Authors’ financial ties with pharmaceutical companies can affect the design, conduct and reporting of clinical trials.1, 2 Although disclosure does not eliminate conflicts of interest (COI), it allows readers and reviewers to consider potential impacts. A systematic review of studies comparing authors’ self-reported COI disclosure with company payment reports 3 found 23 studies (22 US and 1 Danish 4 ; n=5984 authors) with a pooled prevalence of non-disclosure of 66% (95% CI 48–78%). To our knowledge, the adequacy of authors’ disclosures has not been examined in other countries. Since October 2015, Medicines Australia, Australia’s pharmaceutical industry association, has required member companies to report all payments to individual clinicians for consultancies, speaking, advisory boards and educational events.5
This study compares disclosure of industry payments by Australian authors with Medicines Australia (MA) company reports. We examined COI declarations by clinician authors of randomised controlled trials (RCTs) published between January and August 2020, including completeness of authors’ declarations and compliance with International Committee of Medical Journal Editors (ICMJE) criteria.
METHODS
We used two data sources to determine industry payments to authors: MA’s centralised database (www.disclosureaustralia.com.au), from October 2018 to December 2019, and company reports dated from October 2015 to October 2018 via a publicly accessible database. We applied ICMJE standards for timing and relevance of funding.
To identify RCTs with at least one Australian author, we searched Medline using the Cochrane RCT search strategy, limited by the mention of Australia in the text and author affiliations, from January 1 to August 15, 2020. We used duplicate independent screening to identify drug trials (prescription drugs, biologics or vaccines) involving patients. We excluded protocols, secondary analyses and healthy volunteer trials.
If the article submission date was listed, payments within 36 months prior were included. If not, we included payments 39 months prior (imputed 3-month submission period). For all undisclosed payments, we checked companies’ websites for activity in the relevant commercial space, as defined by ICMJE (markets products for the same therapeutic class or condition). We coded payments, published COI, and commercial space in duplicate, with discrepancies resolved by consensus.
RESULTS
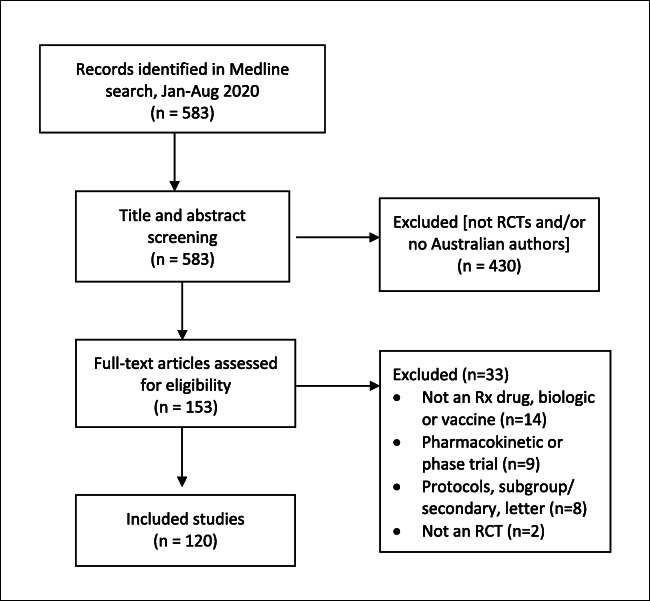
Our search identified 583 unique records, with 430 excluded at the title and abstract stage. Of the remaining 153, 120 met our inclusion criteria (Fig. 1). These trials included 323 Australian authors, 28 of whom authored at least two studies. Most trials (88%) also had non-Australian authors. Table 1 describes COI reporting per study, author and journal. In total, there were 89 missing or incomplete COI declarations among 78 authors in 56 trials (46.6% of trials and 24.1% of Australian authors in the 120 trials). Most authors with inconsistent statements declared they had no COI (46/89, 51.7%), followed by partial declarations with some omitted payments (39/89, 43.8%). The remainder did not name companies (n=2) or the article had no COI statement (n=2). The median value of the 78 authors’ undisclosed payments was AU$8,944 (US$6,543) [range AU$140 to $97,600 (US$102–$71,394)]. We removed imputed 3-month submission times in a sensitivity analysis. Results were similar: 77 vs. 78 authors with undeclared COI.
