Abstract
COVID-19 vaccines are essential public health tools for protecting older adults, who are at high risk of severe outcomes associated with COVID-19. Little is known, however, about how older adults approach the decision to receive a COVID-19 vaccine. We hypothesized that intersections between gender and race may provide unique insight into the decision-making process and the factors that lead to vaccine uptake among hesitant individuals. We performed in-depth interviews with 24 older adults who had been vaccinated against COVID-19 and used the framework approach with an intersectional lens to analyze data. Two typologies emerged: eager compliers did not question the need to vaccinate, whereas hesitant compliers were skeptical of the vaccine and underwent a thorough decision-making process prior to vaccination. For eager compliers, the vaccine offered protection from a disease that posed a serious threat, and few risks were perceived. In contrast, hesitant compliers perceived risks associated with the vaccine product or mistrusted the infrastructure that led to rapid vaccine development. Hesitancy was greater among Black participants, and only Black participants reported mistrust in vaccine infrastructure. At the intersection of gender and race, a ‘White male effect’ was observed, whereby White men perceived the fewest risks associated with the vaccine, and Black women were the most fearful of serious side effects. Nearly all hesitant compliers ultimately got vaccinated due to the threat of COVID-19. Convenient access through vaccine clinics in senior’s buildings was pivotal for hesitant compliers and external and internal influences had differential impacts by race and gender. Emphasizing the risk of COVID-19, convenient and accessible opportunities for vaccination, and messages that are targeted to specific groups are likely to increase vaccine uptake among older adults.
Keywords: Aging, Health disparities, SARS-CoV-2, Vaccine hesitancy
1. Introduction
Older adults are at elevated risk of hospitalization, disability, and death associated with COVID-19 [1], [2], [3]. Vaccination programs that meet the needs of this vulnerable population are, therefore, of considerable public health importance. Much of the existing research measuring the success of vaccine programs is rooted in coverage rates, often ignoring the complexities of how people make decisions about vaccines, and barriers to accessing recommended vaccines. Vaccine behavior (i.e., whether an individual accepts a vaccine), however, does not reveal the true scope of vaccine hesitancy, defined as a continuum between individuals who accept all vaccines with no doubts and those who refuse all vaccines with no doubts [4]. Individuals who accept all vaccines according to recommendations, or who delay vaccination, may be hesitant despite their observed behavior [5]. While the immediate public health concerns surrounding vaccine hesitancy involve those who refuse or delay vaccination, those who accept vaccines but have concerns may be particularly vulnerable to being swayed by misinformation about vaccines and are at risk of refusing vaccines in the future [5]. Individuals who accept vaccines despite hesitations are likely to have carefully considered whether to receive the vaccine and are thus valuable sources of information regarding factors that contribute to vaccine acceptance.
The decision to receive a vaccine is complex, with many contributing factors, including perceived importance of the vaccine, risk perception, trust in healthcare professionals, the government and public health institutions, and past experiences (i.e., adverse events following immunization, negative experiences in healthcare settings) [6], [7]. The influence of gender norms, roles, and relations is often over-looked in the vaccine hesitancy literature, yet there is substantial evidence from other areas of health research that men and women are likely to approach vaccine decisions differently [8]. For example, men’s vaccine decision-making process may be affected by masculine norms prescribing independence and self-reliance, which translate into lower likelihood of seeking healthcare and increased likelihood of partaking in risky behaviors [9], [10]. There are also gender differences in risk perception, with women and men perceiving the same risks differently or perceiving different risks altogether [11]. For example, during the COVID-19 pandemic, women surveyed in the U.S. perceived a greater risk of disease, while men perceived a greater risk of financial hardship (i.e., job loss or reduced income) [12]. In the case of vaccination, differences in risk perception are compounded, as vaccine acceptance can be the result of weighing both the perceived risks associated with the disease prevented by the vaccine (i.e., the risks associated with COVID-19) and the perceived risks associated with the vaccine itself (i.e., side effects) [13].
Gender norms, roles, and relations must be considered in the context of their intersection with other social stratifiers, such as race [14]. Following the theory of intersectionality, the relationships between factors and differences within groups can explain and resolve inequities in health outcomes [15]. Racial disparities in vaccine uptake have been most extensively studied in the context of seasonal influenza vaccination, where the perceived risks of both the disease and the vaccine, beliefs, attitudes, and trust in healthcare have been identified as contributing factors [16], [17], [18], [19], [20], [21], [22]. The direct impact of lived experiences of race and racism in healthcare has also been investigated, with perceived racial fairness emerging as a powerful predictor of vaccine attitudes, such that experiences of unfair treatment by a healthcare professional discourage vaccination [23]. While racial disparities in vaccine attitudes and uptake have been observed during COVID-19 [24], little is known about the intersection of race and gender.
In the context of the COVID-19 pandemic, it is increasingly important to understand how older adults make decisions about vaccines. Much of the literature available on this topic has focused on the seasonal influenza vaccine, but there is evidence to suggest that the decision-making process may be substantially different for the COVID-19 vaccines, given the novelty and rapid development of the vaccines and the politically charged environment of the pandemic [25], [26]. We hypothesized that previously unexplored links between gender and race may provide unique insight into the decision-making process and what factors ultimately lead to acceptance among hesitant individuals. Through qualitative analysis of in-depth interviews (IDI) with older adults, we aimed to understand how these factors can be leveraged to design more effective public health messaging and vaccine programs for this diverse group of individuals.
