Abstract
Background
Isolated antero-medial osteoarthritis (AMOA) of the knee is a distinct pattern of arthritis. Medial arthritis of the knee in select patients can be managed with uni-compartmental arthroplasty (UKA), with studies showing shorter hospital stay, faster rehabilitation and reduced medical complications in the post-operative period compared to TKA. However, the prevalence of AMOA in Indian patients with osteoarthritis of the knee is unknown. The aim of this study was to evaluate the prevalence of AMOA in patients undergoing primary TKA for OA.
Methods
This was a prospective evaluation of 2518 knees in 1936 patients who were selected for primary TKA. Pre-operative radiographs were screened based on the Oxford UKA Radiological decision aid and diagnosis of AMOA was established. All 2518 knees underwent primary total knee arthroplasty and cases of AMOA were confirmed intra-operatively based on ACL integrity, lateral compartment wear and medial compartment wear pattern. Cases with AMOA arthritic wear pattern were considered amenable for UKA if radiographs showed intact lateral joint space, intra-operatively those with intact and functional ACL, acceptable patellofemoral wear (Outerbridge I–II).
Results
We report a prevalence of 46.94% of AMOA, who were amenable for UKA. Obese patients were more likely to have a damaged or non-functional ACL and more likely to have a high degree of wear, not amenable for UKA (p < 0.05). Non-functional ACL was associated with higher prevalence of posterior extension of arthritic wear.
Conclusion
This study demonstrated a high prevalence (46.94%) of antero-medial osteoarthritis (AMOA), amenable for UKA. Patient selection is important for improving outcomes after TKA or UKA. Future studies are warranted to compare outcomes of both UKA and TKA in patients with isolated AMOA of the knee.
Keywords: Knee, Unicompartmental arthroplasty, Total knee arthroplasty, PROMS, Satisfaction
Introduction
Antero-medial osteoarthritis (AMOA) of the knee is a distinct pattern of osteoarthritis (OA) with full thickness cartilage loss on the antero-medial aspect of the tibial plateau with macroscopically normal cartilage on the posterior aspect of the medial compartment [1–3]. Unicompartmental knee arthroplasty (UKA) is an established treatment option, showing good outcomes in patients with isolated medial compartment arthritis [4–11].
Studies have shown that UKA is more likely to have excellent functional knee scores, patient satisfaction, reduced intra-operative complications, lower readmissions within the first year as well as reduced mortality compared to patients undergoing total knee arthroplasty (TKA) in patients with AMOA [10, 12, 13]. However, UKAs have reported a revision rate approximately two to three times higher than TKA in various national joint registries (NJR) based studies, which has resulted in reduced use of this technique by surgeons [14, 15]. However, analysis of the NJR data has shown that higher UKA case volumes are associated with better outcomes and reduced revision rates, leading to the recommendation that surgeons should aim for a UKA usage of at least 20% in their arthroplasty practice [15].
There is considerable variation in the criteria used to select patients who are ideal candidates for UKA. Based on the original selection criteria of Kozinn and Scott [16], only 5% of patients who required knee arthroplasty could have been considered ideal for UKA, whereas if patients are assessed based on Oxford criteria, UKA can be performed in 20 to 50% of patients requiring arthroplasty [17]. However, most of these studies have been done in Caucasian patients and cohort studies have demonstrated ethnic variations in the pattern and prevalence of osteoarthritis [18–20].
The primary aim of this study was to evaluate the prevalence of AMOA in Indian patients undergoing primary total knee arthroplasty, who would otherwise be suitable for UKA based on the Oxford selection criteria. Secondary outcome was to evaluate the relationship between obesity and its influence on arthritic wear pattern and ACL status at the time of primary TKA.
Materials and Methods
This prospective study of patients undergoing primary total knee arthroplasty (TKA) for varus deformity of the knee was conducted at a single tertiary care institute between 2017 and 2019. The study protocol was approved by the institute ethics committee [SS/2017/IEC 193] and was conducted according to the principles laid out in the declaration of Helsinki. Consent for the publication of anonymized clinical details, radiographs and intra-operative photographs was obtained from the study subjects.
All patients undergoing primary TKA for varus deformity of the knee joint secondary to primary osteoarthritis (OA) were included in this study. Patients undergoing TKA for inflammatory arthritis, post-traumatic arthritis or valgus deformities with lateral wear were excluded from the study. Patients with history of any previous knee surgeries, documented ligament injuries of the knee, high-tibial osteotomy were also excluded.
