Abstract
An anatomical understanding of median nerve variation is essential for successful decompression of carpal tunnel syndrome (CTS). Although iatrogenic injury of the thenar branch after carpal tunnel release (CTR) has not been reported in many cases, it can cause serious damage to the patient. In case of rapidly progressing thenar atrophy after CTS surgery, thenar branch of median nerve injury should be suspected. Nerve conduction examination and ultrasound before surgery can be a useful tool for diagnosis.
Keywords: Thenar atrophy, Carpal tunnel release, Median nerve
Introduction
Carpal tunnel syndrome (CTS) is the most common peripheral nerve entrapment syndrome worldwide [1]. When CTS symptoms and signs persist or worsen without relief with a conservative treatment, carpal tunnel release (CTR) is considered a standard surgical treatment [1]. However, an anatomical understanding of median nerve variation is essential for successful decompression. Although iatrogenic injury of the thenar branch after CTR has not been reported in many since its first report in 1985, it can cause serious damage to the patient [2], [3]. We report a case of severed recurrent thenar branch of the median nerve discovered through nerve conduction examination in a patient with suspected thenar branch damage after CTR surgery. It was properly treated through reoperation.
Case presentation
A 50-year-old female patient visited our outpatient department (OPD) due to severe pain in the wrist. The patient had a history of pain with numeral rating scale (NRS) of 3 points and constant aching in the wrist two years ago. She visited an orthopedic surgeon at another hospital where she was diagnosed with CTS. She underwent CTR in October 2019. However, her numbness and pain continued even after the CTR. Mild CTS remained on neurological examination. At the hospital where the first operation was performed, 9 months after the first operation, the second CTR was performed in July 2021. Nevertheless, the patient's pain worsened and a thenar atrophy, which was not present before the second operation, progressed rapidly. She was admitted to our outpatient department (OPD).
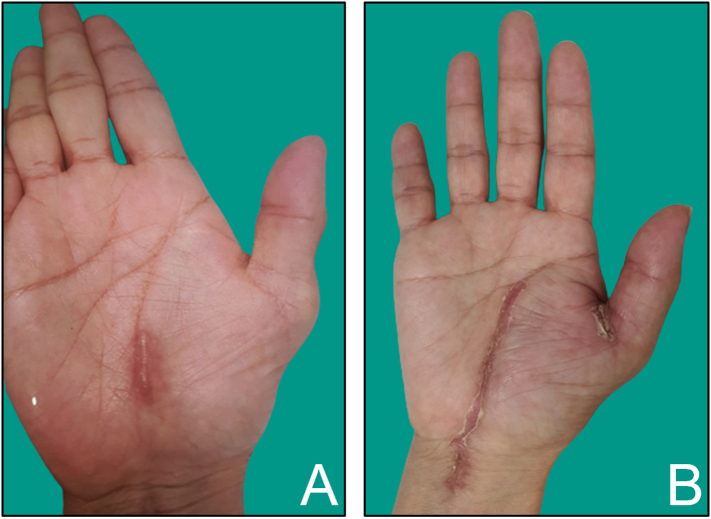
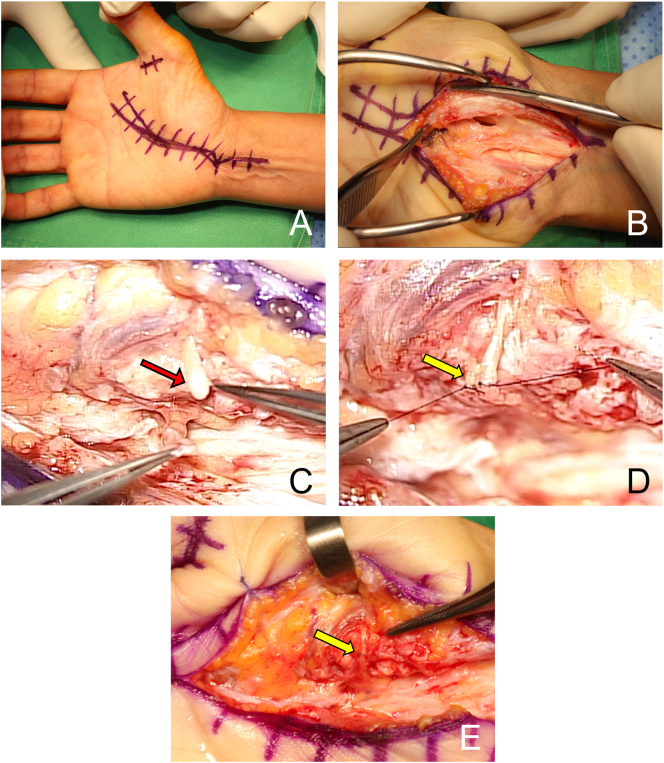
When visiting our OPD, the patient complained of pain and discomfort to the extent that she could not sleep due to numbness in her hands at night (night cry). Physical examination confirmed 1-4th finger tingling sensation and severe thenar atrophy. In ultrasound examination, no specific features were observed except for a mild trigger finger and a slight compressed contour of median nerve at the hamate hook level. However, the patient complained of rapidly progressing thenar atrophy and severe pain even though the neurological examination and ultrasound did not show severe abnormalities (Fig. 1A). Therefore, the author suspected thenar branch injury induced after the 2nd CTR based on neurological symptoms well matched with thenar dermatome and abductor pollicis brevis (APB) atrophy, thumb ablation, and opponens weakness. Findings suggestive of injury to the right thenar branch of median nerve were also confirmed on nerve conduction test and electromyography. Therefore, recurrent motor branch of median nerve rupture and trigger finger (right thumb) were diagnosed. A1 pulley release and classic CTR with nerve repair were performed on October 20, 2021. In the operation field, the thenar branch of the median nerve was severed. Wallerian degeneration was observed on a cut surface of a nerve (Fig. 2). The other nerve ending was found by partial incision of the thenar muscle. The degenerated nerve was resected and nerve repair with tension free was performed under a microscope (Fig. 2). The patient was discharged on the 5th day after surgery without complications. In OPD follow-up at 3 months after the surgery, the patient recovered except for a slight numbness of the tip of the thumb. The thenar atrophy also showed a gradual recovery (Fig. 1B).