2. Methods
2.1. Context
This study took place in the greater Baltimore area, where the population is 30 % White, 62 % Black, and 5 % Hispanic or Latino, and 14 % of city residents are over the age of 65 [27]. Median household income in 2019 was $50,177 and an estimated 17 % of the population over 65 years of age lived below the federal poverty line, compared to national averages of $65,712 and 9 %, respectively [28]. As of this writing, 82 % and 94 % of those over 65 are fully vaccinated against COVID-19 (i.e., received two doses of the Pfizer or Moderna vaccine or one dose of an Johnson and Johnson vaccine) in Baltimore City and County, respectively [29]. Racial inequities in vaccine coverage were prominent among older adults early in the vaccination campaign, however, concerted efforts by the Baltimore City Health Department, partners, and the state’s Vaccine Equity Task Force led to significant improvements in vaccine coverage equity [30], [31], [32]. For example, according to the Baltimore City COVID-19 Vaccination Dashboard, on June 1st 2021, there was a 20 percentage point difference in vaccine coverage between Black and White residents (35 % vs 55 %) but this gap was reduced to 12 percentage points (57 % vs 69 %) by September 2022 [33]. Data disaggregated by both age and race at the city level are limited, but state-level data suggest uniformly high coverage among older adults by the end of 2021 [34].
2.2. Participants and recruitment
Individuals were eligible to participate if they were over the age of 70 and resided in the Baltimore area. Although the age of 65 is often used as the cut-off for older adults, in pilot data, we found that many individuals between the ages of 65 and 70 were not fully retired, and thus had different experiences of the vaccine decision-making process due to their employment (i.e., mandatory vaccination of healthcare workers, feeling at high risk of infection due to childcare work). We therefore restricted analysis to retired individuals over the age of 70. Participants were either recruited from the community or selectively sampled from an existing cohort of older adults [35]. Community recruitment included distributing flyers in seniors’ buildings, snowball sampling, and referrals from Baltimore’s Vaccine Acceptance & Access Lives in Unity Education and Engagement (VALUE) ambassadors. Recruitment was limited to those with a ZIP code that began with “212” to ensure that all participants were located in the greater Baltimore area. Purposive sampling from the existing cohort was based on approximately matching ages to those who had been recruited from the community. Recruitment efforts focused on obtaining a sample with approximately equal numbers of participants by gender and race. Most White participants came from the existing cohort [35], and most Black participants were recruited from the community. Recruitment continued until saturation was achieved, in that interviews no longer yielded new information.
2.3. Data collection
Semi-structured IDI were conducted from October 2021 – February 2022. Due to the on-going COVID-19 pandemic and the high-risk nature of the study population, all interviews were conducted over the phone. After collecting basic demographic information, interviews focused on five key themes: (1) Experience of the COVID-19 pandemic; (2) Sources of information regarding vaccines; (3) Decision-making process for the COVID-19 and seasonal influenza vaccines; (4) Experiences receiving the COVID-19 and seasonal influenza vaccines; (5) Lived experiences of infectious diseases and vaccination. The five key themes of the IDI were chosen based on a literature review and refined after pilot data collection. Participants received a Visa gift card upon completion of the interview. Interviews were 20–60 minutes in duration, and audio recordings were professionally transcribed.
2.4. Data analysis
Data were manually analyzed using the framework approach [36], [37]. Following a familiarization stage, a thematic framework was developed that largely followed the themes of the IDI. The thematic framework was then systematically applied to all transcripts, and key quotes were abstracted and categorized into a series of charts. The first set of charts categorized data by individual, to provide an overview of each participant. The second set organized information by theme, allowing for analysis across participants, and identification of similarities and differences. For the final set of charts, key quotes were categorized by increasingly specific sub-codes, which were deduced from thematic text-based analysis.
An intersectional lens was applied throughout analysis. Instead of focusing on individual factors, analysis focused on how factors interacted at multiple levels and on differences between and within groups [15]. Our primary interest was at the intersection of gender and race. To facilitate this, data were grouped into four key demographic groups (Black women (BW), Black men (BM), White women (WW) and White men (WM)) at all charting steps. The intersection of gender and race was also considered in the greater context of other key socio-economic factors. Accordingly, as a proxy for socioeconomic status, participant’s ZIP codes were linked to Census data to determine the median household income and percent of residents over the age of 65 living below the federal poverty level.
The lead author, who collected data and did much of the analysis, is a young adult White woman. R.M. and L.P.D., who contributed to design of data collection tools and guided analysis, are also White women, although L.P.D. leads the VALUE Peer Ambassador Education program working primarily in the Black community. S.L.K., a White woman, and S.X.L., a man of Asian descent, provided guidance and expertise on the study population, while E.N.R, a Black woman, provided significant editorial contributions. The composition of the study team may have influenced the type of data that were collected and the themes that emerged during analysis.
2.5. Ethics
All participants provided oral consent and the study protocol was reviewed and deemed as exempt research by the Johns Hopkins School of Medicine Institutional Review Board.