A total of 2518 consecutive knees of patients who underwent primary TKA were included in the study. This study included a total of 1936 patients (1354 unilateral TKA and 582 bilateral TKA). During pre-operative work-up, all patients were routinely evaluated with the following radiographs:
Standing radiographs of the knee (AP and True Lateral views)
Stress radiographs of the knee at 20 degrees of knee flexion (Varus and Valgus stress views)
Skyline view for the patella-femoral joint
The radiographs obtained were screened by the consultant and a research fellow. All these patients were counseled for and consented for total knee arthroplasty. They were additionally evaluated based on the Oxford Partial Knee Arthroplasty radiological decision guide [13], to identify patients with AMOA who are eligible for partial knee replacement surgery. Patients who presented with the AMOA diagnostic clinical and radiological criteria (correctable varus deformity of the knee with bone-on-bone medial OA, Functional MCL, no collapse or reduction of the lateral joint space, acceptable patellofemoral joint wear) were considered to have AMOA and ideal patients for medial unicompartmental arthroplasty (UKA).
AMOA Pattern of arthritis was again confirmed intra-operatively, with the following criteria, which were documented photographically.
Intact ACL
Functional ACL with linear striations or fibrillations
Normal lateral compartment cartilage
Antero-medial OA on the resected tibial biscuit
Absence of lateral patellar facet arthritis/ cartilage loss over the trochlea
In all cases, patellar cartilage wear was evaluated intra-operatively and classified according to the Outerbridge classification. Patients with Outerbridge arthritic grades 0–II were included and III–IV (fissuring in cartilage > 1.5 cm area down to sub-chondral bone, and exposed sub-chondral bone with bony erosion/loss, respectively) were excluded. All patients were operated through a standard midline incision and medial parapatellar approach, under spinal anesthesia. After completion of the arthrotomy, the joint was evaluated for AMOA based on intra-operative observation of cartilage wear of all three compartments, status of the ACL, PCL. All findings were photographed in all patients and documented. Intra-operative details that were recorded included the condition of anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), collateral ligaments, and articular cartilage wear pattern on the tibial plateau.
The structural and functional assessment of ACL was done intra-operatively using an arthroscopy ACL hook instrument and by performing the anterior drawer test. The status of ACL was classified as 1—normal (visually and functionally normal ACL, (Fig. 1), 2—functional ACL with Linear striations in the ligament substance (suggestive of mild structural alterations) (Fig. 2), and 3—a grossly damaged and non-functional ACL or in some cases an absent ACL (Fig. 3) [3, 21, 22].
Fig. 1.

Intra-operative photograph showing a normal functional ACL, medial femoral wear, normal lateral femoral cartilage
Fig. 2.

Intra-operative photograph showing a functional ACL with linear striations
Fig. 3.

Intra-operative photograph showing an absent ACL
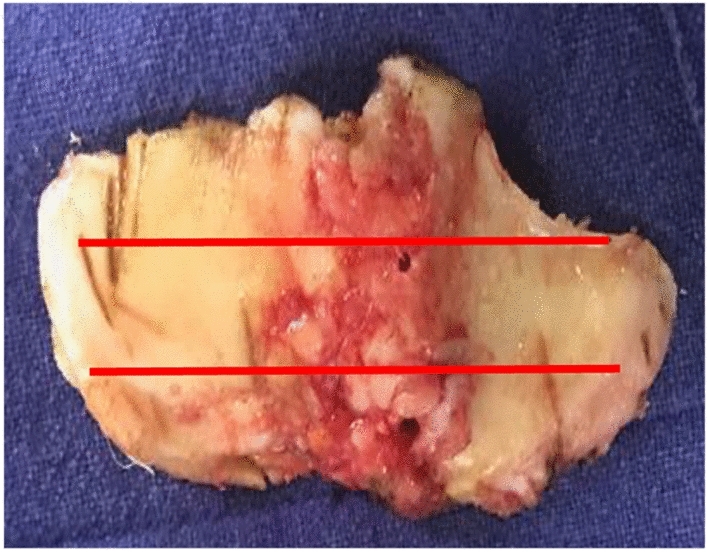
During TKA bone preparation, the tibial plateau was resected 2 mm below the involved side (medial tibial plateau) and the resected tibial plateau was assessed for cartilage wear pattern. The resection depth was decided by the tibial resection stylus placed at the depth of the medial defect. The medial tibial plateau was divided into three equal segments antero-posteriorly by two lines drawn transversely (Figs. 4, 5, 6). Based on the location of medial tibial wear, the pattern of OA was classified as antero-medial (AMOA, Fig. 4), central (Fig. 5) and postero-medial OA (Fig. 6). Cartilage wear in all the segments was assessed for Outerbridge grade IV changes [23]. The knee was considered to have AMOA if there was full thickness cartilage wear in the antero-medial and central segments (not extending to the posterior region) and in this subset, if the ACL was intact, the knee was considered to have been amenable for a UKA.
