalopathy. J. Pediatr. 2015;167(5):987–993. doi: 10.1016/j.jpeds.2015.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kahlke R.M., McConnell M.M., Wisener K.M., Eva K.W. The disconnect between knowing and doing in health professions education and practice. Adv. Health Sci. Educ. 2020;25(1):227–240. doi: 10.1007/s10459-019-09886-5. [DOI] [PubMed] [Google Scholar]
- 54.Knopes J. When physicians don’t know. Perspect. Biol. Med. 2020;63(3):444–457. doi: 10.1353/pbm.2020.0032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1
Supplementary material 2
Supplementary material 3
Supplementary material 4