3. Results
3.1. Study participants
Twenty-four adults over the age of 70 were interviewed, with an approximately equal distribution among the four race/gender categories (Table 1 ). Ages were similar in each of the four core groups, but based on ZIP codes, the Black participants lived in neighborhoods with lower median household incomes and higher levels of poverty in those over 65. Levels of education also varied by group, with White men being the most educated. Most Black participants and some White participants lived in seniors’ buildings. This had important implications for vaccine access, as the Baltimore City Health Department offered in-house vaccine clinics in many seniors’ buildings in the spring of 2021.
Table 1.
Participant demographics.
| Black Women | Black Men | White Women | White men | |
|---|---|---|---|---|
| N | 6 | 5 | 6 | 7 |
| Age - mean | 80 | 79 | 83 | 80 |
| Resident of senior's building - N | 5 | 3 | 2 | 3 |
| Location of COVID-19 vaccine - N | ||||
| Senior’s building | 5 | 2 | ||
| Mass vaccination cite | 1 | 2 | 6 | 5 |
| Pharmacy | 1 | |||
| Veterans Affairs | 2 | |||
| Median household incomea- mean | 38,651 | 47,848 | 83,264 | 79,721 |
| % 65 + living in povertya- mean | 20.9 | 18.9 | 8.5 | 11.2 |
| Highest level of education - N | ||||
| Some high school | 1 | 1 | ||
| High school/GED | 1 | 2 | 2 | |
| Some college/post-secondary | 3 | 1 | 1 | |
| Associates/vocational degree | 3 | |||
| College | 1 | 2 | 1 | |
| Some post-graduate | 1 | |||
| Post-graduate | 3 | |||
| Unknown | 1 | |||
| Typology | ||||
| Eager complier (EC) | 2 | 3 | 5 | 6 |
| Hesitant complier (HC) | 4 | 2 | 1 | 1 |
Estimated by linking zip codes to census data.
3.2. Typologies
While all participants received the primary series of COVID-19 vaccines (either one or two doses), two distinct typologies emerged in how participants approached the decision to get the vaccine: eager compliers (EC) and hesitant compliers (HC). Eager compliers actively sought out opportunities for vaccination and did not question the need for or the validity of the vaccine. In contrast, hesitant compliers were skeptical of the vaccine and underwent a thorough decision-making process. More of the Black participants, particularly women, were characterized as HC. Only two White participants, one man and one woman, were HC. In the sections below, we discuss the factors that contributed to eager and hesitant compliers’ decision to receive a COVID-19 vaccine, with an emphasis on differences that emerged at the intersection of race and gender.
3.3. Eager compliers
For the EC, the vaccine was seen as an obvious way to protect themselves from the risk posed by COVID-19. Coupled with low perceived risk of the COVID-19 vaccine and positive past experiences with vaccines, there was little debate as to whether to receive the vaccine.
3.3.1. Vaccine as solution to COVID-19
All the EC felt that they were at significant risk of getting COVID-19, and that the consequences of disease might be severe. For many, age and comorbid conditions contributed to feelings of risk. Faced with the prominent threat of COVID-19, the vaccines were enthusiastically received as a strong source of protection.
As soon as they said that COVID was respiratory, me with COPD and heart problems, I knew right away that I was not going to be staying on side lines talking about “I’ll wait”. (119_BM).
One participant who had been hospitalized with COVID-19 early in the pandemic was particularly desperate to get the vaccine to avoid further illness. In addition to viewing the vaccine as critical to protecting their own health and well-being, several women noted the benefits of vaccination for their loved-ones and community. This included being able to spend time with grandchildren and protecting medically vulnerable family members.
Part was my husband’s health. He’s a lung cancer survivor… and I always thought if God forbid he got it, you know, it would be the end. (1245_WW).
The perceived need of the vaccine is perhaps best exemplified by how many EC persisted to get a vaccine as soon as possible, despite a range of a barriers, including lack of knowledge about where to receive it, difficulties booking appointments online due to low computer literacy, and physical barriers to accessing mass vaccination sites. Physical barriers were particularly prominent for women.
I was being pushed in a wheelchair. I could not walk. My daughter took me up there… I can do nothing by myself. I have to depend on somebody taking me somewhere. (104_BW).
Overall, COVID-19 posed a serious threat for the EC and receipt of the vaccine was an obvious choice that did not require in-depth deliberations.
3.3.2. Low perceived risk of the vaccine
The EC either did not perceive any risks associated with the vaccine or were not deterred by the risks they were aware of. Participants had trust in the systems that led to the development and emergency use authorization of the vaccines, and in some cases, the speed at which the COVID-19 vaccines were developed reinforced this trust.
It just reinforces my trust in the medical establishment that, you know the medical establishment has managed to find a vaccine that is as effective as these are. (118_WM).
Many noted that with so many people vaccinated, unknown side effects were unlikely. When EC did perceive risks associated with the vaccine, they were of minor side effects, a general fear of the unknown, or were immediately qualified with an acknowledgement that severe risks are exceedingly rare. Several White men were readily willing to assume the risk of a rare adverse event given the tremendous perceived benefit of the vaccine.
I know there is a risk. It can kill, it can cause permanent disability, but that is very rare, and that it is risk I am willing to take, because the chances are so small compared to the benefits of the vaccine. (1085_WM).
Taken together, the risks that the EC associated with the vaccine were perceived as minimal, and largely did not influence their decision to get the vaccine.