Fig. 4.
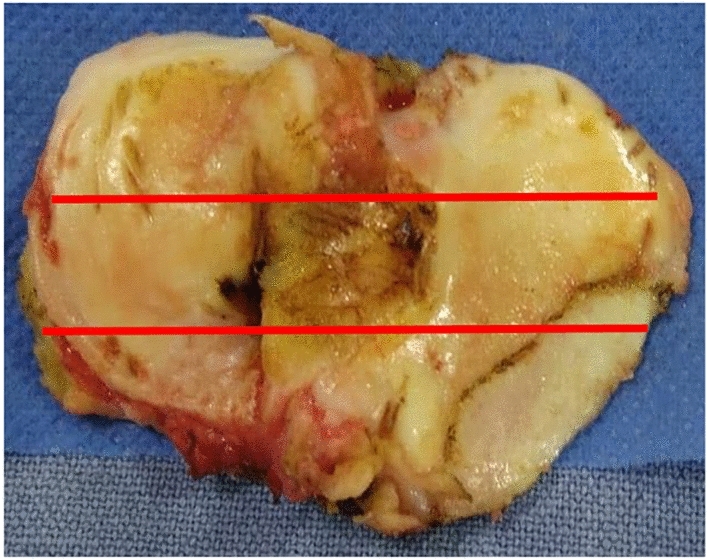
Tibial plateau resection showing antero-medial osteoarthritis of the knee
Fig. 5.

Tibial plateau resection showing antero-medial and central–medial osteoarthritis of the knee
Fig. 6.
Tibial plateau resection showing postero-medial osteoarthritis of the knee
Statistical Methods
Prevalence rate of Isolated medial compartment arthritis of the knee, amenable for UKA, was calculated based on the percentage of knees with antero-medial and centro-medial arthritis of the medial compartment along with other Oxford Criteria. Chi-Squared test was used to assess categorical data, such as significance of BMI (Obese versus Non-obese) in relation to pattern of arthritic wear and ACL status. Continuous data was analyzed with paired t-test. Analysis was conducted using the SPSS 21 Statistical package.
Results
2518 knees (1936 patients with 1354 unilateral TKA and 582 bilateral TKA). were evaluated at the time of primary TKA for prevalence of isolated antero-medial arthritis of the knee. In this study group, there was a female preponderance with 1715 (68.1%) knees in females and 803 (31.89%) knees in male patients. The average age was 62 years (range 48–72 years). The average BMI of all the patients was 30.5 (28 to 35). The average BMI between the genders was comparable (31 kg/m2 in females and 30 kg/m2 in males, p = 1.475). The baseline characteristics of the study population are summarized in Table 1.
Table 1.
Baseline characteristics of study population
| Parameter | |
|---|---|
| Age (years), mean with SD | 62.01 (8.02) |
| Gender distribution (n, %) | |
| Male | 803 (31.89%) |
| Female | 1715 (68.10%) |
| BMI, mean (SD) | 30.50 (16.75) |
| Operated side distribution | |
| Left knee | 1264 (50.2%) |
| Right knee | 1254 (49.8%) |
| ASA classification | |
| ASA I | 758 (30.1%) |
| ASA II | 1760 (69.9%) |
| Patellar wear (Outerbridge classification) | |
| Grade 1 | 226 (8.90%) |
| Grade 2 | 1617 (64.2%) |
| Grade 3 | 575 (22.83%) |
| Grade 4 | 100 (3.97%) |
| Pre-operative deformity (in degrees) | 10.8 (4.64) |
Tibial Wear Pattern
Isolated anterior-medial segment cartilage wear of tibia was documented in 760 knees (30.2%), involvement of anterior and central segment cartilage wear was documented in 527 knees (20.9%), totally accounting for 51.1% of cases undergoing primary TKA.