Fig. 1.
A: preoperative photograph of right hand. A thick scar on previous operation site and thenar atrophy were found. B: Postoperative 3-month photograph of the right hand. Thenar atrophy was restored partially.
Fig. 2.
A: Extensive classical incision line including previous operation scar was marked. B: Dissection to find cutting nerve ending. C: The severed thenar branch of the median nerve with Wallerian degeneration (red arrow) was found after extensive dissection (transligamentous type). D and E: End-to-end nerve repair of the thenar branch (yellow arrow) was done under microscope. F: A photograph just after the surgery.
Discussion
Anatomical variations in pathways of the median nerve and the thenar motor branch (TMB) in the carpal tunnel are very common. An understanding of such variations is essential for safe incision during a carpal tunnel release surgery [4].
Poisel has distinguished TMB paths into three types: extraligamentous (type I), subligamentous (type II), and transligamentous (type III) [5]. Lanz has further expanded Poisel's classification system to describe four groups of TMB variants: group 1, change of single TMB course according to Poisel; group 2, accessory branch of the median nerve in distal carpal tunnel; group 3, high division of the median nerve associated with the presence of persistent median artery; and group 4, accessory branches of the median nerve proximal to the carpal tunnel [6]. The Lanz classification system has been used in most studies. The prevalence of Lanz group variation has been reported variously depending on the study. According to a meta-analysis study by Henry et al., pooled prevalence rates of extraligamentous, subligamentous, and transligamentous courses were 75.2 %, 13.5 %, and 11.3 %, respectively. Prevalence rates of Lanz groups 2, 3, and 4 have been reported to be 4.6 %, 2.6 %, and 2.3 %, respectively [4]. When adding to a hypertrophic thenar musculature superficial to, or interposed within, the TCL, this variant of TMB is at a particularly high risk of damage during a CTR procedure [7].
Although TMB injury during a CTR surgery can cause serious damage to a patient, few cases have been reported. Lilly et al. first reported severance of the thenar branch of the median nerve as a complication of CTR [2]. They observed loss of thenar motor function in two patients who came to the hospital after surgery for CTS, and confirmed denervation of their thenar muscles. After the first operation, the severed motor branch was identified, isolated, and repaired at 5 months and 14 months, respectively. The thenar function was eventually restored in both patients. In the case reported by Lee et al. in 2019, direct nerve repair of severance of the thenar branch accompanied by transligamentous variation of recurrent motor branch was performed at 138 days after open CTR, and the nerve function almost returned two years later [3]. During the first operation, they performed additional dissection of loose connective tissue around the median nerve for more decompression effect of the median nerve after TCL release during the surgical procedure. In the process, a mixer forcep for blunt dissection and a Metzenbaum scissor for sharp dissection were used. They assumed that the thenar branch was probably cut in the sharp dissector. Therefore, they recommended the use of a blunt incision if possible with variation of the thenar branch in mind for patients needing additional incision. Similar to the two reported cases, it took about five months for the patient in this case to elapse from the first operation to the re-operation. Although it took some time, satisfactory function recovery was possible.