3.3.3. Positive experiences with vaccines
Many EC expressed general pro-vaccine sentiments, had a history of compliance with vaccine recommendations, and were willing to receive any future COVID-19 vaccines (e.g., boosters) that become available. Participants reported that most of their families and communities were vaccinated, with the notable exception of some participants’ children or grandchildren who refused the vaccine, which lead to significant frustration and conflict within the family. In other cases, mainly for White women, a family-based decision-making process contributed to confidence in the vaccine.
The family had talked about it, and everybody, the older people in my family, it was not a question. It was yes, of course, we're going to get the vaccine. And so, I didn't question it, I knew I would get it. (109_WW).
Many participants had positive memories of getting vaccines as a child, or ensuring that their own children were vaccinated, leaving them no reason to doubt the COVID-19 vaccines. One Black man linked his experience during the pandemic, and willingness to be vaccinated, to past experiences with infectious diseases.
I had a partner who had been exposed to Syphilis… I have lived through AIDS … So that really raised my awareness about the trans-social diseases. So, I was on board when COVID-19 came along… I am savvy about the trans-social diseases (117_BM).
Three White women discussed how they were confident that the COVID-19 vaccines would have the same effect as the polio vaccine.
I am confident that it [the vaccine] is still working… Like when we had… polio years ago and when you took the pills or the polio shots, they worked. I think this is going to be the same thing (1185_WW).
One notable exception to most EC’s positive history with vaccines, was one Black man’s story of becoming ill after receiving an influenza vaccine many years ago, resulting in refusal of the vaccine since. These feelings were, however, restricted to influenza, as the participant was eager to receive the COVID-19 vaccine after hearing a friend’s story of severe disease following infection. Taken together, the EC either had positive experiences with vaccines or viewed the COVID-19 vaccine as distinct from other vaccines, such that they readily complied with recommendations.
3.4. Hesitant compliers: Sources of hesitation
As opposed to EC, who readily accepted vaccination, HC had a variety of concerns about the vaccine and the system providing it.
3.4.1. Risks associated with the vaccine product
For both White and Black HC, vaccine hesitancy stemmed from perceived risks associated with the vaccine product. For the Black women HC, concerns were primarily focused on unknown long-term consequences. Many suggested that accepting the vaccine required assuming some degree of risk.
It will take a long time before we find out exactly…what benefits the vaccine has and what benefits it does not have, and what side effects it has. (101_BW).
Comorbid conditions also contributed to perceived risk associated with the vaccine. One participant suggested that people with underlying conditions, like her diabetes, need to make sure that the vaccine is appropriate for them.
Unless they have underlying sickness and have to ask a lot of questions, think twice… They need to check it out first. Vaccines don’t work for everyone. (116_BW).
For three Black HC, negative experiences with influenza vaccines contributed to their perception of risk associated with the COVID-19 vaccine. Two women fell ill after receiving an influenza vaccine years ago, which prompted them to stop taking the vaccine for several years. One man reported an allergic reaction to the influenza vaccine, such that in consultation with his doctor, he no longer receives it. Although the influenza vaccine was largely seen as separate from the COVID-19 vaccines, these negative experiences did contribute to general feelings of skepticism about the unknown side effects of vaccination.
The two White HC also perceived risks associated with the vaccine product. The White man who was hesitant referred to perceived lack of efficacy of the vaccines and questioned the need for vaccines altogether.
Most of the arguments that I'm hearing… are that this is going to be like every other flu or virus. It will burn itself out. And it’s not that inoculating people is causing it to burn out. (1225_WM).
The White woman, on the other hand, was concerned about the mRNA technology because it was different than vaccines that she had received in the past. Despite having clear questions about the vaccine, she did not want to be viewed as vaccine hesitant.
I wanted to wait and see, because I did not know what the mRNA vaccine was. Nobody knew… I would not describe myself as vaccine hesitant. I just wanted to know what I was getting. (1023_WW).
Although the types of risks identified in relation to the vaccine product differed by race, for both White and Black HC, they figured heavily in deliberations about the vaccine.
3.4.2. Mistrust in vaccine infrastructure
For two Black HC, but for no White HC, uncertainty stemmed from mistrust in the system that made and provided the vaccine, rather than the vaccine itself. They questioned the motives for making the vaccine and the speed of development, leading them to believe that the vaccines were not adequately tested. For one woman, this mistrust was mainly focused on the pharmaceutical industry. In contrast, one man’s long-standing mistrust in the government supported the notion of collusion between the government and pharmaceutical companies.
I just have a question as to the validity of the testing for the vaccines and how quickly they came out… In order for them to have that ability to get something that quickly, they had to have the information from the Government who created it… If you know the history of this country, it would not be the first time that the Government put something on people (102_BM).
For these participants, distrust in the system providing the vaccines stemmed from existing misgivings with the government and pharmaceutical industry, which were heightened by the novelty of COVID-19 and speed at which the vaccines were developed.
3.5. Hesitant compliers: Decision to vaccinate
Despite the uncertainty surrounding the COVID-19 vaccine, all the HC in our sample ultimately decided to receive the vaccine. Below are the factors that were pivotal in the decision to vaccinate.
3.5.1. High perceived risk of COVID-19
For all the Black HC, while risks associated with the vaccine or distrust in the vaccine infrastructure remained prominent, the threat of COVID-19 made the vaccine seem necessary for protection. They ultimately decided to get vaccinated because the risk of COVID-19 out-weighed the perceived risks associated with the vaccine.