Of these cases, based on Oxford criteria of isolated antero-medial and centro-medial arthritis of the medial compartment of the knee, Intact ACL, with acceptable patellofemoral wear, without radiological or clinical evidence of reduction in lateral compartment space, we report a prevalence of 46.94% (1182 knees of 2518 knees) of AMOA cases which are amenable for uni-compartmental knee arthroplasty.
Involvement of entire medial compartment of tibial plateau (extending to the posterior-medial segment) was seen in 1231 knees (48.9%).
ACL Status
A total of 1306 knees (51.9%) had an intact functional ACL, 194 knees (7.7%) had a striated but functional ACL, and 1018 knees (40.4%) had a non-functional or absent ACL.
Correlation of Medial Tibial Plateau Wear Pattern with ACL Status
Isolated Anterior Segment Tibial Wear Pattern and Status of ACL
760 knees with isolated anterior-medial wear (30%) had an intact ACL and 5.1% of knees [39] had linear striations. Figure 7 shows the frequency distribution of patients with isolated antero-medial segment wear of the medial tibial plateau. Significantly high number of cases were associated with intact and functional ACL.
Fig. 7.
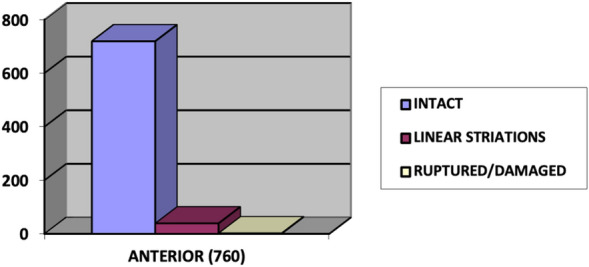
Frequency distribution of patients with isolated antero-medial segment wear of the medial tibial plateau based on ACL status
Central–Medial Segment Tibial Wear Pattern and Status of ACL
422 patients (16.75%) with central wear had an Intact ACL, 0.03% [1] had linear striation and 105 patients (4.16%) had ruptured or damaged ACL. Figure 8 shows the frequency distribution of patients with isolated centro-medial segment wear of the medial tibial plateau based on ACL status. Significantly high number of cases were associated with intact and functional ACL.
Fig. 8.
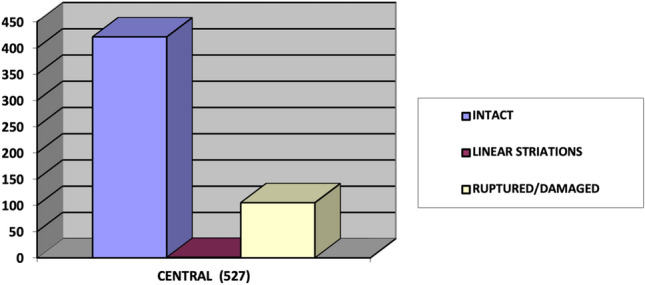
Frequency distribution of patients with isolated centro-medial segment wear of the medial tibial plateau based on ACL status
Posterior Segment Tibial Wear Pattern and Status of ACL
Majority of patients with Posterior wear 911 (36.17%) had damaged or ruptured ACL, 154 patients (6.11%) had linear striations, 166 Patients (6.59%) with posterior wear had an intact ACL. Figure 9 shows the frequency distribution of patients with posterior segment arthritic wear of the medial tibial plateau. Significantly high number of cases were associated with ruptured and non-functional ACL.
Fig. 9.

Frequency distribution of patients with posterior segment arthritic wear of the medial tibial plateau, based on ACL status
Correlation of BMI with ACL Status and Tibial Wear
We observed that obese patients (BMI > 30) had statistically significant prevalence of ACL deficiency and postero-medial tibial wear. The relation between BMI and ACL status is summarized in Table 2. The relation between BMI and pattern of arthritic wear of the study population is summarized in Table 3.
Table 2.
Evaluation of relationship between BMI and ACL status
| ACL status | BMI < 30 | BMI > = 30 | P-Value* |
|---|---|---|---|
| Intact | 806 (32%) | 500 (19.8%) | < 0.05 |
| Linear striations, functional | 84 (3.33%) | 110 (4.36%) | < 0.05 |
| Damaged, non-functional | 466 (18.5%) | 552 (21.9%) | < 0.05 |
*Chi-squared test
Table 3.