Figure 1.
Flow chart of study sample selection
Table 1.
Conflict of interest (COI) reporting by Australian clinical trial authors, January to August 2020
| n (%) | |
|---|---|
| Study reports | 120 (100) |
| All relevant COI declared | 64 (53.3) |
| ≥ 1 Australian author with missing or incomplete COI declaration | 56 (46.6) |
| 1 author | 36 (30.0) |
| 2 authors | 13 (10.8) |
| ≥3 authors | 7 (5.8) |
| Authors | 323 (100) |
| All relevant COI declared* | 245 (75.9) |
| ≥ 1 undeclared COI | 78 (24.1) |
| Types of inconsistent COI declarations | 89 (100) |
| No declaration of COI | 46 (51.7) |
| Partial declaration (some but not all COI) | 39 (43.8) |
| No named companies** | 2 (2.2) |
| Article includes no COI statement | 2 (2.2) |
| Journals with Australian authors with missing or incomplete COI | 32 (100) |
| ICMJE or stricter COI declaration policies | 19 (59.4) |
| Less strict than ICMJE or vague author guidance | 13 (40.6) |
*Includes authors with no COI, authors with complete COI disclosure, and non-clinician authors (no data available in the Medicines Australia database)
**Authors’ COI statements list only “pharmaceutical companies” or “multiple unnamed pharmaceutical companies”, without stating which companies provided funding
The 56 trials involving authors with inconsistent COI declarations were published in 32 journals, 19 of which apply ICMJE or stricter standards; in these, 39.9% (63/158) of authors in 41 trials had inconsistent declarations. The remaining 13 journals provided unclear guidance on disclosure, such as no timeframe, or lower standards than ICMJE; in the 15 trials in these journals, 44.8% (26/58) of authors had inconsistent declarations.
DISCUSSION
In this sample of trials authored by Australian clinicians, missing and incomplete COI declarations were common. Nearly half of the reports and one-fourth of the authors had missing or incomplete declarations, and over half of these authors reported no COI despite relevant industry funding.
Our results likely underestimate non-reporting as MA’s database only includes clinicians; food, drink and research funding are omitted; and payment reports include only its 35 member companies. Judgments of clinical relevance may also differ, although we applied ICMJE standards.
Similarly to US and Danish studies, COI disclosures of Australian authors are often incomplete.3 These discrepancies highlight the need for more transparent and comprehensive COI reporting. Our study adds to the evidence that under-reporting of COI is likely widespread globally.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lundh A, Lexchin J, Mintzes B, Schroll JB, Bero L. Industry sponsorship and research outcome. Cochrane Database Syst Rev 2017;2:MR000033. 10.1002/14651858.MR000033.pub3. pmid:28207928 [DOI] [PMC free article] [PubMed]
- 2.Fabbri A, Lai A, Grundy Q, Bero LA. The influence of industry sponsorship on the research agenda: a scoping review. Am J Public Health. 2018;108:e9–16. doi: 10.2105/AJPH.2018.304677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taheri C, Kirubarajan A, Li X, et al. Discrepancies in self-reported financial conflicts of interest disclosures by physicians: a systematic review. BMJ Open 2021;11:e045306. 10.1136/bmjopen-2020-045306
- 4.Rasmussen K, Schroll J, Gøtzsche PC, Lundh A. Under-reporting of conflicts of interest among trialists: a cross-sectional study. J R Soc Med. 2015;108(3):101–7. doi: 10.1177/0141076814557878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mintzes B, Karanges E, Bero L. Pharmaceutical Industry Payments to Australian Healthcare Professionals (October 2015 to October 2018). The University of Sydney, 2019. 10.25910/5d6710d1d3d20. Permanent link: https://ses.library.usyd.edu.au/handle/2123/20945.