With the number of people dying going up, there was no way to say that was fake news. They showed tractor trailers full of bodies. So, it is like you had to have a come to Jesus moment and go and grin and bear it…You were just rolling the dice when you walked out of your door, and so, I decided to stop rolling the dice. (102_BM).
In contrast, one White HC did not feel at great risk due to COVID-19 due to his rural residence, such that the risk of disease did not figure into his decision to get the vaccine. For all other HC, regardless of race or gender, the risk of COVID-19 was the primary factor in their decision to receive the vaccine.
3.5.2. Convenience & ease of access
For those who lived in senior’s buildings, access to in-house vaccine clinics was a major facilitator and directly contributed to the decision to get the vaccine. Participants listed many benefits of these vaccination clinics, including feeling that they were safer and cleaner than mass vaccination sites, convenience due to the absence of lines or long wait-times, and privacy when getting the vaccine.
I have more faith having it in this building. I may not have gone had it been down at one of the centers that’s close to us.… the centers were not that clean. (105_BW).
Convenience and ease of access were not, however, motivators for all participants. One particularly skeptical Black man refused the vaccine that was offered to him in his building.
So, I did not get a vaccination until June, and it was after they had come into the building … I wanted to make sure that when I made a decision, it was not a hurried decision, and I went jumping the line to get a needle in my arm before I knew anything about it. (102_BM).
3.5.3. Fostered trust in the vaccine
External and internal influences fostered trust in the vaccine for both White and Black HC (see representative quotes in Table 2 ). In terms of external influences, most of the Black HC trusted their doctors and consulted them regarding the vaccine. These recommendations were most influential for those who had safety concerns about the vaccine due to their allergies or underlying conditions. In contrast to consulting his personal physician, for the one White man who was a HC, being contacted by Veterans Affairs motivated him to receive the vaccine. Several White participants (both EC and HC), mostly men, reported being contacted by their healthcare system regarding opportunities to get the vaccine, while none of the Black participants reported this. For a Black woman, the recommendation from the governor was pivotal in her decision to receive the vaccine. Across gender and race groups, media coverage of the vaccine was important in the decision-making process. For one White man, the sheer volume of coverage, compared to how rarely other topics, such as influenza, are discussed, lent credibility to how serious COVID-19 was. For a White woman, information about the mRNA vaccine platform from trusted news sources addressed her hesitations. For a Black woman, on the other hand, seeing an older Black woman get vaccinated on the news was influential. Finally, several participants discussed the role of community. Three of the Black HC, two women and one man, discussed how their families contributed to their decision-making process. Vaccination was seen as a way to protect their communities, with all of them specifically discussing their grandchildren. In contrast, the one White man who was a HC stated that he was not influenced by the anti-vaccine opinions being discussed in his community.
Table 2.
Factors that fostered trust in the vaccine among hesitant compliers.
| Recommendation from healthcare professional |
|---|
| I had to ask my doctor, do you think I should take it, because my other shots didn't work out. And he said, no, it doesn’t have the same things in as the flu shot [has] in it. He said it had different medication in it or whatever. So, I said, “well, I’ll try it”. (120_BM) |
| Recommendation from government |
| I would say more that Hogan [the governor] made the difference… how he cared about his people… he was so adamant with making sure that the people of Maryland got the shot and took care of themselves with it. (103_BW) |
| Media coverage |
| Well, they certainly publicized it more, for one thing. I mean, you never see the television monopolized every single day by one thing like this. You never see the flu…so it definitely had me concerned somewhat if it’s that serious, if it’s something to pay attention to. So, it has its effect. You are reminded of it every day. (1225_WM) |
| For a while, I said I wasn’t going to get it and then, I saw an old Black lady on TV… She was an elderly lady, older than me. I believe she was in her nineties, and she was getting, I think they said she got the first shot, I think. And she gave me courage and I said wow. If she is going through with it, I think I can do it too. (101_BW) |
| Community |
| Well, I have been fortunate enough to have great grandchildren and I love them to death. I wanted to be able to see them and I wanted them to be able to visit me. So, any precautions I can do to help them, I am going to do. (101_BW) |
| Lived experiences |
| Well, I am a child of the fifties and sixties. So, we received vaccinations on the regular for school, etcetera. So, I already had a mindset that vaccines were good. (102_BM) |
| Faith |
| It is an unknown thing but step out on your faith. Believe that the technicians and everybody that has handled it before… At least one of them got to know something about the good lord. (101_BW) |
In terms of internal influences, for many in our sample, the concept of vaccines was familiar. Participants noted that they had been receiving vaccines all their lives and were comfortable with them. Several Black women also referred to their faith in fostering trust in the vaccine. Taken together, unlike the near-unanimous perceived risk of COVID-19 as a motivator to vaccinate, external and internal influences had heterogeneous effects. Each resonated with certain participants, according to their specific concerns about the vaccine or lived experiences.