Evaluation of relationship between BMI and arthritic wear pattern
| Tibial wear | BMI < 30 | BMI > = 30 | P-Value* |
|---|---|---|---|
| Anterior | 550 (21.8%) | 210 8.33%) | < 0.05 |
| Central | 298 (11.83%) | 229 (9.09%) | > 0.05 |
| Posterior | 508 (20.17%) | 723 (28.71%) | < 0.05 |
*Chi-squared test
Discussion
The results of the present study indicate that more than 45% of Indian patients undergoing primary total knee arthroplasty for varus osteoarthritis may be suitable for a medial uni-compartmental knee arthroplasty based on oxford criteria.
In 1991 White et al. [1] characterized a special phenotype of OA known as antero-medial osteoarthritis (AMOA) which is full thickness cartilage erosion on the antero-medial tibial plateau and this term has entered the general concourse on varus knee deformity [24]. AMOA has become the primary indication for medial uni-compartmental knee arthroplasty (UKA) [25]. In this uniform pattern of involvement, also described as antero-medial Gonarthrosis (AMG), the posterior part of the tibia exhibits a normal full thickness cartilage and, full thickness loss of cartilage anteromedially with an intact ACL [1–3, 25].
An intact ACL is the prerequisite for mobile bearing medial UKR [25]. Numerous papers have reported varying percentages of intactness of ACL in osteoarthritis, which ranges from as low as 25% to as high as 94% in different ethnicities [18, 21, 26–34]. The findings of these studies are summarized in Table 4. One study conducted in Asian population demonstrated 66% ACL intact knees; however, it included only 100 knees [21]. To our knowledge, this is the only study that has evaluated ACL functional status and its influence on the pattern of arthritis.
Table 4.
Comparison of published literature reports on the status of the anterior cruciate ligament in patients with osteoarthritis of the knee
| Authors | Year | Number | Intact ACL | Country | |
|---|---|---|---|---|---|
| 1 | Cloutier [26] | 1983 | 110 | 43% | Canada |
| 2 | Harman et al. [18] | 1998 | 143 | 75% | US |
| 3 | Jenny and Jenny [27] | 1998 | 125 | 25% | France |
| 4 | Cloutier et al. [28] | 1999 | 204 | 80% | Canada |
| 5 | Lee et al. [29] | 2005 | 107 | 71% | US |
| 6 | Mullaji et al. [21] | 2008 | 100 | 66% | Asian |
| 7 | Trompeter et al. [30] | 2009 | 50 | 56% | UK |
| 8 | Dodd et al. [31] | 2010 | 50 | 86% | UK |
| 9 | Douglas et al. [32] | 2010 | 95 | 88% | UK |
| 10 | Johnson et al. [33] | 2012 | 200 | 78% | USA |
| 11 | Ishii et al. [34] | 2016 | 247 | 94% | Japan |
| 12 | Present study | 2017 | 2518 | 51% | India |
It has been shown with the integrity of ACL the predominant part of tibia affected is antero-medial. ACL tears have the biomechanical effect of increasing antero-posterior laxity by allowing the tibia to sublux anteriorly on the femur. With ACL disruption wear progresses to affect the postero-medial compartment [25]. Mullaji et al. [21] reported 85% of ACL intact knees demonstrated AMOA in their evaluation of arthritic wear patterns in Asian population. To the best of our knowledge the present study (2518 knees) is the largest series documenting the ACL integrity and arthritic wear pattern in Asian population.
Mullaji et al. [21] found that there was no correlation between BMI and the observed wear pattern on the tibial plateau (correlation coefficient = 0.19) which is in contrast with our study which found a statistically significant relation of BMI and Age on wear pattern and ACL status.
Patello-femoral joint OA being a contraindication for mobile bearing UKA is still questionable. Anterior knee pain does not negatively influence early functional outcomes of a mobile bearing UKA [35, 36]. Hamilton et al. [37] in their 10-year functional outcome study concluded that even severe medial patellofemoral osteoarthritis can be overlooked whereas lateral PFJ compromises on stair descent.
Dissatisfaction rates following TKA have been reported to be between 14 and 39% [38–40]. In one study involving patients undergoing staged knee arthroplasty, more than 50% subjects who had one knee operated with UKA and the opposite knee operated with TKA, favored the UKA over TKA [41].