Recent CTR tends to minimize incision [8]. Although these surgical techniques have advantages such as smaller scars and shortening of recovery time, successful surgery depend on careful technique with attention to important anatomical details so that damage to the palmar cutaneous nerve and the recurrent motor branch could be avoid [8]. It has been reported that the most commonly encountered variation during routine mini-open or endoscopic CTR is the transligamentous branch [9]. Henry BM et al. have recommended an ulnar side approach to CRL to prevent iatrogenic damage to the median nerve and its branches [4]. In the present case, it was thought that the problem occurred because variation of the recurrent branch of the patient could not be confirmed through a minimal incision for mini-open during the first operation. Therefore, surgeons performing CTR with mini-open should be aware of this and always be careful when performing layer by layer dissection to avoid iatrogenic damage to the TMB.
Thenar atrophy appears in advanced CTS. It is characterized by a gradual onset. The initial symptom of CTS is numbness of the hand from the thumb to the ring finger. As the condition progresses, atrophy of the thenar muscle occurs [1]. The use of preoperative ultrasound can help identify patients who are more likely to have TMB variation [4], [7]. However, in this patient, the thenar atrophy progressed rapidly and the patient complained of severe pain although physical examination and ultrasonography did not show severe symptoms. In the present case, the nerve conduction study (NCS) contributed to the patient's diagnosis. In the NCS additionally performed in this hospital, Rt. thenar branch of median nerve injury was suspected. Neurological symptoms, APB atrophy, trigger thumb, and opponens weakness showed were well matched with thenar branch injury induced after 2nd CTR OP. Although NCS is considered the golden standard of CTS diagnosis for evaluating sensory conduction velocity and distal motor latency, correlations between these variables and symptoms remain unclear [10]. Nevertheless, as in the present case, NCS can be a useful diagnostic tool of potentially great value not only for selecting patients for a specific treatment, but also for objective evaluation of treatment efficacy in CTS [10].
Conclusion
In case of rapidly progressing thenar atrophy after CTS surgery, thenar branch of median nerve injury should be suspected. Nerve conduction examination and ultrasound before surgery can be a useful tool for diagnosis.
Funding statement
Not applicable.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Declaration of competing interest
The authors declare no competing interests.
Acknowledgments
The authors thank D. S. Kim for his valuable advice on this clinical case.
References
- 1.Padua L., Coraci D., Erra C., et al. Carpal tunnel syndrome: clinical features, diagnosis and management. Lancet Neurol. 2016;15:1273–1284. doi: 10.1016/S1474-4422(16)30231-9. [DOI] [PubMed] [Google Scholar]
- 2.Lilly C.J., Magnell T.D. Severance of the thenar branch of the median nerve as a complication of carpal tunnel release. J. Hand Surg. Am. 1985;10:399–402. doi: 10.1016/s0363-5023(85)80043-5. [DOI] [PubMed] [Google Scholar]
- 3.Lee C.H., Kim C.U. Delayed repair of severed thenar branch with transligamentous variation after open carpal tunnel release. J. Hand Surg. Asian Pac. 2019;24:494–497. doi: 10.1142/S2424835519720214. [DOI] [PubMed] [Google Scholar]
- 4.Henry B.M., Zwinczewska H., Roy J., et al. The prevalence of anatomical variations of the median nerve in the carpal tunnel: a systematic review and meta-analysis. PLoS One. 2015;10 doi: 10.1371/journal.pone.0136477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poisel S. Ursprung und verlauf des ramus muscularis des nervus digitalis palmaris communis I (N. medianus) Chir. Praxis. 1974;18:471–474. [Google Scholar]
- 6.Lanz U. Anatomical variations of the median nerve in the carpal tunnel. J. Hand Surg. Am. 1977;2:44–53. doi: 10.1016/s0363-5023(77)80009-9. [DOI] [PubMed] [Google Scholar]
- 7.Mullin E.P., 3rd, Deal J.B., Jr., Krul K.P. preligamentous variant of the thenar motor branch of the median nerve. J. Am. Acad. Orthop. Surg. Glob Res. Rev. 2020;4 doi: 10.5435/JAAOSGlobal-D-20-00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang J.H., Zager E.L. Mini-open carpal tunnel decompression. Neurosurgery. 2004;54:397–400. doi: 10.1227/01.neu.0000103669.45726.51. [DOI] [PubMed] [Google Scholar]
- 9.Lutsky K.F., Jones C.M., Kim N., Medina J., Matzon J.L., Beredjiklian P.K. Frequency of incidental median thenar motor nerve branch visualization during mini-open and endoscopic carpal tunnel release. Hand (N Y) 2017;12:60–63. doi: 10.1177/1558944716643095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sonoo M., Menkes D.L., Bland J.D.P., Burke D. Nerve conduction studies and EMG in carpal tunnel syndrome: do they add value? Clin. Neurophysiol. Pract. 2018;3:78–88. doi: 10.1016/j.cnp.2018.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]