3.6. Gender, race, and their intersection
The ways in which gender, race, and their intersection impacted the vaccine decision-making processes described above are summarized in Table 3 . The most prominent impact of gender norms, roles, and relations manifested in how women discussed the impact of their decision to get vaccinated on their communities, acknowledging the role the vaccine could play in protecting themselves and loved ones. In terms of race, it is notable that many of the HC were Black, particularly Black women. In addition, the sources of hesitation varied by race in that several Black HC but no White HC expressed mistrust of the system that developed and provided vaccines. Finally, at the intersection of gender and race, notable differences in risk perception emerged. The Black women in our sample were particularly concerned about unknown long-term consequences associated with the vaccine whereas the White men knew that rare adverse events were possible, but did not think they would be affected.
Table 3.
Findings on vaccine decision-making by gender, race, and their intersection.
| Gender |
|---|
|
| Race |
|
| Intersection of gender and race |
|
Abbreviations: EC: eager complier; HC: hesitant complier.
4. Discussion
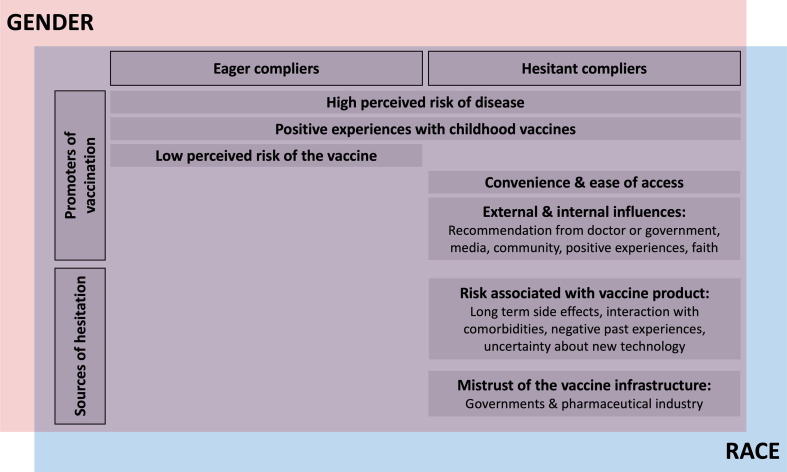
Through IDIs with older adults in the Baltimore area, we found that the risk of severe illness following COVID-19 infection was the primary reason for deciding to receive the COVID-19 vaccine. This was true for both eager and hesitant compliers, even though the two groups approached the decision-making process differently (Fig. 1 ). For EC, the role of vaccines in mitigating the risk of disease was clear, and the decision to vaccinate was as an obvious conclusion. For the HC, however, this conclusion was the result of assessing the competing risks of the vaccine and the disease, and consideration of a variety of external (i.e., recommendations from healthcare professionals) and internal (i.e., past personal experiences with vaccination) influences. In addition, the convenience of in-house vaccine clinics was pivotal for some.
Fig. 1.
Factors that contributed to the decision to vaccinate for eager and hesitant compliers. The promoters of vaccination and the sources of hesitation are summarized for the eager and hesitant compliers. The diagram is positioned at the intersection of gender and race to demonstrate that the process through which individuals approach the decision to vaccinate cannot be disassociated from their lived experiences, which are fundamentally shaped by gender and race.
Our findings on how individuals approached the decision to receive the vaccine cannot be dissociated from their lived experiences, which are fundamentally shaped by gender and race. These observations can be interpreted through existing literature. For example, the role that community played in the decision to vaccinate for many women is consistent with the traditionally feminine roles of caregiving and promoting health [38]. Furthermore, the finding of increased vaccine hesitancy and mistrust among Black participants is likely rooted in the long history of unethical treatment and racism in healthcare settings and should not be viewed as an individual lack of trust, but rather as a failure of the healthcare system [39], [40]. Our finding of hesitant or delayed vaccine acceptance among many of the Black participants is mirrored in national immunization coverage data, where a significant gap in coverage between White and Black Americans was evident in the early stages of the vaccine campaign but largely disappeared by the end of 2021 [41]. Finally, the observation that Black women were concerned about long-term side effects, but White men were not, is consistent with the ‘White Male Effect’, whereby White men perceive the lowest levels of risk and women of color perceive the greatest levels [42]. Researchers have hypothesized that because White men are traditionally in positions of power and control, they feel protected from dangers and are thus more willing to take risks, whereas other groups feel more vulnerable to risks [42]. Along with the observed differences at the intersection of race and gender, we acknowledge that the decision to vaccinate is the result of interactions between various social processes, such that it is difficult to untangle the complex causes of the phenomena observed.
This work has several important implications for public health messaging and the design of vaccine programs. Above all else, highlighting the risk of disease is likely to increase vaccine uptake. Furthermore, the racial and gender differences in the vaccine decision-making process suggest that a ‘one size fits all’ approach to vaccine promotion is likely to be ineffective [43]. Instead, different types of messages may resonate with different groups. For example, emphasizing how receiving the vaccine can protect one’s community and family (particularly grandchildren) is likely to resonate with older women more than men, and vaccine promotion activities located at faith-based institutions or led by faith leaders may have an important effect among Black women. Furthermore, strong recommendations from trusted healthcare providers may be particularly influential among Black participants. In terms of the design of vaccine programs, holding vaccine clinics in seniors’ buildings was a highly effective tool for improving vaccine coverage among hesitant older adults, both men and women alike. Such programs should be expanded to community-dwelling older adults and to include other vaccines recommended for this population.