With a high prevalence of AMOA in Indian patients undergoing TKA, we believe that this subset of patients will benefit from UKA. However, the success of partial knee arthroplasty is dependent on surgeon experience and UKA volumes in their centers. Future studies are needed to compare functional outcomes and clinical benefits of UKA over TKA in patients with AMOA to establish a clinical practice guideline.
Conclusion
This study demonstrated a high prevalence (46.94%) of antero-medial osteoarthritis (AMOA) in Indian patients undergoing primary total knee arthroplasty. These patients were all amenable to medial unicompartmental arthroplasty based on Oxford selection criteria. Patient selection is important for improving outcomes after TKA or UKA. Future studies are warranted to compare outcomes of both UKA and TKA in patients with isolated AMOA of the knee.
Author Contributions
Conceptualization: AVGR, AA; Methodology: DD, AA; Formal Analysis and Investigation: DD, VK, PM; Writing—Original Draft: DD, VK; Writing—Review and Editing: PM, SRS, KKE; Resources: AVGR; Supervision: AVGR, KKE.
Compliance with Ethical Standards
Conflict of Interest
None of the authors have a financial or personal relationship with a third party whose interests could be positively or negatively influenced by the article’s content.
Ethical Approval
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Adarsh Annapareddy, Email: dradarshannapareddy@gmail.com.
Deepesh Daultani, Email: deepesh.daultani@gmail.com.
Praharsha Mulpur, Email: praharshamulpur9@gmail.com.
Vishesh Khanna, Email: visheshkhanna85@gmail.com.
Sukesh Rao Sankineani, Email: sukeshrao.sankineni@gmail.com.
Krishna Kiran Eachempati, Email: kke1975@gmail.com.
A. V. Gurava Reddy, Email: guravareddy@gmail.com.
References
- 1.White SH, Ludkowski PF, Goodfellow JW. Anteromedial osteoarthritis of the knee. Journal of Bone and Joint Surgery. British Volume. 1991;73:582–586. doi: 10.1302/0301-620X.73B4.2071640. [DOI] [PubMed] [Google Scholar]
- 2.Lankester BJ, Cottam HL, Pinskerova V, et al. Variation in the anatomy of the tibial plateau: A possible factor in the development of anteromedial osteoarthritis of the knee. Journal of Bone and Joint Surgery. British Volume. 2008;90:330–333. doi: 10.1302/0301-620X.90B3.19898. [DOI] [PubMed] [Google Scholar]
- 3.Rout R, McDonnell S, Price A, et al. The pattern of cartilage damage in antero-medial osteoarthritis of the knee and its relationship to the anterior cruciate ligament. Journal of Orthopaedic Research. 2013;31(6):908–913. doi: 10.1002/jor.22253. [DOI] [PubMed] [Google Scholar]
- 4.Pandit H, Hamilton TW, Jenkins C, et al. The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. The Bone & Joint Journal. 2015;97:1493–1500. doi: 10.1302/0301-620X.97B11.35634. [DOI] [PubMed] [Google Scholar]
- 5.Borus T, Thornhill T. Unicompartmental knee arthroplasty. Journal of the American Academy of Orthopaedic Surgeons. 2008;16(1):9–18. doi: 10.5435/00124635-200801000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Deshmukh RV, Scott RD. Unicompartmental knee arthroplasty: long-term results. Clinical Orthopaedics and Related Research. 2001;392:272–278. doi: 10.1097/00003086-200111000-00035. [DOI] [PubMed] [Google Scholar]
- 7.Berger, R. A., Meneghini, R. M., & Jacobs, J. J., et al. (2005). Results of unicompartmental knee arthroplasty at a minimum of ten years of followup. The Journal of Bone and Joint Surgery. 87(5):999–1006. [DOI] [PubMed]
- 8.Pandit H, Jenkins C, Barker K, Dodd CAF, Murray DW. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. The Journal of Bone and Joint Surgery. British volume. 2006;88-B(1):54–60. doi: 10.1302/0301-620X.88B1.17114. [DOI] [PubMed] [Google Scholar]
- 9.Rougraff BT, Heck DA, Gibson AE. A comparison of tricompartmental and unicompartmental arthroplasty for the treatment of gonarthrosis. Clinical Orthopaedics and Related Research. 1991;273:157–164. doi: 10.1097/00003086-199112000-00024. [DOI] [PubMed] [Google Scholar]