This work also has several limitations. Based on participant ZIP codes, Black participants were likely of lower socio-economic status than White participants, such that some of the findings attributed to race may be influenced by socio-economic factors or education levels. In addition, interviews were conducted several months after most participants were vaccinated, so it is possible that attitudes may have shifted over time. Because availability of booster vaccines changed substantially over the period of time that interviews were conducted, we were also unable to systematically assess attitudes towards booster vaccines. Finally, the positionality of our research team must also be noted. White women led this research, which likely impacted how data were interpreted.
In conclusion, we find that vaccine acceptance obscures true levels of vaccine hesitancy, and that many who comply with recommendations have unresolved concerns about vaccines. For those who were hesitant, messages that emphasize the risk of COVID-19, along with convenient and accessible opportunities for vaccination, were the most important factors in the decision to ultimately receive the vaccine. Sources of hesitation and the role of external and internal influences on vaccine attitudes varied by gender and race, such that more targeted approaches to vaccine promotion would increase vaccine uptake and better serve this population.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank the study participants, as well as the VALUE ambassadors and service coordinators who helped with recruitment. This work was supported by a NIH/National Institute on Aging Specialized Center of Research Excellence U54 AG062333 awarded to S.L.K. J.R.S was supported by a training award from the Fonds de recherche du Québec – Santé (File #287609).
Data availability
Data will be made available on request.
References
- 1.Kang S.-J., Jung S.I. Age-related morbidity and mortality among patients with COVID-19. Infection & chemotherapy. 2020;52:154. doi: 10.3947/ic.2020.52.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Driscoll M., Dos Santos G.R., Wang L., Cummings D.A., Azman A.S., Paireau J., et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. 2021;590:140–145. doi: 10.1038/s41586-020-2918-0. [DOI] [PubMed] [Google Scholar]
- 3.Chen Y., Klein S.L., Garibaldi B.T., Li H., Wu C., Osevala N.M., et al. Aging in COVID-19: Vulnerability, immunity and intervention. Ageing Res Rev. 2020;101205 doi: 10.1016/j.arr.2020.101205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacDonald N.E. The Sage Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 5.Salmon D.A., Dudley M.Z., Glanz J.M., Omer S.B. Vaccine Hesitancy Causes, Consequences, and a Call to Action. Am J Prev Med. 2015;49:S391–S398. doi: 10.1016/j.amepre.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 6.Dubé E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J.A. Vaccine hesitancy Hum Vacc Immunother. 2013;9:1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brewer N.T., Chapman G.B., Rothman A.J., Leask J., Kempe A. Increasing vaccination: putting psychological science into action. Psychological Science in the Public Interest. 2017;18:149–207. doi: 10.1177/1529100618760521. [DOI] [PubMed] [Google Scholar]
- 8.Flanagan K.L., Fink A.L., Plebanski M., Klein S.L. Sex and Gender Differences in the Outcomes of Vaccination over the Life Course. Annu Rev Cell Dev Bi. 2017;33:577–599. doi: 10.1146/annurev-cellbio-100616-060718. [DOI] [PubMed] [Google Scholar]
- 9.Reny T.T. Masculine Norms and Infectious Disease: The Case of COVID-19. Polit Gender. 2020;16:1–8. [Google Scholar]
- 10.Courtenay W.H. Constructions of masculinity and their influence on men's well-being: a theory of gender and health. Soc Sci Med. 2000;50:1385–1401. doi: 10.1016/s0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- 11.Gustafson P.E. Gender Differences in Risk Perception: Theoretical and Methodological Perspectives. Risk Anal. 1998;18:805–811. doi: 10.1023/b:rian.0000005926.03250.c0. [DOI] [PubMed] [Google Scholar]
- 12.Alsharawy A., Spoon R., Smith A., Ball S. Gender Differences in Fear and Risk Perception During the COVID-19 Pandemic. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.689467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Witteman H.O., Chipenda Dansokho S., Exe N., Dupuis A., Provencher T., Zikmund-Fisher B.J. Risk communication, values clarification, and vaccination decisions. Risk Anal. 2015;35:1801–1819. doi: 10.1111/risa.12418. [DOI] [PubMed] [Google Scholar]
- 14.Morgan R., Klein S.L. The intersection of sex and gender in the treatment of influenza. Curr Opin Virol. 2019;35:35–41. doi: 10.1016/j.coviro.2019.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kapilashrami A., Hankivsky O. Intersectionality and why it matters to global health. Lancet. 2018;391:2589–2591. doi: 10.1016/S0140-6736(18)31431-4. [DOI] [PubMed] [Google Scholar]
- 16.Quinn S, Jamison A, Musa D, Hilyard K, Freimuth V. Exploring the Continuum of Vaccine Hesitancy Between African American and White Adults: Results of a Qualitative Study. Plos Curr. 2016;8:ecurrents.outbreaks.3e4a5ea39d8620494e2a2c874a3c4201. [DOI] [PMC free article] [PubMed]