- 10.Lombardi AV, Jr, Kolich MT, Berend KR, Morris MJ, Crawford DA, Adams JB. Revision of unicompartmental knee arthroplasty to total knee arthroplasty: Is it as good as a primary result? Journal of Arthroplasty. 2018;33(7S):S105–S108. doi: 10.1016/j.arth.2018.03.023. [DOI] [PubMed] [Google Scholar]
- 11.Campi S, Tibrewal S, Cuthbert R, Tibrewal SB. Unicompartmental knee replacement—Current perspectives. J Clin Orthop Trauma. 2018;9(1):17–23. doi: 10.1016/j.jcot.2017.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laurencin CT, Zelicof SB, Scott RD, Ewald FC. Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clinical Orthopaedics and Related Research. 1991;273:151–156. doi: 10.1097/00003086-199112000-00023. [DOI] [PubMed] [Google Scholar]
- 13.Liddle AD, Pandit H, Judge A, Murray DW. Patient-reported outcomes after total and unicompartmental knee arthroplasty: A study of 14,076 matched patients from the National Joint Registry for England and Wales. The Bone and Joint Journal. 2015;97-B(6):793–801. doi: 10.1302/0301-620X.97B6.35155. [DOI] [PubMed] [Google Scholar]
- 14.Swank M, Stulberg SD, Jiganti J, Machairas S. The natural history of unicompartmental arthroplasty. An eight-year follow-up study with survivorship analysis. Clinical Orthopaedics and Related Research. 1993;286(286):130–142. [PubMed] [Google Scholar]
- 15.Murray DW, Liddle AD, Dodd CA, Pandit H. Unicompartmental knee arthroplasty: Is the glass half full or half empty? The Bone and Joint Journal. 2015;97-B(10 Suppl A):3–8. doi: 10.1302/0301-620X.97B10.36542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kozinn SC, Scott R. Unicondylar knee arthroplasty. The Bone and Joint Journal [Am] 1989;71-A:145–150. [PubMed] [Google Scholar]
- 17.Pandit H, Jenkins C, Gill HS, Smith G, Price AJ, Dodd CA, Murray DW. Unnecessary contraindications for mobile-bearing unicompartmental knee replacement. Journal of Bone and Joint Surgery. British Volume. 2011;93:622–628. doi: 10.1302/0301-620X.93B5.26214. [DOI] [PubMed] [Google Scholar]
- 18.Harman MK, Markovich GD, Banks SA, Hodge WA. Wear patterns on tibial plateaus from varus and valgus osteoarthritic knees. Clinical Orthopaedics and Related Research. 1998;352:149–158. [PubMed] [Google Scholar]
- 19.Takahashi TS, Naomi S, Takeshi S, Kohji S, Gerard CG. Patterns of patellofemoral articular cartilage wear in Japanese cadavers. Journal of the Anatomical Society of India. 2017;66(2):83–90. doi: 10.1016/j.jasi.2017.11.004. [DOI] [Google Scholar]
- 20.Hodge WA, Harman MK, Banks SA. Patterns of knee osteoarthritis in Arabian and American knees. Journal of Arthroplasty. 2009;24(3):448–453. doi: 10.1016/j.arth.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 21.Mullaji AB, Marawar SV, Luthra M. Tibial articular cartilage wear in varus osteoarthritic knees: Correlation with anterior cruciate ligament integrity and severity of deformity. Journal of Arthroplasty. 2008;23(1):128–135. doi: 10.1016/j.arth.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 22.Waldstein W, Merle C, Monsef JB, Boettner F. Varus knee osteoarthritis: How can we identify ACL insufficiency? Knee Surgery, Sports Traumatology, Arthroscopy. 2015;23(8):2178–2184. doi: 10.1007/s00167-014-2994-5. [DOI] [PubMed] [Google Scholar]
- 23.Outerbridge RE. The etiology of chondromalacia patellae. The Journal of Bone and Joint Surgery British volume. 1961;43-B:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 24.Thienpont E, Parvizi J. A new classification for the varus knee. Journal of Arthroplasty. 2016;31(10):2156–2160. doi: 10.1016/j.arth.2016.03.034. [DOI] [PubMed] [Google Scholar]
- 25.Goodfellow JW, O’Connor JJ, Dodd CAF, et al. Oxford unicompartmental knee replacement. 1. Oxford University Press; 2006. [Google Scholar]
- 26.Cloutier JM. Results of total knee arthroplasty with a non-constrained prosthesis. Journal of Bone and Joint Surgery. American Volume. 1983;65:906–919. doi: 10.2106/00004623-198365070-00005. [DOI] [PubMed] [Google Scholar]
- 27.Jenny JY, Jenny G. Preservation of anterior cruciate ligament in total knee arthroplasty. Archives of Orthopaedic and Trauma Surgery. 1998;118:145–148. doi: 10.1007/s004020050335. [DOI] [PubMed] [Google Scholar]
- 28.Cloutier JM, Sabouret P, Deghrar A. Total knee arthroplasty with retention of both cruciate ligaments. A nine to eleven-year fol-low-up study. The Journal of Bone & Joint Surgery. 1999;81:697–702. doi: 10.2106/00004623-199905000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Lee GC, Cushner FD, Vigoritta V, Scuderi GR, Insall JN, Scott WN. Evaluation of the anterior cruciate ligament integrity and degenerative arthritic patterns in patients undergoing total knee arthroplasty. Journal of Arthroplasty. 2005;20:59–65. doi: 10.1016/j.arth.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 30.Trompeter AJ, Gill K, Appleton MA, Palmer SH. Predicting anterior cruciate ligament integrity in patients with osteoarthritis. Knee Surgery, Sports Traumatology, Arthroscopy. 2009;17(6):595–599. doi: 10.1007/s00167-008-0701-0. [DOI] [PubMed] [Google Scholar]
- 31.Dodd M, Trompeter A, Harrison T, Palmer S. The pivot shift test is of limited clinical relevance in the arthritic anterior cruciate ligament-deficient knee. The Journal of Knee Surgery. 2010;23:131–135. doi: 10.1055/s-0030-1267473. [DOI] [PubMed] [Google Scholar]
- 32.Douglas MJ, Hutchinson JD, Sutherland AG. Anterior cruciate ligament integrity in osteoarthritis of the knee in patients undergoing total knee replacement. Journal of Orthopaedics and Traumatology. 2010;11(3):149–154. doi: 10.1007/s10195-010-0103-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson AJ, Howell SM, Costa CR, et al. The ACL in the arthritic knee: How often is it present and can preoperative tests predict its presence? Clinical Orthopaedics and Related Research. 2013;471(1):181–188. doi: 10.1007/s11999-012-2505-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ishii Y, Noguchi H, Sato J. Macroscopic evaluation of the anterior cruciate ligament in osteoarthritic patients undergoing total knee arthroplasty. European Journal of Orthopaedic Surgery & Traumatology. 2016;26(2):205. doi: 10.1007/s00590-015-1736-9. [DOI] [PubMed] [Google Scholar]
- 35.Beard DJ, Pandit H, Gill HS, et al. The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. The Journal of Bone and Joint Surgery British Volume. 2007;89-B:1597–1601. doi: 10.1302/0301-620X.89B12.19259. [DOI] [PubMed] [Google Scholar]
- 36.Beard DJ, Pandit H, Ostlere S, et al. Pre-operative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. The Journal of Bone and Joint Surgery British Volume. 2007;89-B:1602–1607. doi: 10.1302/0301-620X.89B12.19260. [DOI] [PubMed] [Google Scholar]
- 37.Hamilton TW, Pandit HG, et al. Anterior knee pain and evidence of osteoarthritis of the patellofemoral joint should not be considered contraindications to mobile-bearing unicompartmental knee arthroplasty. The Bone and Joint Journal. 2017;99-B:632–639. doi: 10.1302/0301-620X.99B5.BJJ-2016-0695.R2. [DOI] [PubMed] [Google Scholar]
- 38.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clinical Orthopaedics and Related Research. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 39.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clinical Orthopaedics and Related Research. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suda AJ, Seeger JB, Bitsch RG, Krueger M, Clarius M. Are patients’ expectations of hip and knee arthroplasty fulfilled? A prospective study of 130 patients. Orthopedics. 2010;33(2):76–80. doi: 10.3928/01477447-20100104-07. [DOI] [PubMed] [Google Scholar]
- 41.Dalury DF, Fisher DA, Adams MJ, Gonzales RA. Unicompartmental knee arthroplasty compares favorably to total knee arthroplasty in the same patient. Orthopedics. 2009 doi: 10.3928/01477447-20090401-21. [DOI] [PubMed] [Google Scholar]