- 17.Jamison A.M., Quinn S.C., Freimuth V.S. “You don't trust a government vaccine”: Narratives of institutional trust and influenza vaccination among African American and white adults. Soc Sci Med. 2019;221:87–94. doi: 10.1016/j.socscimed.2018.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhanu C., Gopal D.P., Walters K., Chaudhry U.A.R. Vaccination uptake amongst older adults from minority ethnic backgrounds: A systematic review. PLoS Med. 2021;18:e1003826. doi: 10.1371/journal.pmed.1003826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harris L.M., Chin N.P., Fiscella K., Humiston S. Barrier to pneumococcal and influenza vaccinations in Black elderly communities: mistrust. J Natl Med Assoc. 2006;98:1678–1684. [PMC free article] [PubMed] [Google Scholar]
- 20.Quinn S.C., Hilyard K.M., Jamison A.M., An J., Hancock G.R., Musa D., et al. The influence of social norms on flu vaccination among African American and White adults. Health Educ Res. 2017;32:473–486. doi: 10.1093/her/cyx070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Freimuth V.S., Jamison A., Hancock G., Musa D., Hilyard K., Quinn S.C. The Role of Risk Perception in Flu Vaccine Behavior among African-American and White Adults in the United States. Risk Anal. 2017;37:2150–2163. doi: 10.1111/risa.12790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Freimuth V.S., Jamison A.M., An J., Hancock G.R., Quinn S.C. Determinants of trust in the flu vaccine for African Americans and Whites. Soc Sci Medicine. 1982;2017(193):70–79. doi: 10.1016/j.socscimed.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quinn S.C., Jamison A., Freimuth V.S., An J., Hancock G.R., Musa D. Exploring racial influences on flu vaccine attitudes and behavior: Results of a national survey of White and African American adults. Vaccine. 2017;35:1167–1174. doi: 10.1016/j.vaccine.2016.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fast H.E., Zell E., Murthy B.P., Murthy N., Meng L., Scharf L.G., et al. Booster and Additional Primary Dose COVID-19 Vaccinations Among Adults Aged ≥65 Years — United States, August 13, 2021–November 19, 2021. Morb Mortal Wkly Rep. 2021;70:1735–1739. doi: 10.15585/mmwr.mm7050e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.International Vaccine Access Center and Morgan State University. Evaluation of Baltimore City Flu Vaccination Initiative, 2020. Baltimore, MD2021.
- 26.Kreps S., Kriner D. Factors influencing Covid-19 vaccine acceptance across subgroups in the United States: Evidence from a conjoint experiment. Vaccine. 2021;39:3250–3258. doi: 10.1016/j.vaccine.2021.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.QuickFacts Baltimore City, Maryland (County). United States Census Bureau, ; 2021.
- 28.United Sates Census Bureau. American Community Survey Data. 2019.
- 29.Maryland Department of Health. Coronavirus Disease 2019 (COVID-19) Outbreak - Vaccinations in Maryland. 2022.
- 30.Maul A., Reddy K., Joshi M. Vaccine equity index shows reduction in Maryland COVID-19 vaccination disparity in less than two months. NEJM Catalyst Innovations in Care Delivery. 2021;2 [Google Scholar]
- 31.Cardona S., Felipe N., Fischer K., Sehgal N.J., Schwartz B.E. Vaccination disparity: quantifying racial inequity in COVID-19 vaccine administration in Maryland. Journal of Urban Health. 2021;98:464–468. doi: 10.1007/s11524-021-00551-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee KH, Marx M. Baltimore City: County-level comparisons of COVID-19 cases and deaths. 2021.
- 33.Baltimore City Health Department. Baltimore City COVID-19 Vaccination Dashboard. 2022.
- 34.Centers for Disease Control and Prevention. COVIDVavView - COVID-19 Vaccination Coverage and Vaccine Confidence Among Adults. 2022.
- 35.Shapiro J.R., Li H., Morgan R., Chen Y., Kuo H., Ning X., et al. Sex-specific effects of aging on humoral immune responses to repeated influenza vaccination in older adults. npj Vaccines. 2021;6:147. doi: 10.1038/s41541-021-00412-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ritchie J., Lewis J. sage; London: 2003. Qualitative research practice: A guide for social science students and researchers. [Google Scholar]
- 37.Gale N.K., Heath G., Cameron E., Rashid S., Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. Bmc Med Res Methodol. 2013;13:1–8. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heise L., Greene M.E., Opper N., Stavropoulou M., Harper C., Nascimento M., et al. Gender inequality and restrictive gender norms: framing the challenges to health. Lancet. 2019;393:2440–2454. doi: 10.1016/S0140-6736(19)30652-X. [DOI] [PubMed] [Google Scholar]
- 39.Corbie-Smith G. Vaccine Hesitancy Is a Scapegoat for Structural Racism. Jama Heal Forum. 2021;2:e210434. doi: 10.1001/jamahealthforum.2021.0434. [DOI] [PubMed] [Google Scholar]
- 40.Bajaj S.S., Stanford F.C. Beyond Tuskegee — Vaccine Distrust and Everyday Racism. N Engl J Med. 2021;384:e12. doi: 10.1056/NEJMpv2035827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Centers for Disease Control. Demographic trends of people receiving COVID-19 vaccinations in the United States. 2021.
- 42.Finucane M.L., Slovic P., Mertz C.K., Flynn J., Satterfield T.A. Gender, race, and perceived risk: The 'white male' effect. Heal Risk Soc. 2000;2:159–172. [Google Scholar]
- 43.Shapiro J.R., Klein S.L., Morgan R. Stop ‘controlling’ for sex and gender in global health research. Bmj Global Heal. 2021;6:e005714. doi: 10.1136/bmjgh-2021-005714. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.